To analyze binocular vision of individuals aged 18 to 35 years diagnosed with keratoconus, utilizing spectacles and rigid gas-permeable (RGP) contact lenses. Research was led by the Universidad Autónoma de Aguascalientes, México and Fundación Universitaria del Área Andina Pereira, Colombia.
MethodsA single center, prospective non-randomized, comparative, interventional, open-label study, in which the differences in binocular vision performance with both spectacles and RGP contact lenses was carried out from December 2018 to December 2019. Sampling was performed according to consecutive cases with keratoconus that met the inclusion criteria until the proposed sample size was reached.
ResultsRigid gas-permeable (RGP) contact lenses notably enhanced distance and near visual acuity in keratoconus patients compared to spectacles. Visual alignment analysis shows exophoria at both distances and is slightly higher with RGP contact lenses. The difference was statistically significant (p<0.05), with 82.5 % presenting compensated phoria with spectacles and pnly 42.50% with RGP contact lenses. Stereoscopic vision improved while wearing RGP contact lenses (42.59 %), although accommodation and accommodative flexibility remained within normal ranges.
ConclusionsPatients with keratoconus fitted with RGP contact lenses have improved binocular vision skills such as visual acuity, stereopsis, and accommodative flexibility. However, even when the vergence and motor system is decompensated with respect to normal ranges, the range between break and recovery points for both fusional reserves and the near point of convergence (NPC) improves with the use of RGP contact lenses, giving indications of an adaptive condition of the motor system from the medium to the long term.
Keratoconus is a corneal ectasia characterized by steepening corneal curvature, changes in refractive error and corneal thickness that results in visual impairment.1 According to Gomes et al. (2015), keratoconus appears between 10 and 30 years of age, usually progressing in the first 10–15 years, while eventually stabilizing after 40 years.2
The incidence of keratoconus ranges from 50 to 230 per 100,000 in the general population, which is approximately 1 in 2000 people; 6–8 % of all cases are due to heredity.2 A majority of keratoconic patients (74 %) can be treated using RGP, hybrid, miniscleral or scleral contact lenses, while the remaining percentage (26 %) are treated with surgical management.3
Binocular vision in patients diagnosed with keratoconus becomes a critically important aspect when considering the two optical correction alternatives: spectacles and RGP contact lenses.4 While the use of RGP contact lenses can offer a significant improvement in binocular vision, it is essential to recognize that the transition from spectacles to RGP contact lenses may introduce discomfort and additional challenges related to binocular vision. These challenges may manifest in the form of accommodative problems, vergence issues, and phoria decompensations, which add a fundamental dimension to the evaluation of the effectiveness of visual correction alternatives.
The critical importance of conducting a comprehensive assessment of binocular vision in patients with keratoconus is underscored when considering the switch between spectacles and RGP contact lenses as optical correction options. Any alteration in this capacity can result in uncomfortable symptoms and reduced visual quality.
In Lovasik's study, it was found that the degree of aniseikonia and anisometropia caused a reduction in stereopsis. It is already known that patients with keratoconus typically have different visual acuity in each eye which can alter stereopsis. For that reason, the use of RGP contact lenses is beneficial as it reduces aniseikonia.5 Previous studies have concluded that with the use of RGP contact lenses, keratoconus patients improve their stereoacuity as wave-front aberrations are decreased. 5Similarly, the use of RGP contact lens improves the quality of retinal images facilitating good fusion. As a result, there is a better perception of depth or stereopsis.6
In Nilagiri's investigation, it was also found that there is greater precision in vergence when RGP contact lenses are used.7 Even so, in the search for literature, there are no studies that have shown a full comparison of binocular vision in patients with keratoconus when using RGP contact lens and spectacles. The objective of this research was to analyze and compare binocular vision, both in the sensory and motor aspects, in patients with keratoconus when using spectacles and RGP contact lenses.
Material and methodsStudy sampleA single center, prospective non-randomized, comparative, interventional, open-label study was conducted in the Medical Didactic Unit at the University of Aguascalientes, México, and at the University Foundation of Andean Area Pereira, Colombia. The study was carried out from December 2018 to December 2019. Sampling was performed according to consecutive cases with keratoconus that met the inclusion criteria until the proposed sample size was reached. Exclusion criteria were patients with eye disorders, such as strabismus or corneal leukoma. The study was reviewed and approved by the Human Research Ethics Committees at both previously mentioned universities. All research was conducted in accordance with the Declaration of Helsinki with all participants providing informed consent. The study's participants were patients diagnosed with bilateral keratoconus, older than 18 years, who had not received any keratoconus or strabismus surgical treatment or visual therapy.
Visual function evaluationThe diagnosis and classification of keratoconus was made based on the Amsler Krumeich scale and standard clinical topographic and tomographic features7,8,9 obtained from corneal topography with the Pentacam system (Oculus Optikgeräte GmbH; Wetzklar, Germany). Eligible participants underwent a complete ophthalmological examination, including measurement of best-corrected distance visual acuity using a Snellen chart (Carl Zeiss Meditec AG, Jena, Germany, version 5.4.4.0006), measurement of stereoacuity at 40 cm using the Randot Stereoacuity test (Stereo Optical l, Inc., Chicago, USA), and a detailed slit-lamp examination (LS Ophthalmic Slit Lamp; ChongQing Medical Sunkingdom Medical Instruments Co., Ltd., ChongQing, China).
Refractions were carried out by three different optometrists at the same distance (6 m), and the same illumination conditions. Manifest refraction was based on subjective refraction in a Topcon Phoropter VT-SE (Topcon Inc., Tokyo, Japan) and the visual acuity at distance. The duochrome test and Jackson's cross cylinder for axis and power test were used to prevent under or over corrections. Manifest refraction was recorded to the nearest 0.25 D with the visual acuity recorded. All eyes were fitted with corneal rigid gas permeable (RGP) contact lenses (Fluoroperm-90 DK value of 90 (cm/s) ([mL O2/mL. mmHg]).
All the tests were performed first with the patients using spectacles and then while using RGP contact lenses. Visual acuity (VA) was measured at 6 m and 40 cm, performed monocularly and then binocularly; the value of the VA was recorded in decimal scale. The eye with better and worse best-corrected distance visual acuity wearing RGP contact lenses and spectacles was termed the ‘better’ and ‘worse’ eye, respectively.
Binocular vision assessmentThe vertical and horizontal visual alignment was evaluated using the modified Thorington method.10 The fusional reserves (FR) were evaluated with the jump vergence test (using a horizontal prism bar and gradually increasing the prism power—internal base or external base—until double vision was reported), reporting two points: break (Br) and recovery (Re).10 The accommodative amplitude (AA) was determined using the push-up method.11
The accommodative facility was evaluated both: binocularly and monocularly, using a reading card and flipper with a power of ±2.00 D. Results were reported in cycles per minute (cpm).12
The near point of convergence (NPC) was assessed using accommodative and non-accommodative targets, measuring break and recovery points in centimeters (cm) for each. The assessment began with the stimulus positioned 40 cm away from the patient, using as stimulus the letter H (0.1 M VA) for accommodative NPC and red filter and a hand lamp for non-accommodative NPC. The distances for each test in cm for the two measuring points were recorded.13 Stereopsis was evaluated with a Randot test at a distance of 40 cm.14 The results were reported in seconds of arc.
To perform the contrast sensitivity test, the Functional Acuity Contrast test (F.A.C.T.® 301, Stereo Optical, Chicago, IL) was chosen.15 This was located at 3 m and was illuminated between 68 and 240 cd/m2. The test was performed with RGP contact lenses and spectacle correction for each eye. The results were evaluated by the Snellen Functional Acuity Equivalent and distributed by percentage according to their stereopsis.
Data analysisCentral tendency measures were used for data analysis, conducted using IBM SPSS Statistics version22.0for Windows (IBM Corp., Armonk, N.Y., USA). The Shapiro–Wilk test assessed the normality of continuous data. Nonparametric statistical tests, including descriptive analysis and the Student's t-test for related samples, were employed for variables such as visual acuity: (VA), heterophoria, fusional reserves, accommodation, sensory aspects, and stereopsis.
The statistical significance threshold was set at P<0.05. Results were presented as mean and standard deviation with a p-value for independent samples t-test or median and range with a p-value for the Mann-Whitney test.
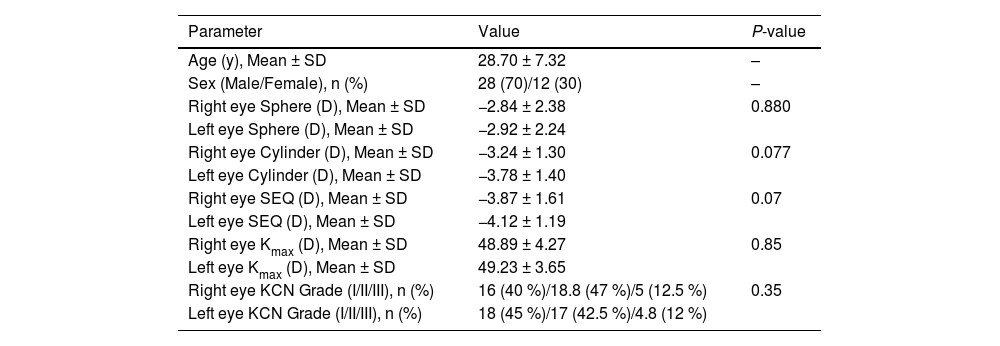
ResultsForty subjects with diagnosis of keratoconus were included. The mean age of the participants was 28.70 ± 7.32 years. There were 28 men (70 %), and 12 women (30 %) in the group.
First, the refractive state was determined for each eye. Table 1 describes the values found. It can be observed that in all the variables studied the values are higher for the left eye, although the difference was not statistically significant. The degree of keratoconus in 80 % of cases in both eyes corresponded to grades I and II.
Demographic, refractive error, and keratometric parameters of study participants with asymmetric bilateral keratoconus.
Abbreviations: y, years; SD, standard deviation; n, number;%, percentage; Sphere, spherical component of refractive error; D, diopter; Cylinder, cylindrical component of refractive error; SEQ, spherical equivalent of refractive error; K, maximum keratometry reading; KCN, keratoconus. P-value: for comparing the right and left eyes.
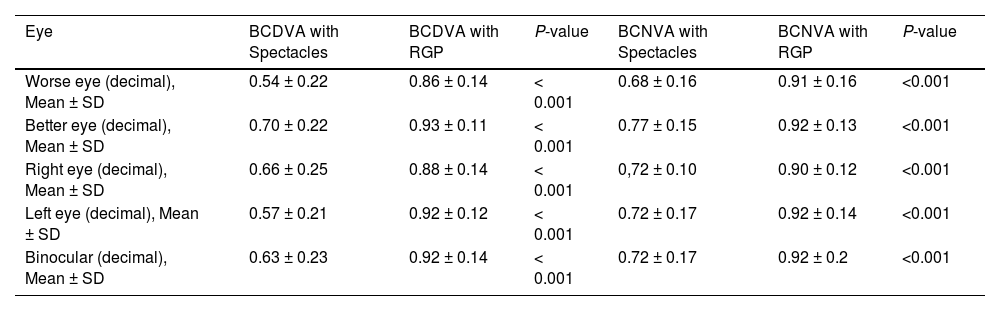
Visual acuity was evaluated for distance and near vision. A better visual acuity was obtained with RGP contact lens compared to spectacles. The difference between the best and worst eye acuity was greater with spectacles at distance vision. These differences were statistically significant (p<0.001) and the values can be seen in Table 2. All values were compared by mean difference through Student's t, with a significance level of *(p<0.05)
Comparison of best-corrected distance or near visual acuities between eyes of study, participants with asymmetric bilateral keratoconus.
Abbreviations: BCDVA, best-corrected distance visual acuity; BCNVA, best-corrected near visual acuity; RGP, rigid gas permeable contact lens; SD, standard deviation. P-value: for comparing between corrected visual acuity with spectacles versus RGP. Note: P-values <0.05 are shown in bold; worse eye, the eye with a worse best-corrected distance visual acuity; better eye, the eye with a better best-corrected distance visual acuity.
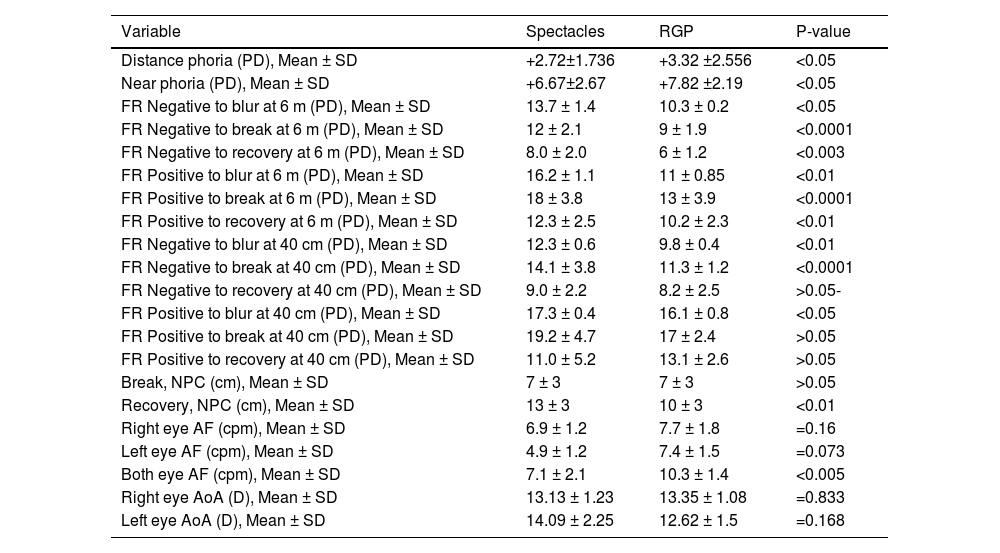
Determined with the Thorrington test in distance and near vision, the mean magnitude of the deviation shows an exophoria at both distances and was slightly higher with RGP contact lenses. This difference was statistically significant (p<0.05) (Table 3).
Comparing phoria and binocular vision parameters between spectacles versus RGP contact lens correction.
Abbreviations: RGP, rigid gas permeable contact lens; PD, prism diopters; SD, standard deviation; m, meters; FR, fusional reserve; cm, centimeter; NPC, near point of convergence; AF, accommodative facility; cpm, cycle per minute; AoA, amplitude of accommodation; D, diopters. P-value: for comparing between corrected visual acuity with spectacles versus RGP. Note: P-values <0.05 are shown in bold.
Positive fusional vergences (PFR) and negative fusional vergences (NFR) were evaluated at far and near distances. Values of blur, break, and recovery were reported. The mean of the values obtained were significantly higher with spectacles compared to RGP contact lenses (p<0.001) Regarding fusional reserves, the criteria of León et al. were followed: negative fusional reserves (NFR) 10/6, 14/10 and positive fusional reserves (PFR) 20/16, 30/22.
Sheard's criterion postulates that "for a subject to have comfortable binocular vision, the value of the fusional reserve must be at least twice the demand; in this sense, phoria would be considered compensated with fusional reserves”.16 Based on the above statement, 82.5 % of patients evaluated presented compensated phoria with spectacles; however, with RGP contact lenses there was only 42.50 % of patients preserving this compensation. (Table 3)
The NPC was also evaluated with results expressed in centimeters. At break point, similar values were recorded with spectacles and RGP contact lenses, however, at recovery point, the value with spectacles was significantly higher (p<0.01). (Table 3). Based on Leon et al., the results are within the normal values with spectacles and RGP contact lenses.
AccommodationAccommodative flexibility was determined for each eye, and the results showed higher values with RGP contact lenses for both eyes. The amplitude of accommodation was slightly higher in the right eye and lower in the left eye with RGP contact lens than with spectacles. These differences were, however, not statistically significant (p>0.05).
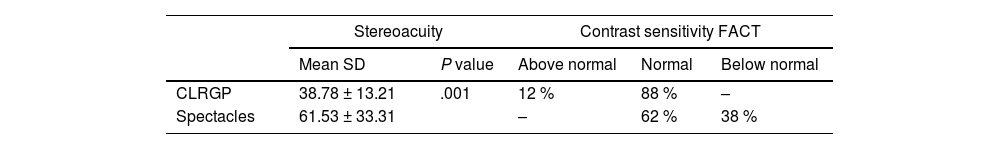
StereoacuityTable 4 shows the stereoacuity comparing the use of contact lenses to spectacles, with the results being greater when using contact lenses (P<0.001). Likewise, it shows the percentages of contrast sensitivity based on those that are above normal on the normal scale and those who are below normal. The data were analyzed by difference in means with Student's t.
DiscussionThe results of the present investigation show a significant improvement in visual acuity with the use of RGP contact lenses instead of spectacles. As it can be seen in the visual acuity table (Table 1), visual acuity in distance and near vision was better with the use of RGP contact lenses.8 The results are consistent with those found by other authors, like Saraç Ö et al., who stated that keratoconus caused refractive changes due to an increased irregular astigmatism with the evolution of corneal ectasia. This astigmatism is non-orthogonal, which makes correction with spectacles ineffective, not offering satisfactory optical results in the more advanced stages of the disease, and making the use of RGP contact lenses the best option for visual rehabilitation.18
Nilagiri et al. mentioned that the logMAR visual acuity of the affected eye improved significantly when switching from best corrected spectacles to RGP contact lenses. The mean interocular difference in logMAR acuity (p = 0.008) and the intersubject variability of binocular logMAR acuity were also reduced with the use of spectacles compared to RGP contact lenses.17
Ana Marta et al. evaluated 96 eyes fitted with RGP contact lenses, hybrid contact lenses (HCL), and hydrogel/silicone hydrogel contact lenses (HGCL) and found that the mean visual acuity of both eyes with contact lenses was better than the visual acuity in both eyes obtained with spectacles (p<0.001). It was also identified that the dynamic optical quality showed statistical differences, being better for the RGP contact lens wearer group".18
Regarding binocular vision, it was expected that visual skills would be better with contact lenses, due to the values obtained in visual acuity. However, the results showed that not all skills improved when using RGP contact lenses, particularly exophoria which was decompensated with the use of RGP contact lenses in some cases. This was probably due to an existing binocular vision deficiency such as hypercorrection and/or partialization of ametropia, as suggested by the Optometric Practical Manual with the purpose of improving VA and tolerance.18
In that sense, one of the elements for the determination of the state of binocular vision is Sheard's criterion where a phoria is considered compensated if the fusional reserve is at least twice the value of the phoria, a very low value of vergence recovery suggests a slow response and lower amplitude which is not sufficient for a sustained near vision. A difference greater than 7∆ between the value of fusion break and the value of recovery may explain the presence of asthenopia due to the difficulty in restoring binocular vision. According to Morgan's criteria, the recovery should be half of the break value in far and near vision at least in 65 % of the break values.19
In this study, when evaluating fusional reserves with respect to the phoric state and comparing the variations with spectacles and RGP contact lenses, it was found that both reserves have lower values with RGP contact lenses than those found with spectacles. According to Prentice's law, with spectacles, a prism is induced in near vision by reduction of the pupillary distance versus the mechanical distance of the lens. The prism induced internal base in a negative lens, favoring the compensation of an exophoria, and therefore this would explain the results obtained, with an increased exophoria with contact lenses. However, these coherent trends are contradicted in the present study showing the opposite behavior.19
Antona et al. analyzed the refractive defect with respect to the direction and magnitude of the phoria where in myopic subjects the phoric results were slightly but insignificantly higher, not being a significant value. Likewise, the difference between the values of break and recovery in 47.5 % of subjects presented a difference equal to or greater than 8∆. It should be considered that different authors20 have reported that a tolerance range of 6.5∆ is associated to greater difficulty in restoring binocular vision with spectacles. In contrast to the tolerance range with RGP contact lenses, our results showed an average of 4.0∆, even though fusional reserves tend to decrease in amplitude with RGP contact lenses. Therefore, the difference between break and recovery points was improved, suggesting that there was better ability in restoring binocular vision.21
A higher value of heterophoria was found in this study with the use of RGP contact lenses, as well as a lower amplitude in fusional reserves and a better fusion recovery, although an increase in the number of cases with decompensated phoria was also observed with the use of RGP contact lenses. Prentice's law explains the increase in phoria when using RGP contact lenses where the induced prism is eliminated both horizontally and vertically in near vision. The imbalance between break and recovery points with spectacles was dependent on the magnitude of the ametropia, since the greater the range of the ametropia the greater the induced prismatic effect. In the case of exophoria and negative optical correction, an internal base induced prism can be induced, which can partially or totally compensate for an exophoria, resulting in a smaller angle of deviation.22
In the study by Raimundo Jimenez et al., a dissociated phoria (esophoria) and lower negative fusional vergence in near vision were found with the use of RGP contact lenses. Contrary to that, in our study, there was a greater magnitude of exophoria and lower values for positive fusional reserves with RGP contact lenses, and according to the Sheard's criteria, this means that there would be a decompensation of phoria. These data can be explained with the results found by Arcot et al.,14 in which they compared two groups, one with a diagnosis of keratoconus and a control group. The presence of exophoria of greater magnitude was frequently found in keratoconus that sometimes evolved to an intermittent strabismus, and where the positive fusional reserves were considered low due to the relaxation of accommodation, with respect to the control group. Additionally, it is mentioned that the binocular condition can be compensated after some months of RGP contact lens adaptation.6 The variations in fusional reserves can be attributed to the relaxation of accommodation when the exophoria tends to increase, for this reason the patient must use the scarce near vergence reserve to compensate for the higher convergence demand. Regarding the results obtained in the accommodative and non-accommodative NPC, the values of break and recovery obtained with the use of RGP contact lenses were closer and the difference between break and recovery was smaller with CL, which suggests that when using RGP contact lenses, the fusional vergence is activated and supported by accommodation, as stated by Duckman.23 Exophoria compensated with the prism induced by a real object proximity stimulus (accommodative) while using spectacles required a greater vergence effort. This caused a slow fusion break at the near convergence point, while at the near point with light (non-accommodative) only the fusional vergence is activated but not the accommodative vergence.24
This study showed stereopsis was better with contact lens correction and worse when the patients used spectacles. In this sense, the contrast sensitivity in more subjects was below normal, being similar to those found in subjects with lower stereopsis. These results are consistent with those reported by Goodwing and Romano, and also by Nilagiri et al., finding a highly significant improvement in stereoscopic visual acuity when switching from spectacles to RGP contact lenses. This is explained by one of the main factors for the loss of stereopsis; 50 % of the study subjects had different degrees of keratoconus in each eye leading to probable aniseikonia.25
Hunt et al. conducted a study on the ocular motor triad in subjects with RGP contact lenses compared to spectacles. It was concluded that when a myopic patient uses monofocal contact lenses, they have a greater accommodative demand, which translates into a greater accommodative effort. The results of the present study do not coincide with the latter; although no significant differences were found in the accommodative amplitude. The results for the left eye are striking as a difference of close to 1.50 D is shown to be lower with contact lenses. This is confirmed by Raimundo Jiménez et al., who found a definite tendency towards a worse accommodative and vergence function in contact lens wearers. So, it is possible argued that myopic under correction favors accommodative demand leading to lower accommodative amplitude results.26
In terms of accommodative flexibility in this study, the values remained within normal ranges both with the use of RGP contact lenses and the use of spectacles.
ConclusionThe present study has shown that keratoconus patients fitted with RGP contact lenses improve binocular vision skills such as VA, stereopsis, and accommodative flexibility. However, other elements such as fusional reserves and phoria may decompensate with the use of RGP contact lenses. Even when the vergence and motor system is decompensated with respect to normal ranges, the difference between break and recovery points for both fusional reserves and NPC improve with the use of RGP contact lenses, suggesting that there is an adaptive condition of the motor system from the medium to the long term.