To compare the preoperative and postoperative bilateral symmetry between OD and OS eyes that have undergone femto-LASIK using the Ziemer LDV femtosecond laser system, the SCHWIND AMARIS Excimer Laser and the Aberrationfree™ profiles implemented in the SCHWIND Custom Ablation Manager software.
MethodsA total of 25 LASIK patients were bilaterally evaluated at the six-month follow-up visit. In all cases standard examinations, pre- and postoperative analysis with corneal wavefront topography (OPTIKON Scout) were performed. Aberration-free™ aspheric treatments were devised using the Custom Ablation Manager software and ablations were performed by means of the SCHWIND AMARIS flying-spot excimer laser system (both SCHWIND eyetech- solutions). In all cases LASIK flaps were created using an LDV femtosecond laser (Ziemer Group).
The OD/OS bilateral symmetry was evaluated in terms of corneal wavefront aberration.
ResultsPreoperatively, 11 Zernike terms showed significant bilateral (OS-vs.-OD) symmetry, and only 6 Zernike terms were significantly different. Overall, 23 out of the 25 patients showed significant bilateral symmetry, and only 2 out of 25 patients showed significant differences. None of the aberration metrics changed from pre- to postoperative values by a clinically relevant amount. At the 6-month postoperative visit, 12 Zernike terms showed significant symmetry, and 8 terms were significantly different. Overall, 22 out of 25 patients showed significant bilateral symmetry (OS vs. OD), and only 3 out of 25 patients showed significant differences. Also, this postoperative examination revealed that 6 Zernike terms lost significant OS-vs.-OD symmetry, but 4 Zernike terms gained significant symmetry. Finally, 4 patients lost significant bilaterality, and 2 patients gained significant bilaterality: bilateral symmetry between eyes was better maintained in those patients with a clear preoperative bilateral symmetry.
ConclusionsAberration-Free Treatments with the SCHWIND AMARIS did not induce clinically significant aberrations, maintained the global OD-vs.-OS bilateral symmetry, as well as the bilateral symmetry between corresponding Zernike terms (which influences binocular summation).
Comparar la simetría bilateral (OD-OS) preoperativa y postoperativa, en ojos sometidos a una operación de femto-LASIK donde se empleó el sistema láser de femtosegundos Ziemer LDV, el láser de excímero SCHWIND AMARIS y donde se implementaron perfiles de ablación Aberration-free™ (sin aberraciones) en el software de control del láser (SCHWIND Custom Ablation Manager).
MétodosSe evaluaron bilateralmente un total de 25 pacientes de LASIK transcurridos 6 meses de la operación. En todos los casos se llevó a cabo una revisión estándar, y se realizaron medidas pre- y postoperativas de topografía corneal (OPTIKON Scout). Se diseñaron tratamientos asféricos de tipo Aberration-free™ utilizando el software de control del láser, denominado Custom Ablation Manager. La ablación se realizó mediante el sistema láser de excímero SCHWIND AMARIS, con tecnología de barrido de punto flotante (flying-spot). Tanto el software como el sistema láser son de SCHWIND eye-tech-solutions. En todos los casos el “lentículo” del LASIK (también conocido como “colgajo” o “flap”) se creó mediante un láser de femtosegundos LDV (Grupo Ziemer).
Se evaluó la simetría bilateral OD/OS comparando la aberración de onda asociada a la superficie anterior de la córnea en uno y otro ojo.
Resultados: Antes de la operación, existía simetría bilateral OD-OS para 11 términos de Zernike, mientras que sólo 6 de ellos eran significativamente diferentes. Globalmente, 23 de los 25 pacientes exhibían simetría bilateral, mientras que sólo para 2 de los 25 pacientes se observaron diferencias significativas. Ninguno de los parámetros utilizados para cuantificar las aberraciones varió de manera significativa (es decir, en una cantidad clínicamente relevante) debido a la operación. En la revisión postoperativa de los 6 meses, se observó una simetría significativa para 12 términos de Zernike, mientras que 8 términos resultaron ser significativamente distintos. Globalmente, 22 de los 25 pacientes presentaban simetría bilateral OD-OS significativa, mientras que sólo para 3 de los 25 pacientes se observaron diferencias significativas entre los dos ojos. En esta revisión postoperativa también se observó que para 6 términos de Zernike se había perdido una fracción significativa de la simetría OS-OD, mientras que para 4 términos la simetría aumentó de manera significativa. Para terminar, 4 pacientes perdieron una fracción significativa de la bilateralidad, mientras que en 2 pacientes la bilateralidad aumentó de manera significativa: la simetría bilateral entre los dos ojos se logró mantener mejor en aquellos pacientes que ya antes de la operación presentaban una clara simetría bilateral.
ConclusionesLos tratamientos Aberration-FreeTM realizados con el sistema láser SCHWIND AMARIS no indujeron una cantidad clínicamente significativa de aberraciones y lograron mantener globalmente tanto la simetría bilateral OD-OS como la simetría bilateral entre términos de Zernike equivalentes (aspecto que influye sobre la sumación binocular).
Human vision is a binocular process. Having two eyes gives binocular summation, with which the ability to detect faint objects is enhanced.1 It can make stereopsis possible, in which the parallax provided by the two eyes’ different positions on the head gives precise depth perception.2 Such binocular vision is usually accompanied by binocular fusion, in which a single image is seen despite each eye's having its own image of any object.2
Literature suggests that marked anisometropia is uncommon, in terms of either the magnitude of sphere or the amount of astigmatism,3 with few notable exceptions4 concluding that the axis of astigmatism does not follow any particular rule (mirror or direct symmetry) between right and left eyes.
Howland and Howland, employing the cross-cylinder aberroscope method they invented,5 found that the optical aberrations of the eye differ greatly from subject to subject and are seldom symmetrical. Liang and Williams, using a Shack-Hartmann wave-front sensor,6 found that although the pattern of aberrations varies from subject to subject, the aberrations (including irregular ones) of the left eye and those of the right eye of the same subject are correlated, indicating that they are not just random defects. Porter et al.7 confirmed this observation in a large population.
The Indiana Aberration Study by Thibos et al.8 characterized the aberration structure and the effects of these aberrations on vision, for a reasonably large population of normal, healthy eyes in young adults, and verified the hypothesis of bilateral symmetry.
Marcos and Burns9 found that not only aberrations but also cone directionality varies across subjects, and that these two functions show a left-right eye symmetry.
Wang et al.10 found that event though the anterior corneal surface's wave aberration varied greatly across subjects, a moderate-to-high degree of mirror symmetry existed between right and left eyes.
To our knowledge, very few studies in the literature have addressed the issue of symmetry of aberrations between eyes after corneal laser refractive surgery.11 Jiménez et al.11 found that binocular function deteriorates more than monocular function after LASIK, and that this deterioration increases as the interocular differences in terms of aberrations and corneal shape increase. They found that interocular differences above 0.4μm of the Root-Mean-Square (RMS) for a 5-mm analysis diameter, lead to a decrease of more than 20% in binocular summation.
If binocular symmetry is manifested on virgin human eyes and it is an important factor for binocular vision, it shall be interesting to assess whether or not the existing symmetry is maintained after treating the cornea for ametropia correction using corneal laser refractive surgery.
Taking into account that corneal ablation in standard refractive-surgery treatments induces aberrations (one of the most significant side-effects in myopic LASIK is the induction of spherical aberration,12 which causes halos and reduced contrast sensitivity13), special ablation patterns were designed to preserve the preoperative level of high-order aberrations (HOAs).14-16
In the current study we present measurements of the corneal wavefront aberration in 50 eyes (right and left eyes of 25 subjects), both preoperatively and 6 months after non-customised treatment. We analyzed the correlation of individual aberrations across the population, as well as the correlation of aberrations between the right and left eyes of the same subjects. In this study, we used non-customised “Aberrationneutral” profiles, i.e., ablations were optimized to induce no change in wavefront aberration within the Optical Zone (OZ) other than sphere and cylinder components, leaving all existing HOAs unchanged because the best-corrected visual acuity (BCVA), in this patient, has been unaffected by the pre-existing aberrations (Artal P, What aberration pattern (if any) produces the best vision?, 6th International Wavefront Congress, Athens, Greece; February 2005). Thus, to compensate for the aberrations induction observed with other types of profile definitions,17 several sources of aberration might be considered. For example, some of those sources of aberration are related to the loss of efficiency of the laser ablation for non-normal incidence.18-20
Patients and Methods50 eyes (25 patients) that had been treated with the AMARIS “aberration neutral” (Aberration-Free™) aspheric ablation profiles were retrospectively analysed.
Inclusion criteria for review were bilateral surgery on the same day targeted for emmetropia, preoperative best spectacle corrected visual acuity (BCVA) ≥ 20/25 (logMAR ≤ 0.1) in both eyes, no signs of amblyopia, and successful completion of the 6-month follow-up.
Six-months follow-up data were available for all 50 eyes (100%), and their preoperative data were as follows: mean manifest defocus refraction: -2.47±2.51 D (range, -8.13 to +5.63 D) and mean manifest astigmatism magnitude: 2.02±0.91 D (range, 0.00 to 4.75 D). For all eyes we measured corneal topography21 and derived corneal wavefront aberrations,22,23 up to the 7th Zernike order (35 terms) (Keratron-Scout, OPTIKON2000, Rome, Italy), manifest refraction, uncorrected visual acuity24 (UCVA) and BCVA. Measurements were performed preoperatively and also 1, 3, and 6 months after surgery.
All ablations were non-wavefront-guided but were based on aspheric25 aberration-neutral (Aberration-Free™) profiles (and not on the profiles proposed by Munnerlyn26) to balance the induction of spherical aberration27,28 (prolateness optimization29,30). This approach included a multidynamic aspherical transition zone, aberration and focus shift compensation due to tissue removal, pseudo-matrix-based spot positioning, enhanced compensation for the loss of efficiency;31 all based on theoretical equations validated with ablation models and clinical evaluations.
A 6.5mm central and fully corrected ablation zone was used in all eyes, together with a variable transition size that was automatically provided by the laser depending on the planned refractive correction (6.7mm to 8.9mm). The ablation was performed using the AMARIS excimer laser (SCHWIND eye-tech-solutions, Kleinostheim, Germany), which is a flying-spot laser system that uses real ablative spot volume locally considered through a self-constructing algorithm and that controls for the local repetition rates to minimize the thermal load of the treatment.32 Therefore, the ablated surface with the aspheric aberration-neutral (Aberration-Free™) profiles should be very smooth, possibly leading also to some benefits in terms of HOAs. Finally, all these optimizations theoretically diminish the induced wavefront aberration after myopic LASIK.The AMARIS laser system works at a true repetition rate of 500Hz and produces a beam with a size of 0.54mm (Full-Width-at-Half-Maximum, FWHM) and a super-Gaussian spot profile.33,34 High-speed eye tracking (pupil and limbus tracker with cyclotorsional tracking) with a 1050Hz acquisition rate is accomplished with a 3-ms latency time.35
All flaps were created using a LDV femtosecond laser (Ziemer Group) with a 100μm nominal flap thickness.
Optical errors centred on the line-of-sight,36 representing the wavefront aberration, are described by means of Zernike polynomials37 and their corresponding coefficients using OSA standard,38 and analysed for a standardised diameter of 6mm in order to derive corneal wavefront aberrations.
Correlations for Bilateral Symmetry of Zernike Terms Across SubjectsTo test this hypothesis, we plotted left-vs.-right-eye scatter graphs for each Zernike term to analyse the predicted correlations between the two eyes. These plots reveal, for our sample, which Zernike modes show symmetry and which type of symmetry they show (pre- and postoperatively). What is expected is that 0 modes show even symmetry; -odd modes show even symmetry; -even modes show odd symmetry; +odd modes show odd symmetry and +even modes show even symmetry. The slope and intercept of the linear regression (least-square fitting) were calculated for each Zernike term up to the seventh radial order (36 coefficients). We assessed the statistical significance of the correlations using Student's T-test; the Coefficient of Determination (r2) was also employed and the significance of the correlations has been evaluated assuming a metric that is distributed approximately as t with N—2 degrees of freedom, where N is the size of the sample.
Correlations for Symmetry of Aberrations in Right and Left Eye of the Same SubjectsTaking symmetry into account, we plotted for each subject left-vs.-right eye scatter graphs of the Zernike coefficients. These plots reveal which patients in our sample show symmetry (pre- and postoperatively). The slope and intercept of the linear regression (least-square fitting) were calculated for each subject (25 patients). We assessed the statistical significance of the correlations using Student's T-tests; the Coefficient of Determination (r2) was also employed and the significance of the correlations has been evaluated assuming a metric that is distributed approximately as t with N—2 degrees of freedom, where N is the size of the sample.
Differences for Symmetry of Aberrations in Right and Left eye of the Same SubjectsTaking symmetry into account, we compared the Zernike coefficients obtained for the left and right eyes of the same subjects. We assessed the statistical significance using paired Student's T-tests.
Dioptrical Differences in Corneal Wavefront Aberration Between the Right and Left Eyes of the Same SubjectsFor our analysis, the concept of equivalent defocus (DEQ) has been used as metric to be able to associate a dioptric power with the RMS of the Zernike coefficients.
DEQ is defined as the amount of defocus required to produce the same wavefront variance produced by one or more HOAs. A simple formula allows us to compute the DEQ in diopters if we know the total RMS wavefront error of the Zernike modes in question:
where Me is the DEQ in diopters, RMS is the RMS wavefront error of the Zernike modes in question, and PD is the pupil diameter considered for the wavefront-aberration analysis.On virgin eyes, DEQ as proposed by Thibos et al.8 seems to be relatively insensitive to a change of analysis diameter.
Taking Symmetry into Account and Analysing the RMS of the Differential Corneal Wavefront Aberrations (RMS(ΔHOAb)) in DEQThis theoretical difference, expressed in terms of DEQ, does not directly provide important answer to the binocular analysis. From experimental results11 on binocular performance it was found that interocular differences above 0.4μm of RMS for a 5mm analysis diameter (0.4 D), lead to a decrease of more than 20% in binocular summation, whereas 0.2μm of RMS (0.25 D), lead to a decrease of about 10%.
We have set a threshold value of 0.25 D to establish whether or not the differential corneal wavefront aberration between the left and the right eye was clinically relevant.
Changes in Bilateral Symmetryof Zernike Terms as a Result of Refractive SurgeryWe analysed the number of Zernike terms that postoperatively lost, gained or preserved symmetry, compared to the preoperative baseline.
Changes in Bilateral Symmetryof Wavefront Aberration as a Result of Refractive SurgeryWe analysed the number of patients that postoperatively lost, gained or preserved symmetry, compared to the preoperative baseline.
Statistical AnalysisThe level of statistical significance was taken to be P<0.05.
ResultsAdverse EventsNeither adverse events nor complications were observed intra- or postoperatively. No patient needed or demanded a retreatment of either eye.
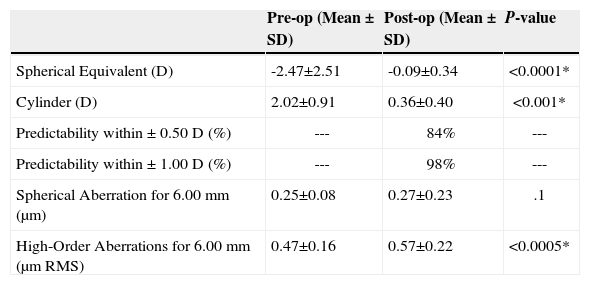
Refractive OutcomesConcerning refractive outcomes, we merely want to outline the fact that at 6 months postoperatively both the spherical equivalent and the cylinder were significantly reduced to subclinical values: mean residual defocus refraction was -0.09±0.34 D (range: -1.00 to +0.75 D; P<.0001) and mean residual astigmatism magnitude 0.36±0.40 D (range: 0.00 to 1.50 D; P<.001). Also, 84% of eyes (n=42) were within ±0.50 D of the attempted correction (Table 1). Despite the fact that the distribution of the corrections was bimodal (i.e., split between myopic and hyperopic corrections), and that single analysis across both groups probably isn’t justified from a rigorous point of view, the analysis showed only a small difference when compared within each group individually.
Comparison of refractive outcomes 6 months after surgery for all 50 eyes
| Pre-op (Mean ± SD) | Post-op (Mean ± SD) | P-value | |
| Spherical Equivalent (D) | -2.47±2.51 | -0.09±0.34 | <0.0001* |
| Cylinder (D) | 2.02±0.91 | 0.36±0.40 | <0.001* |
| Predictability within ± 0.50 D (%) | --- | 84% | --- |
| Predictability within ± 1.00 D (%) | --- | 98% | --- |
| Spherical Aberration for 6.00 mm (μm) | 0.25±0.08 | 0.27±0.23 | .1 |
| High-Order Aberrations for 6.00 mm (μm RMS) | 0.47±0.16 | 0.57±0.22 | <0.0005* |
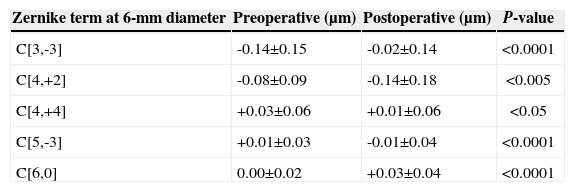
Only 5 high-order Zernike terms (out of 30) changed significantly after treatment (Table 2), whereas 25 high-order Zernike terms (out of 30) did not change after treatment. For all of them, the variation was well below the clinical relevance.
Comparison of induced corneal aberrations after refractive surgery for all 50 eyes
| Zernike term at 6-mm diameter | Preoperative (μm) | Postoperative (μm) | P-value |
| C[3,-3] | -0.14±0.15 | -0.02±0.14 | <0.0001 |
| C[4,+2] | -0.08±0.09 | -0.14±0.18 | <0.005 |
| C[4,+4] | +0.03±0.06 | +0.01±0.06 | <0.05 |
| C[5,-3] | +0.01±0.03 | -0.01±0.04 | <0.0001 |
| C[6,0] | 0.00±0.02 | +0.03±0.04 | <0.0001 |
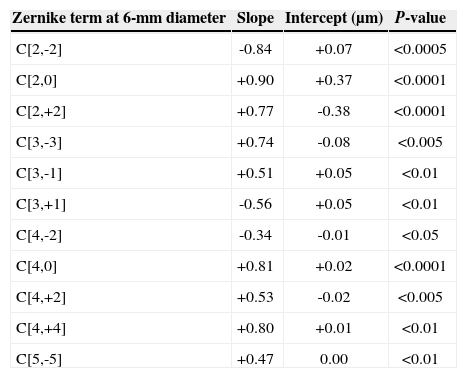
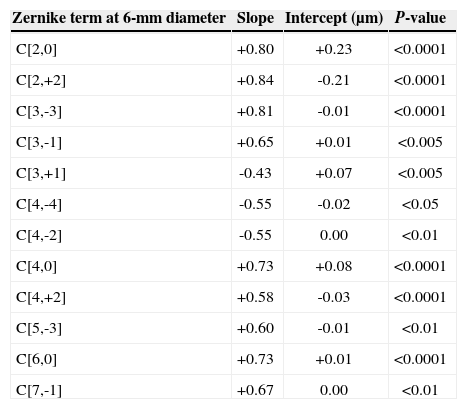
Preoperatively 11 Zernike terms showed significant OS-vs.-OD bilateral symmetry (Table 3), whereas 6 months postoperatively 12 Zernike terms showed significant OS-vs.-OD symmetry (Table 4). For the sake of simplicity, tables 3 and 4 report only the coefficients for which a significant correlation in bilateral symmetry was observed.
Preoperative correlations for bilateral symmetry of Zernike terms across subjects for all 25 subjects (terms in bold face means these coefficients also correlated postoperatively, whereas regular face means these coefficients no longer correlated postoperatively)
| Zernike term at 6-mm diameter | Slope | Intercept (μm) | P-value |
| C[2,-2] | -0.84 | +0.07 | <0.0005 |
| C[2,0] | +0.90 | +0.37 | <0.0001 |
| C[2,+2] | +0.77 | -0.38 | <0.0001 |
| C[3,-3] | +0.74 | -0.08 | <0.005 |
| C[3,-1] | +0.51 | +0.05 | <0.01 |
| C[3,+1] | -0.56 | +0.05 | <0.01 |
| C[4,-2] | -0.34 | -0.01 | <0.05 |
| C[4,0] | +0.81 | +0.02 | <0.0001 |
| C[4,+2] | +0.53 | -0.02 | <0.005 |
| C[4,+4] | +0.80 | +0.01 | <0.01 |
| C[5,-5] | +0.47 | 0.00 | <0.01 |
6-month postoperative correlations for bilateral symmetry of Zernike terms across subjects for all 25 subjects (terms in bold face means these coefficients also correlated preoperatively, whereas regular face means these coefficients did not correlate preoperatively)
| Zernike term at 6-mm diameter | Slope | Intercept (μm) | P-value |
| C[2,0] | +0.80 | +0.23 | <0.0001 |
| C[2,+2] | +0.84 | -0.21 | <0.0001 |
| C[3,-3] | +0.81 | -0.01 | <0.0001 |
| C[3,-1] | +0.65 | +0.01 | <0.005 |
| C[3,+1] | -0.43 | +0.07 | <0.005 |
| C[4,-4] | -0.55 | -0.02 | <0.05 |
| C[4,-2] | -0.55 | 0.00 | <0.01 |
| C[4,0] | +0.73 | +0.08 | <0.0001 |
| C[4,+2] | +0.58 | -0.03 | <0.0001 |
| C[5,-3] | +0.60 | -0.01 | <0.01 |
| C[6,0] | +0.73 | +0.01 | <0.0001 |
| C[7,-1] | +0.67 | 0.00 | <0.01 |
Preoperatively only 6 (C[4,-4], C[4,-2], C[5,+3], C[6,+6], C[7,-7], C[7,+3]) out of 33 Zernike terms were significantly different when comparing OS vs. OD for the same subject, whereas 6 months postoperatively 8 terms (C[4,-2], C[4,+4], C[5,+1], C[6,-6], C[6,-4], C[6,+2], C[7,-5], C[7,+3]) were significantly different when comparing OS vs. OD. For all of them, the difference was well below the clinical relevance.
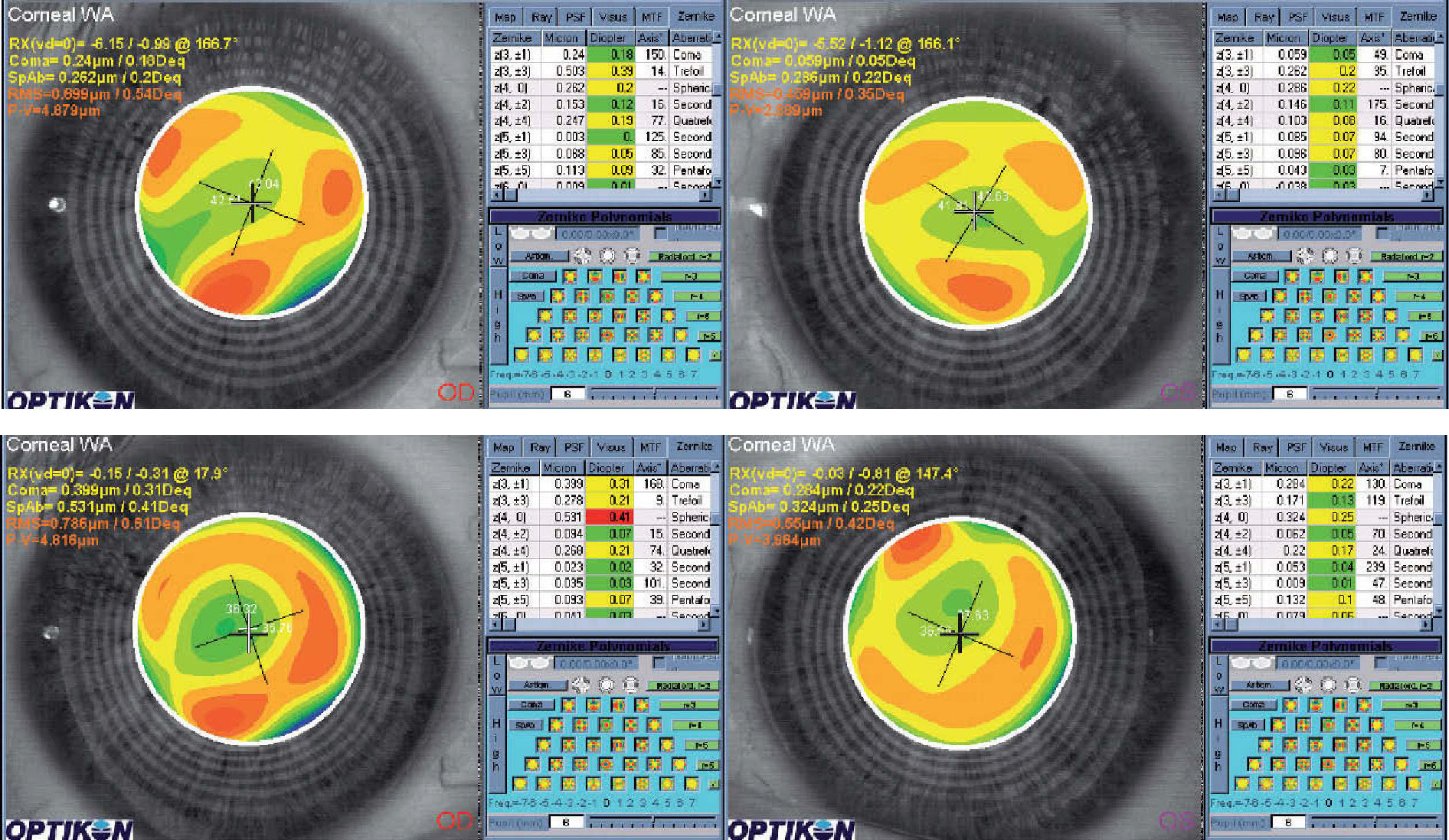
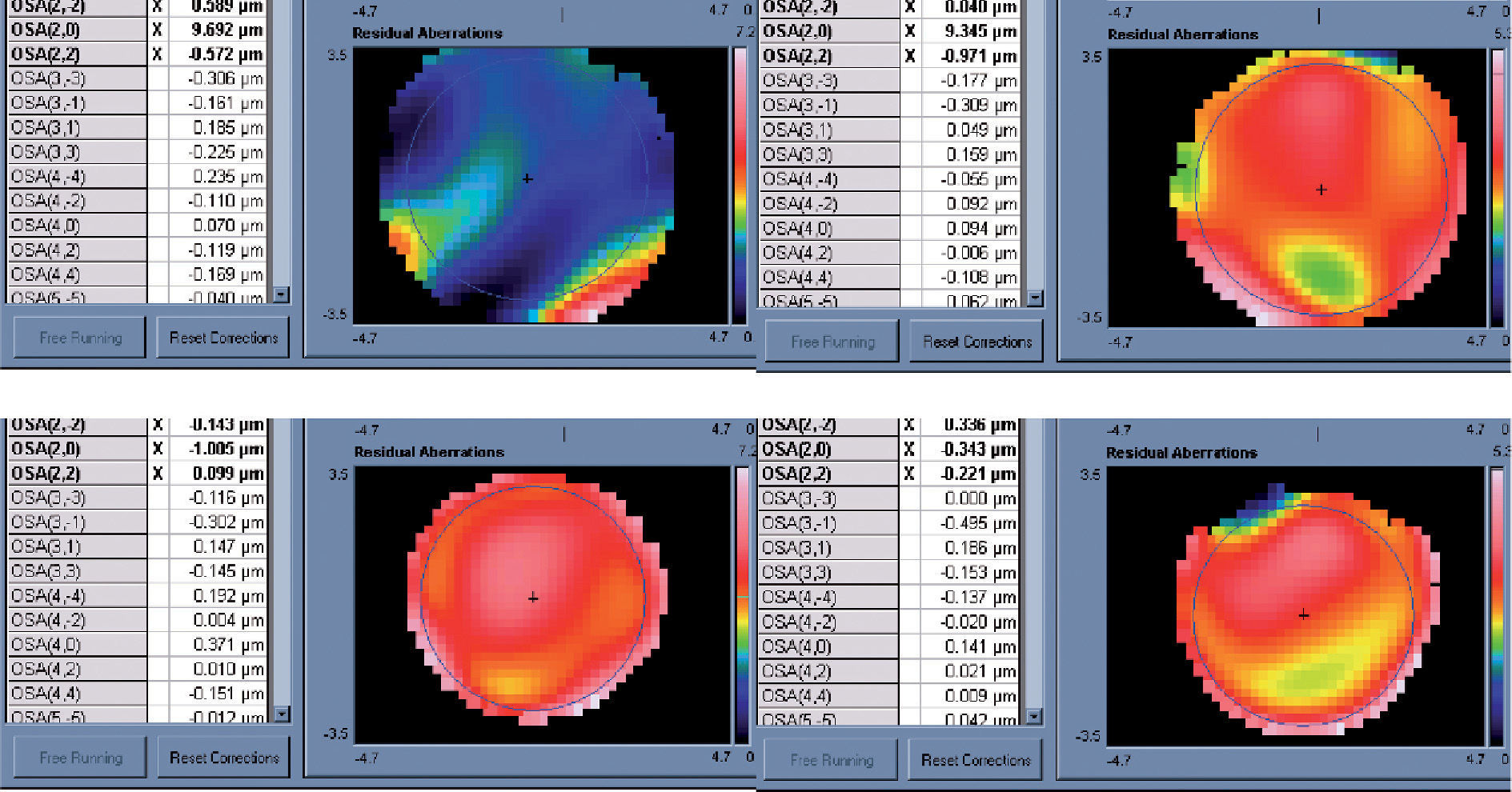
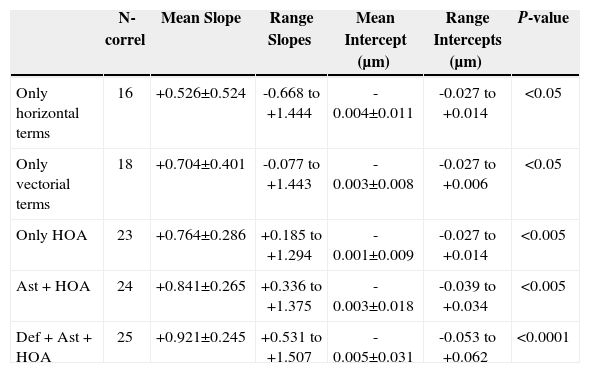
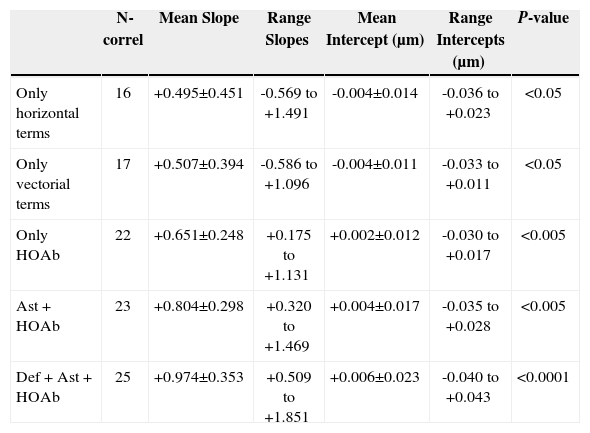
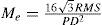
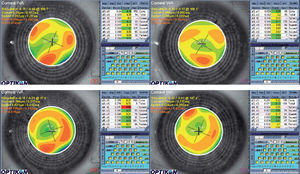
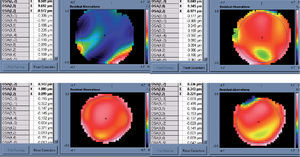
Correlations for Symmetry of Aberrations in Right and Left Eye of the Same SubjectsPreoperatively 23 of 25 patients showed significant OS-vs.-OD bilateral symmetry (Table 5, the example of one patient is shown in Figure 1 for corneal aberrations and in Figure 2 for ocular aberrations), whereas 6 months postoperatively 22 of 25 patients showed significant OS-vs.-OD bilateral symmetry (Table 6, the postoperative example of the same patient is shown in Figure 1 for corneal aberrations and in Figure 2 for ocular aberrations). For the sake of simplicity, tables 5 and 6 report the number of subjects for which a significant correlation in bilateral symmetry was observed, as well as mean values, standard deviation and ranges of the slopes and intercepts for different sets of Zernike terms.
Preoperative correlations for symmetry of right- vs. left-eye aberrations of same subjects for 36 Zernike terms (0th-7th radial order)
| N-correl | Mean Slope | Range Slopes | Mean Intercept (μm) | Range Intercepts (μm) | P-value | |
| Only horizontal terms | 16 | +0.526±0.524 | -0.668 to +1.444 | -0.004±0.011 | -0.027 to +0.014 | <0.05 |
| Only vectorial terms | 18 | +0.704±0.401 | -0.077 to +1.443 | -0.003±0.008 | -0.027 to +0.006 | <0.05 |
| Only HOA | 23 | +0.764±0.286 | +0.185 to +1.294 | -0.001±0.009 | -0.027 to +0.014 | <0.005 |
| Ast + HOA | 24 | +0.841±0.265 | +0.336 to +1.375 | -0.003±0.018 | -0.039 to +0.034 | <0.005 |
| Def + Ast + HOA | 25 | +0.921±0.245 | +0.531 to +1.507 | -0.005±0.031 | -0.053 to +0.062 | <0.0001 |
HOA =high-order aberrations; Ast = astigmatism; Def = defocus.
6-month postoperative correlations for symmetry of aberrations in the right and left eyes of the same subjects for 36 Zernike terms (0th-7th radial order)
| N-correl | Mean Slope | Range Slopes | Mean Intercept (μm) | Range Intercepts (μm) | P-value | |
| Only horizontal terms | 16 | +0.495±0.451 | -0.569 to +1.491 | -0.004±0.014 | -0.036 to +0.023 | <0.05 |
| Only vectorial terms | 17 | +0.507±0.394 | -0.586 to +1.096 | -0.004±0.011 | -0.033 to +0.011 | <0.05 |
| Only HOAb | 22 | +0.651±0.248 | +0.175 to +1.131 | +0.002±0.012 | -0.030 to +0.017 | <0.005 |
| Ast + HOAb | 23 | +0.804±0.298 | +0.320 to +1.469 | +0.004±0.017 | -0.035 to +0.028 | <0.005 |
| Def + Ast + HOAb | 25 | +0.974±0.353 | +0.509 to +1.851 | +0.006±0.023 | -0.040 to +0.043 | <0.0001 |
HOA =high-order aberrations; Ast = astigmatism; Def = defocus
Preoperatively, only 2 out of 25 patients showed significant OS-vs.-OD differences, whereas 6 months postoperatively only 3 out of 25 patients showed significant OS-vs.-OD differences.
Dioptrical Differences of Corneal Wavefront Between the Right and Left Eyes of the Same SubjectsPreoperatively, only 4 out of 25 patients showed clinically relevant OS-vs.-OD differences (i.e., larger than 0.25 D), whereas 6 months postoperatively only 2 out of 25 patients showed clinically relevant OS-vs.-OD differences (i.e., larger than 0.25 D).
Changes in Bilateral Symmetry of Zernike Terms as a Result of Refractive SurgerySix months postoperatively, 3 Zernike terms (C[2,-2], C[4,+4], C[5,-5]) had lost significant OS-vs.-OD correlation symmetry, 4 Zernike terms (C[4,-4], C[5,-3], C[6,0], C[7,-1]) had gained significant correlation symmetry, and 29 Zernike terms preserved correlation symmetry OS vs. OD compared to the preoperative baseline.
Six months postoperatively, for 6 Zernike terms (C[4,+4], C[5,+1], C[6,-6], C[6,-4], C[6,+2], C[7,-5]) the differences in OS-vs.-OD symmetry increased significantly, for 4 Zernike terms (C[4,-4], C[5,+3], C[6,+6], C[7,-7]) the differences in symmetry decreased significantly, and for 26 Zernike terms the OS-vs.-OD symmetry was preserved, compared to the preoperative baseline.
Changes in Bilateral Symmetry of Wavefront Aberration as a Result of Refractive SurgerySix months postoperatively, 3 patients (#2, #15, #22) lost significant OS-vs.-OD correlation symmetry, 1 patient (18) gained significant correlation symmetry, and 21 patients preserved OS-vs.-OD correlation symmetry, compared to the preoperative baseline.
6 months postoperatively, for 2 patients (#6, #15) the differences in OS-vs.-OD symmetry increased significantly, for 1 patient (#7) the differences in symmetry decreased significantly, and for 22 patients the OS-vs.-OD symmetry was preserved, compared to the preoperative baseline.
An example of a patient well maintaining bilateral symmetry is shown in Figure 1 for corneal aberrations and in Figure 2 for ocular aberrations.
DiscussionThe aim of this study was to evaluate the effects of laser corneal refractive surgery on the bilateral symmetry of the corneal wavefront aberration; in particular, following a treatment performed with the AMARIS system, which is based on an Aberration-Free™ ablation profile. The advantage of the Aberration-Free™ ablation profile is that it aims to be neutral for HOA, leaving the visual print of the patient as it was preoperatively with the best spectacle correction. If the aimed Aberration-Free concept would have been rigorously achieved, the bilateral symmetry between eyes would have been automatically obtained. In our group of patients, the aimed Aberration-Free concept does not hold rigorously true, but we had a very minor increase in corneal aberrations for a 6mm pupil.
Our follow-up included 100% of the cases at 6 months and, although no nomogram adjustments were applied, in none of the cases retreatment was necessary. As a proof of stability, longer follow-ups and larger number of eyes would be more convincing, even though refractive spherical and astigmatic results are stable after 3 months.
Residual defocus averaged about -0.1 D, and residual cylinder about 0.4 D, with 84% of the eyes being within 0.50 D and 98% within 1.0 D of the target correction.
In our study, at the 6-month follow-up the percentage of eyes with an UCVA of 20/32 or better was 100% and 84% had an UCVA of 20/20 or better. No single eye had a loss of more than 1 line of BCVA, and 5 eyes had gained 2 or more lines of BCVA (P<.01).
As can be seen from the data presented herein, noncustomised femtosecond LASIK performed with the combination LDV and AMARIS platforms is safe, effective, and it preserves reasonably well the bilateral symmetry of the corneal wavefront aberration between eyes. This may be related to the advantages of profiles aiming to be neutral for HOAs or to the fact that the high-speed AMARIS system reduces variability from stromal hydration effects, which increase with the duration of treatment.39,40 Recognizing the high levels of defocus and astigmatism in this study, analysis of pre- and postoperative binocular vision41 would be of interest and is a partial limitation of this study.42 Further analysis of bilateral symmetry as a function of the analysis diameter is also of interest. Long-term follow-up on these eyes will help determine the stability of these accurate results. Comparing similar outcomes from other lasers to see if any of the parameters we measured are really different for other lasers or microkeratomes and analyses to determine if these parameters are clinically relevant will help to determine the impact of this work.
Cuesta et al.43 found that even differences in corneal asphericity may affect the binocular visual function by diminishing the binocular contrast-sensitivity function. Jiménez et al.11 found that following LASIK, binocular function deteriorates more than monocular function, and that this deterioration increases as the interocular differences in terms of aberrations and corneal shape increase. They also found that interocular differences above 0.4μm of RMS for a 5 mm analysis diameter (0.4 D) lead to a drop in binocular summation of more than 20%.
In our study, only 4 out of 25 patients showed preoperative clinically relevant OS-vs.-OD differences (i.e., larger than 0.25 D), whereas 6 months postoperatively only 2 out of 25 patients showed clinically relevant OS-vs.-OD differences (i.e., larger than 0.25 D).
RMS(ΔHOAb) analysis for interocular differences accounts for the RMS of the differential corneal wavefront aberration and not for the difference of the corneal RMS(HOAb). RMS(ΔHOAb) is a rigorous analysis metric, because it accounts for any deviation (i.e. both inductions and reductions of the wavefront aberration, since both contribute positively to increase the RMS value). Furthermore, it can be mathematically demonstrated that:
Six months postoperatively 3 Zernike terms lost significant OS-vs.-OD correlation symmetry and 4 Zernike terms gained significant correlation symmetry. However, two of them showed borderline correlations. 6 months postoperatively, for 6 Zernike terms the differences in OS-vs.-OD symmetry increased significantly whereas for 4 Zernike terms the differences in symmetry decreased significantly. However, 6 of them showed borderline significances of the difference. Also 6 months postoperatively, 3 patients lost significant OS-vs.-OD correlation symmetry, whereas 1 patient gained significant correlation symmetry. However, two of them showed borderline significances of the difference. All these borderline situations, actually shall be seen as “almost preserved” bilateral symmetry.
Despite large defocus and astigmatism magnitudes, our study shows that HOAs are either minimally increased or unchanged after surgery with the LDV and AMARIS systems (Tables 1 and 2). The main post-op HOAs effects (coma and spherical aberration) are caused by decentration and “edge” effects: i.e., to the strong local curvature change between the OZ and the Transition Zone (TZ) and from the TZ to the non-treated cornea. As a result, it is necessary to emphasize the use of huge OZs, covering the scotopic pupil size plus tolerance for possible decentrations, as well as welldefined TZ. In our study this was approached by the use of a 6.5-mm-diameter fully-corrected ablation zone with a multidynamic aspherical transition zone automatically calculated by the laser depending on the planned refractive correction (6.7mm to 8.9mm diameter).
Although this small series of treated eyes does not allow for definitive conclusions or evidence-based statements, our preliminary results are promising.
Limitations of our study include the moderate number of eyes, limited follow-up and the lack of a control group. The method to determine whether or not symmetry is maintained consist of comparing individual terms in a variety of ad hoc ways both before and after refractive surgery, ignoring the fact that retinal image quality for any given individual is based on the sum of all terms. However, similar methodologies have been already used before.9 At this stage, we did not perform any specific visual tests on binocular vision; for example, stereotests. Some patients may not have good stereopsis but they may show good aberration symmetry. The analysis of bilateral symmetry should be related to the patients’ binocular vision status. Despite these limitations, we were able to demonstrate that “aberration neutral” ablation profiles reasonably preserve the bilateral symmetry between eyes in terms of corneal wavefront aberration. The presented results cannot be extrapolated to patients with symptoms of amblyopia,44 anisometropia, nystagmus, or aniseikonia45 without further studies.
This does not mean any “good or bad” point for binocular vision. Taking into account that we cannot precisely evaluate the role of aberrations monocularly (patients with a high level of aberrations can have an excellent visual acuity and vice versa), it is even more difficult to do it binocularly. The important question in binocular vision is “the role of interocular-differences”, and if they can influence significantly binocular performance. Interocular-differences can be minor but significant for visual performance. Further studies shall help to determine the impact of this on binocular visual performance.
In summary, this study demonstrated that “aberration neutral” profile definitions (as implemented at the SCHWIND AMARIS system), which are not standard in refractive surgery, yield very good visual, optical and refractive results, and reasonably preserve the bilateral symmetry between eyes (which influence binocular summation44) of the corneal wavefront aberration with no clinically relevant induction of HOAs (which influence contrast sensitivity46). In this sense, “Aberration neutral” ablation profiles, as demonstrated here, have therefore the potential to replace current standard algorithms for the non-customised correction of refractive ametropias in laser corneal refractive surgery.
Financial disclosure: Authors Arbelaez and Vidal have no proprietary interest in the materials presented herein