To determine the significance of changes and and inter-relationships between three markers of binocular function (aniseikonia, distance and near stereoacuity) following unremarkable LASIK at 3 and 6 months postoperatively.
MethodsAll patients underwent LASIK using the Schwind Amaris 750S and the flaps were created using Intralase 150 kHz. Patients were I, monocular myopes II, binocular myopes III, binocular hyperopes IV, binocular astigmats V, anisometropes and VI, matched age and gender control (n = 20 in each group except III where n = 18). Aniseikonia (Awaya test), distance and near stereoacuity (Randot tests) were measured before surgery, and at 3 and 6 months after surgery. At all times data were collected under constant conditions and analyzed using appropriate non-parametric statistical tests.
ResultsThe following statistically significant changes were found after applying the Bonferroni correction (p ≤ 0.001); aniseikonia reduced (groups I, III, IV, V), stereoacuity improved at distance (groups I, III-V) and near (groups I, V). Inter-group differences in aniseikonia distance and near stereoacuity were significant preoperatively, but not postoperatively. In groups I, IV and V, the changes in aniseikonia and stereoacuity (near and distance) were significantly correlated with the preoperative value. Aniseikonia was significantly correlated with distance and near stereoacuity preoperatively but not postoperatively.
ConclusionBinocular function improved in all groups after LASIK except in binocular myopes. In general, binocular function was still low compared with the control group at six months postoperatively. It is unclear why binocular function improved in the binocular astigmats.
Determinar la significancia de cualquier cambio, así como las interrelaciones entre tres marcadores de la función binocular (aniseiconía, estereoagudeza de lejos y de cerca) tras LASIK sin complicaciones a los 3 y 6 meses postoperatorios.
MétodosA todos los pacientes se les realizó cirugía LASIK con el laser Schwind Amaris 750S, creándose los flaps con Intralase 150 kHz. Los grupos de pacientes fueron: I miopes monoculares, II miopes binoculares, III hipermétropes binoculares, IV astígmatas binoculares, V anisométropes y VI controles equivalentes en edad y género (n = 20 en cada grupo, exceptuando III donde n = 18). Se midió la aniseiconía (prueba de Awaya), la estereoagudeza de lejos y de cerca (pruebas Randot) durante el preoperatorio, y a los 3 y 6 meses posteriores a la cirugía. En todo momento se recabaron los datos en condiciones constantes, analizándose los mismos con pruebas estadísticas no paramétricas adecuadas.
ResultadosSe encontraron los siguientes cambios estadísticamente significativos tras aplicar la corrección de Bonferroni (p ≤ 0,001); se redujo la aniseiconía (grupos I, III, IV, V), y mejoró la estereoagudeza de lejos (grupos I, III-V) y de cerca (grupos I, V). Las diferencias inter-grupo en cuanto a aniseiconía de lejos y de cerca y la estereoagudeza de cerca fueron significativas en el preoperatorio, pero no en el postoperatorio. En los grupos I, IV y V, los cambios en cuanto a aniseiconía y estereoagudeza (de cerca y de lejos) guardaron una correlación significativa con el valor preoperatorio. La aniseiconía guardó una correlación significativa con la estereoagudeza de lejos y de cerca en el preoperatorio, pero no el postoperatorio.
ConclusiónLa función binocular mejoró en todos los grupos tras la cirugía LASIK, excepto en la miopía binocular. En general, la función binocular fue aún baja al compararse con el grupo control a los seis meses postoperatorios. No queda claro por qué la función binocular mejoró en el astigmatismo binocular.
All refractive procedures have the potential to affect stereoacuity. It is generally accepted that improved stereoacuity after corneal refractive procedures results from correction of any pre-existing anisometropia and reduction of any associated aniseikonia.1,2–9 A significant correlation between the stereoacuity detected at the post-operative (postop) stage and the pre-operative (preop) anisometropia has been reported in relation to LASIK.8 This was, to some extent, not an unexpected finding because inter-ocular differences in axial length remain unchanged after binocular correction of any refractive error. However, there is a paucity of clinical information regarding any change in aniseikonia after LASIK. Aniseikonia, is defined as ‘that condition in which the ocular images are unequal in size and/or shape’.10 Thus, aniseikonia is an inter-ocular difference in the perception of size. This should be eliminated after LASIK when anisometropia is purely refractive, but not when the anisometropia results from differences in axial length. Therefore, as astigmatism is purely refractive, any aniseikonia is expected to reduce, and stereoacuity to improve after any corrective corneal refractive procedure. However, astigmatism is rarely mentioned in previous studies based on LASIK.1,2–9 We are not aware of any previous reports on the effects of LASIK correction of astigmatism on aniseikonia. It would be useful to gain a better understanding of how the correction of astigmatism by LASIK affects clinical measures of aniseikonia and stereoacuity.
The value of any geometric calculations of aniseikonia following refractive surgery are limited by the differences between the eyes of an individual in the distribution of appropriate sensory elements and other neuro-physiological factors. Such factors have been cited as the likely causes for the poor correlation between anisometropia and measured aniseikonia following routine cataract surgery.11–13 Following cataract surgery, stereoacuity declines when aniseikonia exceeds 6%.14,15 A standard ‘rule of thumb’ predicts 6% of aniseikonia should occur when the refractive anisometropia is between 3.00D and 4.00D.16 Stereoacuity tends to improve after LASIK especially when the preoperative anisometropia exceeds 2.50D.17 This points to 1.50D range of uncertainty regarding the minimum level of anisometropia, hence aniseikonia, that is linked with reduced stereoacuity. Other than stereoacuity, LASIK emmetropization of both eyes can also impact on binocular contrast sensitivity function. Inter-ocular differences of corneal shape, higher order aberrations and quality of the retinal images are associated with a deterioration in binocular contrast sensitivity function.18–23 The binocular contrast sensitivity function diminishes when aniseikonia exceeds 5%19 and the upper disparity limit of stereoacuity declines after binocular LASIK.24 This decline is coupled with a rise in the postoperative inter-ocular differences of corneal shape, preoperative anisometria and higher order aberrations. These factors may limit postoperative stereoacuity when the LASIK treatment is applied to both eyes in anisometropic cases. Previous studies rarely included comparisons with control groups. The aim of this clinical investigation was to assess the changes in measured aniseikonia and stereoacuity (at both distance and near) and assess how any relationship between aniseikonia and stereoacuity was affected by LASIK over a broad range of refractive errors.
Materials and methodsStudy designThis was a prospective, consecutive, nonrandomized, partially masked, observational study conducted at University Eye Hospital Svjetlost, Zagreb, Croatia. The study was approved by the Ethics Committee of the Hospital. The tenets of the Helsinki agreement were followed throughout. All patients signed informed consent form in which surgery and other options of treatment were thoroughly explained. All patients gave permissions to use their anonymized data. LASIK was performed on both eyes of patients except for those cases that were designated in group I or VI (see below).
Patient allocationAll patients underwent a complete preoperative ophthalmological examination prior to deciding if they met the criteria for surgery. Patients with stable refractive errors, myopia up to -9.25D, hyperopia up to +5.50D and astigmatism up to -4.25D were included. Ocular criteria were those normally adopted in refractive surgery.25 Patients with history of ocular surgery, abnormal corneal topography, preoperative corneal thickness <490 µm or calculated residual stromal bed thickness <280 µm and those with any signs of amblyopia or strabismus were excluded from the study. Age range was 19 to 59 years. All patients were treated for either myopia or myopic astigmatism, hyperopia or hyperopic astigmatism.
Preoperative assessmentPreoperative examination included uncorrected distance visual acuity (UDVA), best corrected distance visual acuity (BCDVA), manifest and cycloplegic refraction (Tropicamide 1%), corneal topography, slit lamp and dilated funduscopic examination. Visual acuity was measured using a standard Snellen acuity chart at 6 m and recorded in decimal format.
All patients underwent binocular examination consisting of alternating cover test with best spectacle correction at near and distance (back vertex distance fixed at 12 mm) for detection of phorias, accommodation (push up test), and vertical and horizontal fusional reserves. Near stereoacuity was measured at 40 cm using the Randot Stereotest (Precision Vision, Woodstock, USA) using the graded circle test ranging from 400 to 20 s of arc in steps of 20 s. Distance stereoacuity was measured at 6 m using a Randot Stereotest (CSO, Visio Chart CVC03 v2.0.0, Firenze, Italy) with a range from 640 to 20 s of arc in steps of 20 s. The Randot test consists of stereograms where a disparity between binocularly viewed targets is made possible by a polarizing vectographic technique. The patient, wearing the appropriate cross-polarizing glasses, was asked to identify which target in a set stood out as either closer, or further away, from the rest. The test was stopped when the patient made two consecutive mistakes. The stereoacuity value recorded was the setting where the patient correctly identified the target, whether it was closer or further away, just before the consecutive mistakes. Aniseikonia was measured using the 6 m Awaya aniseikonia test, that required the use of red–green glasses.26 The patient views two vertically orientated semi-circles (red and green) of different sizes and asked to match both until they appear to be of identical size. The different sizes change in steps of 1%, thus the limiting resolution of this test is 1%. The value of aniseikonia was the size of the image viewed by the left eye as a percentage (larger or smaller) compared with the size of the image viewed by the right eye. At all times, stereoacuity and aniseikonia were measured with the best spectacle correction.
The patients were asked to discontinue contact lens wear for up to four weeks, depending on the type of contact lenses, prior to the examination. Best corrected visual acuity of all patients before surgery was 1.0 or better.
Surgical procedure and postoperative carePrior to the surgery, 2 drops of topical anesthetic (Novesin, OmniVision GmbH, Puchheim, Germany) were instilled at two-minute intervals and eye was cleaned with 2.5% povidone iodine. A corneal flap was cut using Intralase 150 kHz femtosecond laser (Abbot Medical Optics, Santa Ana, California, USA) with predetermined flap thickness of 100 µm. Schwind Amaris 750S (Schwind Eye-Tech-Solutions, Kleinostheim, Germany) was used for the excimer laser treatment. Mean optical zone of the treatment was 6.68 ± 0.20 mm (range 6.5–7.0 mm). The rationale for changing optical zone was based on the manufacturer’s recommendation to select, at least, a 6.7-mm optical zone for treatment of astigmatism and hypermetropia. However, we did not want to exceed 9.0 mm zone of total ablation. Since the transition zone (automatically calculated by the system for the selected optical zone and applied correction) increases with the complexity of the applied correction, size of an optical zone was chosen to fit within the limits of 9.0 mm of total ablation zone. Total ablation zone was 8.67 ± 0.31 mm (range 7.9–9.0 mm). The Aberation Free™ program was applied in all cases. All ablations were centered on corneal vertex calculated by using the videokeratoscope (CSO, Costruzione Strumenti Oftalmici, Florence, Italy). For all patients, the programmed treatment consisted of cycloplegic spherical correction with manifest astigmatic power (and axis) without any nomogram adjustment. The built-in eye tracker was used to automatically compensates for static and dynamic cyclotorsion of the eye. In all cases, the flap was lifted and excimer laser ablation delivered to the stroma. Patients were instructed to concentrate on the fixation light throughout the ablation. When the ablation was completed, the flap was repositioned after the interface was irrigated with balanced salt solution, removing any debris.
Postoperative therapy included combination of topical antibiotic and steroid drops (Tobradex, Alcon, Fort Worth, Texas, USA) 4 times daily for two weeks, and artificial tears (Blink, Abbott Medical Optics, Santa Ana, CA, USA) 6–8 times daily for at least one month. At three and six months after surgery, all patients included for binocular vision assessment had uncorrected distant visual acuity of 20/20 or better at both eyes.
Postoperative assessmentIn agreement with the preoperative assessments, the postoperative examination included uncorrected distance visual acuity (UDVA), best corrected distance visual acuity (BCDVA), near stereoacuity, manifest refraction, corneal topography, tonometry, slit lamp and dilated funduscopic examination. Stereoacuity and aniseikonia was measured using the same apparatus and under the same conditions as preoperatively. All patients had unremarkable LASIK and all data were obtained under the same ambient conditions with the patient wearing the best spectacle correction.
Patients were included in the following groups:
Monocular myopes (I), one eye required a myopic correction and the contralateral eye required none as it was near emmetropia (manifest refraction no greater than ±1.00D along any single meridian). The anisometropia before surgery was between -0.50D and -8.50D. This was the only group of patients that had LASIK performed on one eye, the eye with significant ametropia. The other eye remained untreated. The other treated groups received LASIK in both eyes.
Binocular myopes (II), where the pre-existing anisometropia was less than 0.75D.
Binocular hyperopes (III), where the pre-existing anisometropia was less than 0.75D.
Binocular astigmats (IV), where the pre-existing astigmatism was no less than 1.00D in both eyes, anisometropic sphere was less than 0.75D and anisometropic astigmatism was no greater than 1.00D.
Anisometropes (V), where the pre-existing anisometropia ranged from 2.00 to 8.00D.
An age, and gender, matched control of binocular emmetropes was also included (group VI). Measurements were recorded at preop, three and six months postop.
Analysis of collected dataAll data were stored on an appropriate spread sheet (Excel, Microsoft Corp), checked for normality and analyzed using appropriate statistical tests. First, tests were used to determine if there was any significant difference in either aniseikonia or stereoacuity at distance and near between groups preoperatively. Second, statistical tests were used to determine if there was any significant difference in either aniseikonia or stereoacuity at distance and near between the groups at three and six months postoperatively. Third, tests were used to determine the significance of any apparent change in either aniseikonia or stereoacuity at distance and near within each group between preoperative, three and six months postoperative visits. Fourth, an analysis was performed to determine the significance of any association between the change (Δ) in aniseikonia and stereoacuity at distance and near with the preoperative value. And, depending on the outcomes of the first four stages of analysis, an additional analysis was done to determine the significance of any association between the aniseikonia and stereoacuity (near and distance) at pre- and postoperative visits. Finally, a checking of the significance of any correlation between the preoperative anisometropia in groups I and V (monocular myopes and anisometropes) with the preoperative aniseikonia and stereoacuity (near and distance) was performed.The significance level was set at a p < 0.05 and adjusted for the Bonferroni correction where appropriate.
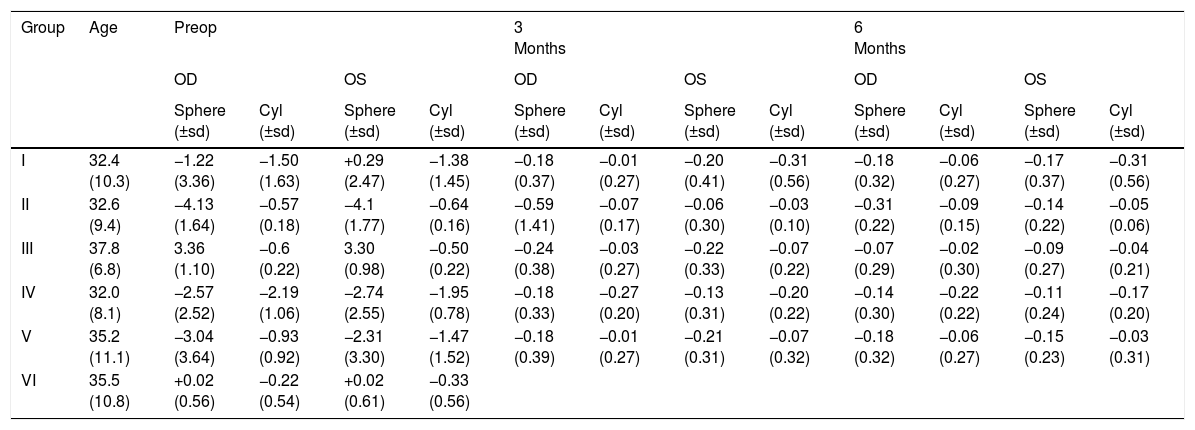
ResultsNinety-eight patients and 20 controls were recruited in this study. The mean (±sd) age and refractive errors of patients and control subjects are shown in Table 1.
Mean refractive error in each group before and after LASIK.
| Group | Age | Preop | 3 Months | 6 Months | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OD | OS | OD | OS | OD | OS | ||||||||
| Sphere (±sd) | Cyl (±sd) | Sphere (±sd) | Cyl (±sd) | Sphere (±sd) | Cyl (±sd) | Sphere (±sd) | Cyl (±sd) | Sphere (±sd) | Cyl (±sd) | Sphere (±sd) | Cyl (±sd) | ||
| I | 32.4 (10.3) | −1.22 (3.36) | −1.50 (1.63) | +0.29 (2.47) | −1.38 (1.45) | −0.18 (0.37) | −0.01 (0.27) | −0.20 (0.41) | −0.31 (0.56) | −0.18 (0.32) | −0.06 (0.27) | −0.17 (0.37) | −0.31 (0.56) |
| II | 32.6 (9.4) | −4.13 (1.64) | −0.57 (0.18) | −4.1 (1.77) | −0.64 (0.16) | −0.59 (1.41) | −0.07 (0.17) | −0.06 (0.30) | −0.03 (0.10) | −0.31 (0.22) | −0.09 (0.15) | −0.14 (0.22) | −0.05 (0.06) |
| III | 37.8 (6.8) | 3.36 (1.10) | −0.6 (0.22) | 3.30 (0.98) | −0.50 (0.22) | −0.24 (0.38) | −0.03 (0.27) | −0.22 (0.33) | −0.07 (0.22) | −0.07 (0.29) | −0.02 (0.30) | −0.09 (0.27) | −0.04 (0.21) |
| IV | 32.0 (8.1) | −2.57 (2.52) | −2.19 (1.06) | −2.74 (2.55) | −1.95 (0.78) | −0.18 (0.33) | −0.27 (0.20) | −0.13 (0.31) | −0.20 (0.22) | −0.14 (0.30) | −0.22 (0.22) | −0.11 (0.24) | −0.17 (0.20) |
| V | 35.2 (11.1) | −3.04 (3.64) | −0.93 (0.92) | −2.31 (3.30) | −1.47 (1.52) | −0.18 (0.39) | −0.01 (0.27) | −0.21 (0.31) | −0.07 (0.32) | −0.18 (0.32) | −0.06 (0.27) | −0.15 (0.23) | −0.03 (0.31) |
| VI | 35.5 (10.8) | +0.02 (0.56) | −0.22 (0.54) | +0.02 (0.61) | −0.33 (0.56) |
I monocular myopes, II binocular myopes, III binocular hyperopes IV binocular astigmats, V anisometropes. The associated standard deviations are noted in parentheses. At 6 months postop, there was no significant differences in either the spherical or cylindrical components of the refractive error between the five treated groups.
In general, binocularity and aniseikonia improved in all 98 patients. There were no cases of stereoacuity or aniseikonia worsening after LASIK. The total number of cases where a change was not found are as follows near stereoacuity, 40; distance stereoacuity, 38; aniseikonia, 35. The majority of these cases were from groups II & III (near stereoacuity, 25 cases; distance stereoacuity, 27 cases; aniseikonia, 21 cases). A summary of the main results is included in Tables 2–4 and Figs. 1–4. The RMS of the differences in the best spherical equivalents between the right and left eyes at pre- and three months postop in group I (monocular myopes) and V (binocular anisometropes) were 2.94D (±1.99) and 3.07D (±1.63), reducing to 0.51D (±0.36) and 0.46D (±0.29), respectively.
Preliminary analysis of the data revealed that stereoacuity and aniseikonia values did not adhere to a normal gaussian distribution (Kolmogorov-Smirnov one sample test, p < 0.05). Therefore, the data were subjected to appropriate non-parametric statistical tests.
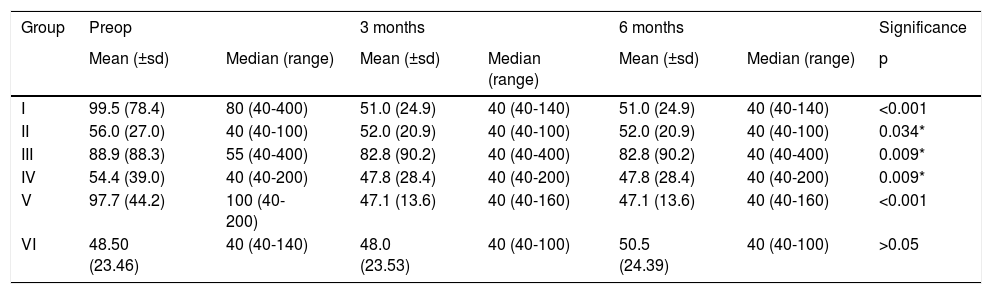
Near stereoacuity before and after LASIK.
| Group | Preop | 3 months | 6 months | Significance | |||
|---|---|---|---|---|---|---|---|
| Mean (±sd) | Median (range) | Mean (±sd) | Median (range) | Mean (±sd) | Median (range) | p | |
| I | 99.5 (78.4) | 80 (40-400) | 51.0 (24.9) | 40 (40-140) | 51.0 (24.9) | 40 (40-140) | <0.001 |
| II | 56.0 (27.0) | 40 (40-100) | 52.0 (20.9) | 40 (40-100) | 52.0 (20.9) | 40 (40-100) | 0.034* |
| III | 88.9 (88.3) | 55 (40-400) | 82.8 (90.2) | 40 (40-400) | 82.8 (90.2) | 40 (40-400) | 0.009* |
| IV | 54.4 (39.0) | 40 (40-200) | 47.8 (28.4) | 40 (40-200) | 47.8 (28.4) | 40 (40-200) | 0.009* |
| V | 97.7 (44.2) | 100 (40-200) | 47.1 (13.6) | 40 (40-160) | 47.1 (13.6) | 40 (40-160) | <0.001 |
| VI | 48.50 (23.46) | 40 (40-140) | 48.0 (23.53) | 40 (40-100) | 50.5 (24.39) | 40 (40-100) | >0.05 |
All units in seconds of arc. The p values are for the comparisons between preop and 3 months postop, * accepted as not significant after applying the Bonferroni correction. There was no significant change between 3 and 6 months postop in each treated group. The control group (VI) remained stable throughout. I monocular myopes, II binocular myopes, III binocular hyperopes IV binocular astigmats, V anisometropes.
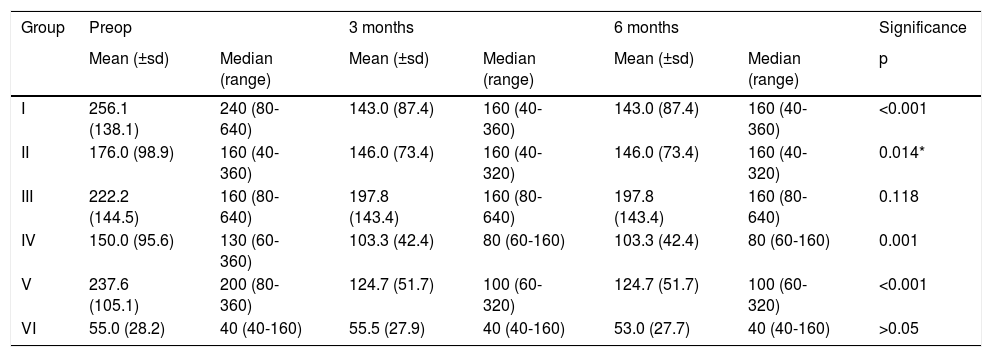
Distance Stereoacuity before and after LASIK.
| Group | Preop | 3 months | 6 months | Significance | |||
|---|---|---|---|---|---|---|---|
| Mean (±sd) | Median (range) | Mean (±sd) | Median (range) | Mean (±sd) | Median (range) | p | |
| I | 256.1 (138.1) | 240 (80-640) | 143.0 (87.4) | 160 (40-360) | 143.0 (87.4) | 160 (40-360) | <0.001 |
| II | 176.0 (98.9) | 160 (40-360) | 146.0 (73.4) | 160 (40-320) | 146.0 (73.4) | 160 (40-320) | 0.014* |
| III | 222.2 (144.5) | 160 (80-640) | 197.8 (143.4) | 160 (80-640) | 197.8 (143.4) | 160 (80-640) | 0.118 |
| IV | 150.0 (95.6) | 130 (60-360) | 103.3 (42.4) | 80 (60-160) | 103.3 (42.4) | 80 (60-160) | 0.001 |
| V | 237.6 (105.1) | 200 (80-360) | 124.7 (51.7) | 100 (60-320) | 124.7 (51.7) | 100 (60-320) | <0.001 |
| VI | 55.0 (28.2) | 40 (40-160) | 55.5 (27.9) | 40 (40-160) | 53.0 (27.7) | 40 (40-160) | >0.05 |
All units in seconds of arc. The p values are for the comparisons between preop and 3 months postop, * accepted as not significant after applying the Bonferroni correction. There was no significant change between 3 and 6 months postop in each treated group. The control group (VI) remained stable throughout. I monocular myopes, II binocular myopes, III binocular hyperopes IV binocular astigmats, V anisometropes.
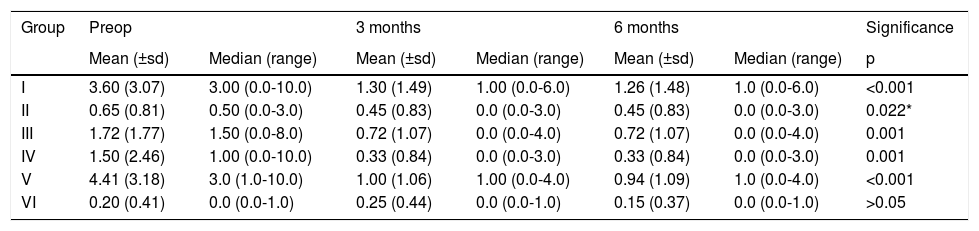
Aniseikonia before and after LASIK.
| Group | Preop | 3 months | 6 months | Significance | |||
|---|---|---|---|---|---|---|---|
| Mean (±sd) | Median (range) | Mean (±sd) | Median (range) | Mean (±sd) | Median (range) | p | |
| I | 3.60 (3.07) | 3.00 (0.0-10.0) | 1.30 (1.49) | 1.00 (0.0-6.0) | 1.26 (1.48) | 1.0 (0.0-6.0) | <0.001 |
| II | 0.65 (0.81) | 0.50 (0.0-3.0) | 0.45 (0.83) | 0.0 (0.0-3.0) | 0.45 (0.83) | 0.0 (0.0-3.0) | 0.022* |
| III | 1.72 (1.77) | 1.50 (0.0-8.0) | 0.72 (1.07) | 0.0 (0.0-4.0) | 0.72 (1.07) | 0.0 (0.0-4.0) | 0.001 |
| IV | 1.50 (2.46) | 1.00 (0.0-10.0) | 0.33 (0.84) | 0.0 (0.0-3.0) | 0.33 (0.84) | 0.0 (0.0-3.0) | 0.001 |
| V | 4.41 (3.18) | 3.0 (1.0-10.0) | 1.00 (1.06) | 1.00 (0.0-4.0) | 0.94 (1.09) | 1.0 (0.0-4.0) | <0.001 |
| VI | 0.20 (0.41) | 0.0 (0.0-1.0) | 0.25 (0.44) | 0.0 (0.0-1.0) | 0.15 (0.37) | 0.0 (0.0-1.0) | >0.05 |
All values are expressed as percentages. The p values are for the comparisons between preop and 3 months postop, * accepted as not significant after applying the Bonferroni correction. There was no significant change between 3 and 6 months postop in each treated group. The control group (VI) remained stable throughout. I monocular myopes, II binocular myopes, III binocular hyperopes IV binocular astigmats, V anisometropes.
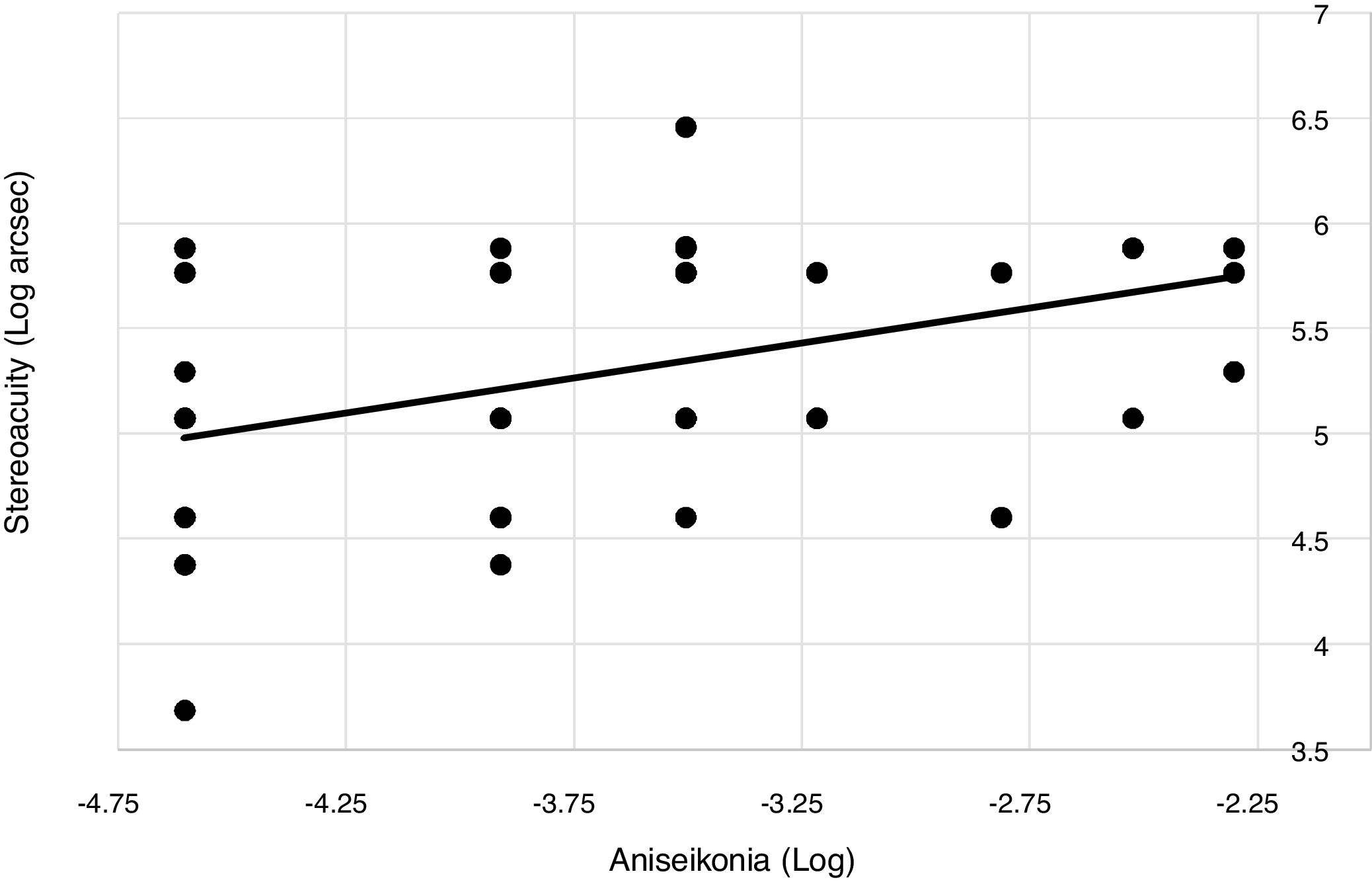
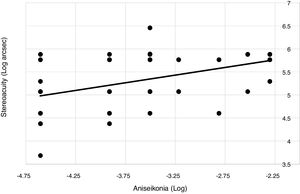
Preop distance stereoacuity and aniseikonia. The results shown correspond to all preop data pooled from groups I–V. The values are natural log transforms of the raw data. The values for aniseikonia are the transformations of the decimal values. The least squares line is characterized by y2 = 0.333x + 6.513 (r = 0.462, n = 76, p < 0.001).
At preop, differences in near stereoacuity, distance stereoacuity and aniseikonia between the six groups were statistically significant. Significant inter-group differences were also found after excluding the data from the control group (Kruskal-Wallis test near stereoacuity H = 27.46, p < 0.001; distance stereoacuity H = 12.8, p = 0.012; aniseikonia H = 30.92, p < 0.001). At three months postop, significant differences between all six groups were also found for distance stereoacuity (H = 41.19, p < 0.001) and aniseikonia (H = 15.53, p = 0.008), but not for near stereoacuity (H = 4.39, p = 0.493). After excluding the control group data, there were no significant inter-group differences in stereoacuity at either near or distance (p > 0.05). However, a significant inter-group difference in aniseikonia was detected (H = 10.84, p = 0.028), but this was rejected after applying the Bonferonni correction.
Tables 2–4 show, after applying the Bonferonni correction, that there were significant changes in near stereoacuity in groups I and V, distance stereoacuity in groups I, IV and V, and aniseikonia in groups I, III, IV and V between pre-and three months postop (Wilcoxon Signed Rank test). In each group, there was no significant change between three and six months postop. For each patient, in groups I, IV and V, the change in stereoacuity (near and distance) and aniseikonia was significantly correlated with the preop value (Kendall correlation coefficient, p < 0.001). However, this was not detected in groups II (binocular myopes) and III (binocular hyperopes).
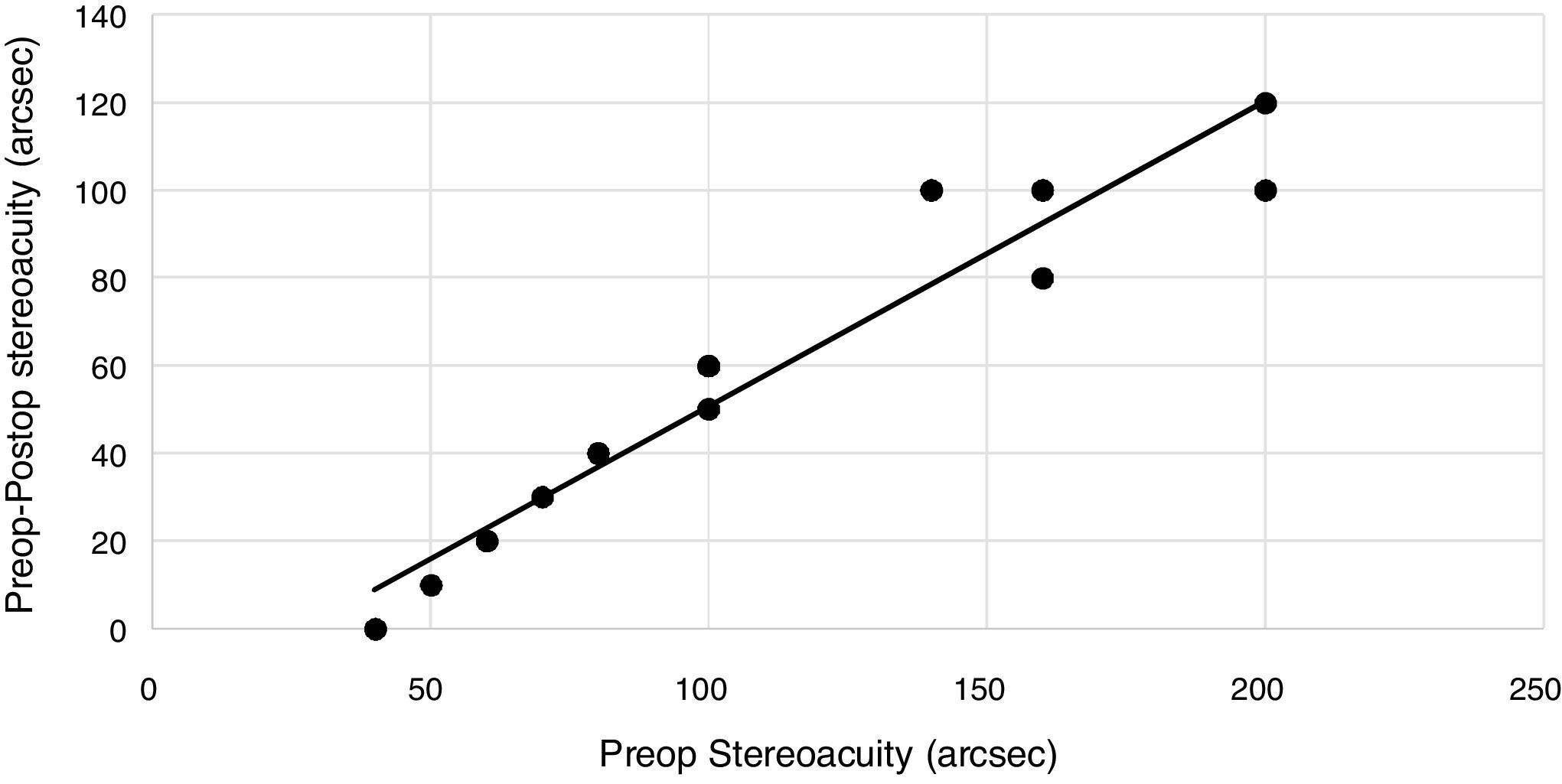
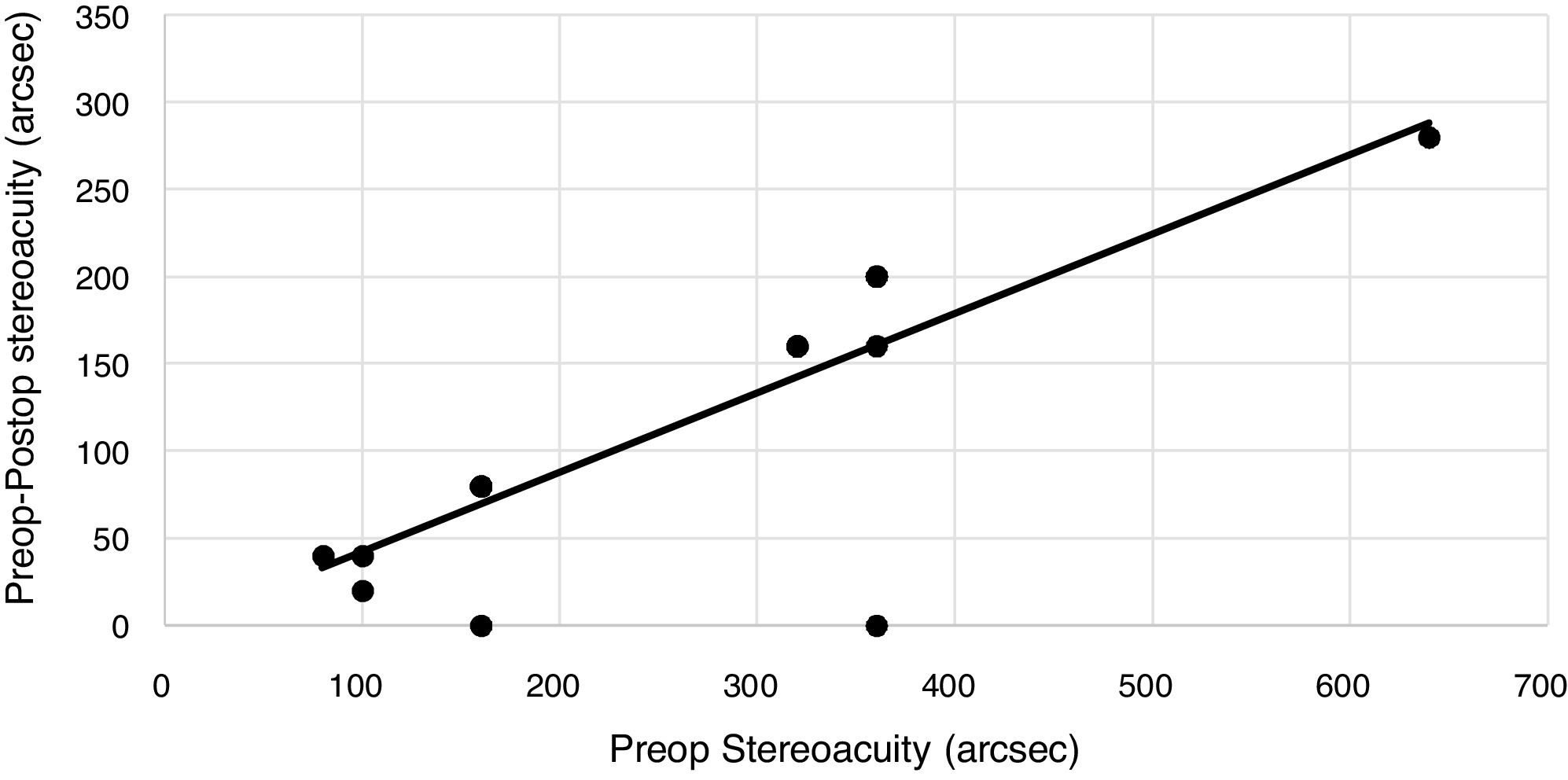
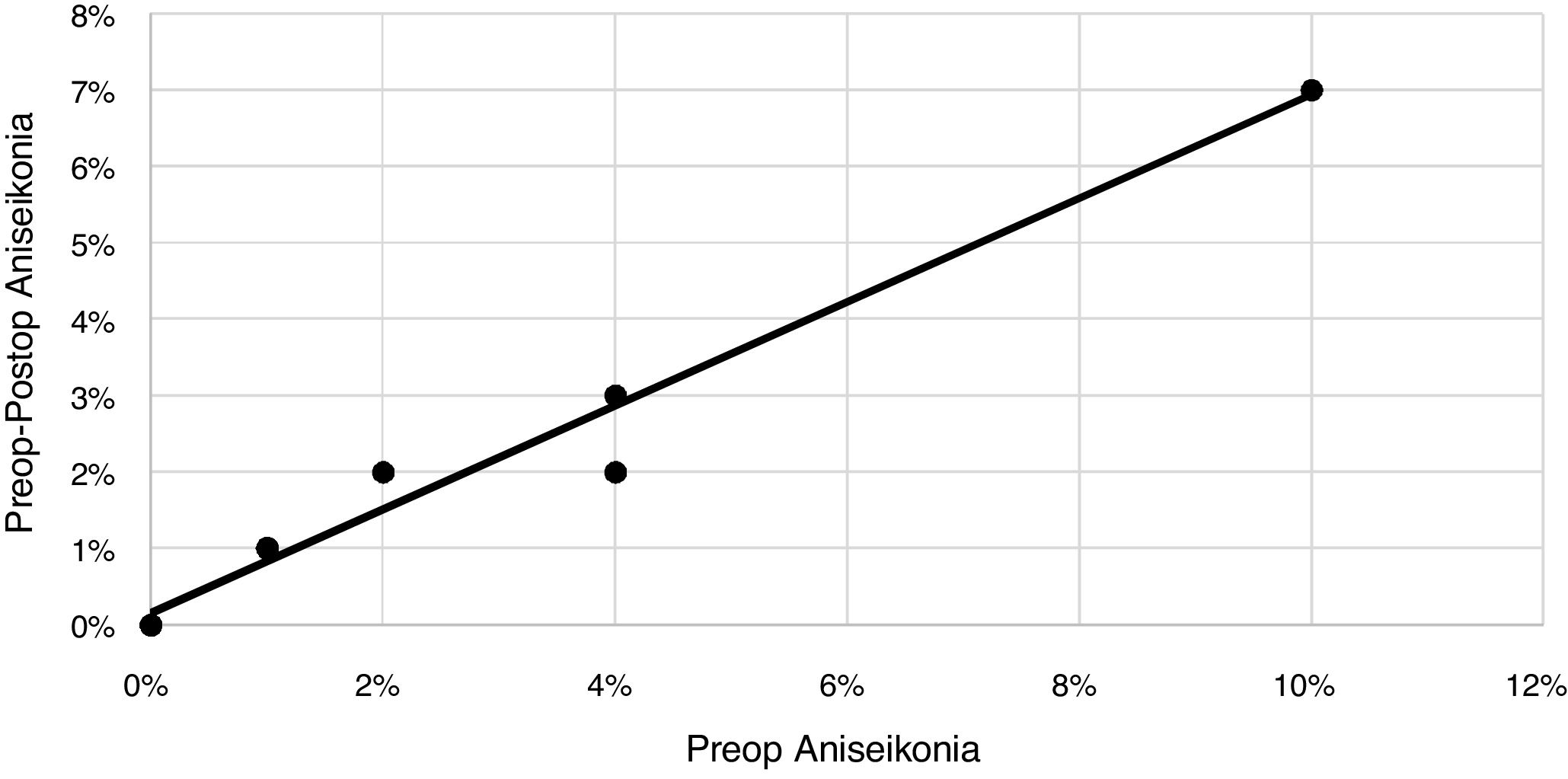
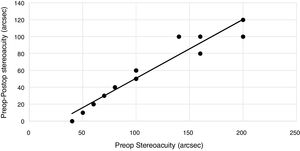
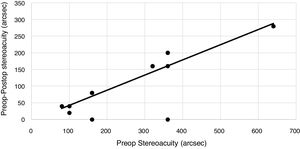
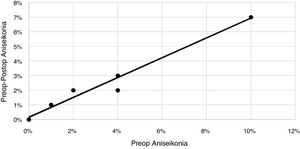
Figs. 1–3 are included to illustrate the association between the change (Δx) and the preop value (x) in stereoacuity (both near and distance) and aniseikonia in three selected groups. The least squares regression lines in the following three selected groups were as follows:
Fig. 1 (Group V, anisometropes, near stereoacuity),
Fig. 2 (Group I, monocular myopes distance stereoacuity),
Fig. 3 (Group IV, binocular astigmats, aniseikononia),
The preop data from the five treated groups were subjected to various permutations to reveal any significant correlations between aniseikonia and stereoacuity. The log transformations of aniseikonia and stereoacuity data were normally distributed (Kolmogorov-Smirnov one sample test, p > 0.05). This allowed the data to become amenable to further scrutiny using parametric statistical tests. Following on from this, significant associations were revealed between the log transforms of aniseikonia and stereoacuity. Excluding all cases where aniseikonia was zero (because the log of zero is not defined), the least squares regression lines equating log preop stereoacuity at near (y1) and log preop stereoacuity at distance (y2) with log preop aniseikonia (x) were as follows:
The use of the same approach with the postop data did not yield any significant correlations between aniseikonia and stereoacuity.
Pooling the preop data in groups I and V (monocular myopes and anisometropes) revealed no significant correlation between preop anisometropia (defined as the RMS of the difference in best spherical equivalents between the right and left eyes) and log near stereoacuity (r = 0.305, n = 40, p = 0.056) or log distance stereoacuity (r = 0.290, n = 40, p = 0.070) or log aniseikonia (r = 0.229, n = 40, p = 0.155).
DiscussionThe long term consequence of anisometropia is impaired binocular function. Thus, significant inter-group differences in binocularity at the pre-operative stage were not an unexpected finding. Tables 2–4 show that prior to surgery the isometropic groups (II, III and IV) had better stereoacuity and aniseikonia. After the LASIK, there was no significant difference between the treated groups. Overall, LASIK improved binocularity and the preop inter-group differences were nullified. Eqs 1–3 indicate that individual changes in stereoacuity and aniseikonia can be predicted in anisometropes and binocular astigmats. LASIK homogenised the five treated groups, but the postop steroacuity and aniseikonia were still below the levels in the control group.
Aniseikonia tended to improve in the treated groups. However, after making the Bonferonni correction, this was not the case in the binocular myopes (group II). Nevertheless, the overall tendency of LASIK to collapse the median value of aniseikonia to zero in three of the five ametropic groups was a positive step towards improving binocular function. If a patient had perceived a 2% larger image in the right eye preop and a 2% larger image in the left eye postop, then the actual change in image sizes would have been 4%. However, with reference to the definition of aniseikonia (as noted in the Introduction), we measured the absolute perceived size differences between the eyes. Thus, in a case such as this, the recorded change in aniseikonia would have been zero. From the outset, our aim was to observe and measure changes in aniseikonia, not the actual change in the size of the image perceived by each eye. With respect to the definition of aniseikonia, we found aniseikonia improved in the binocular hyperopes (group 3) and astigmatics (group 4). Table 1 notes the preop inter-ocular differences in the spectacle corrections within these two groups was no more than 0.50D. Our data clearly refute the findings of Liu et al 17 where they reported aniseikonia improved only in cases where anisometropia exceeed 2.5D. The results reported in Tables 1 and 4 show a tendency towards improved aniseikonia when the anisometropia was much less than 2.5D. In pseudophakes, Kramer et al.12 reported 40% of ophthalmic complaints were related to patients with aniseikonia. If such complaints are indeed attributed to aniseikonia in phakic patients, then we envisage LASIK to be a useful tool to address such cases when significant refractive errors are present.
The high correlation between the changes (Δ) in each of the three markers of binocular vision with the preop values in groups I, IV and V are encouraging. This shows that it is possible to predict the effect of LASIK on an individual case-by-case basis. For example, Fig. 1 indicates that near steroeacuity should improve by 50% after bilateral LASIK in an anisometrope. Fig. 2 predicts a 50% improvement in the distance stereoacuity is expected to occur after LASIK to correct a myopic eye where the contralateral eye is predominately emmetropic. Fig. 2 also shows two cases where a change in distance stereoacuity was not found. In reality, stereoacuity and aniseikonia may well have changed but remained undetected because of errors associated with a patient's ability to make a judgement. After having said that, a change from zero could only be noted in steps of 20 s of arc for stereoacuity and 1% for aniseikonia. Clearly, there is a limit in any prediction because, by defintion, unexpected surprises can never be fully erradicated.
We believe the improved stereoacuity and aniseikonia in the cases of bilateral astigmatism corrected by LASIK has not been reported previously. In Table 4 the median value of aniseikonia in group IV (binocular astigmats) fell from a preop value of 1.0% to 0.0% at three months postop. The change was small, though statistically significant, and it should be viewed in relation to the expected repeatabiliy of the Awaya test. It has been claimed that the repeatability of this test is ±0.50%,27 and as noted in Table 4, the inter-sessional repeatability of the test in the control group (VI) was below ±0.45% on all three occasions. Eq. 3 predicts preop aniseikonia of 2% should reduce to 0.6% following LASIK. Glancing at Fig. 3, it is clear that some cases still presented with persistent aniseikonia postoperatively. Chen et al.28 demonstrated the effect of induced astigmatic blur on stereoacuity. They found the depreciation in steroacuity was greater when the induced astigmatism was against-the-rule as opposed to with-the-rule. A corollary from their report is that steroacuity and aniseikonia following LASIK correction of astigmatism may have meridional dependency. This may account for cases of persistent aniseikonia in Fig. 3. The majority of patients in group IV presented with astigmatism that was predominantly with-the-rule before surgery. There was an insufficient range at our disposal to test this hypothesis. Futhermore, the Awaya test is designed to measure aniseikonia along the vertical meridian. Thus, depending on the preoperative axes of astigmatism of individual cases, aniseikonia may be reduced to zero along the vertical meridian but this may not be the case along all meridia.
The coefficients in eqs. 1–3 indicate that improvements in stereoacuity and aniseikonia are not only expected,but also highly predictable on a case-by-case basis following LASIK correction. For the bilateral astigmats, the improvements could be connected to the aberration free profile of the LASIK ablation, freeing up the astigmatic cases from the aberrations and distorting effects of trial lenses. There is a growing body of opinion that steroacuity, and overall binocularity, can be enhanced by improving the overall quality of the retinal image by targetting the deleterious effects of the high order optical aberrations of the eye.15,29 Inter-ocular differences in the levels of higher order aberrations and retinal image quality are known to impact on binocular contrast sensitivity function.18–23 Thus, improvements in overall binocular function could be achieved by aiming to reduce the negative impact of LASIK on higher order aberrations. Therefore, the aberration-free profile of the LASIK treatment may have contributed to the contracted range in the postop stereoacuity and aniseikonia noted in Tables 3 and 4. Nevertheless, when astigmatism was corrected with trial lenses preoperatively, the relative spectacle magnification (RSM) along the astigmatic power meridian would not have matched the RSM along the perpendicular axis. Hence, there was a propensity towards an ovalization of the retinal image when the spectacle lens corrected astigmatic eye viewed a circular object. This would have further contributed to any divergence in the overall quality, shape and size of the retinal images formed in the two eyes and subsequently impacted on aniseikonia and stereoacuity. The binocular correction of the refractive astigmatism erradicated this contribution to a reduced binocular function. As noted previously, data were obtained with the best spectacle correction in situ at all times. It could be argued that the distorting effects of any postoperative correcting lenses would also have contributed to a divergence in the overall quality of the retinal images formed in the two eyes. Table 1 clearly notes the postoperative residual refractive errors were very small compared with the preoperative counterparts. Thus, the distorting effects of postoperative spectacle corrections would have been negligible compared with the preoperative counterparts. Fig. 3 clearly shows that binocular LASIK correction of astigmatism reduces aniseikonia by 7% when the preoperative level is 10%.
The connection between stereoacuity and aniseikonia was established several years ago.30,31 Highman30 reported a significant correlation between the log of stereoacuity and aniseikonia expressed as a percentage. We did include this in our initial analysis. However, stronger correlations were uncovered after considering the log transformations of both stereoacuity and aniseikonia data. The correlations between preoperative distance and near stereoacuity with aniseikonia (eqs. 4 and 5) could be interpreted as evidence supporting a case of cause and effect. Iincreasing the inter-ocular disparity in perceived size results in a decline in stereoacuity. This clinical finding supports results found under more controlled experimental settings where stereoacuity reduced as the level of induced aniseikonia was artificially increased.31
The content of Fig. 4 shows that poor aniseikonia is associated with poor distance stereoacuity. However, a similar association between the stereoacuity and aniseikonia was not revealed postoperatively. Tables 2–4 show the reduction of range and variance of both stereoacuity and aniseikonia data after LASIK correction of refractive errors. We can only speculate that both homogenizing and narrowing the range in the data contributed to a lack of significance being detected between stereoacuity and aniseikonia postoperatively.
A correlation between preoperative anisometropia, aniseikonia and stereoacuity is expected based on the assumption that anisometropia is a major cause of binocular vision anomalies. The magnitude of stereoacuity after LASIK has been linked to preoperative anisometropia8 and earlier reports showing the associations between anisometropia and aniseikonia add further weight to this hypothesis.32,33 However, our data on the 40 cases of anisometropia (groups I and V) did not reveal any association between preoperative anisometropia and aniseikonia or stereoacuity. Antona et al.34 employed a sophisticated test for measuring aniseikonia and found a correlation between anisometropia and aniseikonia along the vertical meridian, but not along the horizontal. We had expected to uncover some association between preoperative anisometropia and aniseikonia even though the Awaya test estimates aniseikonia along the vertical meridian. This was not the case possibly because the Awaya test has been claimed to underestimate aniseikonia.,35,36 An underestimation may have masked a real correlation between preoperative anisometropia and aniseikonia.Our subjects were adults that probably adapted to their binocular anomalies. Any genuine empirical link between anisometropia and either aniseikonia or stereoacuity may have been modified by the effects of neuro-adaptation.
ConclusionBilateral LASIK tended to improve the binocular status in all groups except binocular myopes. The improved binocular vision in the monocular myopes and anisometropes was, to some extent, expected. However, by six months postoperatively, the binocularity of all five treated groups was still not comparable with the normal control group. Further work is required to investigate why the status of binocularity improved in the binocular astigmats.
Conflicts of interestThe authors have no conflicts of interest to declare.