The impact of visual outcomes of cataract surgery can be measured using a questionnaire. The aim of our study was to evaluate how patient quality of life changes after cataract surgery and if there are differences between the responses of patients with nuclear, cortical, and posterior subcapsular cataracts, which has not been studied before.
MethodWe studied 210 cataract patients who were divided into 3 cataract groups based on their cataract type: nuclear (n = 80), cortical (n = 70), and posterior subcapsular (PSC) (n = 60). The patients completed the Visual Function Index (VF-14) questionnaire before, 2 weeks and 1 month after bilateral cataract surgery. The results were analysed using one-way ANOVA (significance level 5 %) and were compared over time and between the cataract groups.
ResultsBefore the cataract surgery, cortical cataract patients had the lowest questionnaire score compared to nuclear and posterior subcapsular cataract groups (p = 0.08). After cataract surgery, cortical cataract patients experienced the greatest improvement in near distance daily activities, while PSC cataract patients experienced the greatest improvement in far distance daily activities (p = 0.38). Before surgery, nuclear cataract patients had the highest questionnaire scores compared to the other cataract groups (p = 0.08).
ConclusionAt the 1 month follow-up, there were no statistically significant differences in questionnaire scores between the cataract groups for any of the questions. Overall, cortical cataract patients showed a trend to experience the greatest subjective improvement in quality of life after cataract removal, followed by nuclear and posterior subcapsular patients.
A cataract is a clouding of the crystalline lens in the eye. It is a common condition after age of 40 and 4,7 million surgeries per year are performed in Europe.1 In Latvia, around 10,000 cataract surgeries are performed each year.2 Cataracts can be classified based on their location within the lens, with the three most common types being nuclear, cortical, and posterior subcapsular (PSC).1 These types can occur individually or in combination. Cataract progression varies depending on the type of cataract and other factors such as general health and environmental factors.3,4 Nuclear cataracts tend to progress more slowly, while PSC cataracts progress more rapidly than cortical and nuclear cataracts.4 General health conditions such as hypertension and diabetes have also been linked to the development of cataracts. Hypertension can lead to changes in the lens capsule and disruptions in ion transport in lens epithelial cells, as well as an increase in oxidative free radicals.5 Other studies have shown an association between obesity, hyperlipidaemia, and cataracts, particularly PSC cataracts.6
Cataracts usually develop slowly and may not cause symptoms at first. Depending on the location of the opacity, cataracts can affect vision differently, causing different symptoms in each type. If the opacity is located in the centre of the lens (nuclear cataract), it may affect visual acuity more at a distance than up close. If the opacity is in the form of spokes (cortical cataract), patients may complain about glare and monocular diplopia.1,4 If the opacity is located just inside the posterior lens capsule (PSC), it can cause significant visual impairment if it affects the axial region of the lens. The severity of symptoms such as reduced visual acuity, reduced contrast vision, glare, and impaired color vision may vary at different stages of cataract development.7
The treatment outcomes are important and relevant to each patient, and the criteria for a successful outcome can vary depending on patient needs, lifestyle, and medical condition. The outcomes may include reduced visual symptoms, improved visual function, achievement of the desired refractive condition, and improved mental health.8,9 After cataract removal, people may be able to perform everyday tasks more easily and with greater independence, including activities such as driving, reading, and watching TV. Studies have shown that mental health, physical function, and quality of life can be enhanced when visual function is restored through cataract surgery.10,11 However, there is a lack of information in the literature about outcome satisfaction for different types of cataracts.
According to the American Academy of Ophthalmology (2021) guidelines, symptomatic cataracts are considered a surgical disorder. As eye health specialists, it is our responsibility to monitor cataract progression and understand if patient complaints are related to the condition.1 Visual function can be assessed using standard visual acuity tests and contrast sensitivity charts, but these tests may not cover all daily activities.12 The impact of cataracts can be subjectively assessed through self-reported status.13 This is why subjective questionnaires can be a useful method for comparing objective and subjective findings.10,12,13 The aim of our study was to evaluate how patient quality of life changes after cataract surgery and if there are differences between the responses of patients with nuclear, cortical, and posterior subcapsular cataracts. The results of our study can serve as informative material for eye health specialists to help prepare patients for what to expect after cataract surgery.
MethodIn our study we evaluated patient subjective quality of life before and 2 weeks and 1 month after cataract surgery, to nuclear, cortical and posterior subcapsular cataract patients.
PatientsThis study analysed 210 cataract patients (420 eyes, mean age 64 ± 6 years). All the patients were divided in 3 groups depending on their cataract type: nuclear (n = 80 patients; 160 eyes), cortical (n = 70), posterior subcapsular (n = 60). The type of the cataract was diagnosed by an ophthalmologist but the information about cataract grade was not indicated in the patient history and could not be addressed in this study. Patient eye structures before, 2 weeks and 1 month after cataract removal surgery were examined with a slit lamp, anterior and posterior ocular coherent tomography (Zeiss Cirrus 6000), endothelial microscopy (Nidek ConfoScan 4), tonometry (Topcon CT-800), and an autorefractometer (Topcon KR-800). Patients with age related macular degeneration, diabetic retinopathy and glaucoma were excluded from the research.
The cataract surgery was performed for both eyes of the patient with a 2 day delay between them. Surgeons implanted 420 monofocal AcrySof Natura SN60AT (Alcon) intraocular lenses, with a target refraction of 0 Dioptres. The surgery was performed with femtosecond laser-assisted cataract method (Zeiss Victus laser). For all the patients the target refraction was 0 Dioptres. None of the patients experienced complications after cataract removal like macular edema or increased intraocular pressure.
Before and after cataract surgery, patient visual acuity was measured monocularly using the Snellen chart (decimal units). The best corrected visual acuity in far and near distance, and optical refraction pre and post-surgery can be seen in Table 1, which describes both eye data to all the cataract groups (nuclear, cortical, PSC). The best optical correction was measured with a step of 0.25 dioptres (D) and was recalculated in spherical equivalent (SE). Visual acuity in far, near distance, optical correction was collected before, 2 weeks and 1 month after cataract surgery by an optometrist. Binocular vision assessment and far distance stereopsis test was performed before and 2 weeks after the cataract surgery using Worth and polarized tests. Binocular vision and stereopsis was observed to all the patients before and after cataract surgery. The testing took place at Dr. Solomatin Eye center (Riga, Latvia) and was approved by the Ethical Committee of University of Latvia. All the patients were informed about methodology of this research and sigh an approval to use their data for this research. The research was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki.
Baseline characteristics of all enrolled cataract eyes monocularly (n = 420) before and 2 weeks after cataract surgery. The results demonstrates nuclear, cortical, posterior subcapsular patients the best optical correction, uncorrected (UC) and corrected (CC) visual acuity in far and near distances.
To better understand patient subjective feelings before and after cataract surgery we collected information with the Visual function questionnaire (VF-14). The VF–14 is a brief questionnaire designed to measure functional impairment on patients due to cataract. This questionnaire is often used in research studies to measure the effectiveness of a particular treatment or to assess the impact of a visual impairment on patient quality of life, and can be compared across various time periods and populations.13,14
The Visual function questionnaire contains 14 questions which covers daily life activities like reading different size of prints, recognizing people, driving etc. (see Table 2) Patient has to grade their answer form: no = 4; yes, with a little difficulty = 3; yes, with a moderate amount of difficulty = 2; yes, with a great deal of difficulty = 1; yes, and am unable to do the activity = 0; blank if the question is not applicable. Questionnaire scores are calculated as the summated responses divided by the number of valid responses multiplied by 25. The final score ranges between 0 and 100. A score of 100 indicates ability to do all applicable activities, 0 indicates inability to do all applicable activities because of vision. Results from 0 – 29 indicated severe; 30 – 74 moderate; 75 – 98 mild; 99 – 100 no visual impairment.
Visual function (VF-14) questionnaire questions.13
The patients filled out the Visual function questionnaire (VF-14) at various periods: 1 hour before the first eye cataract surgery, 2 weeks and 1 months after the second eye's cataract removal surgery by themselves or with a help of an optometrist. Patients were recommended to compare their subjective feeling to previous follow-ups.
The results were analysed with ANOVA one way test (significance level 5 %). We compared the differences between before and after surgery scores to each question and cataract group.
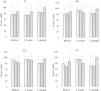
ResultsIn our study, we investigated how cataract affects patient subjective quality of life. The questionnaire scores of all the patients before and after cataract surgery can be found in Table 3. Before cataract surgery, patients reported significant problems with reading small print (see Table 3). The questionnaire score for the first question showed the lowest result compared to the other questions. After cataract surgery, patients experienced significant improvement at the 2-week and 1-month follow-up (p < 0.01). Overall, 2 weeks after cataract surgery, for 34 % of patients near distance visual acuity remained unchanged, while for 47 % improved. Before and 2 weeks after cataract surgery, cortical and nuclear cataract patients had the lowest subjective satisfaction with reading small print (see Fig. 1). The groups showed no statistically significant difference between questionnaire results before (p=0.08) and 2 weeks after surgery (p=0.38). The cortical cataract group experienced the greatest improvement in the first question. One month after cataract removal, there was no statistically significant difference between the groups (p=0.28).
VF-14 questionnaire mean score along with their standard deviations before and after cataract surgery. Table describes patient answers (n = 210) before, 2 weeks and 1 month after the cataract surgery. The questionnaire score is analysed by comparing different follow-up period answers. P values in bold demonstrate statistically significant difference between questionnaire score in different time periods.
Patient questionnaire scores to the first (left) and second (right) question. Figure demonstrates patient (n = 210) answers before, 2 weeks and 1 month after the cataract surgery. Dotted bars corresponds to cortical (n = 80), lined bars to nuclear (n = 70) and grey colour bars to posterior subcapsular patient answers (n = 60) at the different time periods. In the first question before the surgery cortical cataract patients showed the worst subjective feelings about reading small print. In the second question, there were no statistically significant difference between cataract groups (p > 0.05).
Patients experienced significant improvement in reading medium-sized letters (question no.2) after cataract surgery (p < 0.01). Before, 2 weeks, and 1 month after cataract removal, there was no statistically significant difference between the questionnaire scores of the cataract groups. Two weeks after the surgery, posterior subcapsular patients reported a subjective reduction in reading activity (p=0.02), which improved at the 1-month period (see Fig. 1).
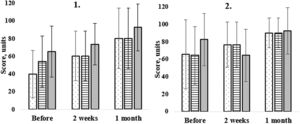
At the 2-week follow-up, patients reported subjective improvement in reading larger print (p < 0.01; n = 210), but there was no statistically significant change compared to the 1-month follow-up data (p=0.23). This function was not affected by cataract and showed relatively high subjective satisfaction with reading larger print. There were no statistically significant differences between the cataract groups (p > 0.16) at all follow-ups (see Fig. 2).
Patient questionnaire scores to the third (left) and fourth (right) question. Figure demonstrates patients (n = 210) answers before, 2 weeks and 1 month after cataract surgery. Dotted bars correspond to cortical (n = 80), lined bars to nuclear (n = 70) and grey colour bars to posterior subcapsular patient answers (n = 60) at the different time periods. There was no statistically significant difference between the cataract groups to at various time periods to both questions (p > 0.05).
To the fourth question all the patients experienced improvement in face recognition 2 weeks after cataract surgery (p < 0.01), but the subjective questionnaire score did not change statistically significantly when compared to before and 1-month follow-up results (p=0.38). The results showed no statistically significant differences between all cataract groups before (p > 0.29), and at 2 weeks (p > 0.16) and 1 month follow-up (p > 0.08).
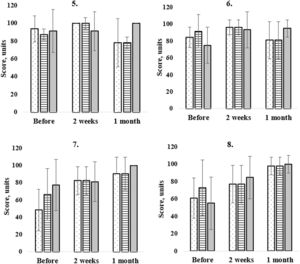
In our study cataract patients (n = 210) did not have difficulties to see stairs and steps (see Table 3; question no.5). Right after bilateral cataract surgery patients did not have a statistically significant difference (p=0.34), but the difference was noted at the 1 month follow-up (p < 0.01).
Before the surgery, nuclear cataract patients had a statistically significant different questionnaire score compared to PSC (p=0.04) (see Fig. 3). Posterior subcapsular patients and cortical patient scores were not statistically different (p=0.40). Two weeks after cataract surgery, nuclear cataract group had the biggest questionnaire score improvement for the fifth question but did not show a statistically significant difference as compared to PSC (p=0.16) and cortical cataract group (p=0.16). At the 1 month follow-up, there were no differences between cataract groups, but the questionnaire score decreased dramatically and showed large standard deviations (see Fig. 3).
Patient questionnaire scores to the fifth (5.),sixth (6.), seventh (7.) and eighth (8.) question. Figure demonstrates patients (n = 210) answers before, 2 weeks and 1 month after cataract surgery. Dotted bars correspond to cortical (n = 80), lined bars to nuclear (n = 70) and grey colour bars to posterior subcapsular patient answers (n = 60) at the different time periods. Before the cataract surgery there was a statistically significant difference in the fifth and sixth question between posterior subcapsular and nuclear patient scores. Before the cataract surgery there was a statistically significant difference between all the groups (seventh question). Nuclear and posterior subcapsular patient scores were statistically significantly different only before the surgery (eight question).
At the sixth question about reading traffic, street or store signs patients experienced a statistically significant improvement at the 2 weeks (p < 0.01) and 1 month follow-up (p < 0.01), but there were no statistically significant differences between preoperative and 1 month postoperative mean questionnaire score (p=0.21). At the 1 month follow-up, 64 % of patients experienced distance visual acuity improvement for 1 or more visual acuity lines. Twenty percent of patients reached the same visual acuity than before surgery but 16 lost 1 or more visual acuity chart lines (0.10 decimal units). Before the surgery, PSC patients reached the worst questionnaire score (see Fig. 3) and there was a statistically significant difference between nuclear and PSC (p=0.02) and cortical vs nuclear (p < 0.01), but there was no difference between PSC and cortical group (p=0.45). At the 2 week (2 weeks: PCS vs NUC p=0.39; PCS vs C p=0.39; NUC vs C p=0.50) and 1 month follow-up, there were no statistically significant difference between all the cataract groups (1 month: PCS vs NUC p=0.21; PCS vs C p=0.18; NUC vs C p=0.32).
With ageing, sewing and knitting gets difficult.15 In our study, the patients experienced trouble with the handwork before the cataract surgery (see Table 3). The questionnaire score to the seventh question improved at 2 weeks (p < 0.01) and 1 month (p < 0.01) after cataract surgery (see Fig. 3). In each follow-up visit, the results significantly improved and patients showed no problems to perform a daily activity of sewing knitting. Before the surgery, all cataract groups showed statistically significant differences in the variables evaluated (p < 0.05).Two weeks after surgery, differences between cortical and nuclear groups were not statistically significant (p=0.50), but there was a difference with PSC group results (C vs PSC p = 0.04; N vs PSC p=0.04). At the 1 moth follow-up, PCS patients showed almost perfect questionnaire score which showed no problems in performing handwork activities. The questionnaire score was not statistically significant between all cataract groups (p < 0.10).
Eighth question covered daily activities like writing checks or filling out forms. The results showed a statistically significant difference between groups before (p < 0.01) and after cataract surgery (p < 0.01). The questionnaire score improved with time, reaching the best results at 1 month follow-up (see Table 3). Before the surgery, PSC patients experienced the biggest trouble filling out the forms and showed a statistically significant difference with nuclear cataract group results (p < 0.01) (see Fig. 3). Two weeks after the surgery, the questionnaire scores increased, with a statistically significant difference between nuclear and cortical groups (p < 0.01), and also between nuclear and PSC groups (p=0.02). At the 1 month follow-up, questionnaire scores did not show a statistically significant difference between all the cataract groups (p < 0.18).
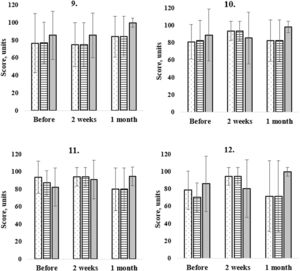
Ninth question scores demonstrate an ability to play a board games before and after cataract surgery (see Table 3). The questionnaire score improved at the 2 week (p < 0.01) and 1 month follow-up visits (p < 0.01). Before and after cataract surgery, there were no statistically significant differences between all the cataract groups (p > 0.05). The cortical group patients experienced the most trouble performing this task, but due to the high standard deviation this fact cannot completely confirmed.
Cataract patients often experience fear of falling, this makes them more careful when doing sport. Two weeks after cataract surgery, the questionnaire score to the tenth question experienced a significant change (p=0.02) (see Table 3). The subjective score did not change at the 1 month follow-up (p=0.48). All the cataract group results did not differ significantly before (p >0.14), at 2 weeks (p > 0.17) and 1 month after cataract surgery (p > 0.21) (see Fig. 4).
Patient questionnaire scores to the ninth (9.),tenth (10.), eleventh (11.) and twelfth (12.) question. Figure demonstrates patients (n = 210) answers before, 2 weeks and 1 month after cataract surgery. Dotted bars correspond to cortical (n = 80), lined bars to nuclear (n = 70) and grey colour bars to posterior subcapsular patient answers (n = 60) at the different time periods. Before the surgery cortical cataract group results were statistically significantly different as compared to nuclear and PSC group results (p = 0.05) (ninth question). At the one month follow-up the mean results were not statistically different.
The ability to watch television significantly improved after cataract surgery (p < 0.01) and did not change at the 1 month follow-up visit (p=0.24) (see Table 3). Before the surgery, PSC patients subjectively felt more affected while watching television than nuclear and cortical patients (see Fig. 4). The PSC group results were significantly different compared to nuclear (p < 0.01) and cortical groups (p=0.03), but there were no statistically significant differences between nuclear and cortical group results (p=0.47). At the 2 weeks follow-up visit, the same trends were observed and PSC results group differed significantly with those from nuclear (p < 0.01) and cortical groups (p < 0.01). However, at the 1 month follow-up visit, questionnaire scores corresponding to the eleventh question did not differ significantly between groups (p > 0.08).
Concerning the thirteenth and fourteenth question, only 76 patients responded that they drove a car. Two weeks after the cataract surgery, 76 answers were collected, but at the 1 month follow-up visit only 36 answers. Before and 2 weeks after surgery, patients did not experience subjective changes while driving in daylight, but at the 1 month follow-up visit there was a significant improvement (p < 0.04) (see Table 3). Before cataract surgery, the nuclear cataract group showed the greatest discomfort while driving during daylight, with statistically significant differences between all the cataract groups (p < 0.01). Two weeks after surgery, the greatest subjective improvement was noted in the nuclear group, but there were no statistically significant differences between the cataract groups at 2 week and 1 month follow-up visits (p > 0.05) (see Fig. 4).
In the fourteenth question, patients did not show subjective changes while driving during night time (see Table 3). The greatest improvement after cataract surgery was experienced by the cortical cataract group, which had a statistically significant difference in questionnaire scores as compared with nuclear (p < 0.01) and posterior subcapsular (p=0.05) patients. There was no statistically significant difference in results between the cataract groups at the 2 week and 1 month follow-up postoperative visits.
DiscussionIn the present study, cataracts significantly impacted the vision-related quality of life in most of the measured parameters, particularly general vision, near vision activities, and dependence. Additionally, greater visual impairment was significantly linked to lower scores on various quality of life subcategories, which predicted increased limitations in daily activities, leading to decreased social interactions and increased dependence, resulting in more psychosocial symptoms. Overall, our findings showed that quality of life improved at 2 weeks after cataract surgery, with a further increase at 1 month after surgery. During the testing, some participants explained that at 14 days after the cataract surgery , they were finally able to be more active and experienced daily activities more than at the 2 weeks of follow-up, being still careful and with reduced activity outside. Our finding correspond to several studies which reached the same conclusions.16-17
Depending on the type of cataract, we would expect that centre-located opacities would affect near functions more than peripheral opacities, as is the case with cortical cataracts.18-20 Cortical cataract patients experienced the biggest trouble doing handwork and had the biggest improvement after cataract surgery. However, our findings showed that cortical cataract patients experienced the greatest improvement in near distance tasks, such as reading and sewing. The refraction of the lens before surgery (whether the patient is myopic or hypermetropic) had a greater impact on daily tasks than the location of the opacity. In a study by Hassan et al. (2012), it was discovered that myopia was more common among individuals with nuclear and posterior subcapsular cataracts, while hyperopia was less prevalent in those with cataracts. From these findings, we can conclude that the location of the opacity primarily affects vision functions such as contrast sensitivity, glare, and colour vision, while the refraction of the lens influences visual acuity-related tasks.21
Patients with PSC experienced the worst results in recognising traffic signs and watching television. These daily tasks contain reflection from the object which strongly affect PSC patient and not been mentioned in the current literature.22 Before the cataract surgery, patients with nuclear cataract showed the highest satisfaction level compared to other cataract types. They typically develop gradually over time and are often associated with ageing. Due to gradual changes, patients do not feel the cataract progression until the refraction changes or the opacity noticeably blocks the light on visual axis. Other cataract types induce non-uniform refractive index change causing effects with noticeably decrease of the quality of vision (glare, halos...). The questionnaire answers related to reading large print, recognizing faces, and doing sports did not differ between cataract types before and after cataract surgery.
Before and after the cataract surgery, cataract type did not have an influence on different questionnaire scores about reading large print, books, recognizing faces and doing sports activities. There was no difference between cataract group answers after the surgery in terms of seeing steps and driving.
Cataract can affect vision and make seeing difficult, which can be a safety concern when driving.23 The severity of the vision impairment caused by cataracts can vary and may be more pronounced at certain times of day, such as at night, or under certain lighting conditions, such as when driving into the sunlight. The results of our study show that, before the cataract surgery, nuclear cataract patients had most of complains, after the surgery – there was no difference between cataract types. Studies have shown that people with cataracts are at an increased risk of being involved in an accident, and this risk is significantly reduced after cataract surgery.24,25 Drivers aged 55 and older are significantly less likely to adjust their driving practices after having cataract surgery in one eye (70 % less likely) or both eyes (90 % less likely). A study by Meuleners et al. (2021) found that the rate of crashes or near-crashes decreased significantly by 36 % after the first eye surgery and by 47 % after the second eye surgery. A separate model found that after the second eye surgery, the amount of time spent driving at speeds of 10 km per hour or more above the limit established was significantly shorter. In our research, only 36 patients filled out a questionnaire at the 1 month follow-up. To make further conclusions about driving-related quality changes in different cataract groups, the number of participants should be increased.26 Our findings showed that, before the cataract surgery, nuclear cataract patients had most of complaints, after the surgery – there was no difference between cataract types.
After cataract surgery, people typically experience an improvement in their vision, including visual acuity, which refers to the ability to see clearly and distinguish fine details. On average, patient visual acuity improved by 3 lines on a Snellen eye chart after surgery. Eye refraction fluctuations after cataract surgery can influence patient subjective feelings about visual acuity-related tasks. Refraction typically stabilizes at 1 week after cataract surgery. A study by Charlesworth et al. (2020) found that there was no statistical difference in sphere, cylinder, and spherical equivalent values at 1 and 4 weeks post-cataract surgery, suggesting that new glasses could be provided 1 week after surgery.27 Corneal swelling is a commonly mentioned factor that can influence the dioptric change post-surgery. It decreases between the first postsurgical day and the first week, and again between post-surgical weeks 1 and 2.27 Although thinning continues through the fourth post-surgical week, the changes are not significant. A large increase in cylinder from pre- to post-surgery is an indicator that refractive stability has not occurred, and these patients should not be prescribed new glasses and should be monitored and re-operated.28
Other factors that could influence the outcome of cataract surgery include the method by which the surgery is performed. In the present study, cataract surgery was performed using femtosecond laser, not phacoemulsification with ultrasound energy. Femtosecond laser-assisted cataract surgery (FLACS) involves three steps: corneal incisions (including optional limbal relaxing incisions to reduce astigmatism), anterior capsulotomy, and lens fragmentation.29 Advantages of FLACS over manual phacoemulsification include its precision and predictability in terms of capsulotomy size and centration, corneal wound construction, and nucleus fragmentation. FLACS may also increase the circularity and centration of the capsulorrhexis and the precision of the corneal incisions and may reduce the amount of ultrasonic energy required to remove a cataract. While FLACS is a safe and precise procedure, it only slightly improves visual outcomes compared to conventional cataract surgery performed by skilled surgeons (Bonnet), so the method should not significantly influence the final outcome.29
Neuroadaptation refers to the ability of the brain to adjust and adapt to changes in the visual system. It is believed that neuroadaptation plays a role on the final visual outcomes after intraocular lens (IOL) implantation.30 Neuroadaptation can take weeks to several months to adjust to the new IOL, but the time frame can vary from person to person. Some people may notice an improvement in their vision shortly after surgery, while others may take longer to adjust. Some people may experience visual side effects after IOL implantation, such as glare, halos around lights, or difficulty seeing at night, which may be due to the material of the IOL. Other factors that could influence the outcome of surgery include the shape or size of patient eyes or pupils.30
ConclusionTwo weeks after cataract removal surgery, patients experience a statistically significant improvement in quality of life, particularly related to near work. Overall, cortical cataract patients experience the greatest subjective improvement in quality of life after cataract removal, followed by nuclear and posterior subcapsular patients. Before surgery, nuclear cataract patients were not as severely affected in their daily activities as cortical and posterior subcapsular patients. Before surgery, patients with posterior subcapsular cataracts had most of complaints about daily activities related to objects with reflections, such as traffic signs. Regardless of the type of cataract, there was no significant difference in the questionnaire scores related to reading large print, books, recognizing faces, and doing sports activities before or after the surgery. After the surgery, there were no significant differences between the cataract group's answers related to visual tasks, such as seeing steps and driving.