To compare the diagnostic performance of glaucoma specialists and experienced optometrists in gonioscopy and optic disc assessment.
MethodsThis study was done to validate the diagnostic performance of two experienced optometrists for using their skills of detecting glaucoma using gonioscopy and optic disc assessment in a major epidemiological study, the L V Prasad Eye Institute Glaucoma Epidemiology and Molecular Genetics Study (LVPEI-GLEAMS). Gonioscopic findings for 150 eyes were categorized as 0, 1 and 2 for open angle, primary angle closure suspect (PACS) and primary angle closure (PAC) respectively. Optic disc findings for 200 eyes were categorized as 0, 1 and 2 for normal, suspects and glaucomatous respectively. Weighted kappa (κ) and diagnostic accuracy parameters were calculated. Two optometrists (#1 and #2) participated in the study.
ResultsAgreement between glaucoma specialists and optometrist for interpretation of gonioscopy to discriminate PACS and PAC from open angles and for interpretation of optic disc to discriminate glaucomatous and suspicious discs from normal, the kappa (κ) was 0.92 and 0.84 and 0.90 and 0.89 for optometrists #1 and #2 respectively. Sensitivities and specificities were above 90% for gonioscopy. Optic disc evaluation had specificities greater than 95% to discriminate normal from glaucomatous discs while the sensitivities were 83% and 93% for optometrists #1 and #2 respectively.
ConclusionAgreement between optometrists and glaucoma specialists, in diagnostic performance of gonioscopy and optic assessment was excellent with high sensitivity and specificity. Hence, we conclude that the experienced optometrists can detect glaucoma accurately in the LVPEI-GLEAMS.
Comparar el desempeño diagnóstico de los especialistas en glaucoma y los optometristas especializados en gonioscopia y evaluación del disco óptico.
MétodosEste estudio se llevó a cabo para validar el desempeño diagnóstico de dos optometristas especializados en gonioscopia y evaluación del disco óptico, y utilizar sus técnicas de detección del glaucoma mediante gonioscopia y evaluación del disco óptico en un gran estudio epidemiológico, el Estudio de Genética Molecular y Epidemiológico del Glaucoma del Instituto Oftalmológico L V Prasad (LVPEI-GLEAMS). Los hallazgos gonioscópicos en 150 ojos fueron clasificados como 0, 1 y 2 para apertura angular, sospecha de cierre angular primario (PACS) y cierre angular primario (PAC), respectivamente. Los hallazgos relativos al disco óptico en 200 ojos fueron clasificados como 0, 1 y 2 para ojos normales, sospechosos y glaucomatosos, respectivamente. Se calcularon los parámetros de kappa (κ) ponderada y de precisión diagnóstica. Participaron 2 optometristas (#1 y #2) en el estudio.
ResultadosLa concordancia entre los especialistas en glaucoma y los optometristas, en la interpretación de la gonioscopia para discriminar los PACS y PAC en la apertura angular, e interpretar el disco óptico y discriminar los discos glaucomatosos y sospechosos en los ojos normales, mediante el parámetro kappa (κ) fue de 0,92 y 0,84, y de 0,90 y 0,89 para los optometristas 1 y 2, respectivamente. Las sensibilidades y especificidades fueron superiores al 90% en la gonioscopia. La evaluación del disco óptico arrojó especificidades superiores al 95% para la discriminación entre discos normales y glaucomatosos, mientras que las sensibilidades fueron del 83% y 93% para los optometristas #1 y #2, respectivamente.
ConclusiónLa concordancia entre optometristas y especialistas en glaucoma, en el desempeño diagnóstico de la gonioscopia y la evaluación óptica, fue excelente en cuanto a sensibilidad y especificidad. Por tanto, concluimos que puede utilizarse la valoración de los optometristas especializados para realizar una detección precisa del glaucoma en el estudio LVPEI-GLEAMS.
Glaucoma is the second leading cause of blindness after cataracts and is the leading cause of irreversible blindness, with an estimated burden of 8.4 million people bilaterally blind from glaucoma worldwide in 2010.1 It is predicted that due to the changing demographics and increased life expectancy there will be a significant increase in the number of glaucoma patients worldwide. More than 90% of glaucoma patients are unaware of the disease in the South Indian population.2,3 There should be an emphasis on a comprehensive ocular examination including gonioscopy for proper case detection and treatment of primary angle closure disease (PACD).4 Identifying and differentiating the type of glaucoma based on gonioscopy and optic disc assessment requires sound clinical experience.
There is a pressing need for eye care professionals at the community level as the ophthalmologist to population ratio is 1:25,000 and 1:219,000 in urban and rural areas of India, respectively. The number of ophthalmologists located in urban areas is 70% despite the fact that only about 23% of the population of India reside in towns and cities.5 Optometry training in India involves 3 years of theory classes and a year of clinical internship in a tertiary eye care centre. After completion of graduation most of the optometry students prefer to undergo a clinical fellowship at the L V Prasad Eye Institute for an year, where the fellows are trained in each and every subspecialty area. India currently has approximately 9000 4-year trained optometrists and needs 115,000 Optometrists in order to address an estimated 456 million people of India's population (of 1.12 billion people total population) who require vision correction (spectacles, contact lenses or refractive surgery) to perform the daily living and 26 million people are blind or visually impaired due to any eye disease. A further 133 million people, including 11 million children, are blind or visually impaired simply from lack of an eye examination.6
Considering the fact that most people are unaware of the presence of glaucoma or its status as one of the major diseases affecting public health, a population based detection strategy is more likely to be effective than individual focussed collective responsibility. In this scenario the availability of suitably trained personnel other than ophthalmologists, such as optometrists, can play a key role by engaging in public health disease detection activities.7,8
This approach fits into the eye care delivery model advocated by of the L V Prasad Eye Institute whereby a focussed examination conducted close to the home location of the individual results in the identification of suspected specific pathologies. This can then initiate an efficient referral process to confirm the diagnosis and administer the appropriate treatment within a reasonable time frame. It also helps developing the communication with fellow eye care professionals.9 As reported in previous studies on shared care for glaucoma diagnosis, highly motivated and skilled community-based optometrists with good agreement are safe, clinically effective and reliable local resources in providing a convenient and appropriate shared care of glaucoma patients.10,11 Myint and associates reported that a shared competency-based approach enables a coordinated training and development model for all professionals involved in glaucoma detection and management.12
To become an integral part of the glaucoma team, optometrists need to acquire the skills required for detecting the designated diseases. It has been shown in various studies that optometrists have a high level of agreement with the reference standard specialist ophthalmologists in glaucoma detection by optic disc examination and management.13,14 To the best of our knowledge, there are no reports on the agreement between optometrists and glaucoma specialists in gonioscopic evaluation of the angle.
The primary goal of this study is to establish the sensitivity and specificity with which the two experienced optometrists can detect glaucomatous changes using gonioscopy and optic disc assessment relative to the gold standard ophthalmologists diagnosis.
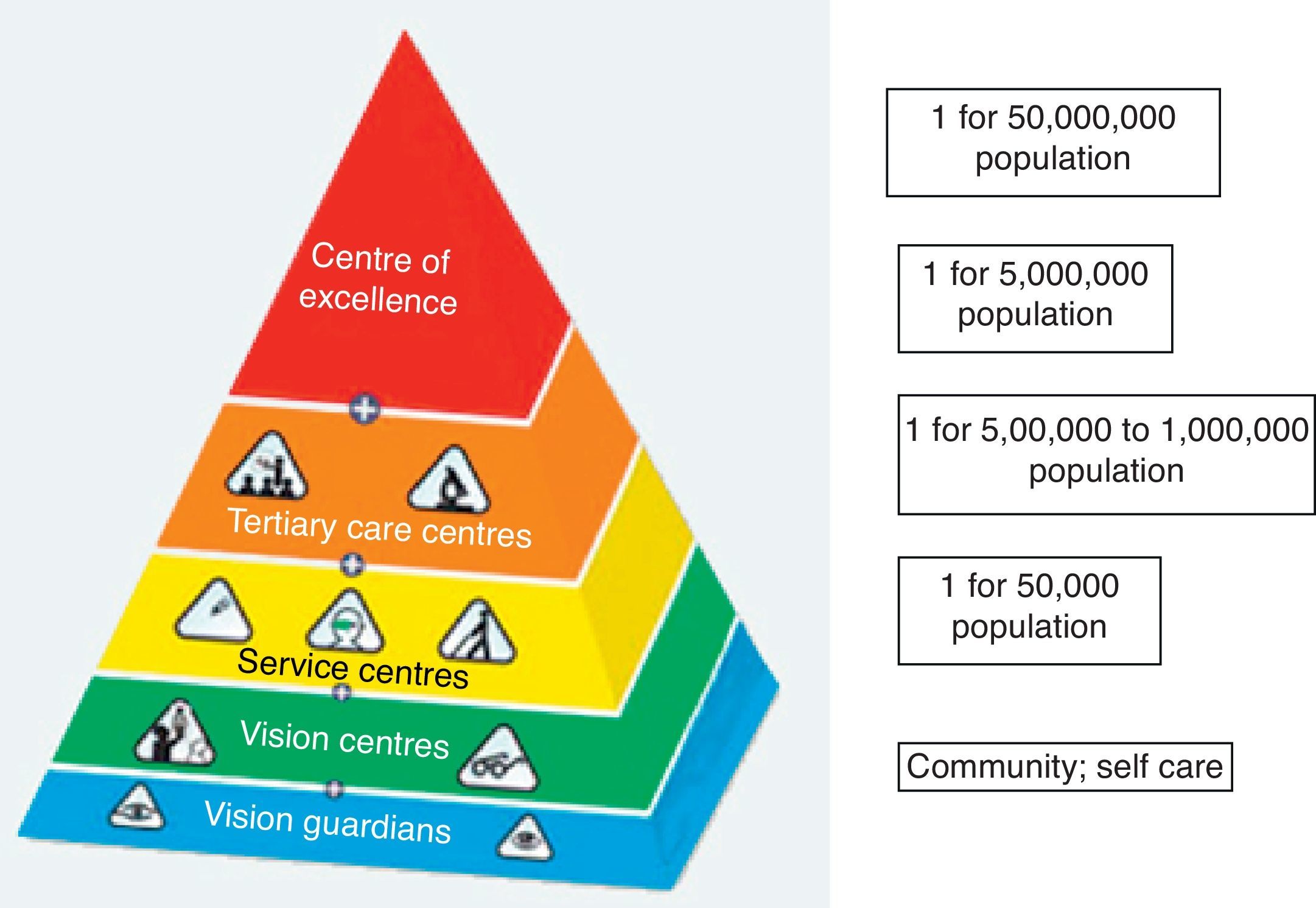
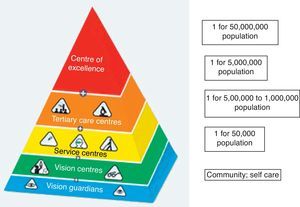
The LVPEI pyramidal model for eye-care delivery that is advocated by the World Health Organization (WHO), at the lowest level of the pyramid is a vision center managed by a vision technician. Primary–secondary interface exists between the primary care services at the vision center and secondary care services at the service centre. Each vision center caters to a population of 50,000.15 (Fig. 1)
Patients and methodsThe study was conducted in the outpatient department of the L V Prasad Eye Institute, Hyderabad, India itself. The study was approved by the ethics committee of the L V Prasad Eye Institute and was conducted according to the tenets of the Declaration of Helsinki. Informed consent was obtained from all the participants.
Three glaucoma specialists with experience ranging from 8 through 23 years and 2 optometrists who had been working with the same specialists for over 7 years in the Glaucoma department of a tertiary eye care centre were available for this work. During this time between 5000 and 9000 glaucoma patients were examined and managed by the ophthalmologists. Both the optometrists performed gonioscopy and optic disc assessment on over 2000 patients while gaining experience in the assessment and management of patients with glaucoma along with the same glaucoma specialist ophthalmologists.
The data were collected prospectively while following the standard proforma of patient examination.
The standard training protocol of the optometrist at L V Prasad Eye InstituteThe L V Prasad Eye Institute, being a centre of excellence in the eye care delivery pyramidal model,15 most of the patients come with complex eye problems. Patients initially report to the front office personnel and are directed to the comprehensive outpatient department where the complete examination is done by both the optometrist and ophthalmologist. Referral to the subspecialty clinic is then made depending on the necessity. The examination procedures were based on the standard proforma. For each patient, post dilation evaluation of the optic disc and fundus was done with a 90.00D (Volk Optical Inc, Mentor, OH, USA) lens. Disc cupping and appearance were documented by drawing important features such as the cup-disc ratio, neuroretinal rim, asymmetry, peripapillary atrophy, disc haemorrhages and collateral vessels. Gonioscopy was carried out for every patient before dilation, with a Sussman 4 mirror gonio lens (Volk Optical Inc., Mentor, OH, USA). The notes were concluded by a summary “impression” of the clinical state, i.e. whether discs, fields and IOPs were stable or progressive. For the current study all examiners retained their own gonioscopic and optic disc assessment information so that the entire procedure remained masked among the observers. No other clinical data were available to the observers.
Categorization of gonioscopy and optic disc findingsFor the purpose of the current study gonioscopic findings were categorized as 0, 1 and 2 for open angle, primary angle closure suspect (PACS) and primary angle closure (PAC) respectively and optic disc findings as 0, 1 and 2 for normal, disc suspect and glaucomatous respectively.
Classification of the optic disc as normal, suspect or glaucomatous was based solely on its appearance. For gonioscopic criteria the standardized International Society for Geographical and Epidemiologic Ophthalmology (ISGEO) classification was used.16
Patient allocationNew patients attending the comprehensive outpatient department at LVPEI were recruited into the study. After the initial work-up by the general optometrists, each of the two experienced optometrists and the glaucoma specialist ophthalmologist carried out gonioscopy. These procedures continued until the glaucoma specialist had recorded a total of 150 eyes including 25 with occludable angles only, 25 with occludable angles and synechiae and 100 eyes with open angles without any other abnormality. Gonioscopy was done after intraocular pressure recording and the category of the angle entered in a separate log book as 0, 1 or 2.
Similarly, post dilated optic disc examination was conducted for all the new patients, by each of the experienced optometrist followed by the glaucoma specialist. Again details of the results were masked between the clinicians and the process continued until the glaucoma specialist had recorded a total number of 200 eyes, 30 with suspect discs, 30 with glaucomatous discs and the rest normal and graded as 0, 1 or 2.
Patients with a history of any ocular surgery or with dense media opacities which would affect the fundus examination and disc assessment were excluded.
Statistical analysisThe primary outcome was the agreement between glaucoma experts and each glaucoma experienced optometrist separately. Three possible diagnostic categorizations were considered both for gonioscopy and optic disc evaluation. Gonioscopic interpretation was categorized into “open”, “primary angle closure suspect” and “primary angle closure”. Optic discs were categorized into “normal”, “suspect” and “glaucomatous”. Weighted kappa statistics were estimated, assigning linear weights to disagreements among the above categories. Details of the kappa statistic have been explained elsewhere.17–19 To evaluate the diagnostic accuracy of gonioscopy and optic disc evaluation by the optometrist, all responses were pooled to calculate the sensitivity, specificity, predictive values and likelihood ratios. For this analysis, the suspect categories in both gonioscopy and optic disc interpretation were combined with the disease category for both optometrists and ophthalmologists. Likelihood ratio (LR) is the probability of a given test result in those with the condition, divided by the probability of the same test result in those without the condition. The LR for a given test result indicates how much that result will raise or lower the probability of disease. A LR of 1, or close to 1, would mean that the test provides no additional information about the post-test probability of the disease. LRs higher than 10 or lower than 0.1 would be associated with large effects on post-test probability, LRs from 5 to 10 or from 0.1 to 0.2 would be associated with moderate effects, LRs from 2 to 5 or from 0.2 to 0.5 would be associated with small effects.
Statistical analyses were performed using commercial software (Stata ver. 10.0; StataCorp, College Station, TX). A p value of <0.05 was considered statically significant.
ResultsSeparate cohorts of subjects were evaluated for agreement in gonioscopy and optic disc interpretation by both optometrists. Optometrist 1 performed gonioscopy in 72 subjects (male:female=41:31). Mean (±standard deviation) age of these subjects was 53±12 years (Range=25 to 80). Optometrist 2 performed gonioscopy in 77 subjects (male:female=46:31). Mean age of these subjects was 50±18 years (Range = 18 to 84).
Optometrist 1 performed optic disc evaluation in 94 subjects (male: female=59:35). Mean age of these subjects was 48±15 years (Range=18 to 74). Optometrist 2 performed optic disc evaluation in 100 subjects (male: female=60:40). Mean age of these subjects was 48±15 years (range, 18 to 80).
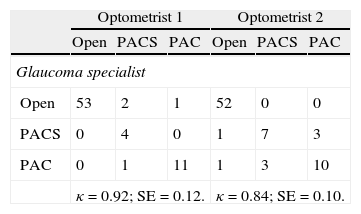
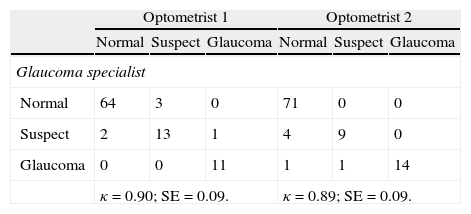
Tables 1 and 2 show the agreement between glaucoma specialist and each optometrist separately for gonioscopy and optic disc evaluation. κ was 0.92 for agreement between glaucoma specialist and optometrist 1, and 0.84 for agreement between glaucoma specialist and optometrist 2 in interpretation of gonioscopy. κ was 0.90 for agreement between glaucoma specialist and optometrist 1, and 0.89 for agreement between glaucoma specialist and optometrist 2 in interpretation of optic disc.
Agreement between glaucoma specialists and optometrists in interpretation of gonioscopy.
| Optometrist 1 | Optometrist 2 | |||||
| Open | PACS | PAC | Open | PACS | PAC | |
| Glaucoma specialist | ||||||
| Open | 53 | 2 | 1 | 52 | 0 | 0 |
| PACS | 0 | 4 | 0 | 1 | 7 | 3 |
| PAC | 0 | 1 | 11 | 1 | 3 | 10 |
| κ=0.92; SE=0.12. | κ=0.84; SE=0.10. | |||||
PACS: primary angle closure suspect; PAC: primary angle closure.
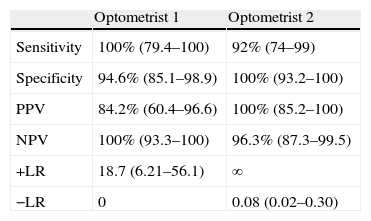
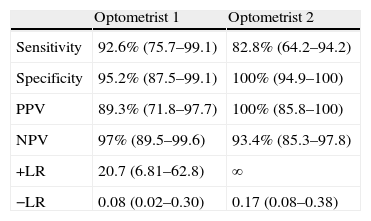
Tables 3 and 4 show the diagnostic accuracies of each optometrist separately for gonioscopy and optic disc evaluation. Gonioscopic evaluation by optometrists had sensitivities and specificities both above 90% to discriminate open from occludable angles. Positive and negative likelihood ratios were significant enough to have large effects on the post-test probability of having occludable angles. Optic disc evaluation by optometrists had specificities greater than 95% to discriminate normal from glaucomatous discs while the sensitivities were 83% and 93%. Positive and negative likelihood ratios were significant enough to have moderate to large effects on the post-test probability of having abnormal optic discs.
Diagnostic accuracies of optometrists in interpretation of gonioscopy.
| Optometrist 1 | Optometrist 2 | |
| Sensitivity | 100% (79.4–100) | 92% (74–99) |
| Specificity | 94.6% (85.1–98.9) | 100% (93.2–100) |
| PPV | 84.2% (60.4–96.6) | 100% (85.2–100) |
| NPV | 100% (93.3–100) | 96.3% (87.3–99.5) |
| +LR | 18.7 (6.21–56.1) | ∞ |
| −LR | 0 | 0.08 (0.02–0.30) |
Diagnostic accuracies of optometrists in interpretation of optic disc.
| Optometrist 1 | Optometrist 2 | |
| Sensitivity | 92.6% (75.7–99.1) | 82.8% (64.2–94.2) |
| Specificity | 95.2% (87.5–99.1) | 100% (94.9–100) |
| PPV | 89.3% (71.8–97.7) | 100% (85.8–100) |
| NPV | 97% (89.5–99.6) | 93.4% (85.3–97.8) |
| +LR | 20.7 (6.81–62.8) | ∞ |
| −LR | 0.08 (0.02–0.30) | 0.17 (0.08–0.38) |
Our results show that there is a high level of agreement between the expert glaucoma specialists and the experienced optometrists. In a situation where over 50% of the persons in developing countries with OAG are unaware that they have the disease,20 this method of training optometrists in gonioscopy and optic assessment can be expected to have a significant impact because it has the potential to make a larger cohort of diagnostically capable individuals available in locations where there is the greatest need. However, our main purpose is to compare the glaucoma trained optometrists and glaucoma specialist ophthalmologist, such that the results can be used to validate the use of the same glaucoma trained optometrists in the LVPEI-GLEAMS.
Various studies have shown that higher rates of visual impairment and blindness are associated with lower economic status and older age and these groups are commonly found in rural areas and in developing countries. As visual acuity assessment alone misses most cases of glaucoma and screening field tests can be ineffective, 21 the need for a more complete evaluation of each individual is evident.
Our results differ from those of Jampel and associates who found poor concordance between glaucoma experts in assessing disc change over time. The observers in that study were not trained however.22
There have also been agreement studies where photographs (stereo or non-stereo optic disc images) or direct ophthalmoscopic assessments were shown to ophthalmologist or optometrists with poor to moderate intra and inter observer reliability being the result. Again however varying levels of experience existed among the various observers23,24 and when clinical documentation of the optics discs through dilated pupils using a stereoscopic viewing system was used, intra-observer agreement improved.24 This approach helped evaluate subtle, early changes to the neuroretinal rim and the retinal nerve fiber layer.
Optic disc appearance has been suggested as the best reference standard for glaucoma diagnosis at present, despite the fact that it suffers from less-than-perfect inter observer agreement.22 Furthermore, standards of Preferred Practice Patterns stress the importance of including a range of appropriate examination techniques like gonioscopy, imaging and visual field tests during examination and diagnosis. While many physicians perform visual field tests and optic disc imaging, they frequently fail to assess the angle by gonioscopy.25 Hence, it has been recommended that vigilant examination of the optic disc and gonioscopy should be maintained during routine evaluation.20
The uniqueness of the current study lies in the involvement of gonioscopy, as listed in the UK NICE guidelines, April 2009 as essential competence for those providing glaucoma care26 and our data provide the first assessment of the diagnostic accuracy of the trained optometrist in this regard.
One limitation of the current study was that for logistical reasons it was not possible to assess agreement among the three glaucoma specialists. The assumption that there exists substantial agreement cannot be formally verified. In conclusion, our results show that there is a high level of agreement between glaucoma specialists and trained optometrists in gonioscopy and optic disc assessment. We suggest that the reason for the significantly higher agreement than has been reported previously is the fact that both optometrists had high levels of glaucoma patient experience gained from working with same consultants for many years. As a consequence they were able to develop judgement criteria similar to those of the supervising consultant ophthalmologists. This suggests that the optometrist with good experience and clinical skills, if trained in optic disc assessment and gonioscopy, can appropriately diagnose glaucoma using these indicators. This adds to and reinforces previous work demonstrating similar results based on the assessment of the optic disc. In situations where glaucoma specialist ophthalmologists are unavailable for whatever reason, we propose therefore, that it would be reasonable to utilize optometrists to facilitate the screening and diagnosis of glaucoma, provided that they have been suitably trained and have access to the appropriate equipment.
Conflicts of interestThe authors have no conflicts of interest to declare.