To report long-term outcomes of strabismus surgery for treatment of third nerve palsy.
MethodsWe performed a 15-year retrospective study of patients who had undergone surgery. We analyzed preoperative mean deviation (at 6 months, 1 year after surgery, and at the end of follow-up), type of surgery, and factors predicting outcomes. A final deviation <10 prism diopters (pd) was considered a good esthetic outcome, and no diplopia in the primary position at the end of follow-up was considered a good functional outcome.
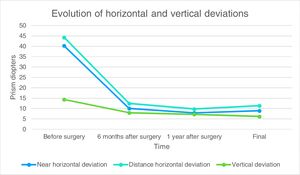
ResultsSurgery was performed in 31 cases. Mean age was 36.27 years (women, 51.6%). Total and complete third nerve palsy was recorded in 22.6% and acquired palsy in 80.6%. Mean preoperative horizontal deviation (HD) in primary position was 40.24pd (near) and 44.29 (distance) and 14.33pd in vertical deviation (VD). Mean final HD was 8.94pd (near) and 11.35pd (distance), and mean final VD was 6.13. One surgery was performed in 68.9%. A favorable esthetic outcome was obtained in 64.5% and a successful functional outcome in 72.2%. Statistically significant differences were found between near HD (p=0.019) and distance HD (p=0.035) at 1 year compared with the end of follow-up and between VD at 6 months and 1 year after surgery (p=0.03). Mean follow-up was 6.05 years. No specific factors predicted a successful outcome.
ConclusionsEsthetic and functional results were similar. No predictors of successful outcome were identified. HD was better 1 year after surgery, and VD improved during follow-up.
Reportar los resultados a largo plazo de la cirugía de estrabismo para tratar la parálisis del III par.
MétodosRealizamos un estudio retrospectivo a 15 años, de pacientes sometidos a cirugía. Analizamos la desviación media preoperatoria (a 6 meses, 1 año tras la cirugía, y al final del seguimiento), el tipo de cirugía, y los factores predictivos de los resultados. Se consideró un buen resultado estético una desviación final <10 dioptrías prismáticas (pd), y un buen resultado funcional la ausencia de diplopía en la posición primaria al final del seguimiento.
ResultadosSe practicó cirugía en 31 casos. La edad media fue de 36,27 años (mujeres, 51,6%). Se registró parálisis total y completa del III par en el 22,6% de los casos, y parálisis adquirida en el 80,6%. La desviación horizontal preoperatoria media (DH) en posición primaria fue de 40,24pd (de cerca) y 44,29 (de lejos), y 14,33pd en desviación vertical (DV). La DH final media fue de 8,94pd (de cerca) y 11,35pd (de lejos), y la DV final media fue de 6,13. Se practicó cirugía en el 68,9% de los casos. Se obtuvo un resultado estético favorable en el 64,5% de los casos, y un resultado funcional exitoso en el 72,2%. Se encontraron diferencias estadísticamente significativas entre DH de cerca (p=0,019) y de lejos (p=0,035) a 1 año, en comparación con el final del seguimiento, y entre DV a 6 meses y 1 año tras la cirugía (p=0,03). El seguimiento medio fue de 6,05 años. Ningún factor específico predijo un resultado exitoso.
ConclusionesLos resultados estético y funcional fueron similares. No se identificaron factores predictivos de un resultado exitoso. DH fue mejor 1 año tras la cirugía, y DV mejoró durante el seguimiento.
Third cranial nerve palsy accounts for one third of all cranial nerve palsies.1 It is also the most difficult paralytic strabismus to be treated from an esthetic and oculomotor point of view,2–4 because the third nerve innervates 4 extra-ocular muscles: the medial rectus (MR), superior rectus, inferior rectus, and inferior oblique. The third cranial nerve also innervates the levator palpebrae superioris, the ciliary muscle, and the constrictor muscle of the pupil.5
Third nerve palsies can be complete or incomplete, total or partial, and congenital or acquired.5,6 In complete palsy, the eye is in exotropia, hypotropia, and cyclotorsion, with limitation of adduction, elevation, and depression. Ptosis and pupillary mydriasis are associated clinical findings, especially in acquired palsies due to trauma and space occupying lesions.7
Numerous studies agree that the main goal of surgery is to achieve the best esthetic outcome in the primary position (PP), with the least number of post-surgical complications, which is usually obtained after more than 1 surgery owing to undercorrections and recurrences in the medium and long term after the first surgery.5,8,9 Since there are no adequate approaches to restore the sensory-motor balance, some authors recommend performing the simplest surgical procedures to avoid the undesirable side effects of more aggressive techniques.7,10 The purpose of this study is to describe the long-term progress and esthetic and functional outcomes after surgery to correct third nerve palsy. We examine the techniques used and analyze the influence of the characteristics of palsy on outcome.
Patients, material and methodsWe performed a retrospective study of the clinical histories of patients surgically treated for unilateral or bilateral third nerve palsy in the ocular motility section of our hospital from 2000 to 2016. The study was approved by the local ethics committee. Data were collected according to the Helsinki protocol. To be included, cases of third nerve palsy (unilateral or bilateral, total or partial, congenital or acquired, solitary or co-occurring with other types of cranial nerve palsy) had to have been diagnosed and surgically treated in our center between the years 2000 and 2016. The exclusion criteria were as follows: third nerve palsy that did not require surgery because it resolved spontaneously within a year of onset, or because the patient refused surgery; cases managed with treatment other than surgery of the extra-ocular muscles (occlusions, prisms, and botulinum toxin); patients with double elevator palsy; and follow-up <6 months.
Near and distance horizontal deviation (HD) were measured using the simultaneous prism and cover test or the Hirschberg test by converting degrees to prism diopters (pd). Head turn was examined subjectively by observing the position of the face and head when fixating a Snellen optotype on a chart. Limitation of ocular duction was rated from 0 (no limitation) to −3 (if the eye did not reach the midline). Total paralysis was defined as a limitation of ocular duction of at least −2 (the eye does not pass the midline), and partial palsy or paresis as a limitation of less than −2. Third nerve palsy was considered complete when all muscles were affected (including ptosis and pupillary involvement). The forced duction test was performed in the operating room. Surgery was indicated at least 1 year after the onset of palsy. Botulinum toxin (Botox®, Allergan, Inc., Irvine, CA, USA) was injected before surgery to resolve antagonist muscle contracture, and/or after surgery in some undercorrected cases.
We recorded the following: mean age at diagnosis, incidence and type of third nerve palsy, affected eye, duration of paralysis (from onset of symptoms until the first visit to the ocular motility section); mean near and distance vertical deviation (VD) and HD in PP, before and after each surgery, at 6 months, at 1 year and at the end of follow-up; incidence of diplopia and head turn before and after surgery; and mean visual acuity before and after surgery. We analyzed the type of surgery and its influence on the final outcome, the mean number of surgeries per patient, and the number of muscles operated on in each surgical procedure. We also recorded the percentage of good esthetic and functional results, their progress over time, and the mean follow-up period. A final deviation of <10pd was considered a good esthetic outcome, 10 and 20pd a normal outcome, and >20pd a poor outcome. A functional outcome was considered good when there was no postoperative diplopia in PP.
The statistical analysis was performed using SPSS Statistics for Windows, Version 22.0 (IBM Corp., Armonk, New York, USA). Statistical significance was set at p<0.05. The t test was used to compare quantitative variables, and Fisher's exact test was used to compare qualitative variables. The chi-square test, Wilcoxon signed rank test, and Pearson's correlation coefficients were used to test the hypothesis. A linear regression analysis was performed to assess the influence of the variables on outcome.
ResultsThe study population comprised 31 patients who had undergone surgery for strabismus secondary to third nerve palsy. The mean±SD age was 36.27±24.52 years (16 women: 51.6%). The right eye was affected in 17 cases (54.8%) and the left eye in 11 (35.5%). Three patients (9.7%) had bilateral palsy. The palsy was complete and total in 7 patients (22.6%), congenital in 6 (19.4%), and acquired in 25 (80.6%). Among the acquired cases, 9 were secondary to head trauma, 7 to vascular disease, 7 to neoplasm of the central nervous system, and 2 to neurosurgical procedures. Before surgery, diplopia was observed in 18 cases (58.1%), head turn in 17 (54.8%), ptosis in 15 (48.4%), and pupillary involvement in 16 (51.6%). The mean duration since onset was 5.06±9.5 years.
Table 1 shows preoperative and postoperative data from the oculomotor examination.
Results of the eye examination before strabismus surgery and at the end of follow-up.
| Variables | Preoperative | Postoperative |
|---|---|---|
| Diplopia (%) | 58.1 | 19.4 |
| Head turn (%) | 54.8 | 35.5 |
| LAD (%) | 77.4 | 41.9 |
| LAD (%) grade-1 | 48.3 | 29.03 |
| LAD (%) grade-2 | 22.5 | 9.6 |
| LAD (%) grade-3 | 6.4 | 3.2 |
| LAB (%) | 3.2 | 54.8 |
| LAB (%) grade-1 | 0 | 51.6 |
| LAB (%) grade-2 | 0 | 3.2 |
| LAB (%) grade-3 | 3.2 | 0 |
| Lsupra (%) | 83.9 | 64.5 |
| Lsupra (%) grade-1 | 25.8 | 32.5 |
| Lsupra (%) grade-2 | 19.35 | 19.3 |
| Lsupra (%) grade-3 | 38.7 | 12.9 |
| Linfra | 80.6 | 54.8 |
| Linfra (%) grade-1 | 38.7 | 29.03 |
| Linfra (%) grade-2 | 16.1 | 12.9 |
| Linfra (%) grade-3 | 25.8 | 12.9 |
| HD distance (mean±SD) | 44.29±25.48 | 11.35±15.28 |
| HD near (mean±SD) | 40.24±27.3 | 8.94±14.71 |
| VD near (mean±SD) | 14.33±9.87 | 6.13±8.99 |
| VA (mean±SD) | 0.55±0.25 | 0.6±0.27 |
LAD: limitation of adduction; LAB: limitation of abduction; Lsupra: limitation of supraduction; Linfra: limitation of infraduction; HD: horizontal deviation; VD: vertical deviation; VA: visual acuity of the affected eye.
Mean preoperative HD was 40.24pd±27.38 for near in PP and 44.29pd±25.48 for distance. VD for near was 14.33pd±9.87. The mean preoperative visual acuity of the affected eye was 0.55±0.25.
Complementary treatment with botulinum toxin was administered to 45.2% of patients (42% before surgery and 9.7% after surgery). The mean number of surgeries was 1.4±0.68, and the mean number of muscles per surgical procedure was 1.93±0.86. Only 1 surgery was performed in 68.9% of cases, 2 surgeries in 24.4%, 3 surgeries in 4.4%, and 4 surgeries in 2.2%. Only 1 muscle was operated on per procedure in 33.3% of cases, 2 muscles in 46.7%, 3 muscles in 13.3%, and 4 muscles in 6.7%. Table 2 shows the techniques performed for treatment of third nerve palsy. Third and sixth nerve palsy were diagnosed in 1 case, and augmented vertical rectus transposition to the lateral rectus (LR) was performed owing to esotropia.
Types of surgery performed in each surgical procedure.
| Type of surgery | Number of surgeries |
|---|---|
| Muscle recession | 17 |
| Muscle resection | 6 |
| Combined (recession+resection) | 14 |
| Recession with partial tenotomy | 2 |
| Transposition (MR to LR; VR to LR) | 2 |
| Anchorage to periosteum | 3 |
| Resection+anchorage to periosteum | 1 |
MR: medial rectus; LR: lateral rectus; VR: vertical rectus.
The mean near and distance HD 6 months after surgery were 10.61pd±15.08 and 12.41pd±15.15, respectively. The mean VD after 6 months of surgery was 7.93pd±6.9. The mean near HD 1 year after surgery was 7.87pd±14.34, and the mean distance HD was 9.72pd±14.01. The mean vertical deviation 1 year after surgery was 7.15pd±7.28. The mean near and distance final HD were 8.94pd±14.71 and 11.35pd±15.28, respectively. The mean VD at the end of follow-up was 6.13pd (±8.99). Fig. 1 shows the progress of the preoperative and postoperative horizontal and vertical deviations in primary position during the follow-up.
Diplopia was resolved in PP at the end of follow-up in 80.6% of cases. No head turn was recorded in 64.5% of cases (resolved in 35.2%: 6 out of 17 cases). A good esthetic outcome was observed in 64.5% of cases, a normal outcome in 25.8%, and a poor outcome in 9.7%. A good functional outcome was achieved in 72.2% of cases (diplopia resolved in 13 out of 18 cases). At the end of follow-up, 5 cases remained overcorrected regarding HD (exotropia that turned into esotropia) and a single case was overcorrected in VD (hypertropia that turned into hypotropia). The mean postoperative VA at the end of follow-up was 0.6±0.27. There was no significant difference between the pre- and postoperative VA of the affected eye. Mean follow-up was 6.05±4.6 years. No intra- or postoperative complications were observed.
Statistical results: Age was significantly correlated with acquired paralysis. Neither the type of palsy nor the etiology significantly influenced the final outcome. Better esthetic and functional outcomes were related to older age, shorter duration of palsy, and lower HD and VD, although the differences were not statistically significant. Similarly, no statistically significant differences were found between the surgical techniques used and the results. A statistically significant difference was observed between the preoperative mean HD and VD and postoperative mean HD and VD at 6 months, 1 year, and the end of follow-up (p <0.0001). VD also improved significantly between the sixth month and the first year after surgery (p=0.03), as did near HD (p=0.019) and distance HD (p=0.035) at 1 year compared with the end of follow-up (Table 3).
Statistically significant difference between the mean horizontal and vertical deviation: preoperative and postoperative data at 6 months, 1 year, and the end of follow-up.
| Mean statistical differences | t test (p)* |
|---|---|
| Near HD pre-Near HD 6 months | 0.000 |
| Distance HD pre-Distance HD 6 months | 0.000 |
| VD pre-VD 6 months | 0.000 |
| Near HD pre-Near HD 1 year | 0.000 |
| Distance HD pre-Distance HD 1 year | 0.000 |
| VD pre-VD 1 year | 0.000 |
| Near HD pre-Near HD final | 0.000 |
| Distance HD pre-Distance HD final | 0.000 |
| VD pre-VD final | 0.000 |
| Near HD 6 months–Near HD 1 year | 0.801 |
| Distance HD 6 months–Distance HD 1 year | 0.903 |
| VD 6 months–VD 1 year | 0.038 |
| Near HD 6 months–Near HD final | 0.070 |
| Distance HD 6 months–Distance HD final | 0.129 |
| VD 6 months–VD final | 0.983 |
| Near HD 1 year–Near HD final | 0.019 |
| Distance HD 1 year–Distance HD final | 0.035 |
| VD 1 year–VD final | 0.614 |
HD: horizontal deviation; VD: vertical deviation.
In this study, most of the third nerve palsies that required surgery were unilateral (90.3%) and acquired (80.6%: traumatic 36%); higher percentages of congenital and traumatic palsies (30% and 50% respectively) have been reported elsewhere.7 Treatment of strabismus and diplopia owing to third nerve palsy is very challenging for the ophthalmologist, and while many surgical techniques have been published,8,11–14 none achieve a definitive solution.15 The simplest techniques for the correction of HD are supra-maximal resection and recession of the MR and LR, respectively (classic surgery), in combination with vertical rectus recession for VD.10 Innervational surgery on the unaffected eye is another initial therapeutic option that may decrease the deviation and correct the signs caused by aberrant regeneration.16 We agree with those authors who choose the simplest and most predictable technique to correct strabismus in third nerve palsy.1,7 Therefore, we performed maximal recession and resection of the LR and MR, respectively, in all those patients who have not undergone surgery previously (39 procedures) and graded them according to the initial deviation. Superior oblique muscle transposition has been proposed to limit abduction and depression of the paralyzed eye and to correct its torsion.13,17 This can be performed with or without resection of the muscle, with or without trochleotomy, and with insertion of the muscle below the insertion of the superior rectus muscle.18 However, surgery can generate side effects, such as restrictive hypertropia and abnormal eye movements.19 This technique was not used in any of our patients. Salazar-León et al.11 published another technique in which they attached the eyeball to the nasal periosteum with fascia lata to improve the eye position. In our sample, 4 fixations were made to the periosteum (2 cases): 3 to the nasal bone (in 1 case, first with non-absorbable suture and then with fascia lata due to recurrence of the deviation) and 1 to the temporal bone. Both patients had a regular esthetic result, and 1 had a good functional result. In both cases, we used anchorage to the periosteum for the second and third surgery. Transposition of the vertical rectus to the MR is not indicated if the palsy is complete, because the function of the superior and inferior recti muscles will not be sufficient and the transposition will not work. In recent years, good results have been published with nasal transposition of the LR to the MR, with or without splitting of the LR.2,20–22 However, this technique is not free of complications, such as choroidal effusion, central serous chorioretinopathy, and compressive neuropathy.21 We considered this approach as our first surgical option in a case of complete third nerve palsy which is treated with classic surgery at another center. However, the esthetic result was poor, and the patient further underwent 2 procedures, with nasal periosteum fixation.
The mean number of surgeries performed was 1.4, and the mean number of muscles per surgical procedure was 1.9. Only 1 surgery was performed in 68.9% of cases, and only 2 muscles were operated on in 46.7%. These data are similar to those published elsewhere.7 Other authors argue that several surgical procedures are required.3,5,9 In a pediatric study by Schumacher-Feero et al.,9 a mean of 2.3 surgical procedures were performed per patient with complete third nerve palsy, and a mean of 1.5 interventions in those with partial palsy.13 Complementary treatment with botulinum toxin injections can reduce the number of muscles operated on and surgeries performed.13,14 In our sample, it was used before surgery and may account for the lower number of muscles operated on and surgeries performed compared with other series.
At the end of follow-up, an ocular deviation of less than 10pd was obtained in 64.5% of cases, diplopia in PP resolved in 72.2% of cases, and torticollis resolved in 35.2%. These findings are similar to those reported in other publications,6,7,13,21 which can reach 90% with combined procedures.17 In any case, regardless of the type of surgery, favorable esthetic results can only be obtained in PP, as eye rotations cannot be completely re-established.3 In our sample, preoperative adduction was limited in 77.4%; this decreased to 41.9% in the postoperative period. Preoperative abduction was limited in 3.2% of cases; this increased to 54.8% after surgery (51.6% with grade 1). The percentage of limitation of supraduction and infraduction decreased in the postoperative period. Our results cannot be compared with those for other palsies, since the criteria are less strict than with other palsies, such as fourth or sixth nerve palsy.
None of the characteristics analyzed significantly influenced the outcome of surgery. Mean HD was better after 1 year than at the end of follow-up, with a statistically significant difference for near (p=0.019) and distance (p=0.035). These data are similar to those published elsewhere for progressive deterioration of outcome, undercorrections, and long-term relapses,5–7,23,24 However, some publications report stability of deviation 4 months after surgery.6 Mean VD improved with time, and there was a significant difference between the VD at 6 months and VD 1 year after surgery (p=0.03).
In conclusion, most third nerve palsies requiring surgery were acquired and unilateral. The main techniques used were supra-maximal recession and resection of the horizontal recti to correct HD, which were combined with recession of the vertical recti in cases with VD. Nasal and/or temporal periosteum fixation were performed as secondary procedures, as was, exceptionally, medial transposition of the LR. Although none of the variables analyzed significantly influenced the esthetic and functional outcome, better results were recorded in older patients, cases with smaller deviations, and cases where the palsy was acute in onset. Postoperative HD was better 1 year after surgery than at 6 months and at the end of the follow-up. VD improved with follow-up.
Conflicts of interestThe authors have no conflicts of interest to declare.
Meeting presentation: this study was presented as an oral communication at the 25th Spanish Society of Strabismus Meeting in Tarragona, Spain (May 2018).