The purpose of this study is to demonstrate and compare the use of optical coherence tomography (OCT) in measuring sagittal depth (SD) and in describing the corneo–scleral junctions with the use of scleral angles, in a population of keratoconics (KC) and of normals (normal).
MethodsFourteen participants (one eye randomly selected) in the normal group and fourteen eyes of nine participants in the keratoconus group were enrolled in the study. Orbscan II (B&L, Rochester) topography was performed to establish eligibility, steep and flat K readings (axes) and HVID. Measurements of the sagittal depth of the cornea and the scleral angles along a particular chord diameter (their HVID and 15mm) both flat and steep were taken with the use of the on screen measurement tools from the profile view of the cornea of the Visante™ OCT (Carl Zeiss, Dublin, CA).
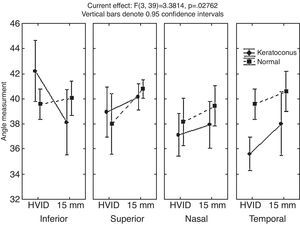
ResultsData were taken from 14 eyes (11 Females; 3 Males) in the normal group and 14 eyes (5 females; 9 males) in the KC group where either or both eyes were measured. The study participants had a mean age of 33±7yrs (normal) and 40±14yrs (KC). The groups were matched according to HVID: 11.77±0.41mm (normal) and 11.75±0.35mm (KC), (p=0.880). The steep K readings were 53.74±5.98D for the keratoconus eyes as compared to 43.77±1.35D for the control (p<0.0001). The sagittal depths (±SD) of the keratoconic cornea were significantly different than the normal corneae at their HVID and at 15mm in the steep meridian only (3.41±0.88mm versus 2.42±0.09mm, p=0.001 and 3.93±0.25mm versus 3.70±0.16mm, p=0.009, respectively). In addition, when the two groups were compared there was no difference in the scleral angles at the HVID's overall (p=0.490), but there were differences by location (inferior and temporal, p=0.003). At the 15mm chord, there was a significant difference between the groups (p=0.012) overall, but not by location (p=0.130).
ConclusionsMeasurement of the sagittal depth and the corneal-scleral junction angle in the steepest meridian at either the HVID or at 15mm are two metrics that significantly differentiate normals from keratoconics.
El objetivo de este estudio fue el de demostrar y comparar el uso de la tomografía de coherencia óptica (OCT) para medir la profundidad sagital, y describir las uniones córneo-esclerales con el uso de ángulos esclerales, en una población de pacientes normales y con queratocono.
MétodosSe incluyó en el estudio a catorce participantes (eligiendo un ojo al azar) en el grupo normal, y a catorce ojos de nueve participantes en el grupo de queratocono. Se realizó una topografía Orbscan II (B&L, Rochester) para establecer la elegibilidad, las lecturas (ejes) K flat (plana), K steep (inclinada), y el HVID (diámetro del iris visible horizontal). Se midieron la profundidad sagital de la córnea y los ángulos esclerales, así como un diámetro particular de la cuerda (HVID y 15mm), tanto plano como inclinado, utilizando las herramientas de medición en pantalla desde la visión de perfil de la córnea del Visante™ OCT (Carl Zeiss, Dublin, CA).
ResultadosSe obtuvieron datos de 14 ojos (11 mujeres; 3 varones) en el grupo normal, y de 14 ojos (5 mujeres; 9 varores) en el grupo de queratoconos, midiéndose un ojo o ambos. La edad media de los participantes en el estudio fue de 33±7 años (grupo normal) y 40±14 años (queratocono). Los grupos se emparejaron conforme al HVID: 11,77±0,41mm (normal) y 11,75±0,35mm (queratocono), (p=0,880). Las lecturas K del meridiano más curvo fueron 53,74±5,98D para los ojos con queratocono, en comparación a 43,77±1,35D para el grupo de control (p<0,0001). Las profundidades sagitales (±SD) de las córneas con queratocono fueron considerablemente diferentes a las de las córneas normales tanto en el HVID como a 15mm, únicamente en el meridiano más curvo (3,41±0,88mm frente a 2,42±0,09mm, p=0,001 y 3,93±0,25mm frente a 3,70±0,16mm, p=0,009, respectivamente). También, al comparar los dos grupos, no existió diferencia en los ángulos esclerales con un HVID global (p=0,490), aunque existieron diferencias según la localización (inferior y temporal, p=0,003). Con una cuerda de 15mm, se produjo una diferencia significativa entre los grupos (p=0,012) globalmente, aunque no según la localización (p=0,130).
ConclusionesLa medición de la profundidad sagital y del ángulo de unión corno/escleral en el meridiano más curvo, tanto para el HVID como para 15mm, son dos valores que diferencian considerablemente a las córneas normales y a aquellas con queratocono.
Keratoconus (KC) is a non-inflammatory thinning of the cornea that causes structural changes in the cornea resulting in scarring and appearance of Vogt's striae i.e. stress lines due to stretching of the corneal tissue, as well as shape alterations in the cornea inducing irregular astigmatism.1 These morphological changes cause significant visual distortions, streaking, sensitivity to light and loss of night vision.2 KC affects approximately 0.1% of the general population, with vision deterioration reducing significantly the patient's visual function.3 Mild KC cases are treated by wear of custom designed rigid, gas-permeable, corneal or scleral lenses, which correct for the irregular astigmatism of the cornea4 and maintain excellent corneal health. A number of procedures are currently available for treating various stages of KC: intra-stromal ring segment placement (INTACs), corneal collagen cross-linking, or transplantation of donor corneas. While these procedures may result in some corneal flattening, they lack the precision to induce sufficient change to eliminate the need for an over-correction with contact lenses.5 More recently scleral lenses are finding their way back into practices and many publications on their use in the management of irregular corneae.6–9
The use of instrumentation that can measure corneal and corneo-scleral sagittal depth and peripheral angles (which can be used to define the shape of the corneal-scleral junction10) can aid the practitioner in selecting the correct lens base curve. With semi-scleral lenses the base curve is no longer as closely related to the corneal curvature due to the large optic zone diameters of these lenses and the fact that they do not come in contact with the cornea but, in fact settle on the conjunctival tissue instead. In recent studies, optical coherence tomography (OCT) has been presented predominantly as a microscopic imaging technique for in vivo examination of the posterior and the anterior segment.11–13 Several imaging methods are capable of providing shape information of the anterior eye14 such as, Orbscan II (B&L Surgical) and Scheimpflug camera systems (Pentacam by Oculus, Lynnwood, WA). However, optical coherence tomography (for example, the Visante™ OCT (Carl Zeiss, Dublin, CA)) can visualise the anterior segment up to and beyond the limbus.10,15 The Visante™ is a non-contact device utilising optical coherence tomography to image the anterior segment with a wavelength of 1310nm and scan rate of 4000 axial scans per second.16,17
The aim of this pilot study was to look at the anterior segment maps of fourteen normal eyes, HVID matched to keratoconic (KC) eyes and measure parameters that may be useful to design large diameter gas permeable contact lenses that may sit outside the region normally viewed by the corneal topographers. Secondly, the aim was to compare the distribution of these parameters in the normal eye to the KC eye and see how well they correlated with each other.
MethodsThis was a cross-sectional study that involved fourteen participants/eyes in each group. Corneal topography confirmed the medical chart diagnosis for each group (that is, either “average or normal” or KC) by looking for any abnormal indices of SAI or SRI and any characteristic inferior-temporal steepening and lazy eight patterns. The participants were asked to discontinue contact lens wear on the day prior to the visit. Data and observations were collected at one scheduled appointment (screening combined with study visit) and the study was conducted according to the Tenets of Helsinki.
Imaging of the corneal topography and anterior segment of the eye were performed using the Orbscan™ II (B&L Surgical, Rochester, NY) and the Visante™ OCT (Carl Zeiss, Dublin, CA) respectively. Three scans per eye were taken for each participant using both devices and the best images were chosen. The Orbscan II™ was used to measure the steep and flat K readings and the HVID of each participant (labelled as “white to white”). The best image was chosen for analysis with the least amount of missing data shown as black areas in the curvature map. We ensured that the scans were orthogonal to the optical axis of the eye with the Visante™ OCT. The images were taken individually along both the steepest and flattest meridians. This occurred when a bright specular reflection of the scanning beam from the tear film surface was reflected directly back into the coaxial detector. For each participant, scans were completed at approximately the same time on each day using the same equipment that was calibrated daily, with the same instructions and procedure by the same investigator.
The Visante™ OCT uses a wavelength of 1310nm reducing the amount of signal scattering and allowing for better penetration past the limbus and sclera up to 16mm. With a scan rate of 4000 axial scans per second, the very fast image capture reduces the impact of image distortion caused by ocular movement. Since the images are affected by changes in the index of refraction across the corneo–scleral surface, dewarping software automatically makes the appropriate adjustments prior to their display. With the built-in callipers, it is possible to obtain sagittal depth (SD) and chord measurements at any point of the anterior segment. Sagittal depths were measured both at a 15mm chord and at the participant's HVID, as were the scleral angles as an indicator of peripheral scleral shape. Data were analysed using Statistica 7 and Medcalc 9.3.
ResultsThere were 14 eyes of 11 female and 3 male study participants and the test eyes were randomly selected for the normal group and 14 eyes of 9 males in the KC group where either or both eyes were measured. The study participants had a mean age of 33±7yrs (normal) and 40±14yrs (KC). The HVID (“white to white” chord diameter) measurements for both groups were not different and were 11.77±0.41mm (normal) and 11.75±0.35mm (KC) (p=0.88). The groups were matched based on HVID rather than gender or age since in an adult normal population our test parameters of corneal shape does not vary with age and gender, but does vary with chord diameter. The steep K readings were 53.74±5.98D for the keratoconus eyes as compared to 43.77±1.35D for the normal corneae which were significantly different (p<0.0001).
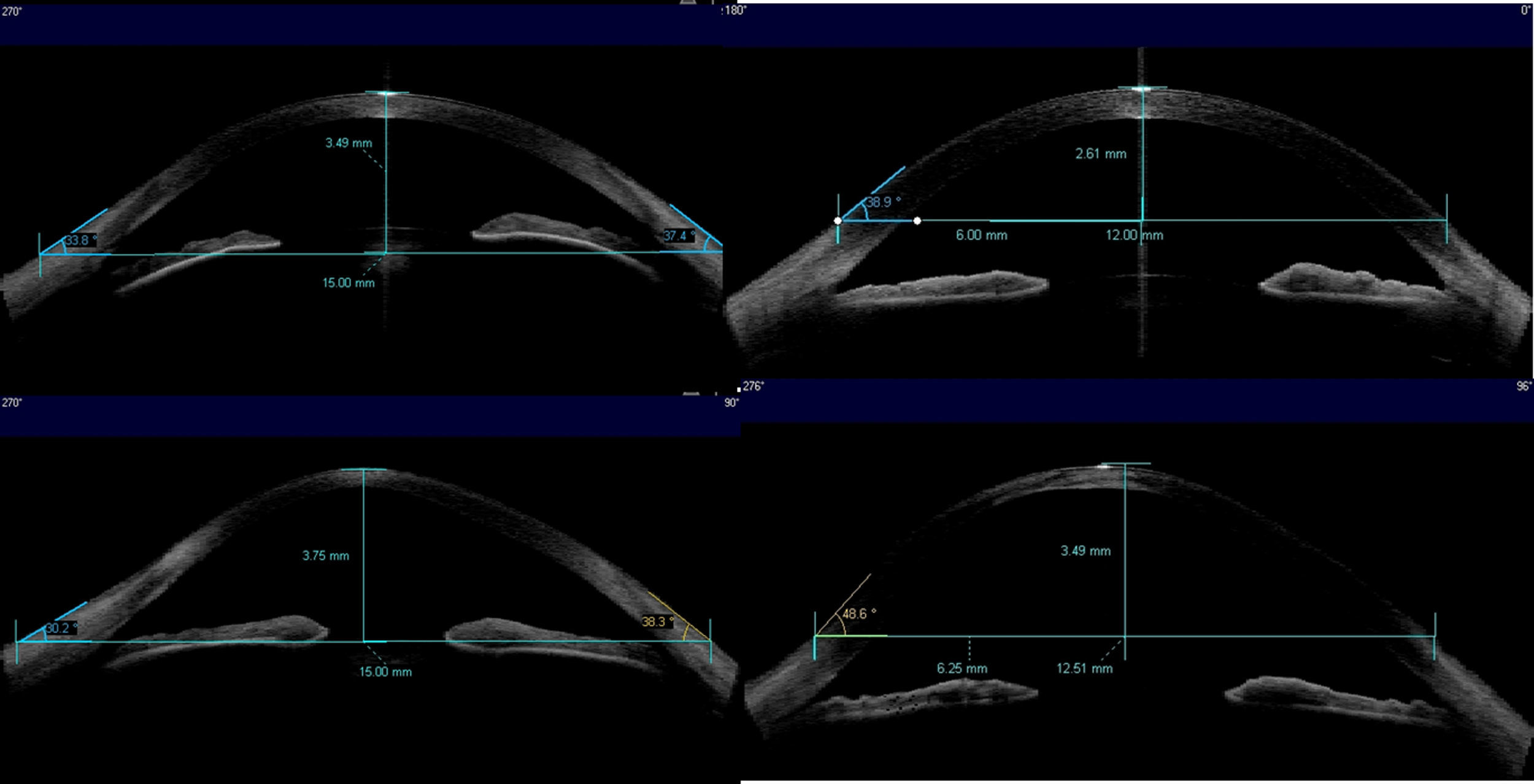
Corneal sagittal depth and peripheral scleral angles were measured at 15mm chord length and their HVID as shown in Fig. 1, a composite of normal or normal and KC.
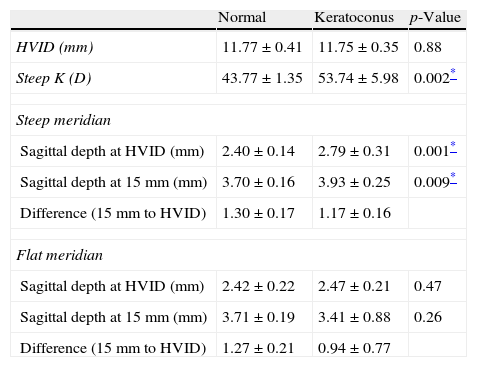
Table 1 summarises the data from the Orbscan II™ and the Visante™ OCT for the sagittal depth measurements. When the steep and flat meridians for the normal eyes were compared, there was no significant difference at both the two chord diameters (p>0.05, both). On the other hand comparisons for the KC eyes indicated significant differences for both chord diameters in sagittal depth (p=0.025 and p=0.040), the steep meridian showing the largest change for both meridians.
Baseline comparison of the two groups (normal and KC) and comparison of sagittal depths for the steep and flat meridians at both the HVID and 15mm chords.
| Normal | Keratoconus | p-Value | |
| HVID (mm) | 11.77±0.41 | 11.75±0.35 | 0.88 |
| Steep K (D) | 43.77±1.35 | 53.74±5.98 | 0.002* |
| Steep meridian | |||
| Sagittal depth at HVID (mm) | 2.40±0.14 | 2.79±0.31 | 0.001* |
| Sagittal depth at 15mm (mm) | 3.70±0.16 | 3.93±0.25 | 0.009* |
| Difference (15mm to HVID) | 1.30±0.17 | 1.17±0.16 | |
| Flat meridian | |||
| Sagittal depth at HVID (mm) | 2.42±0.22 | 2.47±0.21 | 0.47 |
| Sagittal depth at 15mm (mm) | 3.71±0.19 | 3.41±0.88 | 0.26 |
| Difference (15mm to HVID) | 1.27±0.21 | 0.94±0.77 | |
Comparisons were made between the normal eyes and KC with respect to sagittal depths at HVID chord. There was a significant difference at only the steep meridian (p=0.001), but not along the flat meridian (p=0.047). Along the 15mm chord, the results were similar, where only along the steep meridian was a difference found (p=0.009) and there was no difference found along the flat meridian (p=0.260).
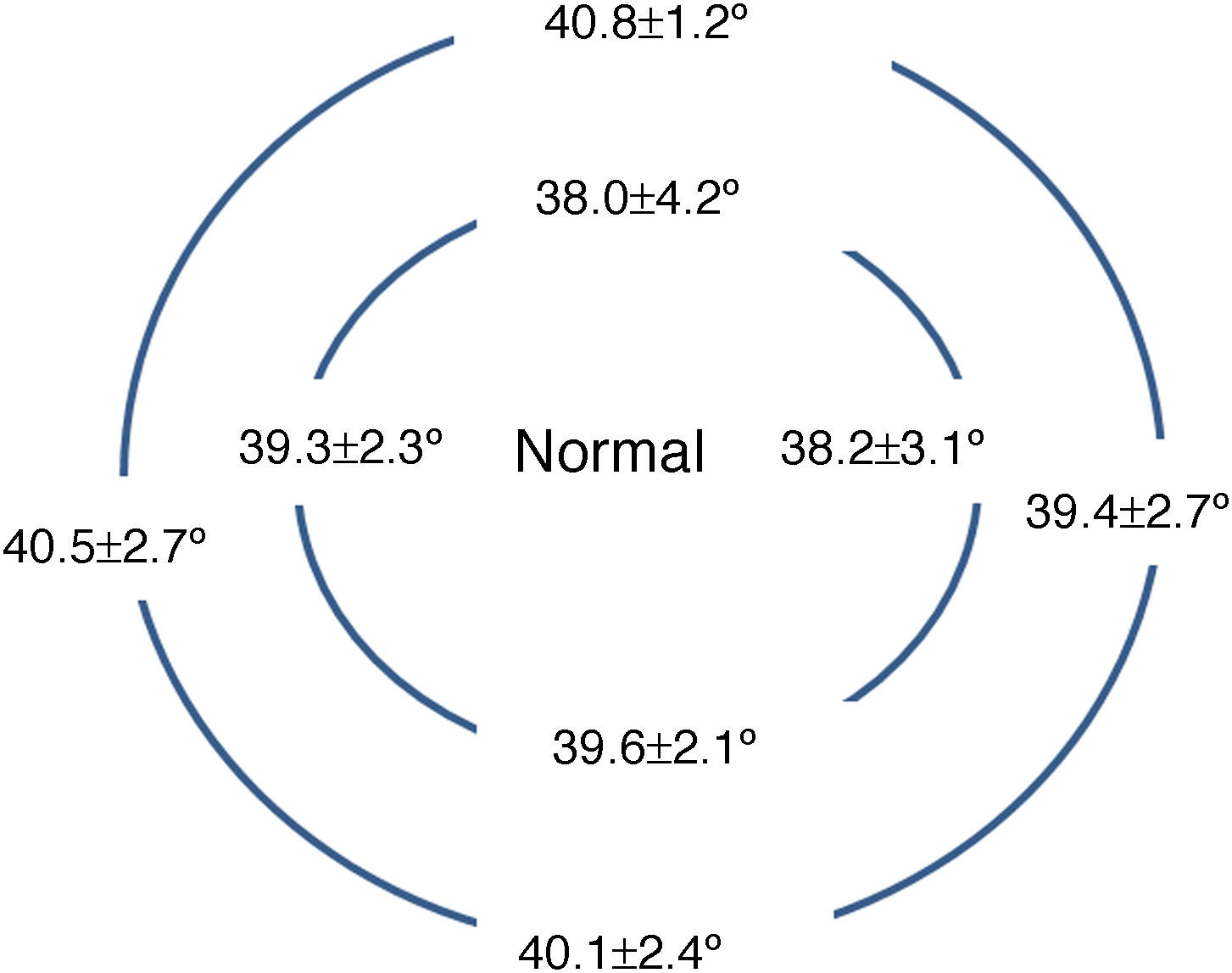
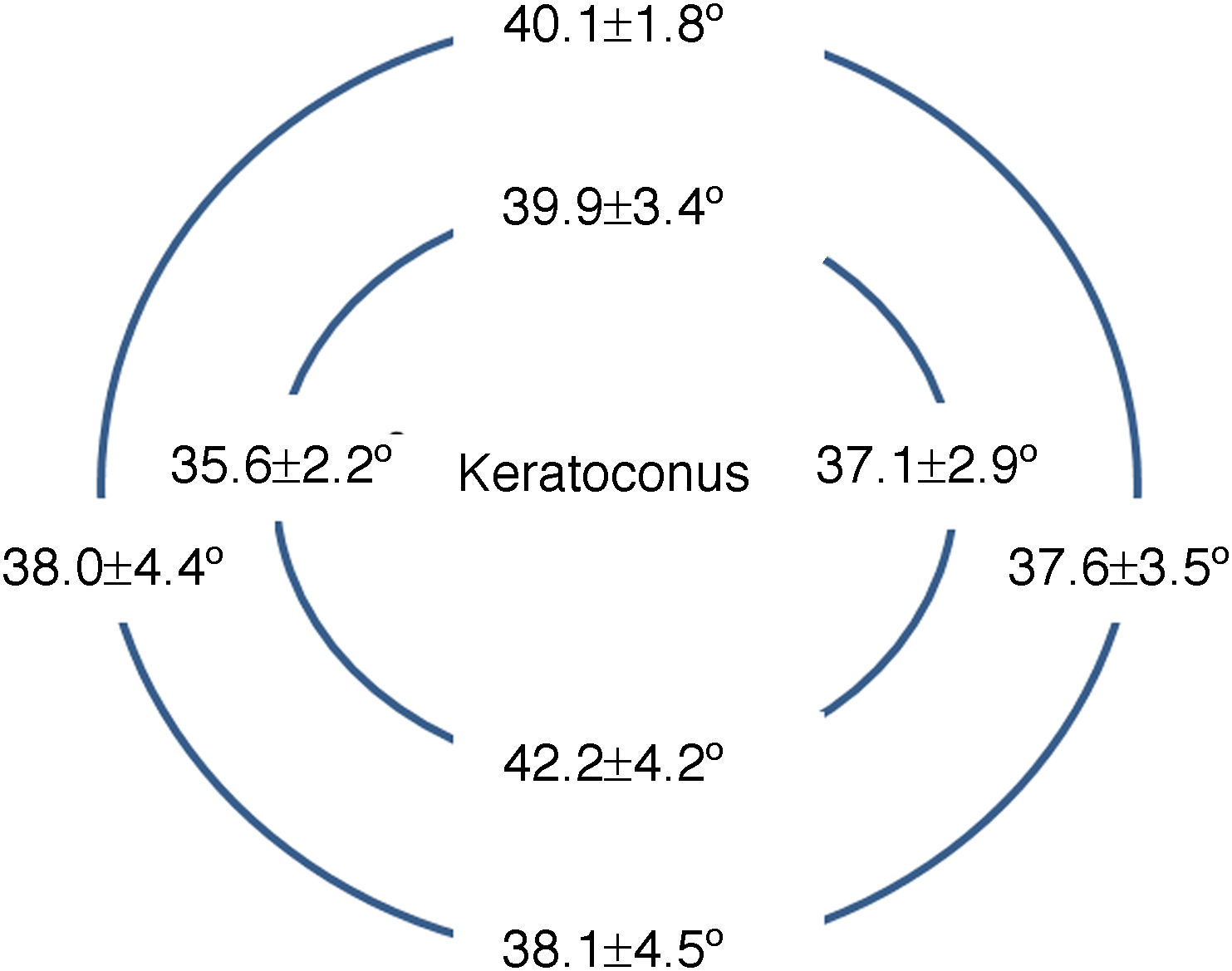
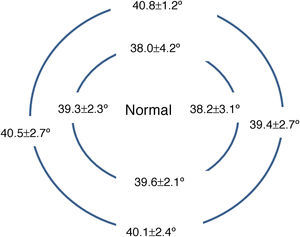
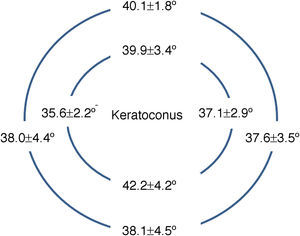
For the normal population, there were no significant differences at either the HVID or the 15mm chord comparing the peripheral scleral angles at the inferior, superior, nasal and temporal locations (p=0.320 and p=0.280, resp.). The peripheral scleral angles are illustrated in Fig. 2. However, for the KC group (Fig. 3), at the HVID chord there was a significant difference by location (p<0.0001), the temporal location being different from the rest. However, at the 15mm chord diameter, the KC group was not significantly different when the angles at the four locations were compared (p=0.240).
When the two chord diameters were compared, only the normal eye group showed a difference overall by diameter (p=0.024) in scleral angles, whereas, the KC group did not (p=0.910). The KC group did show a difference by location and chord diameter (p=0.004) again pointing to the inferior location.
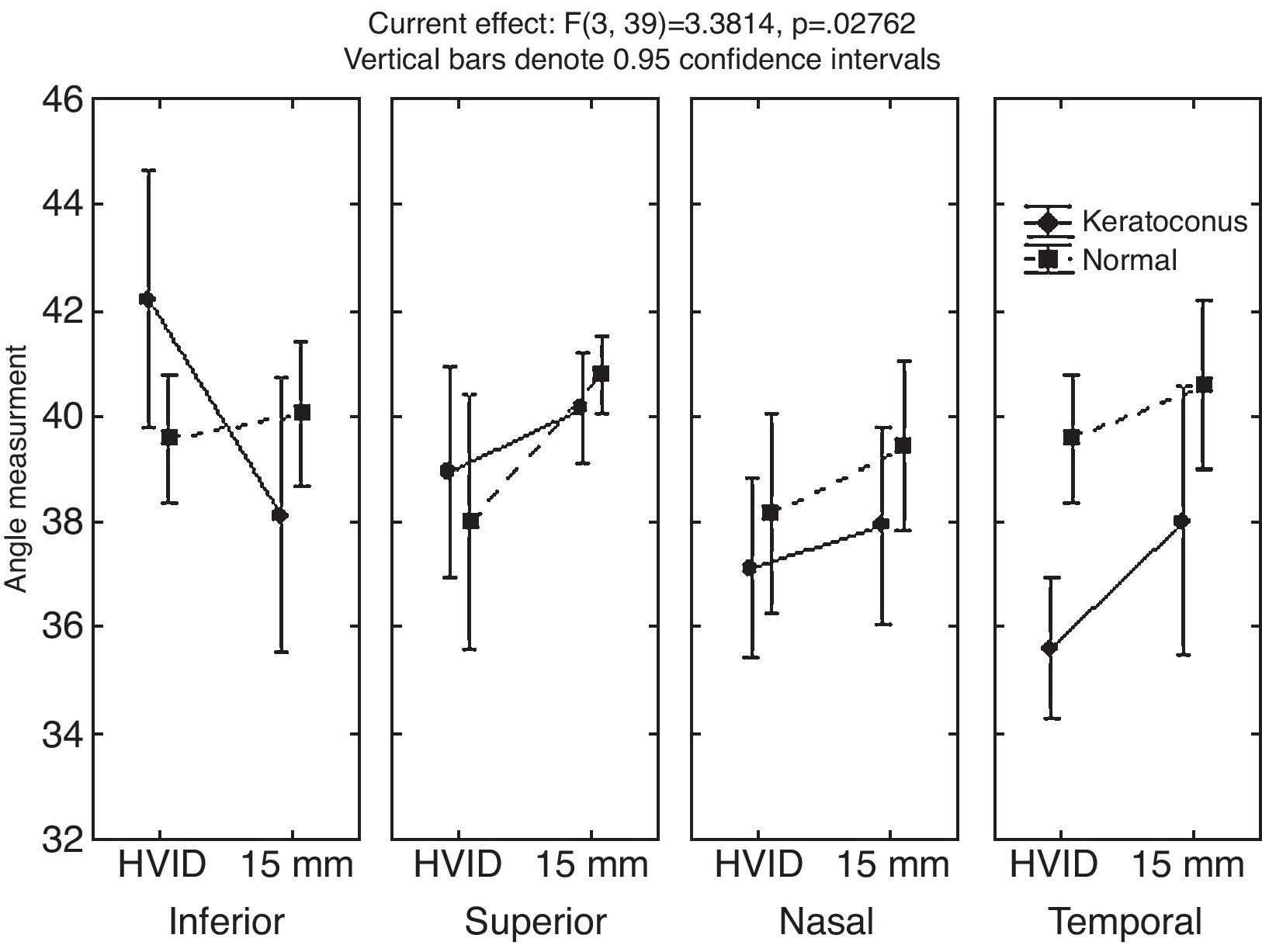
Finally, comparisons were made between the normal eye and the KC groups with respect to peripheral corneal angles (see Fig. 4). At the HVID chord diameters, there was no overall difference between the groups (p=0.490), but there was a location difference where the inferior and temporal angles were different (p=0.001). At the 15mm chord, there was a significant difference between the two groups (p=0.012) overall, but not specifically by location.
Correlation coefficients of concordance (CCC) were performed to see how well the HVID and 15mm chord diameter, the steep K readings and the peripheral angles corresponded to the sagittal depths.
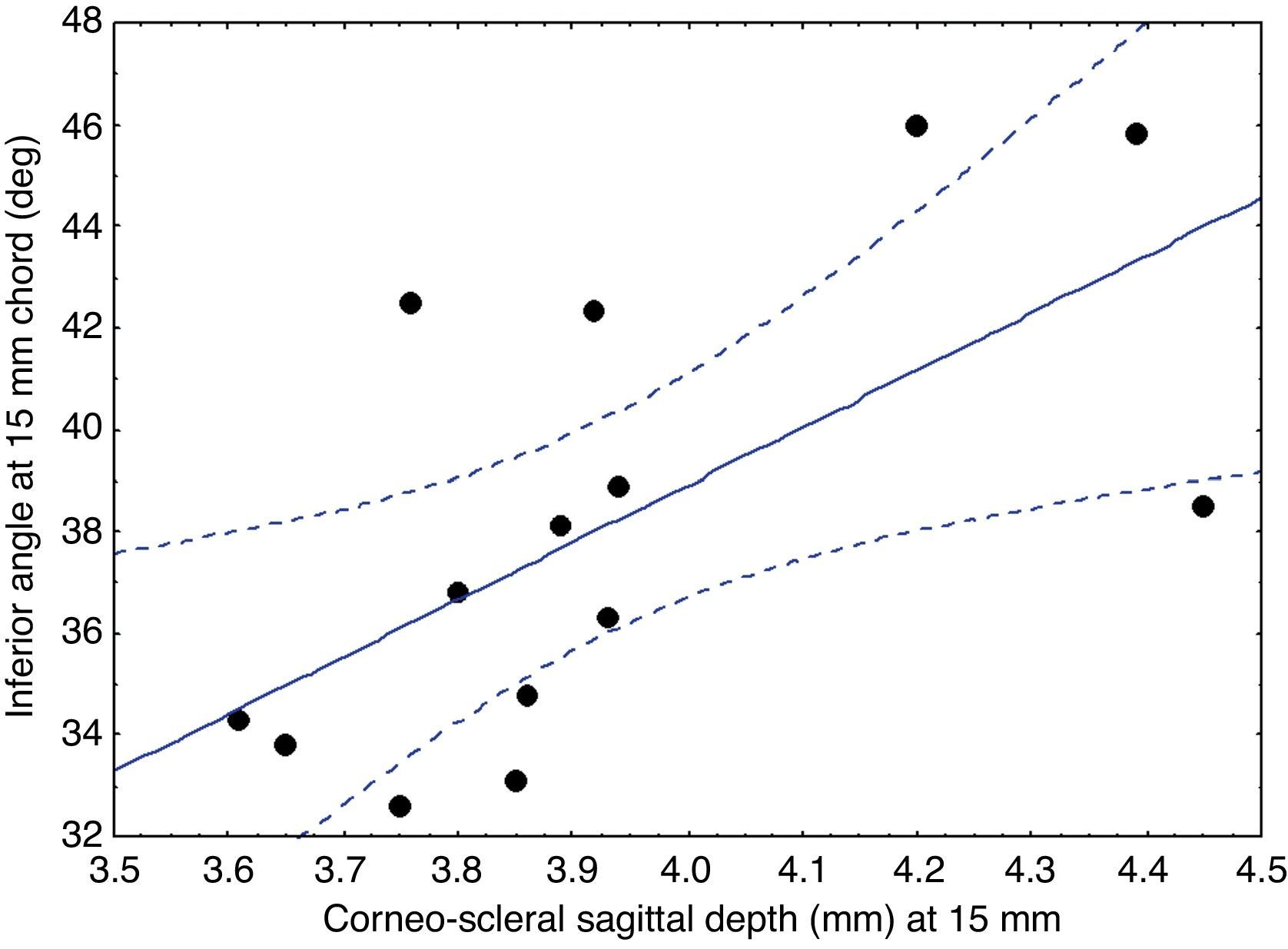
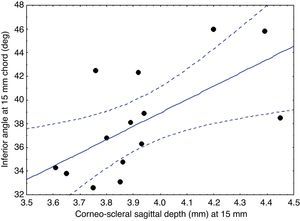
There was a strong correlation between HVID and the sagittal depth, as the HVID increases so does the corneal sag for the KC group (r=0.82, p=0.040) and for the normal group (r=0.75, p=0.046), which would be expected. There was a strong correlation between the sagittal depth and the inferior angle for the KC group (r=0.62 (HVID) and r=0.63 (15mm), p=0.047 and p=0.020, resp.) and a weak one for the normal group at HVID and 15mm (r=0.12 and 0.21, p=0.700 and p=0.890) respectively. This indicates that the inferior angle was a better indicator of peripheral scleral shape for KC (see Fig. 5).
DiscussionVisante™ OCT anterior segment imaging is a simple method in providing biometry of the peripheral cornea/sclera with its measurement technique and tools. The results indicate that especially for KC patients it is important to measure the sagittal depth (SD) at either chord diameter at the axis of the steep meridian, since the cone is usually displaced slightly away from the vertical meridian. The SD will be represented more appropriately especially when compared to normal eyes. On the other hand, the SD in the flat meridian of oval or inferiorly displaced cones showed little difference as compared to normal eyes at either chord diameter.
The peripheral scleral angles measured at the HVID varied between the two groups at the inferior and temporal locations only. However, at 15mm they did not vary by location, but overall were significantly different between the two groups. Multiple measurements of inferior and temporal angles at many chord diameters may be required in order to find a better correlation with SD considering that for normal eyes the same central K reading results in varying sagittal depths dependent on the peripheral corneal shape and HVID. The steep K readings alone are not as predictive of sagittal depth. The CCC results indicate that only the inferior scleral angles are moderately correlated with the SD measured at either chord diameter. A larger sample size would improve this correlation as there is only a tendency for an increase is SD as the inferior scleral angle increases. This indicates the importance of measuring sagittal depth directly, combining this information with the inferior and to a lesser extent temporal angles when fitting very large diameter contact lenses as it has been shown in a study by Gemoules.18 Manufacturing software was derived from the data of this study to predict the scleral lens design. Thus far, OCT-derived sagittal depth and scleral angles have not been commonly used for the fitting of scleral lenses but, only for soft lens fitting has SD been employed.19 The combination of the measurement of sagittal depth and inferior angles may prove to be vital parameters that the Visante™ OCT can supply to improve the efficiency of scleral lens fitting, once the relationship between the OCT corneal SD and the scleral lens SD has been established.
We have shown in a previous study,10 where nasal and temporal angles at a single chord were measured tangentially to the sclera in order to describe the flatter scleral shape, results that supported the notion that the sclera may have a more tangential shape as opposed to an actual curvature change at the specified location. This is demonstrated by the perfect alignment of the angle measuring tool of the Visante™ OCT in this location.
Visante™ OCT anterior segment imaging is a simple method for providing biometry of the peripheral cornea and sclera. Large diameter lenses may become the preferred method of fitting difficult corneal topographies in the hope of producing more comfortable, better fitting lenses by resting on the sclera instead of the cornea, thus reducing lens re-orders and having a higher percentage of initial lens success.20–24 The anterior segment Visante™ OCT can help visualise the corneal/scleral anatomy.
Conflicts of interestThe authors declare that they do not have any conflicts of interest.
SponsorCentre for Contact Lens Research.