To evaluate distance, intermediate and near visual performance in patients who had undergone implantation of the multifocal aspheric AcrySof ReSTOR intraocular lens (IOL).
MethodsBinocular best distance corrected visual acuity (BCVA) at high and low contrast [4m], best distance corrected near visual acuity (BCNVA) [40 cm], intermediate visual acuity [80 and 60 cm], and distance contrast sensitivity (CS) under photopic [85cd/m2] and mesopic [3cd/m2] conditions, were measured in 36 eyes that underwent implantation of the AcrySof ReSTOR Aspheric IOL (SN6AD3).
ResultsAt the 3-month postoperative visit, binocular BCVA was -0.058±0.091, 0.200±0.079, and 0.258±0.071 logMAR, for 100%, 25% and 12.5% of contrast, respectively. Binocular BCNVA was -0.025±0.062 logMAR. Intermediate visual acuity varied significantly as a function of the distance to the test (P<0.01), but all patients showed 20/25 or better visual acuity at any distance. Photopic CS was within the standard normal range. Under mesopic conditions CS was lower particularly at higher spatial frequencies compared to photopic conditions.
ConclusionsThe AcrySof ReSTOR Aspheric IOL provide good high-contrast visual acuity at both distance and near; and CS at photopic and mesopic conditions. Intermediate vision is improved in relation to that found with the spherical AcrySof ReSTOR model.
Evaluar la calidad visual para visión lejana, intermedia y cercana en pacientes a los que se les ha implantado una lente intraocular (LIO) multifocal asférica AcrySof ReSTOR.
MétodosSe midió la agudeza visual binocular con la mejor corrección (en inglés, BCVA) de alto y de bajo contraste [4m], la agudeza visual cercana [40cm] con la mejor corrección para lejos (en inglés, BCNVA), la agudeza visual intermedia [80 y 60cm] con la mejor corrección para lejos, y la sensibilidad al contraste (SC) lejana en condiciones tanto fotópicas [85cd/m2] como mesópicas [3cd/m2]: todo esto en 36 ojos en los que se había implantado una LIO asférica AcrySof ReSTOR (SN6AD3).
ResultadosEn la revisión realizada 3 meses después de la operación, la BCVA binocular fue de -0,058±0,091, 0,200±0,079 y 0,258±0,071 (escala logMAR), para un contraste, respectivamente, del 100%, del 25% y del 12,5%. La BCNVA binocular fue de -0,025±0,062 logMAR. La agudeza visual intermedia varió significativamente en función de la distancia al test (P<0,01), pero para todos los pacientes y todas las distancias evaluadas se obtuvieron valores de agudeza visual de 20/25 o mejores. Los valores de la SC fotópica están dentro del intervalo habitual. En condiciones mesópicas la SC fue inferior a la obtenida para iluminación fotópica, particularmente para las frecuencias espaciales más elevadas.
ConclusionesLa LIO asférica AcrySof ReSTOR proporciona una buena agudeza visual de alto contraste, tanto de lejos como de cerca, y una buena SC en condiciones fotópicas y mesópicas. La visión intermedia mejora, en relación con lo hallado para el modelo esférico de AcrySof ReSTOR.
Implantation of pseudoaccommodative intraocular lenses (IOLs) has gained wide popularity among ocular surgeons. These IOLs are designed to reduce dependence on eyeglasses after cataract or refractive lens exchange surgery. Monofocal IOLs provide excellent visual function but for many patients their limited depth-of-focus means that they cannot provide clear vision at both distance and near.
It remains for optical scientists to design a pseudoaccommodative IOL that provides unaberrated optical imagery at all focal distances. Two separate focal points along the optical axis are generated to provide good unaided distance and near vision as well as functional intermediate vision. Current designs of pseudoaccommodative IOLs use diffractive optics1-5, zones of differing refractive power6-9 or both principles (hybrid IOLs)10-13. Recent studies performed on hybrid AcrySof ReSTOR IOL pointed out satisfactory visual results. An improvement of this concept was recently introduced by the same company on an aspheric platform under the name AcrySof ReSTOR Aspheric IOL. The addition of asphericity aims to reduce unwanted visual phenomena, associated with multifocal IOL performance, and to increase the range of focus improving image quality. Then, it is expected to obtain good distance and near vision as well as (due to the asphericity) functional intermediate vision.
The purpose of this study was to assess distance, intermediate and near visual acuity, distance contrast sensitivity (CS) under photopic and mesopic conditions in patients who had undergone bilateral implantation of the AcrySof ReSTOR Aspheric IOL in the capsular bag after lens extraction.
Patients and MethodsStudy DesignWe prospectively examined 36 eyes of 18 consecutive patients who underwent bilateral implantation of the AcrySof ReSTOR Aspheric IOL (SN6AD3 model) at the Fernández-Vega Ophthalmological Institute (Oviedo, Spain). Inclusion criteria were age between 50 and 70 years, bilateral implantation (considering the visual benefit of bilateral implantation12) and their motivation: the desire to no longer wear any form of spectacle or contact lens correction for distance and near. Exclusion criteria included ≥1D of corneal astigmatism, history of glaucoma or retinal detachment, corneal disease, previous corneal or intraocular surgery, abnormal iris, pupil deformation, macular degeneration or retinopathy, neuro-ophthalmic diseases and history of prior ocular inflammation.
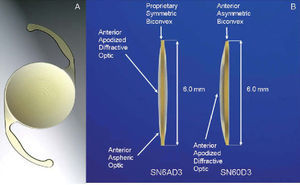
The AcrySof ReSTOR aspheric multifocal IOL combined the functions of both apodized diffractive and refractive regions (Figure 1). The apodized diffractive optics is found within the central 3.6 mm optic zone of the anterior surface of the IOL. This area comprises 12 concentric steps of gradually decreasing (1.3-0.2 microns) step heights creating a multifocality from near to distant (2 foci). The refractive region of the optic surrounds the apodized diffractive region. This area directs light to a distance focal point for larger pupil diameter, and is dedicated to distance vision. The IOL has a symmetric biconvex design with an anterior aspheric optic to reduce whole-eye spherical aberration (The IOL has a negative spherical aberration of -0.10 μm for a 6 mm pupil). The aspheric optics flattens the edge and reduces the central thickness (about 4.5% thinner for a 20D IOL compared to the spherical model14). The overall diameter of the lens is 13.0 mm and the optical diameter is 6.0 mm. Lens power varied from +10.0 D to +30.0 D incorporating a +4.0 D near addition power. The AcrySof ReSTOR Aspheric IOL is manufactured with a material which includes a blue-light-absorbing chromophore designed to approximate more closely the light-transmittance characteristics of the natural lens at wavelengths below approximately 500 nm. It has been shown that the use of this blue-light filter would be more advisable because it avoids retinal ultraviolet light alterations without disturbance of CS12,13 and chromatic vision15,16.
All surgeries in this study were operated by phacoemulsification with the Infiniti Vision System (Alcon, Fort Worth, TX) using topical anaesthesia and a clear corneal 2.2-3.2 mm incision performed by two experienced surgeons (J.F.A., L.F.V.). Phacoemulsification was followed by irrigation and aspiration of the cortex, and IOL implantation in the capsular bag. There were no complications in any of the cases. The tenets of the Declaration of Helsinki were followed in this research. Informed consent was obtained from all patients after the nature and possible consequences of the study were explained. Institutional Review Board approval was obtained.
Patients were scheduled for clinical evaluation preoperatively and 1 day, 1 month, and 3 months postoperatively. Standard ophthalmologic examination, including manifest refraction, slit-lamp biomicroscopy, Goldmann applanation tonometry, and binocular indirect ophthalmoscopy, was performed at all visits.
Visual Performance MeasurementsBinocular uncorrected distance visual acuity (UCVA) and best-corrected distance visual acuity (BCVA) were measured by means of the logarithm of the minimum angle of resolution (logMAR) for 100% contrast EDTRS charts under photopic conditions (85cd/m2) with the Optec 6500 at 4m (Stereo Optical Company, CA). BCVA was also measured at low contrast with the 25% and 12.5% contrast EDTRS charts. Binocular uncorrected distance near visual acuity (UCNVA) and best distance-corrected near visual acuity (BCNVA) were measured by means of the Precision Vision Logarithmic Visual Acuity Chart 2000 New EDTRS at 40cm under photopic conditions (85 cd/m2). Binocular best distance-corrected intermediate visual acuity (BCIVA) was measured at 60 and 80 cm with the same test used for near assessment but adjusting for the distance.
Binocular photopic (85cd/m2) and mesopic (3cd/m2) CS was measured with the best distance correction using the Optec 6500 with a Functional Acuity Contrast Test chart. Absolute values of log10 CS were obtained for each combination of patient, spatial frequency and luminance, and means and standard deviations were calculated.
The pupil diameter in distance vision was measured in each patient under the two levels of illumination by means of a pupillometer (Colvard pupillometer, OASIS, Irvine, CA) before and after IOL implantation. Tilt and centration of the multifocal IOL in relation to the visual axis was assessed using a Scheimpflug videophotography system (EAS-1000, Nidek).
Data AnalysisAll examinations were performed at 3 months after implantation by one ophthalmic technician who was unaware of the objective of the study. Data analysis was performed using SPSS for Windows version 12.0 (SPSS Inc., Chicago, IL). Differences were considered to be statistically significant when the P value was <0.01 (i.e., at the 1% level). To explore any correlation between the visual acuity measured at different distances (far, intermediate and near), a one-way ANOVA test was carried out, in which the interactions between the changes in visual acuity and the distance of the test were assessed. Statistical significance of any intergroup CS differences was assessed with a t-test (absolute log CS values) at each frequency for both illumination conditions.
ResultsEighteen patients were enrolled in this study. The mean age of the 7 men and 11 women was 61.0±6.6 years (range 50 to 70 years). Mean IOL power was 21.04±2.93 D. Patient demographics are shown in table 1. After the surgery and IOL implantation, the pupils of all patients were round, without iris trauma, and showed a good responsiveness to light. All cases showed good centration and no tilt of the IOLs.
Demographic characteristics of participants
| AcrySof ReSTOR Aspheric IOL (SN6AD3) | |
| Number of eyes | 36 |
| Age (years) | 61.0±6.6 |
| Gender (Male/Female) | 7/11 |
| IOL Power (D) | 21.04±2.93 |
| Axial Length (mm) | 23.51±1.00 |
| Preoperative Sphere (D) | 0.15±2.13 |
| Preoperative Cylinder (D) | -0.54±0.46 |
| Postoperative Sphere (D) | -0.08±0.35 |
| Postoperative Cylinder (D) | -0.35±0.35 |
| Pupil diameter (mm) | |
| Photopic (85cd/m2) | 3.6±0.5 |
| Mesopic (3cd/m2) | 5.0±0.6 |
IOL = intraocular lens; mean ± standard deviation.
The means and standard deviations of binocular visual acuity for distance, intermediate and near vision are summarized in table 2.
Binocular visual acuity results for distance, intermediate and near vision. Mean and standard deviation logMAR (logarithm of the minimum angle of resolution) values for the AcrySof ReSTOR Aspheric IOL (SN6AD3) at 3 months after the implantation.
| AcrySof ReSTOR Aspheric IOL (SN6AD3) | |||
| Mean | 20/40 or better | 20/25 or better | |
| Distance (4m) | |||
| UCVA | 0.050±0.188 | 16/18 (88.8%) | 14/18 (77.7%) |
| BCVA | -0.058±0.091 | 18/18 (100%) | 18/18 (100%) |
| Low contrast BCVA (25%) | 0.200±0.079 | 18/18 (100%) | 4/18 (22.2%) |
| Low contrast BCVA (12.5%) | 0.258±0.071 | 18/18 (100%) | 2/18 (11.1%) |
| Intermediate (80cm) | |||
| BCIVA | 0.222±0.065 | 18/18 (100%) | 18/18 (100%) |
| Intermediate (60cm) | |||
| BCIVA | 0.201±0.082 | 18/18 (100%) | 18/18 (100%) |
| Near (40cm) | |||
| UCNVA | -0.005±0.085 | 18/18 (100%) | 15/18 (83.3%) |
| BCNVA | -0.025±0.062 | 18/18 (100%) | 18/18 (100%) |
UCVA= uncorrected distance visual acuity; BCVA= best-corrected distance visual acuity; BCIVA= best-corrected distance intermediate visual acuity
UCNVA= uncorrected distance near visual acuity; BCNVA= best distance-corrected near visual acuity.
Mean UCVA was 0.050 logMAR (about 20/20). When post-operative residual refractive error was corrected (see table 2) it improved to -0.058 logMAR (>20/20). 100% of the patients achieved a BCVA of 20/25 or better. Low contrast BCVA was 0.200 (20/32) and 0.258 (20/40) logMAR for 25% and 12.5% of contrast, respectively. In both cases, 100% of the patients achieved a BCVA of 20/40 or better. However, these percentages were reduced to 22.2% and 11.1%, respectively, for a BCVA of 20/25 or better. For a detailed description of the efficacy at different contrast under corrected and uncorrected conditions see table 2.
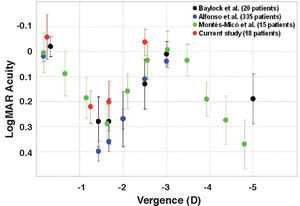
Intermediate Visual AcuityMean BCIVA was 0.222 and 0.201 logMAR (about 20/32) for 80cm and 60cm, respectively. At both distances, 100% of the patients achieved a BCVA of 20/25 or better. To better illustrate the change in visual acuity at different distances, figure 2 was created. The mean value ranged from -0.005 logMAR (about 20/20) at 40cm to 0.201 and 0.222 logMAR (about 20/32) at 60 and 80cm, respectively. Red circular symbols in figure 2 show the post-implantation, through-focus, best-corrected binocular logMAR visual acuity. Data of Blaylock et al.18 (black circles), Alfonso et al.12 (blue circles) and Montés-Micó et al.19 (green circles) with the ReSTOR Natural IOL have been included for comparison. The one-way ANOVA revealed a statistically significant variation in the intermediate visual acuity as a function of the distance to the test for the AcrySof ReSTOR aspheric IOL (P<0.01).
Mean, high-contrast, binocular visual acuity (logMAR) with a best correction for distance vision, as a function of the chart vergence for the AcrySof ReSTOR aspheric IOL (SN6AD3 model). Red circular symbols show data from the present study, black symbols are data from Blaylock et al.18 (SN60D3 model), blue symbols from Alfonso et al.12 (SN60D3 model) and green symbols from Montés-Micó et al.19 (SN60D3 model). Data from Baylock et al.18, Alfonso et al.12, and for the present study were obtained by varying the chart distance and from Montés-Micó et al.19 by altering chart vergence with lenses (last one was corrected for lens effectivity and spectacle magnification at the 15mm vertex distance used). Note that some points on the graph at the same vergence were slightly displaced to facilitate visualization.
Mean binocular UCNVA and BCNVA were -0.005 and 0.037 logMAR (about 20/20 in both cases), respectively. In both situations, uncorrected and best distance corrected, all patients (100%) achieved a visual acuity of 20/40 and better. 83.3% and 100% of the patients achieved a UCNVA and a BCNVA of 20/25 or better, respectively.
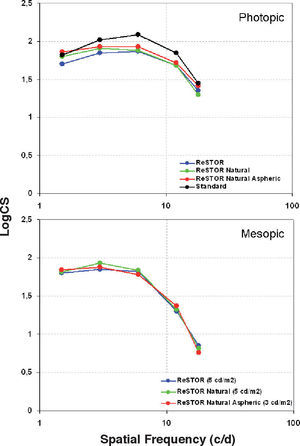
CS under Bright and Dim ConditionsThe mean values of log10CS are plotted as a series of CS Functions (CSFs) in figure 3 for the two luminance levels. For comparison, data corresponding to the standard photopic CSF17, to the CSF for the AcrySof ReSTOR (SA60D3) and to that for the AcrySof Natural ReSTOR (SN60D3) IOLs were included12. Under photopic conditions (85 cd/m2), the performance was very similar for all groups and was close to the standard CSF. At a mesopic level of 3cd/m2, however, the CS for all groups was generally lower, particularly at higher spatial frequencies. No statistically significant differences in photopic and mesopic log10CS were found between the three groups at all spatial frequencies (P>0.1).
Photopic and mesopic binocular contrast sensitivity functions for the AcrySof ReSTOR aspheric IOL (SN6AD3 model). For comparison, we included the mean values obtained for the AcrySof ReSTOR as well as the AcrySof ReSTOR Natural IOLs as found by Alfonso et al.12, and standard values typical of healthy eyes9. Note the different lighting condition for mesopic examination across studies (5cd/m2 versus 3cd/m2). Standard deviation error bars have been omitted for clarity.
Previous clinical trials evaluating clinical, optical, functional and quality-of-life outcomes after AcrySof ReSTOR IOL implantation10-13,18,19 have shown that this IOL can improve near vision while providing a good level of distance vision. Multifocal patients reported less limitation in visual function and less spectacle dependency than patients with bilateral monofocal IOLs. In the current study, we have assessed the performance of the new AcrySof ReSTOR aspheric IOL. This IOL is based on the previous ReSTOR IOL but improving its optical design with aspheric technology to achieve better visual outcomes. We have evaluated visual acuity and CS measured at different distances and lighting conditions in patients implanted with this IOL.
Our study shows an excellent binocular BCVA, with 100% of the patients having BCVA of 20/25 or better at 3 months (Table 2). Kohnen et al.10 using the AcrySof ReSTOR IOL (SA60D3) reported similar values and percentages of binocular BCVA in 118 patients at 120-180 days after the surgery (mean BCVA of -0.05 logMAR (>20/20); 100% of the patients with 20/40 or better and 97.5% of the patients with 20/25 or better). Alfonso et al.12 on a sample of 335 patients implanted with the AcrySof Natural ReSTOR IOL (SN60D3) at 6 months found a mean BCVA of 0.01 logMAR (about 20/20) and 100% of the patients with 20/40 or better and 95.5% of the patients with 20/25 or better. No comparison with previous studies about the visual performance of the AcrySof ReSTOR aspheric is possible because this is the first study that evaluates it. However, mean BCVA values found with the new aspheric IOL are similar to those found in other studies for the spherical ReSTOR IOLs. In relation to low-contrast BCVA, we have obtained an expected reduction of the values with contrast reduction: about 20/32 and 20/40 of BCVA for 25% and 12.5% of contrast, respectively. Considering the optical quality improvement provided by the aspheric profile of the new IOL, differences in visual acuity between spherical and aspheric ReSTOR IOLs may be found for low-contrast BCVA. Future studies should focus on distance visual acuity measurement at different contrast and lighting conditions.
The results found at near vision, revealed that the AcrySof ReSTOR aspheric IOL provides a high near visual performance, with 100% of the eyes having a binocular BCVA of 20/25 or better (Table 2). Mean BCNVA was -0.025 logMAR. Kohnen et al.10 reported a 83.9% of patients with 20/25 or better binocular BCNVA at 33 cm (mean 0.05 logMAR). Alfonso et al.12 found a 99.1% of patients with 20/25 or better binocular BCNVA at the same near distance (mean 0.03 log-MAR). Despite of slight differences between the three models of the ReSTOR IOL, the new aspheric design shows the best outcomes. The addition of asphericity aims to improve image quality, thus, yielding a better near visual acuity.
In relation to intermediate visual acuity, we may observe, from figure 2, a statistically significant change of the binocular visual acuity as a function of the distance to the test. However, a better intermediate visual performance is found compared to that yielded by monofocal IOLs (Souza et al.11 reported a mean BCIVA of 0.23±0.12 logMAR at 60 cm with the AcrySof ReSTOR IOL). If we analyse figure 2, the through-focus measurements of binocular visual acuity show that, as expected, although acuity is good at distance and near, there is some loss in vision at intermediate distances. For the spherical ReSTOR Natural IOL (data from Blaylock et al.18, Alfonso et al.12 and Montés-Micó et al.19) we may observe two peaks in the graph at the expected near and far foci (corresponding to 0 and -3.2 D, respectively) with somewhat reduced acuity (0.3 logMAR, equivalent to 20/40) at intermediate distances. The results with the aspheric ReSTOR IOL show a V-pattern similar to that found by theses authors with the spherical IOL12,18,19. However, the visual acuity at intermediate distance is better: 0.2 logMAR (about 20/30). The asphericity of the IOL improves functional intermediate vision. Blaylock et al.18 and Alfonso et al.12 have previously reported that patients implanted with the AcrySof ReSTOR IOL may experience difficulties at intermediate distances and have suggested that, for patients for whom intermediate vision is important, this can be overcome by aiming for a partial monovision correction. One may argue that the improvement reported in this study for intermediate vision achieved with the aspheric design, would be enough to alleviate the difficulties reported by some patients at intermediate distances. Further analysis with a quality of vision questionnaire on this should be performed to prove this statement.
There have been several previous studies of photopic CS after multifocal IOL implantation (see Montés-Micó et al.9 for a review). Most of the literature published on this topic point out that photopic CS with a multifocal IOL is reduced compared with that for a monofocal IOL, being, however, within the normal range. The results found for the AcrySof ReSTOR aspheric IOL agree with this (Figure 3). Decreased CS in patients with multifocal IOLs, as compared with patients with monofocal IOLs (as observed by Rocha et al.21 and Souza et al.11,22) or phakic eyes (standard, figure 3), is explained by the multifocal's division of the available light energy in the image between two or more focal points. Light energy distribution for the AcrySof ReSTOR IOL depends on the pupil diameter and varies approximately from 40 to 90% at the far focus and from 9 to 40% at the near focus20. The loss in photopic CS observed for the aspheric ReSTOR IOL is somewhat smaller compared to standard values and comparable to that found for spherical ReSTOR IOLs (P>0.1). It may be that the effect of the aspheric profile combined with the ocular longitudinal chromatic and other types of ocular aberration, together with the blending zones of the IOL, tend to mask the differences in CS.
Under mesopic conditions distance CS would be expected to be little affected since, thanks to the relatively small diameter of the apodized diffractive zone and the contribution of the purely refractive outer zone (pupils >5mm), more than 80% of the light contributes directly to the distance image20. Correspondingly less than 20% of the light contributes to the near image, leading to noticeably worse mesopic CS at near20. Differences between the three IOLs at all spatial frequencies were not significant (P>0.1). Note the different lighting condition for mesopic examination across studies: 5cd/m2 for the spherical ReSTOR IOLs versus 3cd/m2 for the aspheric ReSTOR IOL. One should consider that the loss in retinal image contrast has little effect on acuity as measured with high-contrast letters, since contrast can be reduced to quite low levels before acuity is affected23.
In conclusion, the present study shows that the AcrySof ReSTOR aspheric apodized diffractive IOL yields good high-contrast visual acuity at both distance and near; as well as a good CS at photopic and mesopic conditions. Intermediate vision is improved in relation to that found with the spherical AcrySof ReSTOR.