Practising optometrists and vision researchers often rely on the patient's recollection of past optometric events to compile a refractive history. The work reported here attempted to evaluate the reliability of such an approach in a clinical population by comparing self-report of previous spectacle prescription change against actual recorded refractive details.
MethodsA documented healthy clinical population with mildmoderate myopia habitually corrected by spectacles was invited to complete a short tick-box questionnaire. Subjective recall of spectacle prescription changes over the past five years was investigated. Subsequently, these recollections were compared against individual recorded optometric histories.
Results155 persons (42% of those canvassed: mean age 36.2± 9.1 years) responded to the invitation to complete the questionnaire. The subjective estimate of the interval since the most recent sight test was accurate (P=0.7). However the question “Has your distance glasses prescription been changed over the past five years?” had a sensitivity of 0.67/specificity of 0.64, and a positive predictive value (PV) of 0.43/negative PV of 0.82. With a calculated value of K= 0.25, the strength of the agreement between subjective recall and the actual record could at best only be regarded as “Fair”.
ConclusionsThe accuracy of subjective recollection as an indication of refractive change over an immediately-preceding time interval of several years must be treated with caution. Whether questioning patients in the optometric practice or establishing the background of participants in a clinical vision research project, there is no substitute for reference to a contemporary record detailing refractive history.
Los optometristas en ejercicio y los investigadores en visión a menudo se basan en aquello que recuerdan sus pacientes a la hora de elaborar el historial optométrico de los mismos. El trabajo que aquí se presenta trata de evaluar la fiabilidad de este enfoque en una población de pacientes; para ello, compara los cambios en la graduación de las gafas, tal y como los recuerda el paciente, con los datos de refracción reales, extraídos de la historia clínica.
MétodosA una población sana y bien documentada de pacientes con miopía leve o moderada, corregida habitualmente mediante gafas, se le invitó a responder a un breve cuestionario (donde simplemente había que marcar las casillas apropiadas). Se les preguntó por su recuerdo (subjetivo) sobre los cambios de graduación de las gafas producidos durante los 5 años anteriores. A continuación, se comparó esta información con los datos individuales de cada paciente, extraídos de su correspondiente historia clínica.
Resultados155 personas (42% del total de personas preseleccionadas: edad media 36,2±9,1 años) respondieron a la invitación recibida para responder al cuestionario. La estimación subjetiva del tiempo transcurrido desde la última revisión de la vista fue precisa (P=0,7). Sin embargo, la pregunta “¿Ha cambiado la graduación de sus gafas para ver de lejos a lo largo de los últimos 5 años?” presentó una sensibilidad de 0,67, una especificidad de 0,64, un valor predictivo (VP) positivo de 0,43 y un VP negativo de 0,82. Con un valor calculado de K=0,25, el grado de acuerdo entre la memoria subjetiva y los datos reales de la historia clínica se puede considerar, como mucho, como “Aceptable”.
ConclusionesHay que ser cautos a la hora de evaluar la exactitud del recuerdo subjetivo sobre los cambios en la refracción que se han producido a lo largo de un periodo de varios años inmediatamente anterior. Tanto si se está interrogando a los pacientes en la consulta del optometrista como si se están estableciendo los antecedentes personales de los participantes en un proyecto de investigación clínica sobre visión: no existe ningún sustituto válido que pueda eliminar la necesidad de consultar los datos históricos de refracción incluidos en la historia actualizada del paciente.
During the initial stages of a sight test, especially when the patient is attending the practice for the first time, the optometrist relies substantially upon patient recall elicited by careful questioning to compile a relevant personal ophthalmic optical history.1 But as many practitioners are undoubtedly aware, this verbal questioning can produce what, as both parties acknowledge, is often a partial or imprecise record of prior events. This uncertainty can extend to the refractive history, even if previous spectacles are available for inspection. Without reference to a written record of actions with dates, a certain degree of guesswork on the part of the patient is inevitably involved when it comes to determining specifics such as a chronology of optical prescription issue and change.
A similar reliance upon subjects’ recollections of their refractive history has often been necessary to provide context or background for several vision-related investigations. Such studies have frequently been concerned with establishing a myopic refractive history, with the investigators tacitly relying upon the disruption or inconvenience caused by the (distance) visual blur, and its amelioration by an appropriate refractive correction, to provide key ‘life events’ that the patient will subsequently recall when questioned.2 A nonexhaustive listing of those aspects investigated using this subjective-recall approach over the past two decades includes: socio-historical prevalence of refractive correction;3 influence of a family history of refractive error,4,5 or parental use of spectacles;6 age of onset as regards regular spectacle use;7 also the refractive influence of pathology in older persons (i.e., cataracts).8 In addition, there has been consideration of myopia progression in adult contact lens wearers,9 and the potential influence upon refractive change of specific occupations including microscopy,10,11 and office work;12,13 and also the possible long-term effects of intense periods of college study (i.e., in law students).14
Given the breadth of the foregoing topic range and (so far as one could judge) the fact that in all cases the questionnaire- elicited responses were accepted without corroboration against any contemporary clinical records, it seems reasonable to enquire just how accurate subjective recollection in this area might be. This issue is relevant to clinicians and researchers alike whenever they are relying upon self-reported changes of refractive error as a surrogate record of refractive history and, in particular as a proxy measure for myopia progression. The purpose of this study was to evaluate the degree of fallibility of optometric patients recall of spectacle prescription changes over the preceding 5 years: responses elicited by a printed questionnaire regarding an individual's refractive history were compared to the details of that individual's optometric examinations held on contemporary clinical records.
MethodsSubjectsAll data were collected following informed verbal consent and were entirely analysed without any link to personal information, preserving patient confidentiality.
The patients’ records at the author's independent optometric practice were surveyed in Spring 2008 to identify cases with a specific profile: namely, teenage and adult myopic persons aged 16-45 with normal binocular vision correctable to at least 6/6 Snellen (≤0.00 logMAR) who had attended for two or more sight tests over the preceding 5 years (60 months).
Myopic cases were specifically chosen on the grounds that instances of subjective awareness of blurred or unsatisfactory distance vision would likely have prompted such individuals to attend for a sight test, potentially providing a memorable event that the patient would recall if subsequently questioned about their refractive history (a scenario corroborated by Fledelius).2 A five-year period was chosen as being a reasonable time interval for interrogation of subjective recall: it was also the investigative interval quoted in at least two of the studies previously referred to.10,14 The stipulation of a minimum of two sight tests per patient over this period was to facilitate the assessment of inter-record comparative detail over the intervening years.
The screening of the practice's current patients’ records produced 370 suitable candidates. In summary, within the review window all cases were non-presbyopic habitual myopic spectacle (not contact lens) wearers. The right eye was arbitrarily chosen for investigation. All patients had a maximum myopic refractive error in this eye of -6.00 diopters (D) of sphere and of -2.00 D of cylinder, and attained a monocular visual acuity (VA) of at least 6/6 Snellen. All subjects were recorded as being in consistently good general health, with no adverse ocular history. Physical testing conditions in the consulting room had remained unchanged over the investigative time-span and all sight tests had been conducted by the author.
Inter-test myopic refractive progression was defined as a change in the spherical equivalent refraction (SE) of the right eye of 0.38 D or more, always towards more negative (myopic) values. This was the significant refractive interval adopted by Adams & McBrien.10 Loman et al.14 opted for -0.50 D or more, and larger changes have been specified in other studies (i.e., -1.00 D or greater over five years in an adult contact-lens population).9 In a clinical setting where a patient visits a single practitioner for repeat refractions (a situation where examiner-based test variability can be assumed to be low) and where previous prescription details are readily available for reference at each successive examination (i.e., the situation that pertained to the present work), a SE-based prescription change of -0.38 D or greater might be regarded as clinically significant.15
ProceduresOn a single day a personalised letter was mailed to each of the 370 patients that had previously been preselected, inviting them to attend the practice at their convenience for a brief interview and assessment of their current VA. No incentives were offered.
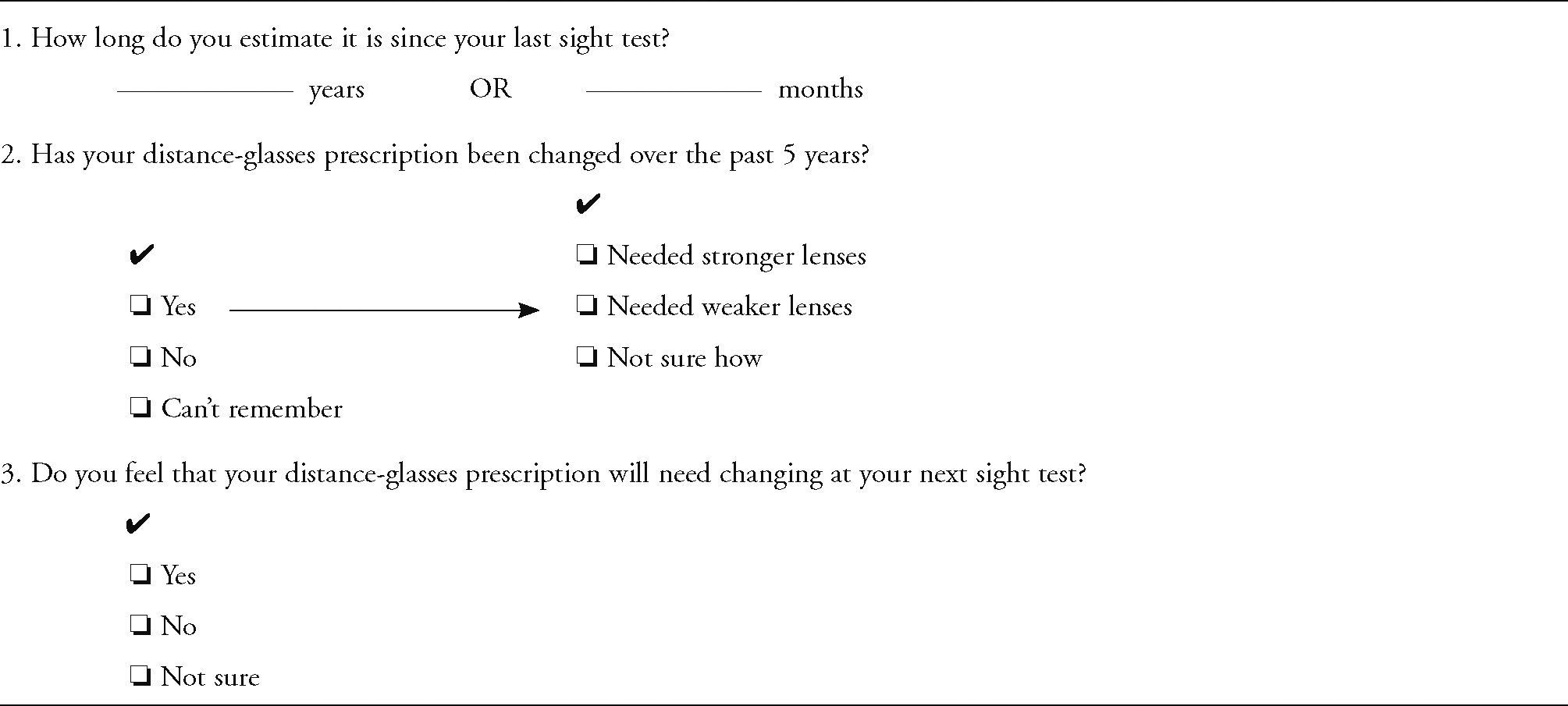
At the interview the patient was requested to mark his/her responses to a set of questions on a printed sheet: only the responses to the first 3 items on the questionnaire will be analysed in the present report (Appendix I). The combined procedures (including the recording of monocular and binocular VA at 6m with their current spectacles) detained the patient for only a few minutes and were all undertaken under photopic conditions in the practice's main consulting room, at all times under the author's direction. No feedback was given, and the subjects were thanked but not remunerated for their attendance.
A period of 8 weeks was allocated to data collection. Only after this time had elapsed were the participating patients’ responses collated and entered into a spreadsheet. The data were subsequently analysed and compared with the relevant data of their refractive history as obtained from their clinical record cards held at the practice.
Statistical AnalysisData management and statistical analyses were undertaken using STATISTICA/Mac software (v4.1: StatSoft, Inc., Tulsa, OK, USA). All data were entered into a spreadsheet and each variable was assessed in turn for normality of distribution using frequency-distribution histograms and the Kolmogorov-Smirnov test. In those cases where a Gaussian distribution was demonstrated, parametric analytical procedures were employed (including t-testing for independent or correlated samples, as appropriate). Testing of non-Gaussian data utilised distribution-free alternatives; these included the Mann-Whitney U test (for independent samples), and either the Kruskal-Wallis test (between groups) or Friedman's analysis (repeated measures) for multiple comparisons. The level of statistical significance was set at P<0.05. In the text and tables, data are summarised in terms of the mean and the standard deviation (SD); the 95% confidence interval (CI = ±1.96 SD) is also quoted where appropriate.
ResultsOut of the 370 patients that were initially canvassed, a total of 155 (42%) individuals responded. The majority of the respondents (66%) attended within the first 2 weeks of the mail-shot; the remainder called over the following 3.5 weeks, with no further responses received beyond that point; i.e., the allocation of an 8 week response period proved adequate.
Practice records indicated that at the point of administration of the questionnaire the mean age of the respondents was 36.2 years (SD 9.1). On average, males (n=55: 35%) were aged 37.7 years (SD 8.5), and females (n=100: 65%) were aged 35.4 years (SD 9.4): the gender-based age distributions were not significantly different in statistical terms (t-test, independent samples: P=0.14).
Further preliminary reference to the record cards indicated that, as a group, these 155 patients had undergone a total of exactly 400 sight tests over the review period: this amounts to a mean of 2.6 tests per patient (SD 0.8), with no difference between genders (t-test, independent samples: P=0.68).
There was no difference in terms of gender in the patient responses to the second question of the questionnaire, as to whether their spectacle prescription had changed over the past five years (Mann-Whitney U test, independent samples: P=0.10); also, where subjects indicated that they believed that it had, there was no difference in terms of gender in the stated direction of this change (Mann-Whitney U test, independent samples: P=0.16). Consequently, unless indicated otherwise in the text, the data will be grouped across genders (maximum n=155) in the following summary and in subsequent comparative analysis of the questionnaire responses and associated material.
Question 1. How Long Do You Estimate It Is Since Your Last Sight Test?The subjects’ mean estimate of the time elapsed since their last (i.e., most recent) sight test was 1.11 years (SD= 0.68). The actual mean interval, as calculated from the clinical records, was 1.09 years (SD=0.61): apparently, the subjective estimation was highly accurate on this point (t-test, dependent samples: P=0.67). Analysis of the paired time intervals revealed a close correlation (Pearson r=0.69), with a coefficient of determination (r2) of 48% (P=0.0001).
Question 2. Has Your Distance-Glasses Prescription Been Changed Over the Past 5 Years?All of the subjects were able to answer this question without equivocation: 70 (45%) believed that their distancespectacle prescription had been changed over the previous five years and 85 (55%) felt that it had not. Of the former, the majority (79%) indicated that it was their recollection that they had needed stronger lenses, only 7% felt that a reduced-power prescription was given, and 14% were not sure of their prescription change.
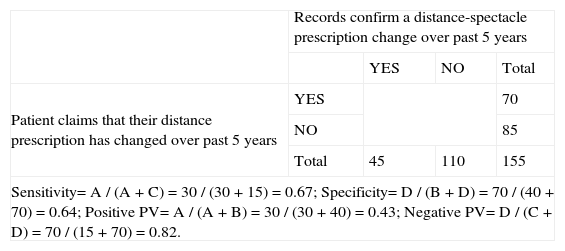
Setting these subjective recollections against the actual clinical records in a 2×2 (true/false × positive/negative) contingency table (Table 1) indicated that the question “Has your distance-glasses prescription been changed over the past 5 years?” had a sensitivity of 66.7% and a specificity of 63.6%. This outcome will be considered further below, in the Discussion.
Subjective recollection vs clinical record in response to the question: “Has your distance-glasses prescription been changed over the past five years?” (n=155)
| Records confirm a distance-spectacle prescription change over past 5 years | ||||
| YES | NO | Total | ||
| Patient claims that their distance prescription has changed over past 5 years | YES | 70 | ||
| NO | 85 | |||
| Total | 45 | 110 | 155 | |
| Sensitivity= A / (A + C) = 30 / (30 + 15) = 0.67; Specificity= D / (B + D) = 70 / (40 + 70) = 0.64; Positive PV= A / (A + B) = 30 / (30 + 40) = 0.43; Negative PV= D / (C + D) = 70 / (15 + 70) = 0.82. | ||||
The majority (64.5%) of persons felt that their distancespectacle prescription would not need changing at their next sight test. Although 29% of the subjects were unsure, less than 7% felt that a change would be necessary.
The last item that was checked at the voluntary patient visit was distance acuity with the current spectacle prescription: the mean result for the right eye of the subject group was -0.031 logMAR (SD=0.093), equivalent to 6/5.6 Snellen.
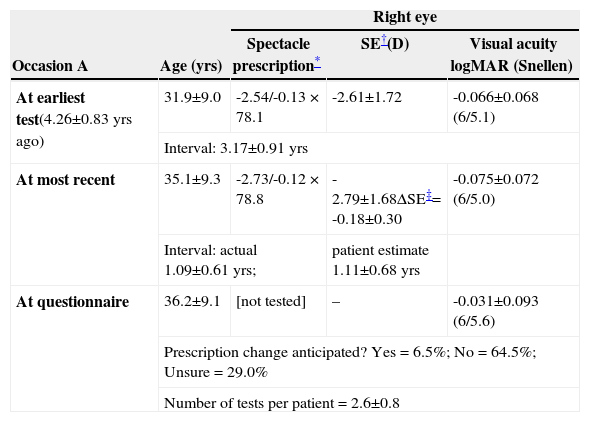
The clinical records for each of the 155 participants in the voluntary survey were accessed to obtain details of their relevant optometric histories. Table 2 (upper section) summarises this material, alongside the results from the questionnaire (lower section).
Summary of patients’ optometric details (grouped data, n=155: mean ± SD) as sourced from clinical records and from the responses to the questionnaire
| Occasion A | Age (yrs) | Right eye | ||
| Spectacle prescription* | SE†(D) | Visual acuity logMAR (Snellen) | ||
| At earliest test(4.26±0.83 yrs ago) | 31.9±9.0 | -2.54/-0.13 × 78.1 | -2.61±1.72 | -0.066±0.068 (6/5.1) |
| Interval: 3.17±0.91 yrs | ||||
| At most recent | 35.1±9.3 | -2.73/-0.12 × 78.8 | -2.79±1.68ΔSE‡= -0.18±0.30 | -0.075±0.072 (6/5.0) |
| Interval: actual 1.09±0.61 yrs; | patient estimate 1.11±0.68 yrs | |||
| At questionnaire | 36.2±9.1 | [not tested] | – | -0.031±0.093 (6/5.6) |
| Prescription change anticipated? Yes = 6.5%; No = 64.5%; Unsure = 29.0% | ||||
| Number of tests per patient = 2.6±0.8 | ||||
Across the <5 year inter-test period it was only the spherical element of the mean spectacle prescription that underwent a change, i.e., an increase of approximately -0.20 D of sphere towards more negative values. The cylindrical component (power and axis) remained little altered. Consequently, the SE will serve as an indicator of chronological prescription change in these data.
Mean visual acuity (spectacle-corrected right monocular) was similar at the time of each of the two tests, and superior to the level recorded at the questionnaire visit. At the latter, the patient's current spectacles were used for the acuity determination: as noted by Pointer16 this approach represents determination of ‘habitual’ acuity, as compared to a (superior) ‘optimal’ level, probably recorded with a recently-determined refractive correction (i.e., immediately subsequent to a sight test).
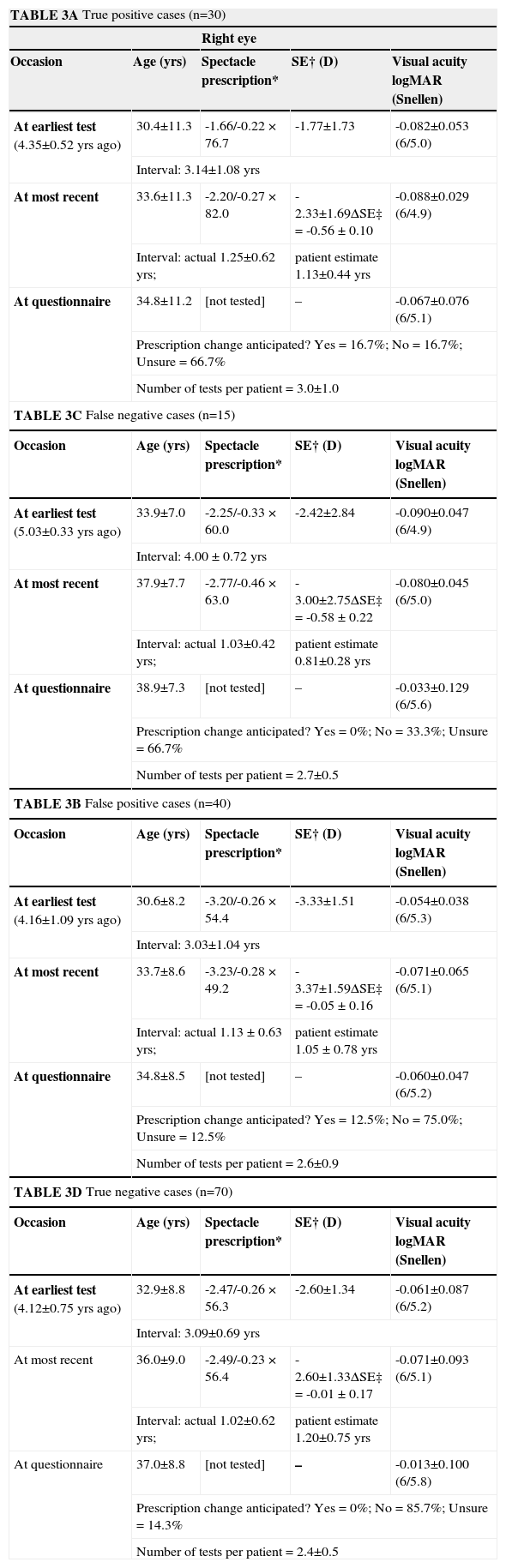
Tables 3A-D present a breakdown of the group results given in table 2, quartered as per the frequency distribution of table 1, i.e., on the basis of patient recollection [rows] versus the clinical record [columns].
| TABLE 3A True positive cases (n=30) | ||||
| Right eye | ||||
| Occasion | Age (yrs) | Spectacle prescription* | SE† (D) | Visual acuity logMAR (Snellen) |
| At earliest test (4.35±0.52 yrs ago) | 30.4±11.3 | -1.66/-0.22 × 76.7 | -1.77±1.73 | -0.082±0.053 (6/5.0) |
| Interval: 3.14±1.08 yrs | ||||
| At most recent | 33.6±11.3 | -2.20/-0.27 × 82.0 | -2.33±1.69ΔSE‡ = -0.56 ± 0.10 | -0.088±0.029 (6/4.9) |
| Interval: actual 1.25±0.62 yrs; | patient estimate 1.13±0.44 yrs | |||
| At questionnaire | 34.8±11.2 | [not tested] | – | -0.067±0.076 (6/5.1) |
| Prescription change anticipated? Yes = 16.7%; No = 16.7%; Unsure = 66.7% | ||||
| Number of tests per patient = 3.0±1.0 | ||||
| TABLE 3C False negative cases (n=15) | ||||
| Occasion | Age (yrs) | Spectacle prescription* | SE† (D) | Visual acuity logMAR (Snellen) |
| At earliest test (5.03±0.33 yrs ago) | 33.9±7.0 | -2.25/-0.33 × 60.0 | -2.42±2.84 | -0.090±0.047 (6/4.9) |
| Interval: 4.00 ± 0.72 yrs | ||||
| At most recent | 37.9±7.7 | -2.77/-0.46 × 63.0 | -3.00±2.75ΔSE‡ = -0.58 ± 0.22 | -0.080±0.045 (6/5.0) |
| Interval: actual 1.03±0.42 yrs; | patient estimate 0.81±0.28 yrs | |||
| At questionnaire | 38.9±7.3 | [not tested] | – | -0.033±0.129 (6/5.6) |
| Prescription change anticipated? Yes = 0%; No = 33.3%; Unsure = 66.7% | ||||
| Number of tests per patient = 2.7±0.5 | ||||
| TABLE 3B False positive cases (n=40) | ||||
| Occasion | Age (yrs) | Spectacle prescription* | SE† (D) | Visual acuity logMAR (Snellen) |
| At earliest test (4.16±1.09 yrs ago) | 30.6±8.2 | -3.20/-0.26 × 54.4 | -3.33±1.51 | -0.054±0.038 (6/5.3) |
| Interval: 3.03±1.04 yrs | ||||
| At most recent | 33.7±8.6 | -3.23/-0.28 × 49.2 | -3.37±1.59ΔSE‡ = -0.05 ± 0.16 | -0.071±0.065 (6/5.1) |
| Interval: actual 1.13 ± 0.63 yrs; | patient estimate 1.05 ± 0.78 yrs | |||
| At questionnaire | 34.8±8.5 | [not tested] | – | -0.060±0.047 (6/5.2) |
| Prescription change anticipated? Yes = 12.5%; No = 75.0%; Unsure = 12.5% | ||||
| Number of tests per patient = 2.6±0.9 | ||||
| TABLE 3D True negative cases (n=70) | ||||
| Occasion | Age (yrs) | Spectacle prescription* | SE† (D) | Visual acuity logMAR (Snellen) |
| At earliest test (4.12±0.75 yrs ago) | 32.9±8.8 | -2.47/-0.26 × 56.3 | -2.60±1.34 | -0.061±0.087 (6/5.2) |
| Interval: 3.09±0.69 yrs | ||||
| At most recent | 36.0±9.0 | -2.49/-0.23 × 56.4 | -2.60±1.33ΔSE‡ = -0.01 ± 0.17 | -0.071±0.093 (6/5.1) |
| Interval: actual 1.02±0.62 yrs; | patient estimate 1.20±0.75 yrs | |||
| At questionnaire | 37.0±8.8 | [not tested] | – | -0.013±0.100 (6/5.8) |
| Prescription change anticipated? Yes = 0%; No = 85.7%; Unsure = 14.3% | ||||
| Number of tests per patient = 2.4±0.5 | ||||
Out of the following variables: patient age, number of sight tests per patient, inter-test and test-to-questionnaire time intervals, and SE at both test occasions, none of them were significantly different in statistical terms (Kruskal-Wallis test: P≥0.08) when the respective values were compared across the four subject subgroups summarised in tables 3A-D. In addition, optimal logMAR acuity was not statistically different between the four groups neither at the earliest recorded sight test more than 4 years ago (Kruskal-Wallis test: P=0.3) nor at the most recent test, approximately 1 year ago (Kruskal-Wallis test: P=0.8). The habitual VA level, however, as measured at the administration of the questionnaire, was more variable (Kruskal-Wallis test: P=0.001) across the four subject subgroups. Indeed, a pattern was apparent in these latter results: patients in those groups who had indicated that they believed their spectacle prescription had been changed over the past five years (Table 3A and 3B) recorded a VA at time of questionnaire similar to their optimal (i.e., sight test) acuity levels (Friedman's analysis: P>0.2); by contrast, those subjects who believed that there had been no prescription change (Table 3C and 3D) registered a similar (values in table 3C versus 3D; Friedman's analysis: P=0.1) but, compared to their optimal VA levels (and to the questionnaire VA of the other subjects), lower acuity (Friedman's analysis or Kruskal-Wallis test, as appropriate: P<0.01) at the time of the questionnaire.
A second significant result is evident in this tabulation if subgroups are compared left vs right (refer to the layout of table 1); i.e., if those cases where the clinical records confirmed the subjective recollection regarding prescription change (Table 3A and 3C) are compared with those where the clinical records disagreed with the patient's recollection (Table 3B and 3D). As anticipated, ΔSE (“most recent” minus “earliest” sight test SE) was > -0.50D in the former cases and ≤ -0.05 D in the latter (a statistically significant difference, according to the Kruskal-Wallis test: P=0.0001). But allied to this factual result is the pattern of the subjects’ responses to Question 3 (see Appendix I) regarding the possibility of future spectacle prescription change: 67% of subjects with a confirmed previous prescription change indicated that they felt equivocal about their future prescription stability and were not unprepared for future spectacle change. In contrast ≥75% of the confirmed “no change” subjects indicated that they believed their present spectacle prescription would still not need any revision at their next test.
Putting these two outcomes together it appears that those individuals who believed that their distance spectacle prescription had been changed within the 5 years preceding the administration of the questionnaire maintained a consistently good visual acuity level; in those cases where clinical records confirmed their assertion (Table 3A: true positive) 67% of patients appeared to acknowledge the possibility that further change could not be ruled out, in marked contrast to those subjects where there had been no prescription change (Table 3B: false positive) and where a similarly high proportion of cases (75%) asserted that no imminent change was anticipated. Alternatively, where patients correctly claimed that their prescription had not been changed (Table 3D: true negative) and overwhelmingly indicated (86%) that they believed no spectacle revision would be necessary, a reduced acuity at questionnaire was recorded; where a spectacle prescription change had taken place which the patient had failed to recall (Table 3C: false negative) it is possible that the reduced acuity demonstrated at the time the questionnaire was completed might have lead these patients to their “not been changed” assertion and similarly their equivocation in two-thirds of the cases as regards future prescription change.
In summary, this descriptive analysis inclines one to support the intuitive belief that the degree of coincidence between patient assertion and recorded fact will be a reflection of the interplay of the individual's memory of events influenced by (recent) experience. But the core question for discussion remains: how much faith might the clinician or vision researcher put in the patient's recollection of his/her optometric (or, specifically, refractive) history? Might a ‘global index’ be computed to simplify this issue?
DiscussionThe distribution of subjective versus objective data in table 1 enables a quantitative determination of the agreement between patient recollection and the clinical record to be attempted. Prima facie total agreement is present in 30 (true positive) plus 70 (true negative) cases, i.e., 100/155 or 64% instances. However, it must be acknowledged that a proportion of the agreement will occur by chance: the expected agreement for the “Yes” category (refer to Table 1) is (45 × 70)/155 or 20.32, and for “No” is (110 × 85)/155 or 60.32. Thus, the summed chance agreement is 80.64; given as a proportion of the total number of cases (155) this corresponds to a value of 0.52. Maximum agreement would be 1.00 (and no agreement better than chance would be zero), so the calculated agreement better than chance, K (kappa) = (0.64 – 0.52)/(1.00 – 0.52) = 0.25. A ‘chance-corrected proportional agreement’17 of this strength could be interpreted as “Fair” according to Landis and Koch18 although, with a calculated 95% CI of 0.17 to 0.33, in reality “Poor” might be a more pragmatic conclusion.
This investigation was undertaken to assess the accuracy of subjective recollection of clinical changes as a proxy for refractive history. Column-based calculations from table 1 derive values for sensitivity of 0.67 (95% CI 0.53 to 0.81) and specificity of 0.64 (0.55 to 0.73). Thus, based on the results of the optometric population surveyed here, 67% of the patients who claimed that their spectacle prescription has changed over the preceding five years actually have recorded a prescription change, and 64% of those who stated that there had been no change were correct in their recollection.
An alternative row-based analysis of table 1 allows to derive predictive values (PV): thus, the proportion of patients with an actual change who asserted this (the positive PV) is 0.43, and that proportion of patients where no change occurred who stated this (the negative PV) is 0.82.
However the predictive cross-table analysis in particular must take into account the prevalence of claimed prescription change, which in this population is 70/155 or 0.45 (95% CI 0.37 to 0.53). The question as to how reliable subjective recollection should be to become an acceptable substitute for the actual clinical record must acknowledge the prevalence of claimed prescription change in the study population. As the interpretation of the calculated value of K has suggested above, the surrogacy of subjective recollection for clinical fact appears to be weak.
A final perspective is gained if we regard our investigation as akin to a screening of young adult myopic patients with a refractive change ≥ -0.38 D SE over the preceding five years. It should be evident that high specificity and a high negative PV are desirable: false negative results should be avoided and false positives should be minimal. Perusal of the relative numbers in the cells of the 2 × 2 frequency table 1 suggests that these data really do not match this ideal.
ConclusionsThese results apparently confirm, possibly for the first time specifically within the literature relating to optometric practice, what many practitioners anecdotally believe: namely, that patients frequently have unreliable recollection of their individual (recent) refractive history. Consequently, whether questioning patients in optometric practice or establishing the background of participants in a clinical vision research project, there is no substitute for reference to a contemporary record detailing refractive history.
On the basis of this preliminary result, generated by an intentionally short and direct series of questions, a possible future study might be expanded to encompass a more detailed sampling of subjects, and also to address a broader or alternative range of refractive groups. A questionnaire-based approach might be supplemented or replaced by a structured interview, whereby subjective aspects including self-awareness and health beliefs could be explored in tandem with attitudes to personal eye care. Many factors, including emotional, intellectual and economic ones, are likely to affect recall of previous decisions and events; eliciting and delineating these issues would greatly enhance the grading and interpretation of subjective responses at the point of comparison with the cognitive objective record(s) available in each case.