To understand the clinical pattern of keratoconus in patients visiting a tertiary eye-care center. This may improve the knowledge of the disease and treatment options.
MethodsThe records from a tertiary eye-care hospital-based center were reviewed retrospectively to collect the required data. Medical records from 187 patients who had visited the contact lens clinic in the course of a three-month period were reviewed. The data available on demographics, year of diagnosis of keratoconus, topographic measurements, slit-lamp biomicroscopic findings, previously used or currently advised refractive correction, visual acuity and contact lens parameters were reviewed and recorded.
ResultsOf the 187 patients, 365 eyes were included in the study. Six eyes that had previous corneal grafting and 3 eyes that were fellow normal eyes of unilateral keratoconus were excluded. The patients’ mean age was 21.3±6.96 years. There were 172 (47.12%) eyes previously diagnosed as keratoconus and 193 (52.87%) eyes that had been newly diagnosed as keratoconus. In the newly diagnosed group, 188 eyes were fitted with different types of contact lenses and 5 eyes were advised surgery. In the previously diagnosed group, 138 eyes and 6 eyes continued wearing conventional and multicurve custom rigid gas permeable (RGP) contact lenses, respectively. Of the remaining 28 eyes, 3 eyes were fitted with RGP lenses, 16 were refitted with piggyback, 2 with multicurve custom RGP and 7 were advised for scleral lenses or surgery.
ConclusionThis study brings out the clinical profile of keratoconus patients in a tertiary eye-care center in south India. The findings in this study stresses out the importance of defining the treatment options in keratoconus with the appropriate contact lenses.
Conocer el patrón clínico del queratocono entre aquellos pacientes que acuden a a una clínica especializada de la visión. Esto puede permitir ampliar la información disponible sobre el estado de la enfermedad, así como las distintas opciones de tratamiento.
MétodosSe analizaron de manera retrospectiva los historiales médicos de un centro médico especializado en oftalmología y adscrito a un hospital, extrayéndose de ahí los datos de interés. Se revisaron con detalle los historiales médicos de 187 pacientes que habían acudido a la clínica (especializada en lentes de contacto) durante un periodo de 3 meses consecutivos. En particular, se recogieron datos demográficos, el año en el que se había diagnosticado el queratocono, datos de topografía corneal, características biomicroscópicas observadas con la lámpara de hendidura, corrección refractiva empleada (en el momento de la visita o anteriormente), agudeza visual, y parámetros de la lente de contacto (si utilizaban una).
ResultadosSe incluyeron en el estudio 365 ojos de los 187 pacientes mencionados. Se excluyeron 6 ojos, por haberse realizado un transplante de córnea, así como otros 3 ojos que eran normales (es decir, había 3 pacientes tenían queratocono sólo en uno de sus ojos). La edad media de los pacientes era 21,3±6,96 años. Había 172 (47,12%) ojos que ya habían sido previamente diagnosticados con queratocono y 193 (52,87%) ojos donde el queratocono estaba recién diagnosticado. En el grupo recién diagnosticado, 188 ojos se adaptaron con diferentes tipos de lentes de contacto y a 5 se les aconsejó cirugía. En el grupo de los pacientes previamente diagnosticados, 138 ojos continuaron usando lentes rígidas permeables al gas (RPG) convencionales y 6 ojos lentes multicurvas. De los 28 ojos restantes, a 3 se les adaptaron lentes RPG, 16 fueron readaptados con piggyback, 2 con lentes RPG multicurvas y a 7 se les aconsejó lentes esclerales o cirugía.
ConclusionesEste estudio pone de manifiesto el perfil clínico de los pacientes de queratocono que acuden a una clínica especializada de la visión en el sur de la India. Los resultados de este estudio resaltan la importancia de definir las distintas opciones de tratamiento para el queratocono con las lentes de contacto más adecuadas a cada caso particular.
Keratoconus is a non-inflammatory, self-limiting ectasia of the axial portion of the cornea1 characterized by a progressive thinning and steepening. Patients typically report symptoms of visual distortion, observable corneal irregularities (detected during refraction and corneal topographic evaluations) that worsens with time, classic slit-lamp biomicroscopic signs (Vogt's striae and Fleischer's ring), and progressive corneal scarring. As the cornea steepens and thins, the patient experiences a decrease in vision that depends on the amount of corneal distortion produced. Typically, decreased vision can be corrected in the early stages by means of spectacles; later on, irregular astigmatism requires correction with rigid contact lenses.2 The rigid contact lenses provide a uniform refracting surface and, therefore, improve vision.
Keratoconus is optically managed in its early stages by means of spectacles. Prior to the availability of gas-permeable rigid (RGP) contact lenses, the optical correction of keratoconus was a challenge. Spectacles cannot correct the irregular astigmatism that appears as a result of keratoconus. Before the era of contact lenses, surgery was the only resource for keratoconus management. Today, RGP contact lenses are the method of choice for optimizing vision and managing the irregular astigmatism associated with keratoconus.3 As the disease advances, contact lens fitting becomes increasingly difficult, and surgery becomes an option. However, fitting contact lenses in keratoconus is a complex task.4 The challenge is to keep the patient tolerant with good visual acuity, with a cornea that may be undergoing changes in shape over time.5
The surgical options for keratoconus currently practiced include collagen cross-linking or intra-stromal ring segment implantation and, in advanced stages, corneal transplantation. Corneal transplantation is the best and most successful surgical option for advanced keratoconus, a stage where management with all other modalities fails.6 Although the ectatic area of the cornea is generally displaced inferiorly,7-9 the corneal irregularities lead to vision problems even in the early stages of the condition. Contact lens intolerance, decreased vision and/or central corneal scarring accounts for 10-25% of those keratoconus patients undergoing penetrating keratoplasty.10-13
Most of the previous studies reporting the demographic and clinical details of keratoconus are based on western populations. Few reports are available that analyze a population of Asian ethnicity. A previous study carried out in an Indian tertiary eye-care facility concluded that the majority of the keratoconic eyes in Asian-Indian patients reach the severe stage of the disease by the second decade.14 A 4-fold increase in the incidence of keratoconus among Asians was reported, compared with Caucasian patients.15 A previous study had found a 7.6-fold difference between the Asian and Caucasian patients.16 Despite the claim by Rabinowitz,17 who states that all ethnic groups are equally affected, the variation in prevalence suggests that there is a geographical factor influencing the disease. This fact is supported by an increased keratoconus manifestation in the Mediterranean18 and the Middle Eastern areas19,20, influenced probably by their hot, dry climate. Furthermore, it was found that the Asian keratoconus patients reported were generally younger when the condition first presented and required corneal grafting at an earlier age.15
This retrospective study was planned with the aim to understand the clinical pattern of keratoconus attenging to a tertiary eye-care center in South India (Asia). This may improve the knowledge of the disease status and its treatment options.
MethodsMedical records from a tertiary eye-care facility situated in South India were reviewed retrospectively to collect the data of interest. This work was approved by the Institutional Review Board (IRB) and Ethics committee of the institution in which this study was conducted. Out of 4060 patients who visited the contact lens clinic over a period of one year, there were 609 keratoconus patients. Of these 609 patients, a three-month dataset that included 187 patients who had visited the clinic in the period between October 2006 and December 2006 were reviewed. The patients either had been previously diagnosed with keratoconus or were newly diagnosed as keratoconus during that period, based on clinical features or by means of corneal topographic measurements. The criteria for diagnosis was: the presence of irregular corneal surface in either eye (determined by distortion of keratometric mires, or the retinoscopic reflex, or of the oil-droplet reflex seen in an ophthalmoscopic system) and the presence of Vogt's striae in the deep stroma or Fleischer's ring of at least 2 mm of arc or corneal scarring characteristic of keratoconus in either eye. Patients were also included if they were diagnosed with keratoconus based on their corneal topography pattern (TMS4 Tomey Inc, Version 3.5E), with at least one of the screening systems (the Smolek/Klyce or the Klyce/Maeda) revealing the presence of keratoconus.
The data available on demographics, year of diagnosis of keratoconus, topographic measurements, slit-lamp biomicroscopic findings, previously used or currently advised refractive correction, visual acuity and contact lens parameters were reviewed and recorded. The eyes were grouped into “previously diagnosed” and “newly diagnosed”, in order to have a better understanding of the clinical features during the first presentation and the choice of visual correction advised.
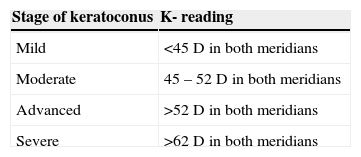
Keratoconus is classified in different ways, in terms of the shape of the cone, the severity level (based on central keratometric readings) or its progression.21 In this study keratoconus was classified as shown in table 1, based on the central corneal curvature value given by keratometric reading, as established by Buxton.22
Classification of keratoconus22
| Stage of keratoconus | K- reading |
| Mild | <45 D in both meridians |
| Moderate | 45 – 52 D in both meridians |
| Advanced | >52 D in both meridians |
| Severe | >62 D in both meridians |
More than 14% (n=609) of the patients attending to a contact lens clinic over a period of one year had a diagnosis of keratoconus. Of those 609 patients, 187 of them (examined during three consecutive months) made up the population of this study. Of those 187 patients from whom data was collected, 6 of them had previously had a corneal grafting done in the fellow eye, and 3 patients had unilateral keratoconus, wherein the fellow eye was clinically and topographically normal. As a result, a total of 365 eyes with keratoconus were included in this study. Regarding gender, of the 187 patients 116 patients (62%) were male. The patients’ mean age was 21.3±6.96 years (range: 10-58 years). When grouped into “previously diagnosed” and “newly diagnosed” patients, the group's mean age was 22.21±6.97 years and 20.48±6.87 years, respectively. There were 172 eyes (47.12%) that had been previously diagnosed of keratoconus, and 193 (52.87%) eyes that were newly diagnosed of keratoconus. The average number of years since the diagnosis, for previously diagnosed patients, was 1.32±2.48 years (ranging from 0.2 to 20 years).
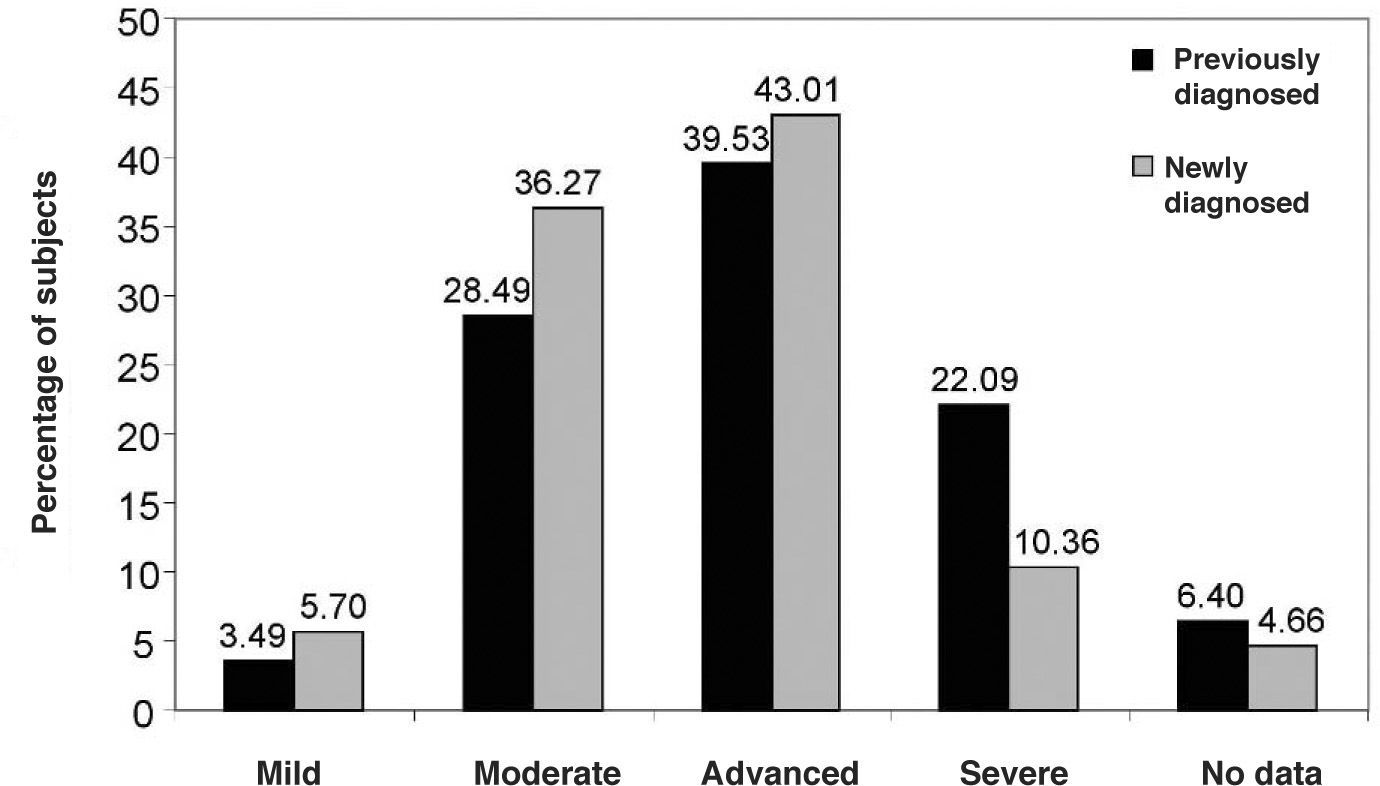
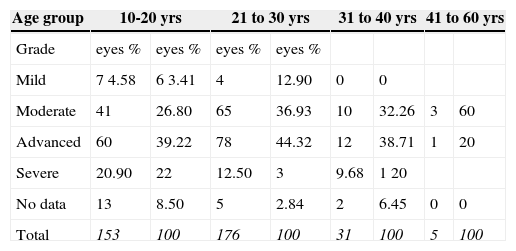
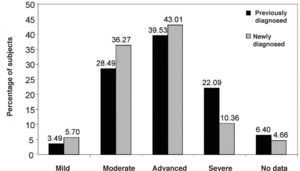
The mean flat and steep simulated keratometric readings were 54.73±6.94D and 48.95±5.57D, respectively. Figure 1 shows the number of eyes found to be in each grade of keratoconus at presentation. It was noted that the majority of patients presented during the moderate (32.6%) or advanced (41.37%) stages of keratoconus. Table 2 shows the distribution of the keratoconus eyes in terms of the stage of the keratoconus, for each age group. It can be observed that 90% of the patients were less than 30 years of age at presentation.
Distribution of the different age group of subject's eyes with different stage of keratoconus. Number (and percentage) of keratoconus eyes within the sample that were found to be at each keratoconus stage, for the different age groups under study
| Age group | 10-20 yrs | 21 to 30 yrs | 31 to 40 yrs | 41 to 60 yrs | ||||
| Grade | eyes % | eyes % | eyes % | eyes % | ||||
| Mild | 7 4.58 | 6 3.41 | 4 | 12.90 | 0 | 0 | ||
| Moderate | 41 | 26.80 | 65 | 36.93 | 10 | 32.26 | 3 | 60 |
| Advanced | 60 | 39.22 | 78 | 44.32 | 12 | 38.71 | 1 | 20 |
| Severe | 20.90 | 22 | 12.50 | 3 | 9.68 | 1 20 | ||
| No data | 13 | 8.50 | 5 | 2.84 | 2 | 6.45 | 0 | 0 |
| Total | 153 | 100 | 176 | 100 | 31 | 100 | 5 | 100 |
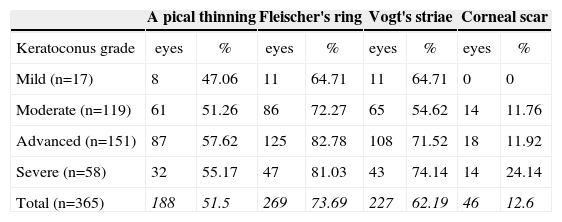
Table 3 shows the distribution of slit lamp biomicroscopic signs for the different grades of keratoconus. There were 32 eyes that showed no clinical features of keratoconus, but which were diagnosed of keratoconus after close examination of their corneal topography pattern.
Percentage of keratoconus eyes, grouped by grade, for which each of the following slit-lamp clinical signs were observed
| A pical thinning | Fleischer's ring | Vogt's striae | Corneal scar | |||||
| Keratoconus grade | eyes | % | eyes | % | eyes | % | eyes | % |
| Mild (n=17) | 8 | 47.06 | 11 | 64.71 | 11 | 64.71 | 0 | 0 |
| Moderate (n=119) | 61 | 51.26 | 86 | 72.27 | 65 | 54.62 | 14 | 11.76 |
| Advanced (n=151) | 87 | 57.62 | 125 | 82.78 | 108 | 71.52 | 18 | 11.92 |
| Severe (n=58) | 32 | 55.17 | 47 | 81.03 | 43 | 74.14 | 14 | 24.14 |
| Total (n=365) | 188 | 51.5 | 269 | 73.69 | 227 | 62.19 | 46 | 12.6 |
*Of the 365 eyes there was no data available for 20 eyes (5.48%).*For 32 eyes no slit lamp clinical signs were observed. Those eyes belong to the mild and the moderate groups.
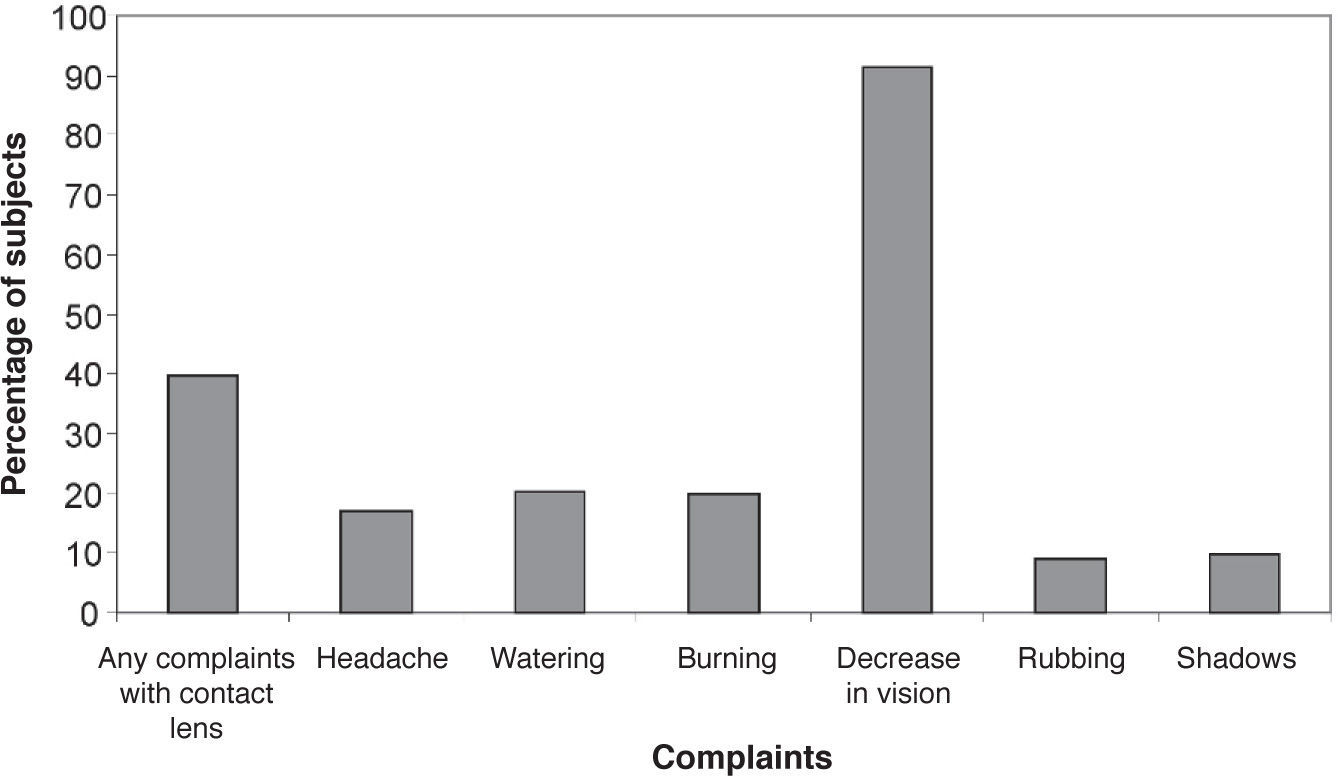
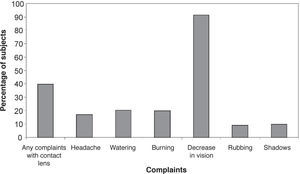
The symptoms reported by the patients were: headache, complaints of intolerance to contact lens due to discomfort and worsening in vision with current contact lens, watering, burning, decrease in vision, allergic reaction and eye rubbing, complaints of ghost images and shadows (Figure 2).
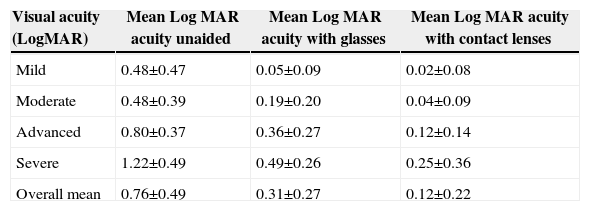
Table 4 summarizes the uncorrected visual acuity (UCVA), best spectacle-corrected (BSCVA) and best contact-lens-corrected visual acuity (BCCVA) according to the Log MAR scale. The best corrected visual acuity with contact lenses and glasses showed a statistically significant difference (P<0.05). The average contact lens acuity was one line and four letters (SD of 2 letters) higher than that observed with glasses.
Mean visual acuity (LogMAR units) for the different keratoconus groups (according to the keratoconus grade). P<0.05 between any two groups
| Visual acuity (LogMAR) | Mean Log MAR acuity unaided | Mean Log MAR acuity with glasses | Mean Log MAR acuity with contact lenses |
| Mild | 0.48±0.47 | 0.05±0.09 | 0.02±0.08 |
| Moderate | 0.48±0.39 | 0.19±0.20 | 0.04±0.09 |
| Advanced | 0.80±0.37 | 0.36±0.27 | 0.12±0.14 |
| Severe | 1.22±0.49 | 0.49±0.26 | 0.25±0.36 |
| Overall mean | 0.76±0.49 | 0.31±0.27 | 0.12±0.22 |
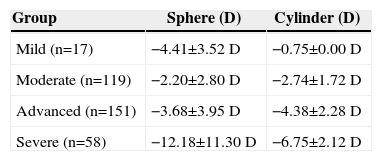
The refractive error in the different groups of keratoconus are tabulated in table 5. The table illustrates the variability in myopia between severity groups and increase in astigmatic prescription with increasing severity.
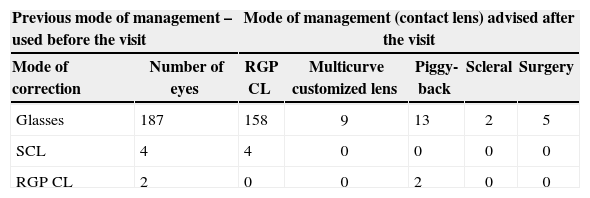
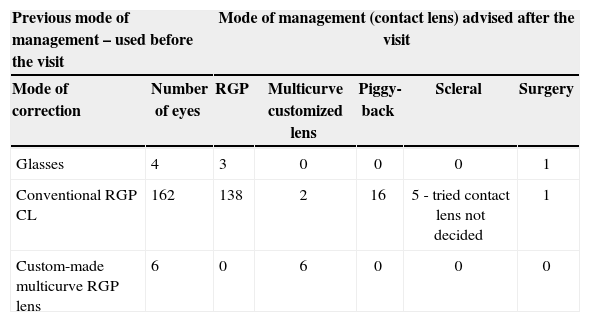
The refractive correction that the subject was using at the time and the corrective approach advised after the presentation varied. This change is summarized for both new and previously diagnosed patients in tables 6and7. In the group of 193 eyes newly diagnosed, all of them changed their mode of refractive correction of whom 84% changed to RGP lenses and 16% to other forms of contact lens correction such as custom multicurve lenses, piggyback, scleral lenses or surgery.
Change of refractive correction advised after the visit, for the group of “newly diagnosed keratoconus eyes” n=193 (SCL – soft contact lens, RGP CL –Rigid gas-permeable contact lens)
| Previous mode of management – used before the visit | Mode of management (contact lens) advised after the visit | |||||
| Mode of correction | Number of eyes | RGP CL | Multicurve customized lens | Piggy-back | Scleral | Surgery |
| Glasses | 187 | 158 | 9 | 13 | 2 | 5 |
| SCL | 4 | 4 | 0 | 0 | 0 | 0 |
| RGP CL | 2 | 0 | 0 | 2 | 0 | 0 |
Change of refractive correction advised after the visit, for the group of “previously diagnosed keratoconus eyes” n=172 (SCL – Soft contact lens, RGP CL –Rigid gas-permeable contact lens)
| Previous mode of management – used before the visit | Mode of management (contact lens) advised after the visit | |||||
| Mode of correction | Number of eyes | RGP | Multicurve customized lens | Piggy-back | Scleral | Surgery |
| Glasses | 4 | 3 | 0 | 0 | 0 | 1 |
| Conventional RGP CL | 162 | 138 | 2 | 16 | 5 - tried contact lens not decided | 1 |
| Custom-made multicurve RGP lens | 6 | 0 | 6 | 0 | 0 | 0 |
In the 172 previously diagnosed eyes, there were 4 eyes corrected earlier with spectacles, of which, 3 eyes shifted to RGP lens and 1 underwent surgery. Of the remaining 168 previously contact lens wearing eyes, 138 eyes continued wearing RGP lenses and 6 eyes continued wearing multicurve custom made RGP lenses. Sixteen eyes in the group wearing RGP lenses shifted to piggyback fitting and 5 eyes were advised for scleral lens trial and 1 eye undergone surgery.
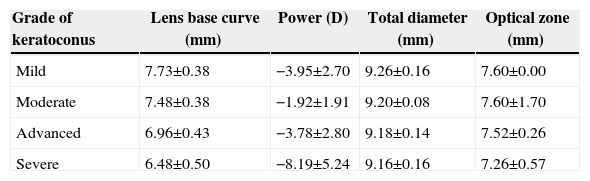
The gas-permeable Fluroperm 30 DK lens that the patients were fitted with had different lens parameter values (base curve radius and diameter), depending on the particular case. The average basecurve employed for the different grades of keratoconus is detailed in table 9. The base curve ranged from to 5.9mm to 8mm.
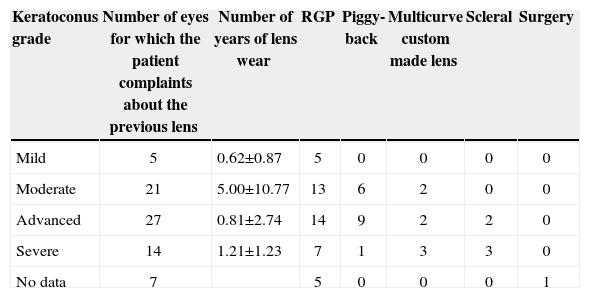
Number of eyes that brought patient complaints (like intolerance, poor comfort, vision) about the previous contact lens, and the chosen mode of management after presentation
| Keratoconus grade | Number of eyes for which the patient complaints about the previous lens | Number of years of lens wear | RGP | Piggy-back | Multicurve custom made lens | Scleral | Surgery |
| Mild | 5 | 0.62±0.87 | 5 | 0 | 0 | 0 | 0 |
| Moderate | 21 | 5.00±10.77 | 13 | 6 | 2 | 0 | 0 |
| Advanced | 27 | 0.81±2.74 | 14 | 9 | 2 | 2 | 0 |
| Severe | 14 | 1.21±1.23 | 7 | 1 | 3 | 3 | 0 |
| No data | 7 | 5 | 0 | 0 | 0 | 1 |
There were 51 eyes (13.9% including the 5 eyes with no data for grading but with scar) for whom the scar was clinically identified by means of slit-lamp biomicroscopy. Out of those eyes, 27 of them (52.9%) were previous contact lens users for an average period of 3.49±2.93 years. The average base curve radius of the lens fitted to these eyes with corneal scar was 6.47±0.41mm, the average total diameter was 9.1±0.11mm and the average optical zone was 7.3±0.54mm. All 51 patients were either in the moderate, in the advanced or in the severe group of keratoconus. The average age of those patients showing corneal scar was 20.93±5.55 years.
DiscussionThere were 609 (14.78%) keratoconus patients out of a hospital-based population of 4060 patients who visited the contact lens clinic over a period of one year. Of these 609 patients, 450 (73.8%) had been previously diagnosed with keratoconus and 159 (26.1%) were newly diagnosed patients. There have been studies reporting incidences of keratoconus ranging from 50 to 230 cases per 100,000 people in the general population.17 In a study by Lim and Vogt, 16.4% of all the patients that came to the contact lens department over 12-month period had keratoconus.5 Among Asians, the incidence of keratoconus was found to be 19.6 cases per 100,000 people.15 The incidence of keratoconus has been reported to be 2 cases per 100,000 people per year, with a prevalence of 55 cases per 100,000 people.13
Analyzing these data, apparent differences arise across racial and ethnic groups: reports indicate a 4-7.6-fold increase in keratoconus incidence among Asian population, compared to Caucasians.15,16 Georgiou et al., whose study population mostly comprised people from the Indian continent (Indian, Pakistani/Bangladeshi) found a lower incidence of atopy among Asians, compared to whites.16 These findings show that the ethnic origin influenced incidence, which suggested that a genetic factor might be involved in etiology.16 Furthermore, Asian keratoconus patients are generally younger at first presentation of the condition and require corneal grafting (in those cases where their condition progresses to that extent) at an earlier age.15 In the present study, the mean age of those patients who were advised to undergo corneal grafting was 21.16 years. It is generally accepted that a higher incidence of keratoconus exists in those countries that have a hot, dry and dusty tropical or sub-tropical climate. It is hence evident that the etiology of keratoconus is multifactorial.
In the present study, the patient's mean age was 21.3±6.96 years. As shown in figure 1, there were only 4.66% eyes (17 eyes) that fell in the mild-keratoconus category, whereas 89.86% (328 eyes) of them were in the moderate-to-severe groups; data was not available for 5.47% (20 eyes). In this study 90% of the patients were between 10 and 30 years of age. Comparing the severity level for the different age groups there were more cases of advanced keratoconus in the groups comprising those under 30, and it is distributed between moderate, severe and advanced stages in the age groups of those having more than 30 years of age (Table 2). The majority of Asian/Indian keratoconus patients reach the severe stage of keratoconus by the second decade.14,15 Saini et al reported a mean age of 20.2±6.4 years during presentation to the tertiary eye-care center.14 Some claim that approximately the same proportion of males and females are diagnosed with keratoconus. However, some others claim that males develop keratoconus more frequently, while others claim that females are more often affected, showing that with regards to published data, considerable variation exists.6,13,23 Over a 1-year period, more than 16% of the patients attending a tertiary specialist contact lens clinic at a UK hospital had keratoconus. In that study, the mean age of the predominantly male patients was 34.9 years, while their mean age at the moment of first referral to the centre was 28.6 years.5 In this study there was a male predominance (62% of male patients). This study reveals a male predominance and a younger age group for those subjects diagnosed with moderate-to-severe keratoconus. These results emphasize the need for early screening, detection and treatment in the younger population, especially in those countries having a similar population and climate to that where this study was undertaken.
The proportion of eyes showing biomicroscopic clinical signs in each keratoconus group in this study are summarized in the table 3. Previous studies by Zadnik et al had observed either Fleischer's ring or Vogt's striae in 68% of the eyes and Vogt's striae, Fleischer's ring, or corneal scarring was observed in
Spherical rigid gas-permeable contact lens parameter range, for the different groups of keratoconus eyes
| Grade of keratoconus | Lens base curve (mm) | Power (D) | Total diameter (mm) | Optical zone (mm) |
| Mild | 7.73±0.38 | −3.95±2.70 | 9.26±0.16 | 7.60±0.00 |
| Moderate | 7.48±0.38 | −1.92±1.91 | 9.20±0.08 | 7.60±1.70 |
| Advanced | 6.96±0.43 | −3.78±2.80 | 9.18±0.14 | 7.52±0.26 |
| Severe | 6.48±0.50 | −8.19±5.24 | 9.16±0.16 | 7.26±0.57 |
The best corrected visual acuity (BCVA), for the majority of the subjects, was observed to be 0.2 LogMAR or better. The CLEK study reported a visual acuity of 20/40 (0.3 LogMAR) or better for 95.5% of the subjects.26 Another study by Weed et al analyzing the Scottish population reported that the majority (97%) of the subjects achieved a binocular visual acuity of 6/9 (0.17 LogMAR) or better.27 These observations regarding BCVA stress that eye care practitioners need to evaluate their patients’ current mode of correction more critically and try to improve visual acuity.
The visual correction and management was changed to a better option in many patients, as can be concluded from tables 6and7. Of the 187 eyes with spectacles, 182 of them were fitted with some kind of contact lens. Keratoconus is known to be the most common indication for penetrating keratoplasty in developed countries. In this study, due to contact-lens intolerance and poor fitting, 5 of the spectacle wearers were advised to undergo surgery. Of the 168 eyes previously fitted with a contact lens (162 with RGP and 6 with multicurve custom-made ones), 138 eyes and 6 eyes continued wearing conventional RGP and multicurve custom lenses, respectively. Sixteen eyes were refitted with piggyback, 2 were advised multicurve custom made lenses and 6 were advised for either scleral lenses or surgery due to poor contact lens fitting and intolerance. There were 74 patients, among the 172 previous contact lens wearer group, that reported intolerance and difficulty with contact lens. The number of years of contact lens wear and the severity of keratoconus among these patients varied significantly. There were also 5 patients with complaints of intolerance and with 0.62±0.87 years of contact lens wear; all of them were refitted with a gas-permeable contact lens of a different power and curvature and were then comfortable. Table 9 summarizes the change in the mode of management of contact lens for those patients who reported intolerance with the contact lens that they were previously using. In the CLEK study's baseline finding, in most cases the patient's vision was corrected with contact lenses in both eyes (892 [74%] out of 1209); of these 892 patients, 571 (64%) also used glasses in some capacity.25 Other studies have reported that about 10-30% of the patients with keratoconus undergo penetrating keratoplasty.29,30 Dana et al confirmed the reasons for referral for penetrating keratoplasty (PK); these were contact lens intolerance, frequent lens displacement, and unsatisfactory visual acuity.6 Patients undergoing PK had best corrected visual acuity ranging from counting fingers to 0.8 LogMAR. In Lim and Vogt's study, eight out of 130 (6%) patients (11 eyes) had undergone PK by the time they were seen at the initial hospital visit. The main reasons for the patients undergoing PK were: contact lens discomfort (83%), unstable contact lens fit (8.5%) and poor visual acuity with contact lenses (8.5%).5 In this study, 3.28% of the patients were advised to consider either PK or deep anterior lamellar keratoplasty. The total percentage of patients having intolerance or reduced visual acuity or poor lens fitting with contact lens in the previously diagnosed cases was 20.27%. But after being refitted with a new model of contact lens, only 5 eyes was advised for surgery. The number of years of contact lens wear ranged from 0.1 to 12 years among those in the previous contact lens wearer group who reported complaints of intolerance with the habitual contact lens. The results in this study regarding the change in mode of vision correction implies that contact lens intolerance is not only a criteria seen in new contact lens wearers. The intolerance reported could be due to other factors like lens fit, lens stability on the eye, contact lens power, severity of the disease and corneal status, even for the previous contact lens users. This emphasizes the need for experienced and trained personnel in fitting irregular corneas, such as in keratoconus, with a stable fit, vision and comfort. Previous studies have shown that patients referred for surgery managed to be fitted with rigid gas-permeable contact lenses when an additional contact lens refit was attempted before surgery.14,16 Similar findings in this study emphasize the need for a retrial of contact lenses of various types in different time periods and even before the decision of surgery.
Previous studies have reported that only 10-25% of keratoconus patients ultimately require corneal surgery.10-13 Of the 187 patients identified as keratoconus in the three-month dataset, 6 eyes had undergone penetrating keratoplasty. Although contact lens intolerance and/or poor vision with contact lens are the most frequent indications for surgical intervention, several studies have indicated that contact lens fitting can help delay or even avoid surgery, and that nonsurgical treatment remains the dominant option in the management of keratoconus.12,30,31,32 The possible limitation of this study could be that the keratoconus population is not calculated from the overall patients seen at the tertiary center. The number and nature of patients reported with keratoconus may be different due to different entries of referrals, the patients may be referred for surgery even before a contact lens trial and the patients may have been identified as keratoconus when they were screened for refractive surgery. Although there could be a data bias due to the fact that the data is from a tertiary eye care facility and was gathered from a three-month period, we expect to derive findings that will allow to sketch the clinical profile of those keratoconus subjects seen in this Asian South Indian tertiary eye care facility.
This study brings out the clinical profile of keratoconus patients in a tertiary eye-care center in south India and also stresses the importance of defining the treatment options in keratoconus with the appropriate contact lenses, especially in developing countries. Further prospective studies can help to develop centers for keratoconus and, possibly, to assess and improve the quality of life in keratoconus patients.
Financial disclosure: None of the authors have a commercial or financial interest in the methods, devices or procedures mentioned in the study.