To study topographic epithelial and total corneal thickness changes in myopic subjects undergoing successful orthokeratology treatment in connection with the objective assessment of contact lens decentration.
MethodsA prospective-observational and non-randomized study in 32 Caucasian myopic eyes undergoing Ortho-k for 3 months. Total, epithelial, and stromal thicknesses were studied before and after Ortho-k treatment, using optical coherence tomography with anterior segment application software. Central, paracentral, and mid-peripheral values are taken along 8 semi-meridians.
ResultsThe central average total corneal thickness was 4.72 ± 1.04 μm thinner after Ortho-K. The paracentral corneal thickness showed no significant changes (p = 0.137), while the mid-peripheral corneal thickness was increased by 3.25 ± 1.6 μm associating this increase exclusively to the epithelial plot (p<0.001). When lens centration was assessed, a lens fitting decentration less than 1.0 mm was found for the whole sample, predominantly horizontal-temporal (87.5%) and vertical-inferior (50%) decentring. Corneal topographical analysis revealed a horizontal and vertical epithelial thickness asymmetric change profile with paracentral temporal thinnest values, and mid-peripheral nasal thickest values.
ConclusionsThe present study found a central corneal thinning induced by Ortho-k lenses in subjects with moderate myopia, only associated with a change in epithelial thickness, as well as mid-peripheral thickening, that seems to be mainly epithelial in origin. The authors also found a tendency of contact lens decentration toward temporal and inferior areas conditioning an asymmetric epithelial redistribution pattern.
Orthokeratology (Ortho-k), corneal reshaping, corneal refractive therapy or vision shaping treatment is a technique to correct the refractive errors by moulding the corneal shape with the use of reverse-geometry rigid gas permeable (RGP) contact lenses (CL). Most frequently used for the reduction of myopia, Ortho-k allowed adults to be void of daytime corrective lenses. This reduction in myopia is temporary, with some regression occurring progressively throughout the day after CL removal.1-3 Different studies have found that almost 60% of myopia reduction occurs after the first overnight wear to be complete after the first week and stabilize after one month of therapy.4-6 Several studies have confirmed the safety and efficacy of overnight Ortho-k to correct myopia up to 5.0 D and corneal astigmatism up to 1.5 D.7-9
Previous studies have reported this refractive change mainly linked to epithelial thickness (ET) changes. However, there are some controversies about detailed topographic epithelial and stromal thickness (ST) changes correcting the myopic refractive error by corneal moulding involving different CL-fitting conditioning factors. Different studies report that central epithelial thinning occurs after Ortho-k lens wearing, while mid-peripheral ET or ST changes are not completely clear because global research have found different results (Table 1). Technological limitations in imaging capture and difference in important methodological aspects are probably behind this controversy. Currently, anterior segment OCT (AS-OCT), offer the possibility to high-speed capture non-contact images of the cornea with a very high axial resolution (near 3 to 5 μm), with the ability to capture epithelial and total corneal segment scans.10,11 Different authors have measured ET and ST using AS-OCT, with different Ortho-k lens designs and mainly concerning to myopic Asiatic subjects. Moreover, recent AS-OCT studies are short-term (<1 month) and only Kim study analyse long-term changes (>3 months).12
Summary of studies (including data of the present study) involving underlaying changes in corneal tissue after Ortho-k with compatible myopic refractive error. Overall, total corneal thickness decreased in the centre and increased at the mid-periphery. The lenses were manufactured with the Boston XO (AUTEK, NKL BE and OrtoK E&E Optics), Fluorosiloxanylstyrene (Menicon Z), Oprifocon A (Equalens II) and Paflufocon D (Paragon CRT) materials.
ET (epithelial thickness); ST (stromal thickness); D (dioptre); H (horizontal); V (vertical); w (women); m (men); *p<0.05.
The knowledge of the nature of the tissue changes in relation to the behaviour of the lenses allows to verify how the mobility and decentration of orthokeratology contact lenses minimizes the risk of oedema and is compatible with optimal visual acuity. Likewise, it is important to know what we measure when we analyse the data obtained when the patient is looking at the fixation point of an instrument such as the OCT or the corneal topographer. This study hypothesizes that the ET asymmetric changes determining using a modern AS-OCT can be explained by the lens decentration in Caucasian patients after 3-month Ortho-k treatment. The aim of the present study is to objectively quantify the topographical distribution of the epithelial and stromal corneal thickness in eyes undergoing Ortho-k treatment (in the long-term period) in association with the objective assessment of CL decentration.
Material and methodStudy design and subjectsTo evaluate the implications of overnight Ortho-k lens wear on corneal tissue redistribution, we conducted a prospective, observational, nonrandomized, and single-centre case series included 32 myopic eyes undergoing Ortho-k for 3 months. Sample size calculations were performed using the Epidat 3.1 software with α = 0.05 and β = 0.20 (power = 80%). Sample size estimates were calculated for each specific objective. To detect significant changes in epithelial thickness, the required sample size for 80% power is 30 subjects.
The study was performed according to the renewed and revised rules of Helsinki Declaration and was approved by the Ethics Committee of the University of Santiago de Compostela. Patients were provided an informed consent form and required to sign this document before considered for participating.
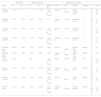
Ocular examinationAll patients underwent a complete pre-fitting examination, including routine evaluation of Snellen uncorrected distance visual acuity (UDVA), refraction, Snellen best-corrected distance visual acuity (BDVA), slit lamp biomicroscopy, corneal topography and pachymetry with particular attention to the occurrence of ocular adverse events. ET and ST data was obtained at baseline and after 3 months treatment, using the spectral-domain optical coherence tomographic 3D OCT-1 Maestro with anterior segment application (Topcon, Tokyo, Japan) using the headrest attachment. The instrument operates a fully automated alignment, focus and capture procedure, and captures 50,000 axial scans per second, producing a 20 µm lateral and 5 µm axial resolution. The epithelial and total corneal thickness was measured by an automated algorithm that detects epithelium, Bowman layer, and endothelium limits on the cross-sectional images of the cornea (Fig. 1). All OCT images were checked for correct identification of the corneal surface and the mean value from three consecutive measurements was taken for each thickness value. Quality of OCT scans were graded in three categories: “high”, “acceptable” and “unacceptable”. Only acceptable and high-quality images were processed. When possible, additional scans were taken at the operator's discretion if image quality was unacceptable or by the lack of 6 mm chord data at any of corneal locations studied. All OCT captures were performed by the same investigator, and images have been reviewed by a masked reader. OCT scans were extracted with an own programmed Python application (Python Software Foundation, Wilmington, DE) and then processed with the ImageJ software package (free software, National Institute of Health – Bethesda Softworks, Rockville, MD, USA) after calibration to the scale on the image. One measurement was manually obtained in a panel of 17 corneal locations, 1 central, 8 para-centrals at 1.5 mm (3 mm in diameter) and 8 mid-peripherals at 3 mm (6 mm in diameter) from the centre at 0°, 45°, 90°, 135°, 180°, 225°, 270° and 315°. To ensure the assessment of the thicknesses at a time of maximum corneal moudling, measurements were made between 2 and 4 h after lens removal. To minimize diurnal variations, all measurements were taken between 10:00 and 12:00.
3D OCT Maestro-1 corneal images showing corneal epithelium, Bowman's layer, and endothelium (A) with meridian selector application (B). Graphs were automatically performed and represents the epithelial thickness (microns) for the 6 mm chord corneal area before Ortho-k lens wear (C) and during treatment (D).
The present study includes 32 right eyes of 32 healthy subjects voluntarily enroled at the Ocular Surface and Contact Lens Laboratory (Lab. SOYLC) at the Universidade de Santiago de Compostela (La Coruña, Spain). The inclusion criteria involve age greater than18 years, regular corneal topographic pattern, myopia between −6.00 D and −0.75 D, no more than −1.75 D of refractive astigmatism, correctable to 20/20 or better. Exclusion criteria included previous refractive surgery, corneal diseases, other systemic or ocular diseases, use of topical medications, and insufficient OCT scan quality of the anterior segment. Due most subjects were CL wear, baseline measurements were done after the subject had a 2-week washout period without wearing their lenses, and then were fitted with the calculated Ortho-k lenses.
Contact lens and fitting procedureReverse geometry Paragon CRT lenses (Paragon Vision Sciences, Inc, Mesa, Arizona, USA) were used for 3 months. Table 2 shows CL parameters used in this study. Trial lenses were derived from nomograms in the form of sliding tables provided by the manufacturer, from the patient's refractive and topographic data. CL fit was assessed using slit lamp to ensure good movement, centration and finally to evaluate post-lens tear layer thickness profile, using fluorescein. Ortho-k lenses were fitted with apical clearance ≤10 μm and different tear thickness for the reverse zone areas with different target refractive corrections. The typical “bullseye pattern” must be present in the corneal topography after an overnight trial. A multipurpose solution (Avizor GP Multi, Avizor SA, Madrid, Spain) for RGP lenses was used to condition the lenses before storage in the lens case and physiological serum was used before CL fitting. Moreover, every 2 weeks the lenses were conditioned using a preservative free solution based on hydrogen peroxide (Avizor Ever Clean, Avizor SA, Madrid, Spain) for a more complete clean and disinfection. Cases for CL storage were replaced monthly.
Geometry reverse contact lens parameters.
FSA (Fluoro Silicone Acrylate); *(cm2/s) (mLO2) / (mL x mmHg) ISO/ANSI method, ISO 9913-1; BOZR (Back Optic Zone Radius); BOZD (Back Optic Zone Diameter); D (dioptre).
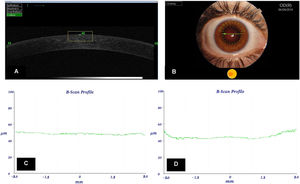
Lens misalignment was analysed with ImageJ (National Institute of Health – Bethesda Softworks, Rockville, MD) software from frames extracted with an own programmed Python (Python Software Foundation, Wilmington, DE) software. The frames have been taken from a video recorded using a Topcon DC-3 (Topcon, Tokyo, Japan) biomicroscope. Lens misalignment was captured with a narrow-slit beam (≈ 0.5 mm) at with a wide beam at x10 magnification. The frames used on current study have been the clearest just in the middle of two complete blinks with eyes always in primary gaze. Lens misalignment was measured in mm relative to zero position (pupil centre). Superior and inferior misalignment was positive and negative sign, respectively, while nasal and temporal misalignment was with positive and negative sign, respectively. Lens misalignment was averaged from 3 different measurements for each subject 3 months after Ortho-k lens wear. Finally, a masked reader conducts a second analysis to avoid bias for the study.
Statistical analysisThe Shapiro-Wilk normality test was implemented to assess all data sets for normal distribution. Data are described as mean ± SD. To compare VA and refractive descriptive statistics before and after treatment, the paired samples t-test was used. One-way analysis of variance (ANOVA) was used to compare differences amongst total, epithelial and stromal thicknesses at baseline and 3 months after Ortho-k lens wear. The relationship between VA, myopic refraction, or lens decentration and ET and ST changes were tested using simple linear regression analyses. The level of statistical significance for each parameter was set at p<0.05. The statistical analysis was carried out with the SPSS v.27.0.0.0 (IBM Corporation, Armonk NY) and Excel v.16.54 (Microsoft Corporation, Redmond WA) software.
ResultsSampleA total of 32 myopic patients (22 females and 10 males) with a mean age of 21.81±4.71 years (range; 19 to 39) were included in this study. All enroled patients completed the period planned for the study without presenting noticeable adverse events, with an average duration of Ortho-k treatment of 91.31±2.84 days.
Visual acuity and refractive changesAt baseline, the mean spherical refractive error was −2.48±1.14 D, the mean refractive cylinder was −0.37±0.35 D while mean manifest refraction spherical equivalent (MRSE) was −2.62±1.11 D. After 3-month Ortho-k treatment 32 eyes got the UDVA of Snellen 1.0 or better. VA and refractive changes found in this research are summarized in Table 3.
Visual acuity and refractive descriptive statistics (mean ± SD) for the sample at baseline and 3 months after Ortho-k lens wear. The statistical significance of change in each variable from baseline is based on post hoc t-tests. Statistical significance (p<0.05) is indicated by an asterisk.
D (dioptre); MRSE (manifest refractive spherical equivalent); UDVA (Snellen uncorrected distance visual acuity); BDVA (Snellen best-corrected distance visual acuity).
During the fitting process, all the subjects were managed to avoid any scleral interaction with the Ortho-k lens, resulting a lens fitting decentration less than 1.0 mm for the whole sample. There were 28 eyes (87.50%) showing Ortho-k lens horizontal decentration with a mean displacement of −0.31±0.25 mm, which means a trend of decentration toward temporal locations. However, only 2 eyes (6.25%) observed a nasal decentration and 2 eyes (6.25%) observed no horizontal misalignment. Mean vertical decentration was −0.03±0.15 mm, where 7 eyes (21.87%) observed no vertical misalignment, 16 eyes (50.00%) observed an inferior decentration and 9 eyes (28.13%) showing a superior decentration. Fig. 2 shows an Ortho-k lens misalignment diagram for the sample.
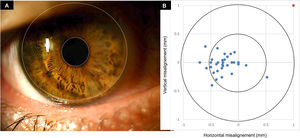
Total, stromal and epithelial thickness changesData analysis revealed central corneal thinning and mid-peripheral corneal thickening after 3-month wear of Ortho-k lenses. Table 4 summarizes AS-OCT all pachymetric data baseline and 3 months after overnight Ortho-k lens wear. This study shows a central ET decrease by −12.1% (−6.10±1.45 μm) and mid-peripheral increase by +5.5% (+2.84 ± 0.56 μm) with no significant changes in the paracentral area (3 mm chord). As shown in Fig. 3, the flattening effect of Ortho-k lens design was more evident in the temporal area (p<0.05) when compared with the nasal readings, while the mid-peripheral thickening effect appears to be stronger in the nasal locations.
Corneal thickness descriptive statistics (mean ± SD) for the sample at baseline and 3 months after Ortho-k lens wear. Values where pair-wise comparisons revealed a significant change from baseline are highlighted with an asterisk (p<0.05).
μm (microns); TT (Total Thickness); ET (Epithelial Thickness); ST (Stromal Thickness).
Corneal topography and epithelial thickness changes between baseline (left) and after 3-month Ortho-k treatment period (right). Data of corneal location showing significant differences (p<0.05) appear in bold. Note the stronger central and temporal epithelial thinning, and highest mid-peripheral thickening corresponding to nasal area in clear association with temporal decentration observed in this study.
When correlation analysis was made, the magnitude of change in central ET was positively associated with a change in mid-peripheral ET (R2=0.876; p<0.007). The decrease in central total and ET showed a significant correlation with UDVA and the magnitude of myopia correction (Table 5). The association of vertical lens decentration with changes in central ET or ST was weak for all corneal locations. However, a significant positive correlation (p<0.05) was found between horizontal lens decentration and mid-peripheral nasal and superior ET, while a negative correlation was found between horizontal lens decentration and mid-peripheral temporal ET (Table 6). Stromal thickening in the paracentral area showed no significant association with lens decentration, post Ortho-k UDVA or refractive change.
Correlation between refractive error, UDVA and corneal layers change after 3-months of Ortho-k lens wear. Statistical significance (p<0.05) is indicated by an asterisk.
| Myopia Correction | UDVA | |||
|---|---|---|---|---|
| Changes | R2 | P | R2 | P |
| ET central (μm) | 0.410 | <0.001* | 0.365 | <0.001* |
| ET Cord 3 mm (μm) | 0.093 | 0.171 | 0.038 | 0.103 |
| ET Cord 6 mm (μm) | −0.037 | 0.568 | 0.236 | 0.085 |
| ST central (μm) | 0.269 | 0.125 | 0.178 | 0.243 |
| ST Cord 3 mm (μm) | −0.191 | 0.093 | −0.033 | 0.102 |
| ST Cord 6 mm (μm) | 0.154 | 0.112 | 0.007 | 0.428 |
μm (microns); TT (Total Thickness); ET (Epithelial Thickness); ST (Stromal Thickness); UDVA (Snellen uncorrected distance visual acuity).
Simple linear regression between horizontal lens decentration and epithelial thickness changes. Statistical significance (p <0.05) is indicated by an asterisk.
| Magnitude of Lens decentration (mm) | |||||
|---|---|---|---|---|---|
| Factor | r | R2 | B | β | P |
| Epithelium Change | |||||
| Central | 0.168 | 0.090 | −0.062 | −0.271 | 0.523 |
| Paracentral Nasal | 0.336 | 0.017 | −0.197 | −0.438 | 0.126 |
| Paracentral Temporal | −0.471 | −0.317 | −0.114 | −0.591 | 0.017* |
| Paracentral Superior | 0.415 | 0.058 | −0.544 | −0.201 | 0.275 |
| Paracentral Inferior | −0.288 | −0.027 | −0.009 | −0.078 | 0.321 |
| Mid-peripheral Nasal | 0.808 | 0.421 | −0.189 | −0.653 | 0.009* |
| Mid-peripheral Temporal | −0.322 | −0.029 | 0.008 | 0.093 | 0.106 |
| Mid-peripheral Superior | 0.725 | 0.123 | −0.612 | −0.299 | 0.040* |
| Mid-peripheral Inferior | −0.393 | −0.010 | 0.005 | 0.079 | 0.081 |
CCT changes induced by overnight Ortho-k have been well documented and have been found limited to the epithelial layer, while changes in the mid-peripheral corneal thickness present some controversy in relation with the stromal contribution (Table 1).7,13-18
This study found that total thickness changes responsible of the orthokeratological effect were mainly epithelial in origin which agrees with different authors using high resolution technology.12-18 Alharbi and Swarbrick using an optical pachymeter reported that mid-peripheral thickening was stromal in origin.7 It is likely that main discrepancy on peripheral thickness is due to the method used to measure ET and ST, and the fact that only five corneal locations across the horizontal meridian were measured. Haque et al., using the Humphrey OCT-2, also found certain degree of mid-peripheral stromal thickening although the magnitude of stromal changes was less than epithelial ones, mainly in the lower Dk lens group and only for 1 night.14 Kim et al., also found certain degree of central, paracentral and mid-peripheral stromal thickening but less than found by Haque´s group and less than epithelial changes.12 Recently Zhang et al. in their study found the epithelial thinning as the major contribution to the central corneal thickness effect induced by the reverse base curve of the CL, but at 1 month of Ortho-k treatment the thickness of central stroma was significantly lower than baseline values suggesting some amount of deep compressive stress in this area.18 The difference between studying the effect at one night, one or three months can clarify up to when there may be stromal changes and if from a certain moment there are no more, as seems to occur in our study.
On the epithelial thinning (central) and thickening (mid-peripheral)The epithelium is the most malleable corneal layer with a low elastic modulus, which means it is easy to deform.19 A decrease in central ET has been well documented in myopic subjects wearing Ortho-k lens of different brands and using different methods (Table 1), being the compressive effect of the Ortho-k lens designs against the central epithelial layer the main reason. However, the mechanisms behind the epithelial thickening in the mid-periphery are unclear. Molecular analysis of tear samples from Ortho-k lens wearers revealed increased levels of metalloproteinase MMP-9 and epidermal growth factor (EGF), mediators involved in the cellular redistribution mechanisms linked to the reparative corneal response.20 In this sense, the orthokeratological effect initiated by the reverse curve of the Ortho-k lens, may well be in nature, a process of epithelial redistribution from the centre or the limbus to the CL reverse zone area causing the epithelial thickening in the mid-peripheral cornea. Another contribution may be an epithelial deformation caused by negative pressure exerted by the reverse curve zone on the mid-peripheral area.21-26 These phenomena should be also supported by a decreased rate of desquamation because of the Ortho-k lens design that may provide for cellular and tear stasis at the mid-peripheral cornea.24 Central and mid-peripheral epithelial values found in this study agree with these observations. Further work is necessary to elucidate the nature of the cellular events underlying the ST and ET changes associated with Ortho-k treatment.
On the stromal thickening or notStudies in animal models reported no modification in stromal collagen metrics during Ortho-k, attributing the refractive improvement only to the epithelial changes.25,26 However, in humans, some studies found stromal thickening which nature is not clear. Holden and Merz suggested that a Dk/t of 87 is necessary to prevent overnight hypoxia and thus stromal swelling induced by the CL.27 Alharbi et al. reported that central pressure exerted by the flat-fitting base curve of the Ortho-k lens and the mechanical pressure from the eyelid acts locally as a "clamp" to inhibit overnight central corneal swelling, while certain levels of corneal oedema, consistent with CL Dk/t, can be observed in the mid-periphery using a modified optical pachymeter.28 Other studies have found different amounts of mid-peripheral stromal thickening but not attributed to overnight corneal oedema, but to the same effect of negative pressure behind the CL reverse curve causing epithelial and stromal tissue redistribution.12,14 In the present study, only a trend of stromal thickening (+3.85%) have found in the paracentral area (3 mm chord), which is in agreement with other authors who found no mid-peripheral stromal changes.15 A potential source of this controversy is the time of measuring after lens removal. In the present study, we measured at least 2 h after lens removal, justifying the absence of significant stromal oedema. Haque et al. measured ET and ST after 1, 3, 6 and 12 h of less removal showing that the oedema with the highest Dk/t lens is appreciable within 3 h.14 However, recently Zhang et al. found a −3.7% decreased ST, measuring corneal thickness 2 h after lens removal in a 1-month period suggesting some degree of global compression.
On the epithelial asymmetric redistributionThe present study also noted different ET changes along the horizontal and vertical meridians. Topographic pachymetry graphs revealed more epithelial thinning in temporal mid-periphery than found in nasal areas and in the superior zone while no thickening appears in the inferior area which disagrees with some previous studies.13,16,17 ET asymmetry in CL wearers had been previously described in long-term wearers of low-Dk soft CL, with chronic superior oedema being the likely aetiology.28 Wang et al. found more compression in nasal zones in an overnight study in a more myopic Asiatic population with different palpebral implications, using the 1st generation Humphrey OCT, and no data of CL decentration were reported that appear to be the more reasonable explanation. Lian et al. have found no differences in nasal and temporal thickening and found the same superior and inferior epithelial thickening in an Asiatic sample for 1 week. However, horizontal differences found in this study is in good agreement with a recent study using similar technology, but our study revealed vertical differences with epithelial thickening only in the superior zones whereas Kim et al. found more epithelial thickening in the inferior location using the same CL and OCT technology.12 These differences may be due to variations in the eyelid pressure acting in different eye regions or due to different lens-on-eye decentrations amongst individuals.16-18
CL decentration effectDuring the night, the Ortho-k lenses are relatively restricted and fixed to the more curved region of the cornea. However, low to moderate CL decentration is common despite a successful fitting process, but in most cases, the amount of decentration is moderate and acceptable. Recently, it has been proposed different predictors of CL decentration in Ortho-k wearers.29,30 Corneal topography, corneal and ocular aberrations, as well as the geography of corneal tissue redistribution induced by Ortho-k could be influenced by lens fitting decentration.12,31,32 In this study we found a tendency of CL decentration toward temporal and inferior areas, which agrees with previous studies.12,33,34 The main reason for this tendency may be that the temporal corneal shape is commonly steeper than the nasal one, and the lenses tended to drift to the steeper side.29,35 So, the asymmetric compression pattern observed in this study, can be attributable to inherent Ortho-k effect on asymmetric corneal surface.36 Simple linear regression analysis showed that there was no association between vertical lens decentration and regional ET or ST changes, but there was association between post Ortho-k ET and the magnitude of horizontal lens decentration. The magnitude of horizontal decentration was positively associated with change in mid-peripheral ET (nasal and superior) and negatively associated with change in mid-peripheral temporal ET. A reason of this meridional difference is that vertical Ortho-k lens decentration was usually smaller than the horizontal, probably due to the CL can be supported by the vertical corneal limbus and lids limiting vertical decentration. Therefore, horizontal decentration conditions lower ET values at the temporal 3 mm chord, as well as less increased values in the temporal 6 mm chord locations corresponding with the inner limit of the reserve zone of the CL. On the other hand, this decentration conditions higher values in the nasal 3 mm chord and an apparent greater increase in ET in the nasal 6 mm chord locations, which in the cases of greater lens decentration, fully correspond to the reserve zone area of the Ortho-k lenses (Fig. 3). Thus, we can affirm that for a better monitoring redistribution of corneal tissue in subjects undergoing Ortho-k, it would be desirable to have instruments that allow an automated larger analysis area, covering at least the central 8 mm of the cornea, which is no possible with most of the current AS-OCT systems.
LimitationsThis study has several limitations. First, the AS-OCT defined ST as total corneal thickness minus ET. Thus, ST in this study included the Bowman, Descemet, and endothelium. Second, the epithelial or stromal contribution had been determined using a fixed corneal location panel to compare the baseline and the Ortho-k treatment corneal thickness. Results found in this study shows that everyone had a difference reshaping area, ranging 4 to 7 mm, although the base curve zone design of the lens is 6 mm. Thus, the reshaping area was not always in the central cornea, with different degrees of decentration in this sample. Therefore, the reverse curve area may fluctuate in the paracentral and mid-peripheral corneal zones as described above. In the bibliographic review carried out in this research, only one study monitored the characteristics of ET redistribution on the corneal areas affected topographically by the Ortho-k treatment.18 Consequently, the authors found a similar epithelial thinning and a notably greater mid-peripheral epithelial thickening, since the values obtained were determined from the mean of the ring corresponding to the base curve or from the reserve area of the lenses respectively. Another limitation has to do with the fact that the OCT used does not provide automatic peripheral thickness values, being necessary the use of the calliper tool for the measurement of the topographic thicknesses. As far as the authors have reviewed, this is one of the few studies where this is done with an OCT that does not provide the values automatically.37 Assuming the greater versatility of the new automatic OCTs, it is interesting to know that previous generation OCTs can be used to perform these measurements but spending a longer amount of time.
In conclusion, this study shows that Ortho-k corneal thinning in subjects with moderate myopia, is only associated with a decrease in ET, with a stronger effect in the temporal side. Likewise, mid-peripheral thickening seems to be only associated with an increase of the ET, showing a stronger effect at the nasal locations. A correlation was found between the VA and refractive parameters with changes in ET, while ST changes do not appear to have any association, therefore, refractive changes induced by Ortho-k in the long-term period can be explained entirely by the epithelial redistribution. Since measurements were made taking as a reference the centre of the cornea, lens decentration conditioning a moderate asymmetric epithelial redistribution pattern characterized by a thinner paracentral temporal and thicker mid-peripheral nasal ET values.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The authors declare that they do not have any proprietary or financial interest in any of the materials mentioned in this article.