The present case study is of an 8-year old male who was found to have refractive instability due to corneal distortions that were associated with chronic habit of abnormal eye rubbing (CHAR). Psychiatric evaluation and treatment alleviated the CHAR and at the same time refraction stabilized and the cornea resumed a regular shape. Treatment of this case was made possible by close collaboration between the health care professionals caring for this child.
El presente caso de estudio se refiere a un varón de 8 años que fue diagnosticado de inestabilidad refractiva debida a distorsiones corneales asociadas al hábito crónico de frotamiento anormal de los ojos (CHAR). La evaluación y el tratamiento psiquiátricos aliviaron dicho hábito, lo que al mismo tiempo estabilizó la refracción y repuso la córnea a una forma regular. El tratamiento de este caso fue posible mediante la estrecha relación entre los profesionales de cuidados sanitarios que atendieron a este niño.
Refractive error has been documented to change as a result of epithelial thinning, which is the basis of myopic Ortho-K treatment.1 In keratoconus (KC), thinning of the stroma layer of the cornea results in a corneal protrusion forming a conical shape, with a severe effect on refraction.2–4
Attention-deficit/hyperactivity disorder (ADHD) is characterized by problems with attention, impulsivity, and hyperactivity.5 In children, attention deficit hyperactivity disorder (ADHD) is associated in 60–100% of all cases with at least one other psychiatric diagnosis. These include oppositional defiant disorders in 50–60%, depressive syndromes in 16–26% and anxiety disorders in about 15% of all children with ADHD as well as tic disorders and developmental disorders like reading and spelling disorders.6 Another report indicates that approximately 30–40% of children with attention-deficit/hyperactivity disorder (ADHD) meet the criteria for a comorbid anxiety disorder in clinical samples.7
This report, presents the case of an 8-year old child with ADHD who suffered from anxious thoughts and whose CHAR appears to have caused severe corneal distortions leading to changes in refractive error. Pharmacological treatment for ADHD alleviated the CHAR consequently restoring the corneal topography returned to a normal pattern.
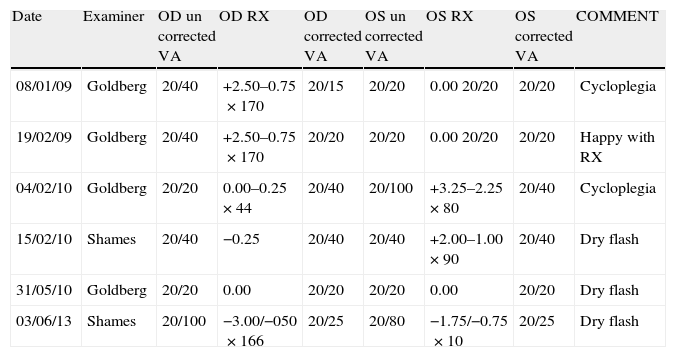
Case presentationAn 8-year old male presented to an ophthalmologist with a complaint of difficulty in reading. Initial work-up revealed anisometropia. Cycloplegic refraction was performed and spectacles were prescribed based on the cycloplegic refraction (Table 1, 08/01/09). No additional pathology was noted in either the anterior or posterior segment. Symptoms of ocular itch, allergies or sensitivity were not observed nor were a history of such reported by the mother. Uncorrected visual acuity was right eye (OD) 20/40 and left eye (OS) 20/20, while best corrected VA was OD 20/40 OS 20/20. Six weeks later the patient was doing well with a stable refraction (Table 1, 19/02/09). Corrected VA was 20/20 OU.
Refractive error over time.
| Date | Examiner | OD un corrected VA | OD RX | OD corrected VA | OS un corrected VA | OS RX | OS corrected VA | COMMENT |
| 08/01/09 | Goldberg | 20/40 | +2.50–0.75×170 | 20/15 | 20/20 | 0.00 20/20 | 20/20 | Cycloplegia |
| 19/02/09 | Goldberg | 20/40 | +2.50–0.75×170 | 20/20 | 20/20 | 0.00 20/20 | 20/20 | Happy with RX |
| 04/02/10 | Goldberg | 20/20 | 0.00–0.25×44 | 20/40 | 20/100 | +3.25–2.25×80 | 20/40 | Cycloplegia |
| 15/02/10 | Shames | 20/40 | −0.25 | 20/40 | 20/40 | +2.00–1.00×90 | 20/40 | Dry flash |
| 31/05/10 | Goldberg | 20/20 | 0.00 | 20/20 | 20/20 | 0.00 | 20/20 | Dry flash |
| 03/06/13 | Shames | 20/100 | −3.00/−050×166 | 20/25 | 20/80 | −1.75/−0.75×10 | 20/25 | Dry flash |
One year later the patient returned to the ophthalmologist complaining of trouble with his current prescription (Table 1, 04/02/10). Ophthalmologic exam revealed a large shift in refraction in both eyes, anisometropia and reduced VA in both eyes. The patient was referred for repeat refraction by an optometrist. All other findings were normal: no ocular itch was reported, slit lamp and ophthalmascope exams were within normal limits and no corneal staining was found. Two weeks later (Table 1, 15/02/10), retinoscopy revealed scissor reflex in both eyes, anisometropia and reduced VA in the left eye. Visual acuity of 20/20 was not achieved in either eye. Keratometry showed distorted mires in both eyes. Slit lamp and ophthalmoscopy exams were normal. Keratoconus (KC) was suspected and the patient was referred for videokeratography (VKG) and wavefront aberrometry. On history, the patient's mother noted that the child constantly rubs his eyes, but did not complain of itchy or watery eyes. Mother described child as being very sensitive.
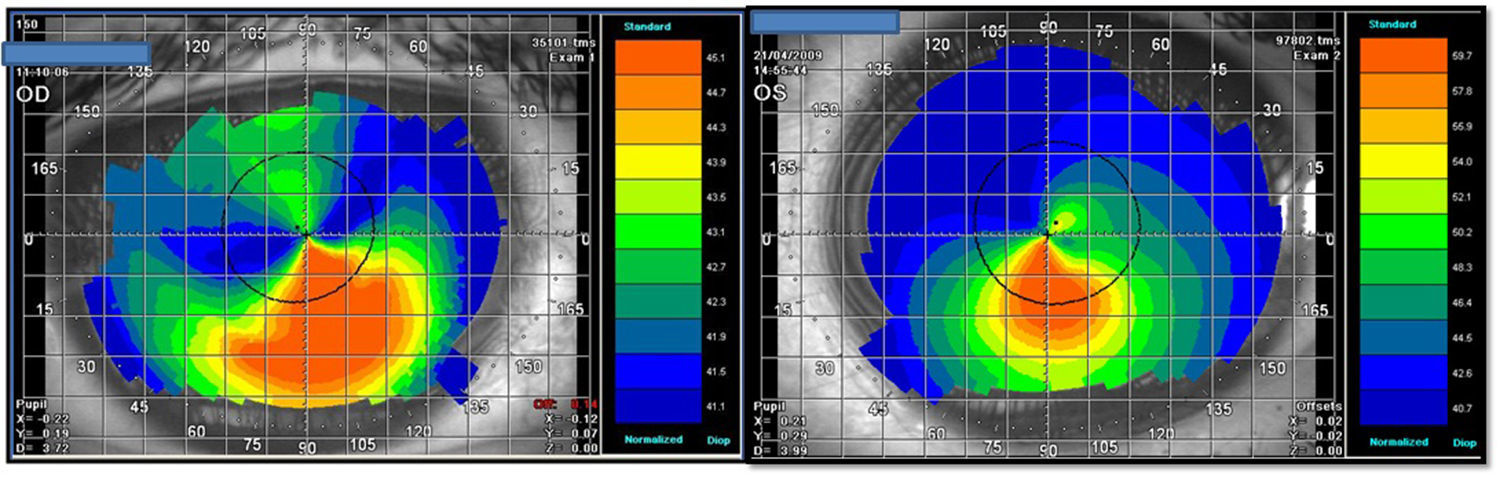
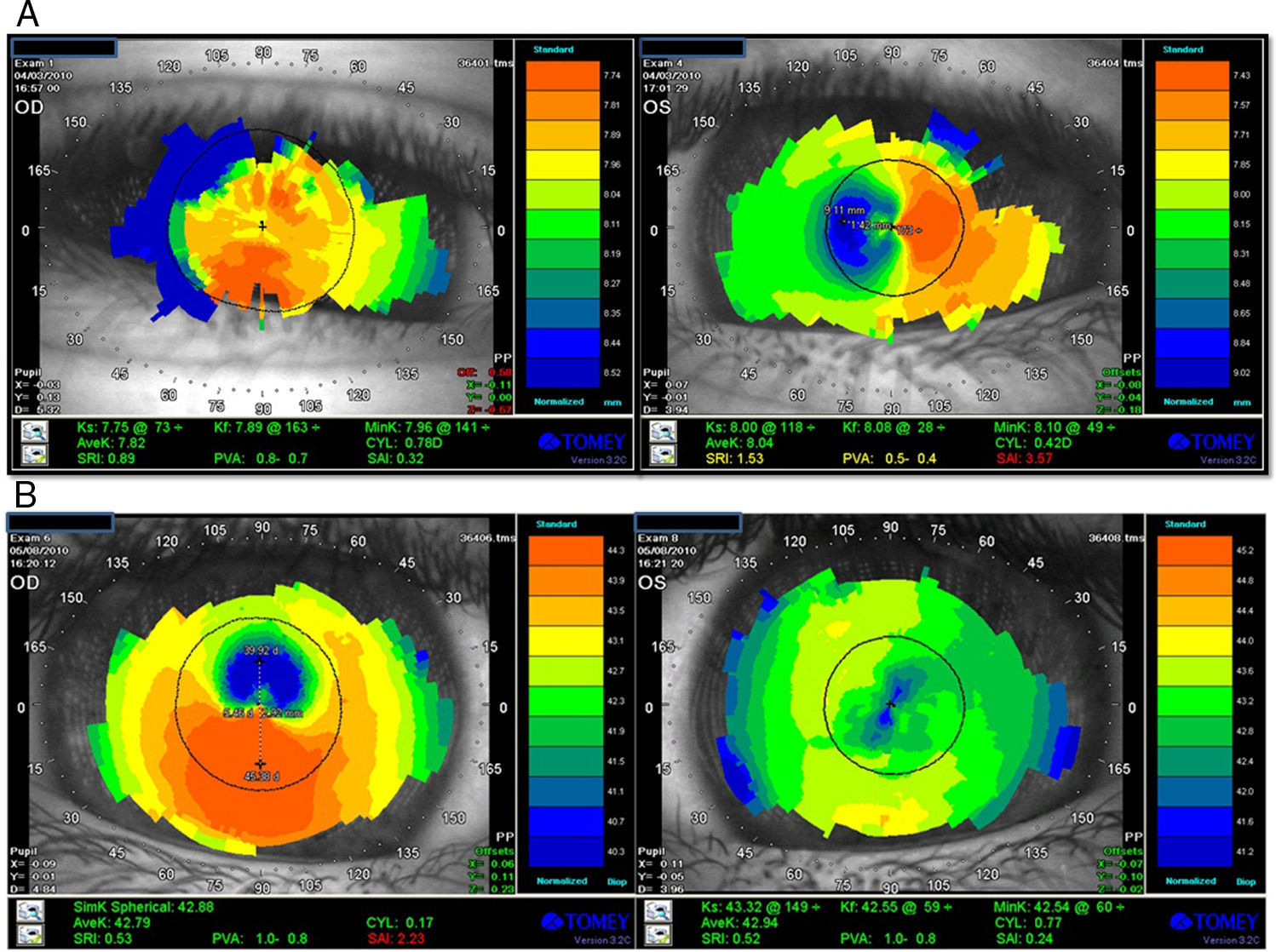
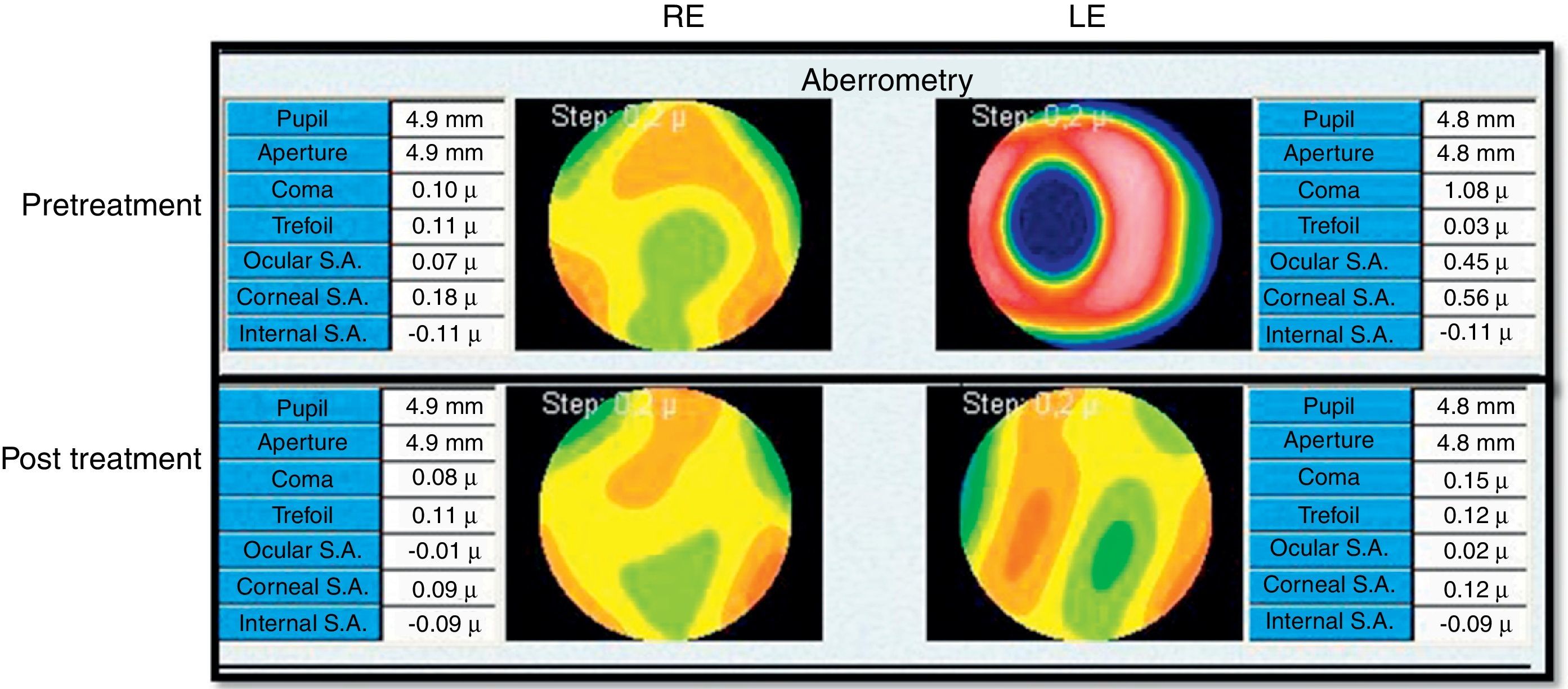
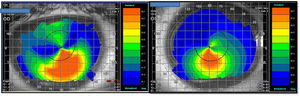
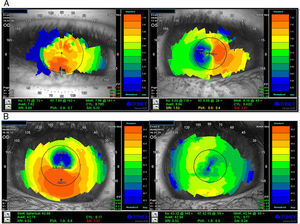
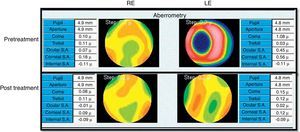
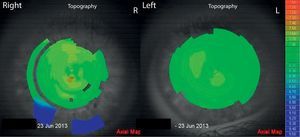
VKG (Tomey TMS-4) showed distortions in both corneas (Fig. 2), but not a typical skewed asymmetrical bowtie as usually seen in KC3 (see Fig. 1 for comparison). The astigmatism found in the VKG was different from that found in the subjective refraction and retinoscopy. During the corneal mapping the patient struggled to keep the OD open and otherwise cooperating in the VKG examination of that eye so that the VKG output may not accurately indicate his corneal topography. Wavefront aberrometry with a Hartmann Shack device (L80 Wave+, Luneau, FR) showed an aberrant pattern, with coma and total ocular spherical aberration being the dominant aberrations in the OS (Fig. 3). In KC, coma is often observed as the most aberrant part of the wavefront.8 Due to the fact that also during the aberrometry measurements the patient encountered difficulty keeping the OD open, the wavefront data might not reflect the actual pattern in this eye. The patient was referred to his pediatrician to discuss treatment for ADHD and to possibly to help alleviate his CHAR. The pediatrician subsequently referred him for psychiatric evaluation.
The patient presented to the psychiatrist with a history of carelessness, losing things, difficulty sustaining attention, difficulty following through on instructions, difficulty organizing tasks, excessive talking, impulsivity, rage outbursts, and sensory processing problems. In addition, he exhibited anxiety relating to the well-being of family members, leading to the need for ongoing reassurance. Mother also described CHAR. The patient met criteria for ADHD, and though he did not meet criteria for a specific anxiety diagnosis, he was definitely impaired by his anxious thoughts. It was not clear whether his eye rubbing was a result of his impulsive fidgeting, or was a compulsive behavior etiologically connected to his anxiety. Play therapy was recommended to treat his anxiety, and treatment with Ritalin (10mg, twice a day) was initiated to target his inattentive and impulsive behaviors. The patient's mother was asked to note the prevalence of CHAR.
At a 2-month follow-up, the patient's ADHD symptoms were relieved, and a significant reduction in the eye rubbing was reported. Ophthalmological follow-up three months later revealed spontaneous emmetropia in both eyes with an uncorrected vision of 6/6 in both eyes (Table 1, 31/05/10). Repeat VKG by the optometrist revealed marked reduction in the corneal distortion (Fig. 2b) alongside improved ocular wavefront findings (Fig. 3). Ophthalmascope and slit lamp exams were within normal limits and no staining was found.
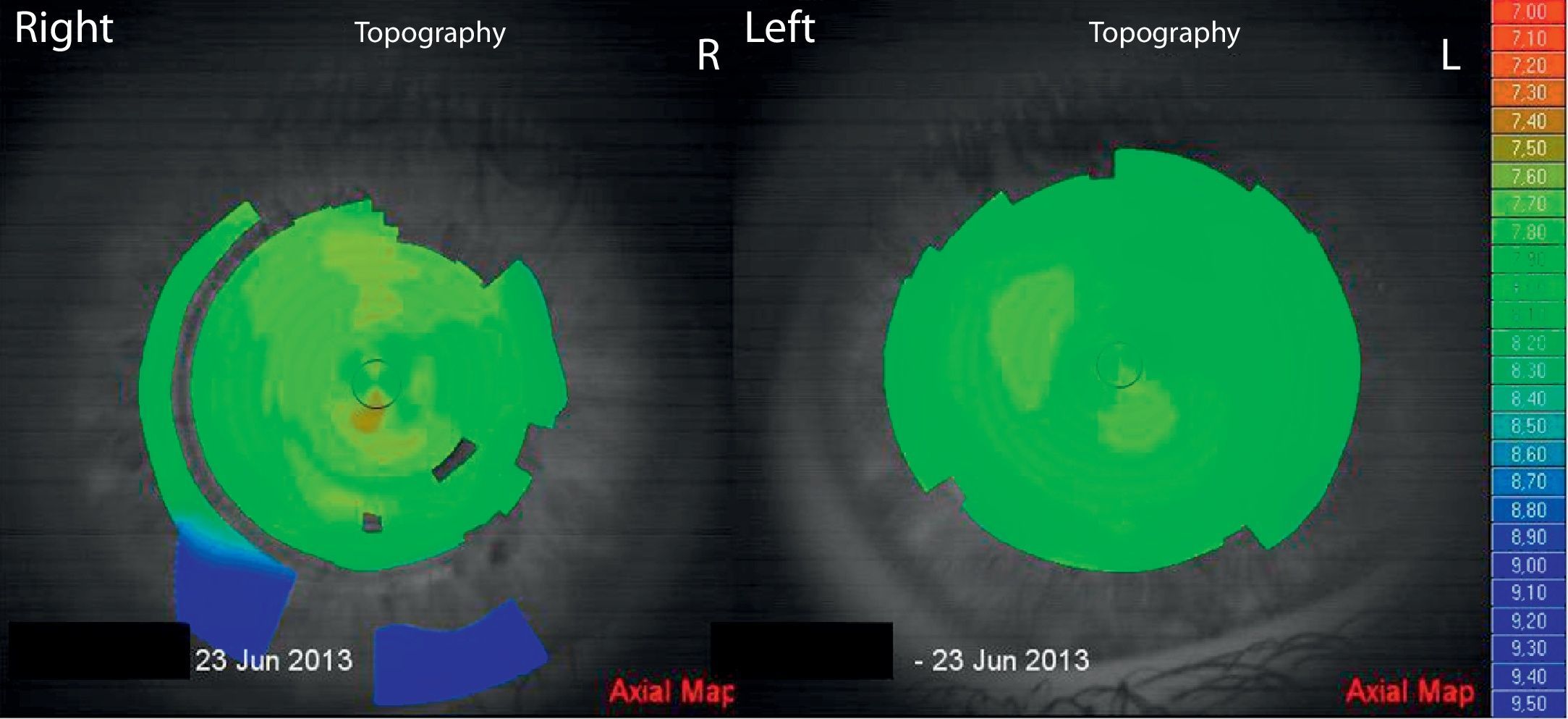
Three years later the patient returned to the optometrist. He presented without any ocular complaints. The mother reported that the child does not suffer from allergies or ocular itch and does not exhibit CHAR. Ophthalmoscopy and slit lamp showed no abnormal findings. Refraction showed a moderate amount of anisometropia and slight regular astigmatism with OD-3.00/-0.50X 166 OS-1.75/-0.75X10 (Table 1, 31-05-13). Visual acuity was corrected to 20/25 in each eye. Difficulty concentrating on the subjective refraction was apparent. VKG was performed with the L80 wave+ and both corneas exhibited a regular symmetrical topography pattern (Fig. 4). The K readings were found: OD 7.76mm/7.64mm (43.5 D/44.1 DX 7), OD 7.86/7.73 (42.9 D/43.6 DX 42). Sheimpflug camera imaging (Sirius, CSO, Florence) showed corneal thickness at the thinnest point to be 503.9μm and 511.6μm for OD and OS, respectively. All anterior chamber parameters were within the range found for normal corneas.
The psychiatrist currently reports that the patient continues to struggle with his ADHD symptoms. His impulsivity affects his academic and social performance. He is taking Concerta 27mg, daily. In general, his self care, including resisting rubbing his eyes, is greatly improved.
DiscussionWe described a pediatric patient presenting with unstable refraction, anisometropia and abnormal topography and aberrometry who suffered from CHAR, without a history of ocular itch or allergy. Psychiatric evaluation showed ADHD complicated by anxious thoughts. Pharmacological treatment of ADHD and play therapy for anxiety resulted in control of obsessive behavior, including CHAR. This improvement was associated with a marked improvement in refraction, corneal topography and aberrometry. Long term follow-up revealed that the patient is still struggling with his psychiatric conditions, but CHAR is under control, as is his topography and refraction.
Anisometropia presented at several visits. It is possible that CHAR was worse in one eye and therefore led to larger shifts in the refraction in that eye. Similarly, asymmetric KC has been found to be associated with abnormal eye rubbing of the more severely affected eye.9–11
The astigmatism found in the VKG was different from that found in the subjective refraction and retinoscopy. However, refraction and retinoscopy were carried out on a different day than the VKG. The cornea of a child is very flexible and rapid changes in corneal shape could conceivably take place, accounting for the discrepancy.12 OD did not exhibit a large change in aberrometry data after treatment. However, data from the corneal topography and wavefront (04.03.10) from OD may not be accurate since the patient had difficulty opening this eye during these procedures.
One of the most important factors strongly associated with the progression of KC can be the chronic habit of abnormal eye rubbing (CHAR). This association has been demonstrated by numerous case series and large case controlled studies3,13,14,2,15–18 and by meta-analysis.19 Multiple reports link vigorous eye rubbing to the development of acute hydrops.20–22 Several case studies demonstrate that unilateral KC is observed in subjects with CHAR. Mashor23 describes three patients who presented with unilateral KC who also had Tourette Syndrome (TS). Patients’ histories revealed asymmetric or unilateral rubbing of the affected eye as a result of a TS tic without any other organic causes. Ioannidis24 describes a 7-year old patient who presented with unilateral KC associated with chronic eye rubbing and no other organic cause. Nocturnal padding to reduce eye rubbing stabilized the dystrophy of the cornea. Coyle25 report the occurrence of unilateral KC in a boy who used digital massage of the affected eye to control episodes of paroxysmal atrial tachycardia.
The mechanism by which CHAR may cause KC is not clear. Gritz26 suggests that the microtrauma of eye rubbing by susceptible individuals injures the epithelium, leading to cytokine release, myofibroblast differentiation, a change in biomechanical forces, and thinning of corneal tissue. This cascade of events might produce the ectatic process recognized as KC. In fact, it has been suggested that trauma may be the common underlying factor in eye rubbing, vernal and atopic disease, contact lens wear, and Down Syndrome that, via a common biochemical cascade, leads to development of KC.9 McMonnies also hypothesizes that a reduction in shear strength and cone-forming deformation may be the responses to rubbing trauma.15 This case study presents further evidence suggesting that CHAR may cause corneal distortions that significantly affect refraction. However, the topographic pattern was not a typical KC pattern and pachymetry was not performed, so we cannot be certain that the CHAR caused any corneal thinning. Nevertheless, the corneal distortions appeared with the CHAR and were alleviated when the CHAR was treated, implying a causative mechanism.
ADHD is characterized by chronic problems in attention and impulse control, age-inappropriate hyperactive behaviors as well as emotional dysregulation including tantrums or mood swings.7 Along with ADHD, the patient experienced considerable anxiety and was impaired by anxious thoughts, despite not meeting the criteria for a specific anxiety disorder. CHAR is thought to have a calming effect on anxiety via the oculocardiac reflex.27 Thus, the patient may have been using CHAR as a means to calm his anxiety. Play therapy and pharmacological treatment might have been effective in reducing the anxiety and reducing the urge for CHAR.
Health care professionals have long recognized the value of interdisciplinary collaboration. However, many obstacles prevent professionals from regularly consulting or working on teams with other health care providers. These obstacles include professional parochialism, competition for clientele, lack of understanding about other professionals’ knowledge and skills, busy schedules and separate office facilities.28 As optometry develops and the optometric practitioner concerns himself with this broader scope of practice: e.g. vision therapy, developmental vision care etc., as opposed to primarily refraction, the more he becomes more aware that he must understand the patient as a whole before successfully dealing with the patient's visual system. In addition, familiarity with the patient as a person can also assist with the visual treatment. This case illustrates that vision is but one aspect of an integrated organism with physical, emotional and intellectual components29 and that a multidisciplinary approach can most appropriately address a patient's needs in some cases.
ConclusionMarked swings in refraction in a pediatric patient should alert the treating eye care professionals to possible self induced corneal trauma. Interdisciplinary care of such patients can significantly improve their outcome. In this case, the patient benefitted from interdisciplinary treatment from his pediatrician, ophthalmologist, optometrist and psychiatrist. This case demonstrates the need for interaction and communication between different disciplines for holistic treatment of complicated patients.
Conflicts of interestThe author has no conflicts of interest to declare.
We would like to thank Prof. Michel Millodot for advice and Dr. Liat Gantz for critical reading of the manuscript.