To evaluate the prevalence of diagnosed dry eye syndrome, meibomian gland dysfunction, and blepharitis amongst the low vision population.
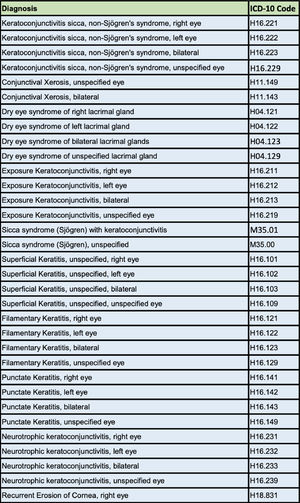
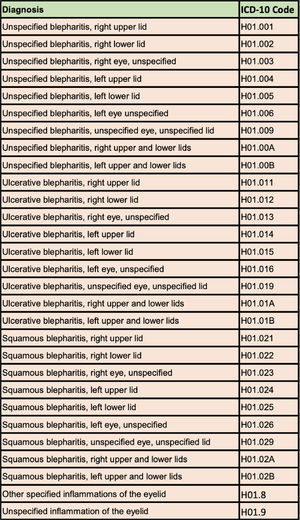
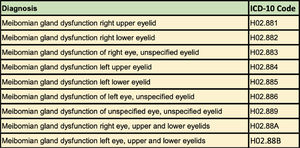
MethodsA retrospective analysis was conducted on patients seen in the University of Colorado Low Vision Rehabilitation Service between the dates of 12/1/2017 and 12/1/2022. 74 ICD-10 codes were used to identify patients as having dry eye syndrome or not having dry eye syndrome. Data was further analyzed to determine the prevalence of blepharitis and meibomian gland dysfunction using 29 blepharitis and 9 meibomian gland dysfunction ICD-10 codes. Data were also analyzed to determine the age and sex of the patients with diagnosed dry eye syndrome.
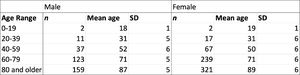
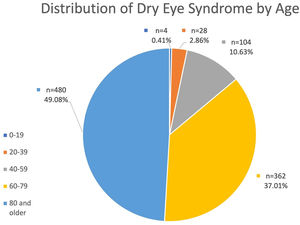
ResultsThe percentage of patients with a diagnosis of dry eye syndrome by an eyecare provider was 38.02 %. The prevalence of dry eye syndrome by age group was 3.57 % for 0–19 years, 14.35 % for 20–39 years, 29.07 % for 40–59 years, 43.79 % for 60–79 years, and 46.21 % for 80 and above. The prevalence of meibomian gland dysfunction and blepharitis was 11.90 % and 9.1 % respectively. Dry eye syndrome prevalence amongst males was 31.59 % and 42.47 % for females.
ConclusionThis study demonstrates that dry eye syndrome in the low vision population is a significant co-morbidity occurring in over a third of patients in the University of Colorado Low Vision Rehabilitation Service. These findings are meaningful as ocular comfort should not be overlooked while managing complex visual needs.
In the United States, visual impairment is one of the leading causes of disability.1-3 The prevalence of visual impairment and blindness is increasing the United States largely due to an aging population and shifting demographics.4,5 Data from 2017 estimated the prevalence of low vision amongst adults 45 years and older to be 3 % based on a best-corrected visual acuity (BCVA) of less than 20/40, 1.1 % based on a BCVA of less than 20/60, and 0.8 % based on a BCVA of less than 20/200.6 The leading causes of visual impairment in the United States includes macular degeneration, cataracts, glaucoma, and diabetic retinopathy.4 The overall prevalence of visual impairment increases with age, and the predominant underlying causes vary by race and ethnicity.4,7 In Colorado, according to the Vision Eye Health Surveillance System data from the Behavior Risk Factors Surveillance System, the percentage of people who are blind or have serious difficulty seeing, even when wearing glasses, was 2.91 % in 2018.8 Similarly, in 2019 the Vision Eye Health Surveillance System data from the American Community Survey reports the percentage of Coloradans who are blind or have serious difficulty seeing, even when wearing glasses, was 1.94 %.8
Visual impairment is known to reduce quality of life through decreasing independence, negatively impacting mobility and orientation, impacting enjoyment from leisure activities,9-11 and is also associated with cognitive decline.12 Healthcare practitioner attention and effort is primarily spent on the visual diagnosis, management of ocular disease, management of associated systemic disease, methods to maximize visual potential, and therapies to assist with vocation, independence, and transportation needs. Given the considerable clinical management, challenging visual accommodations, and extensive lifestyle modifications it is not only plausible, but likely, that the ocular comfort in patients with low vision may be neglected or at least overshadowed.
One of the primary causes of ocular discomfort is dry eye syndrome (DES)13 which was estimated by a recent meta-analysis to occur in approximately 8.1 % of the population in the United States.14 Symptoms of DES commonly include dryness, grittiness, burning, stinging, sharp pain, dull pain, foreign body sensation, tearing, photophobia, and blurred vision.15 People with DES are three times more likely to report difficulty with activities of daily life such as driving, reading, computer work, and watching television16 and have a worse quality of life compared to an age-matched normative data.17 Survey assessments have demonstrated that mild dry disease is as burdensome as mild psoriasis, while severe DES has a similar effect on quality of life as moderate to severe angina.18 DES also is known to affect visual function by worsening visual acuity, visual fluctuations, higher order light aberrations, irregular astigmatism, contrast sensitivity, and overall visual quality.19-22
Therefore, it is in the best interest of patients suffering from vision loss to mitigate ocular discomfort originating from DES to ensure quality of life is not unnecessarily diminished. Furthermore, treatment of DES may allow patients to fully utilize their remaining vision through stabilization of the tear film and corneal surface.
To our knowledge, only one manuscript has ever been published on the topic of low vision and dry eye. Researchers from Montreal, Quebec, Canada randomly selected 201 charts from their vision rehabilitation clinics and investigated symptoms of DES, systemic medications with an ocular surface dry effect, artificial tear usage, and corneal assessment (only performed in 8.95 % of patients).23 Our investigation differs as it is larger in scale and relies on a formal diagnosis of DES.
MethodsA records review was conducted on all patients seen in the University of Colorado Low Vision Rehabilitation Service between the dates of 12/1/2017 and 12/1/2022. A list of 74 ICD-10 codes consistent with DES (Tables 1a) or dryness-related ocular surface disease (Table 1b, 1c) were used to identify DES and patients were grouped into two categories as having DES or not having DES. A positive hit was determined whenever a unique patient seen in the Low Vision Rehabilitation Service had a formal diagnosis of DES with any of the 74 dryness related ICD-10 codes at any encounter in the University of Colorado Department of Ophthalmology during this five-year period. Data was further analyzed to determine the prevalence of blepharitis and meibomian gland dysfunction specifically using a list of 29 blepharitis ICD-10 codes (Table 1b) and a list of 9 meibomian gland dysfunction ICD-10 codes (Table 1c). Over 84,000 records were reviewed and there were 5164 unique patient encounters where a patient was seen in low vision who had an ICD-10 diagnosis code matching one of the 74 diagnosis codes and a total of 2572 unique patients amongst these encounters. Data were also analyzed to determine the age and sex of the patients with diagnosed DES seen in the Low Vision Rehabilitation Service.
The total number of individual patients seen in the Low Vision Rehabilitation Service at the University of Colorado during this timeframe was 2572 (n1051=male, n1521=female). Of these patients, the number of patients with a formal diagnosis of DES by an eye care professional was 978 (n332=male, n646=female). Table 2 demonstrates the number of patients with diagnosed DES by age range and sex. In the Low Vision Rehabilitation Service at the University of Colorado, the overall prevalence of diagnosed DES was 38.02 %. The prevalence of DES amongst this population varied by low vision provider and ranged from 33.37 % to 41.70 %. The prevalence of meibomian gland dysfunction was 11.90 % and the prevalence of blepharitis was 9.1 %. The distribution of DES amongst the low vision population by age range is depicted in Graph 1. The youngest patient was 17 years old while the oldest patient was 107 years old. 66.05 % of the patients with DES were female while 33.95 % were male. The prevalence of DES by age group is demonstrated in Table 3. The prevalence of DES amongst males was 31.59 % and 42.47 % for females. All patients identified as either male or female.
This study demonstrates that DES in the low vision population is a significant co-morbidity occurring in over a third of low vision patients at the University of Colorado Low Vision Rehabilitation Service. While this may be partially attributable to the climate of Colorado these numbers are significantly higher than national averages thus demonstrating that DES may be a co-morbidity affecting persons with low vision at higher rates than the general public.14 A systemic review and meta-analysis published in 2022 by McCann et al. estimated the prevalence of DES to be only 8.1 % while the prevalence was 38.02 % in our cohort.14 McCann et al. found a meibomian gland dysfunction prevalence of 21.2 % compared to our 11.9 % prevalence. One potential explanation for this discrepancy is that low vision specialists may be more likely to diagnose DES based on symptoms consistent with dry eye rather than identifying the cause of these symptoms to be meibomian gland dysfunction. This is entirely plausible as these providers are generally more focused on visual concerns rather than diagnosing ocular surface disease. Low vision specialists are also less likely to have meibography technology available to assess meibomian gland atrophy as this is not particularly relevant to their area of eye care.
Interestingly, of the only two manuscripts pertaining to low vision and DES, both investigations demonstrate evidence of a higher DES prevalence compared to the general population. Bitton et al. found 25 % of low vision patients have DES symptoms with 36.8 % regularly using artificial tears.23 Although our prevalence was determined through formal diagnosis of DES, our results more closely align with these numbers than the general population.
There are many plausible explanations as to why this population may be more susceptible to DES. Glaucoma, the leading cause of blindness worldwide,24 oftentimes requires long-term use of topical medications known to cause DES.25 Individuals with visual impairment are more likely to have had prior ocular surgery, especially cataract surgery,26 which may alter ocular surface anatomy resulting in DES.27 Another cause of visual impairment includes injury to the cornea,28,29 which may result in corneal nerve dysfunction thereby impairing blink rate and lacrimal gland secretions.30 Furthermore, visual impairment is associated with increased mental health burden and other systemic conditions (ex. hypertension),31 where the systemic treatments utilized commonly cause or worsen DES through reduced tear secretions.27 In their low vision cohort, Bitton et al. reported 30.3 % of their patients using systemic medications known to cause DES, 49.2 % having a systemic condition associated with DES, and 72.1 % with a history of ocular surgery.23
In our retrospective analysis, the prevalence of dryness increased with age which is consistent with other studies.32-34 This study also aligns with prior studies when it demonstrated that DES was also more commonly found in women as compared with men.32,35
These findings are meaningful as the ocular comfort of low vision patients should not be overlooked while managing their visual needs. Both visual impairment and DES are associated with a significant reduction in quality of life, and it is conceivable that the effect of living with both conditions may compound the reduction in quality of life.16,36 Furthermore, while visual impairment is oftentimes irreversible,37 DES is oftentimes treatable and appropriate intervention may result in improved quality of life.38
It is imperative for all professionals working with the low vision population to recognize the potential for DES and to coordinate DES management for these individuals when appropriate. Ocular comfort assessment should be performed in adjunct with typical visual function assessment to better screen for DES which may go overlooked if not specifically assessed. Questions assessing the degree of ocular discomfort may be quick and efficient methods to gain valuable insight on the level of ocular comfort in low vision patients. Additionally, short questionnaires such as the SPEED or the DEQ-5 may be utilized to formally grade the level of dry eye symptoms being experienced by a patient.39
The most obvious limitation of this study is the narrow sample of patients from only within the University of Colorado Low Vision Rehabilitation Service. One future goal is to carry forth a similar investigation with other departments of optometry and ophthalmology in the United States to compare prevalence of DES by condition as well as geographical location. We believe that this retrospective analysis is a key step in better understanding the prevalence and significance of DES within the visually impaired population at large.