Informed consent means the process whereby patients are informed of all the necessary information about health care and subsequent treatment plans. In socioeconomically developing semi-urban setting, where most of the patients are illiterate, we wanted to assess knowledge, attitude and anxiety of patients towards informed consent.
MethodsPatients were recruited from the waiting list for ophthalmic surgery at the department of Ophthalmology, Dhulikhel Hospital. A detail optometric and ophthalmologic evaluation was carried out. Data were collected through a 12-item questionnaire and an 8-item Likert scale. Statistics included regression analysis, chi-square test as well as frequency and percentages.
ResultsOf 42 questionnaire responders, female participation was high (64.3%). Sixty two percent of patients wanted the physician to decide for or against the surgery. Most of (69%) patients thought that by signing the consent they were agreeing for surgery and few (16.7%) thought that the consent was a legal document. Twenty two patients (52.4%) gave importance to the surgical intervention even though there were chances of serious complications. The preoperative anxiety was affected by surgical outcome (81%), complication (40.5%) and anaesthesia (9.5%). The patients prioritized the preoperative information on nature of illness, need for operation and the chances of vision improvement after surgery.
ConclusionMost of patients wanted the doctor to decide their treatment. Many patients wanted to know about the disease, treatment and the success rate of surgery. The success of the operation, the anaesthesia and the long list of complications tended to provoke anxiety.
El consentimiento informado es el proceso mediante el cual se aporta a los pacientes toda la información necesaria en relación a la atención sanitaria y los consiguientes planes de tratamiento. En un entorno semi-urbano, en vías de desarrollo socio-económico, quisimos evaluar el conocimiento, la actitud y la ansiedad de los pacientes con respecto al consentimiento informado.
MétodosSe seleccionaron pacientes en lista de espera para cirugía oftálmica del departamento de Oftalmología del Hospital Dhulikhel. Se llevó a cabo una evaluación optométrica y oftalmológica detalladas. Los datos de un cuestionario de 12 preguntas, y de una escala Likert de 8 cuestiones fueron recolectados. Las estadísticas incluyeron análisis de regresión, prueba de χ2, así como estudio de frecuencias y porcentajes.
ResultadosDe entre los 42 pacientes que respondieron al cuestionario, la participación femenina fue alta (64.3%). El sesenta y dos por ciento de los pacientes quisieron que fuera el médico quien decidiera a favor o en contra de la cirugía. La mayoría de los pacientes (69%) pensaron que la firma del consentimiento constituía la aceptación de la cirugía, y pocos pensaron (16.7%) que se trataba de un documento legal. Veintidós pacientes (52.4%) otorgaron importancia a la intervención quirúrgica, incluso cuando podían producirse graves complicaciones. La ansiedad pre-operatoria estuvo afectada por el resultado quirúrgico (81%), las complicaciones (40.5%) y la anestesia (9.5%). Respecto a la información preoperatoria, los pacientes dieron prioridad a la naturaleza de la enfermedad, la necesidad de la operación y las posibilidades de mejora de la visión tras a la cirugía.
ConclusiónLa mayoría de los pacientes quisieron que el médico tomara la decisión sobre su tratamiento. Muchos pacientes solicitaron información relativa a la enfermedad, el tratamiento y el porcentaje de éxito de la operación. Dicho éxito, la anestesia, y la larga lista de complicaciones tendieron a provocar ansiedad.
The relevant and comprehensive information about invasive surgical procedures is important for every patient. Recently it has become an important part of medical practice and often a legal necessity for surgical procedures.1,2 The concept of patient consent evolved from a judgement in the US supreme court during 1914 and it became a part of international law following World War II with the basic concept that patient consent is mandatory prior to performing any invasive procedure.3,4 The term ‘informed consent’ means the process whereby patients are provided with all the necessary information about health care and subsequent treatment plans. It has many benefits including patient cooperation, thus minimizing surgical complications and increasing the chances of successful defence against possible medico-legal cases.5 The legal aspects of consent are based around the rights of the patients to make their own decision and the ethical aspects of the concept of the shared process of decision making.6 Thus, shared decision making allows both patient autonomy and physician responsibility. In the socioeconomically developing countries like Nepal, it is less likely that patients will be involved in the decision making process about the management plans of their health conditions. In fact they prefer that the involved physician should decide the treatment.
Patients undergoing eye surgeries are concerned of their visual improvement, time taken to improve the vision and the overall risks of visual loss.7 In recent years, eye surgeries have evolved with shorter surgical procedures and better outcomes. So, the patient's expectations are also high. Managing unrealistic patient expectations are paramount in reducing the medico-legal risk associated with these procedures.8 The appropriate pre-operative counselling will not only help to strengthen the patient–doctor relationship but also protect the doctor against medico-legal risks. So, we designed this study to determine what patients want to know when their surgery is advised and to assess their knowledge, attitude and curiosity towards the informed consent.
MethodsPatientsPatients were recruited from the waiting list for ophthalmic surgery at the Department of Ophthalmology, Dhulikhel Hospital. Data were collected over a period of 6 months from February 2012. Ethical approval for the study was obtained from the Dhulikhel Hospital Clinical Research Ethics Committee. All patients were approached prior to surgery and given a briefing about the intended study and its purpose, i.e.; ‘to help institute improve the quality of its health services’. They were also given the assurance about the confidentiality of the information gathered. Education (highest degree earned), occupation and regional provenance (rural, town or city) were recorded. All patients waiting for eye surgery under local anaesthesia including those for lids, conjunctiva, reconstruction and cataract surgery were included in the study. The exclusion criteria were set as follows: patients with age 15 years or younger, patients with abnormal psyche, that is, anxiety disorders, depression and chronic confusional states, patients who were not competent to take the particular decision, those who have not received sufficient information to make a decision, those acting under duress and those who could not understand and respond in the local language.
Examination procedureA complete ophthalmic examination was carried out which included preoperative habitual visual acuity measurement with self illuminated Snellen chart, refraction, slit lamp examination, funduscopy as well as keratometry and biometry. Ophthalmologist provided comprehensive information about the diagnosis, planned eye surgery, operative procedure, complications, operative risks and benefits involved, postoperative care and the outcome as well as risks and benefits of doing nothing. Alternative treatments, if any, were also mentioned. All medical expressions were explained using layperson's terms. After the surgery, patients were followed up on the first, fourth and sixth week for the study purpose. Postoperative visual acuities were recorded on the first day and the sixth week of the surgery. Intra-operative and postoperative complications, if any, were noted.
Consent procedureOn the day of surgery, surgical consent form was signed by both the patient and surgeon. A trained paramedical staff interviewed all participants with a set of structured questions specially designed for this study. The tenets of the Declaration of Helsinki were followed and the verbal consent was taken from all patients.
Questionnaires (Appendix 1)The first part of the questionnaire included 12 items which were developed based on the publications by Elder7 and Dawes.9 It was translated into Nepali language and pretesting was done in twenty patients attending the ophthalmology department. The questions were revised and modified to ensure the ease of comprehension and completeness. The questions in the interview covered three aspects of the consent: preoperative information provided, patient's decision and the attitude towards consent.
Assessment of attitude, knowledge and anxiety using Likert scaleThe second part of the questionnaire included eight questions to respond to the extent they agree. Respondents were offered a choice of five pre-coded responses which ranged from strongly agree to strongly disagree with the neutral point being neither agree nor disagree.
Statistical analysisStatistical analysis was done by performing multiple logistic regression models to delineate the strength of association among occupation, education, gender (independent variables), and patients’ satisfaction (dependent variable) with the surgical outcome (yes or no). Chi-square test statistics was done for gender and Likert scale questionnaires. Frequency and percentages were also calculated. Software ‘Statistical package for Social Sciences, version 11.5; SPSS Inc., Chicago, Illinois’ was used to analyze the data. A p-value less than 0.05 was considered to be statistically significant.
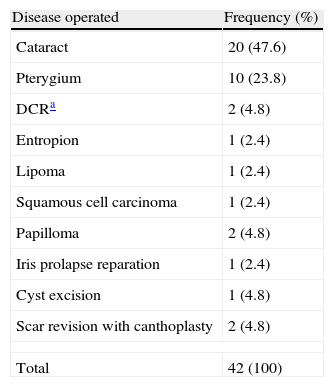
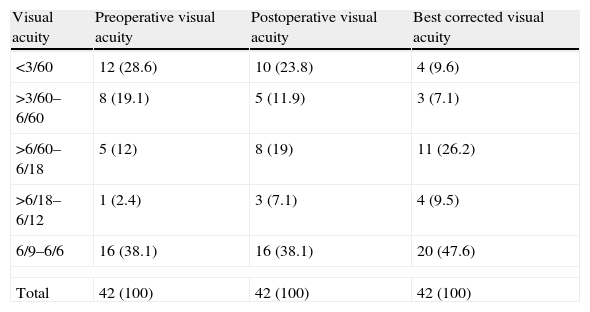
ResultsAll forty two patients who were invited to participate responded to the questionnaire (response rate: 100%). Mean age of patients was 53.48±6.41 years and 64.3% were female. Eleven patients (26.2%) had undergone prior surgery for either eye diseases or other systemic conditions. More than half the patients (57.1%) had no formal education. Only 19% had either higher secondary education or professional degree. Disease treated and visual acuity pre and post operatively are presented in Tables 1 and 2. Final visual acuity was improved in all the patients.
Disease pattern.
| Disease operated | Frequency (%) |
| Cataract | 20 (47.6) |
| Pterygium | 10 (23.8) |
| DCRa | 2 (4.8) |
| Entropion | 1 (2.4) |
| Lipoma | 1 (2.4) |
| Squamous cell carcinoma | 1 (2.4) |
| Papilloma | 2 (4.8) |
| Iris prolapse reparation | 1 (2.4) |
| Cyst excision | 1 (4.8) |
| Scar revision with canthoplasty | 2 (4.8) |
| Total | 42 (100) |
Visual acuity.
| Visual acuity | Preoperative visual acuity | Postoperative visual acuity | Best corrected visual acuity |
| <3/60 | 12 (28.6) | 10 (23.8) | 4 (9.6) |
| >3/60–6/60 | 8 (19.1) | 5 (11.9) | 3 (7.1) |
| >6/60–6/18 | 5 (12) | 8 (19) | 11 (26.2) |
| >6/18–6/12 | 1 (2.4) | 3 (7.1) | 4 (9.5) |
| 6/9–6/6 | 16 (38.1) | 16 (38.1) | 20 (47.6) |
| Total | 42 (100) | 42 (100) | 42 (100) |
Twenty six (61.9%) patients wanted their physician to decide for or against the surgery, eleven (26.2%) preferred the physician dominated decision but wanted to know the treatment process and five (11.9%) wanted to come to a decision by themselves. From 42 patients, 12 (28.6%) reported that the doctor decided for the surgery and 22 (52.4%) said that the decision was made consensually.
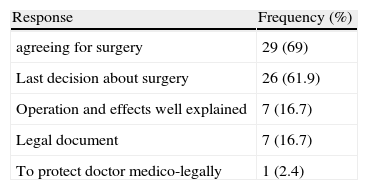
Attitude towards consent form (Questions 2, 3, 4, 5 and 6)More than half of the patients (54.8%) knew that they had to sign the consent form and for most of them it meant an agreement for surgery (Table 3). Twenty six patients (61.9%) were not sure if they could withdraw the surgery after signing the consent form where only four (9.5%) marked that they could defer the surgery. Patients reported that consent helped them in different ways, like giving enough information regarding surgery (35.7%) and helping them to make up mind (26.2%). Few patients marked that to sign the consent form was not important either because they would completely depend on doctor's decision (19%) or they had already decided for the surgery (28.6%).
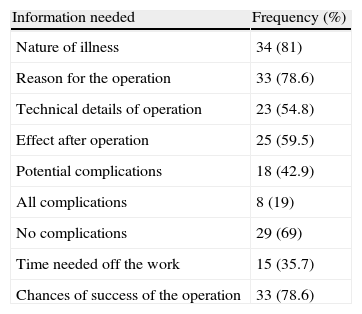
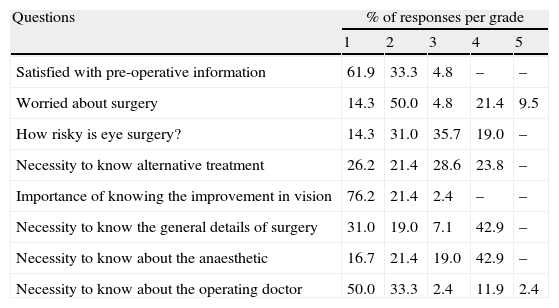
Assessment of knowledge, attitude, anxiety and desired pre-operative information (Questions 7, 8, 11 and Likert scale)Twenty two patients (52.4%) gave importance to the surgical intervention even though there were chances of serious complications whereas thirteen (31%) would defer the surgery in this case. Only seven (16.7%) marked that they would take a balanced decision between need and risk of the operation. The preoperative anxiety was affected by the thought of success of surgery (81%), risk of surgical complication (40.5%) and the anaesthesia (9.5%). Patients prioritized the preoperative information on nature of illness, need for operation, chances of success and the effect of operation (Table 4). The most important information desired was the chance of visual improvement after surgery followed by preoperative information and knowledge about the surgical doctor. The technical details of the surgery and the anaesthesia were reported as the least important (Table 5). Fifty percent patients graded 2 the answer to the question regarding the fear of the surgery whereas 9.5% awarded grade 5 out of 5 pre-coded responses ranging from 1 to 5. Males gave more importance on knowing the surgical doctor (p=0.016). Females reported high scale grades on fear of the operation (p=0.049).
Preoperative information desired (Question 11).
| Information needed | Frequency (%) |
| Nature of illness | 34 (81) |
| Reason for the operation | 33 (78.6) |
| Technical details of operation | 23 (54.8) |
| Effect after operation | 25 (59.5) |
| Potential complications | 18 (42.9) |
| All complications | 8 (19) |
| No complications | 29 (69) |
| Time needed off the work | 15 (35.7) |
| Chances of success of the operation | 33 (78.6) |
Responses to questions on Likert scale.
| Questions | % of responses per grade | ||||
| 1 | 2 | 3 | 4 | 5 | |
| Satisfied with pre-operative information | 61.9 | 33.3 | 4.8 | – | – |
| Worried about surgery | 14.3 | 50.0 | 4.8 | 21.4 | 9.5 |
| How risky is eye surgery? | 14.3 | 31.0 | 35.7 | 19.0 | – |
| Necessity to know alternative treatment | 26.2 | 21.4 | 28.6 | 23.8 | – |
| Importance of knowing the improvement in vision | 76.2 | 21.4 | 2.4 | – | – |
| Necessity to know the general details of surgery | 31.0 | 19.0 | 7.1 | 42.9 | – |
| Necessity to know about the anaesthetic | 16.7 | 21.4 | 19.0 | 42.9 | – |
| Necessity to know about the operating doctor | 50.0 | 33.3 | 2.4 | 11.9 | 2.4 |
Eye surgery was thought to be relatively a risky procedure by 28 (66.7%) patients and it was thought to be an easy and harmless procedure by 14 patients (33.3%).
Satisfaction with the surgical outcome (Question 12)Majority of patients (35, 83.3%) were satisfied with the surgical outcome. Among patient variables, occupation (housewives) (odds ratio, OR, 22.251; 95%CI, 0.013–5.267; p=0.000) and the better visual outcome (best corrected visual acuity better than 6/60) (OR, 1.887; 95%CI, 0.008–2.829; p=0.000) were strongly associated with satisfaction.
DiscussionIt is a general legal and ethical principle that a valid informed consent is obtained before starting treatment.10 In the western countries, treating a patient without valid consent may invite to a civil or criminal offence.11 Before signing consent form, patient should be well informed of the benefits, risks and complications of the intended procedure as well as alternative treatment options.12 Many factors such as access to information, emphasis on patients autonomy and medico-legal considerations have become part of the process of informed consent.
In the present study, the most important information desired by patients pre-operatively was the nature of illness, reason for operation and the chances of success of the operation. These findings are similar to a study by Pimentel et al. carried out in patients with cancer who reported that most of patients wanted to know as much as possible about their illness and treatment.13 Explaining all the desired information to the patients before surgery helps to establish a trustful relationship.12 In our study we observed that patients preferred to abstain from taking part in the management decision regarding their care. This observation is similar to that of Kiss et al.14 Higher number of illiterate patients in our study could have led to this observation because these patients are more likely to let their physician make decision regarding surgery. We observed that more males wanted to know about the surgical doctor. This could be because of the male dominated society where the family head (senior male) makes the decision regarding all the family members. This leads the doctor to act in a paternalistic way in our society where doctor decides everything for the better management of patient.5 In contrast, in developed countries, it is now accepted that a competent individual may go as far as to refuse any treatment even if as a result the may die.15
Most of our patients (69%) did not want to know about any complications prior to the surgery which is in contrast to a study where patients wanted to know about the important complications of their Ear, Nose and Throat (ENT) surgery.9 Kang observed that 35.6% of their patients did not want to know about the complications and risk of surgery, which is similar to our observations. It is understandable that different patients with different anxiety levels and interest would express different degrees of acceptance or tolerance to how much information they would want to know prior to undergoing surgery.11 It is postulated that providing information about risks and complications causes undue and unnecessary anxiety.16 This might be the reason behind our observation where only a few patients wanted to know all the details about their surgery and the complications. Our results show that preoperative anxiety was affected by the thought of operation success, complications and anaesthesia. It is well mentioned that patients tend to be more interested to know about what will happen to them during surgery and the outcome rather than understanding their surgical condition.11
Most of our patients (83%) were satisfied with the surgical outcome. Multivariate analysis was used to explore which factors influence patients’ satisfaction. Of the patient variables, better final visual acuity and occupation (housewife) were strongly associated with the satisfaction. The reason might be the adequacy of the visual performance in daily activities. However, selection bias leading to higher number of housewives in the study group may have lead to this observation.
The majority (61.9%) of our patients were not sure if they could withdraw the surgery at any time if they wished so which is similar (74%) to the observation made by Kang.10 From the ethical point of view, the consent will be valid only when the patient feels that it would have been possible to refuse and change their mind. It is possible only when patients understand the meaning and the significance of consent. Many patients (69%) thought that to sign the consent form was equivalent to agree for surgery. It reflects that these patients allow doctor to determine the treatment without blaming them of the possible adverse effects. Few (16.7%) patients considered the consent form as a medico-legal document which is, in fact, true from the doctor's perspective.17
To conclude, in this study most of patients were happy to let doctors decide their treatment. Many of patients wanted to know about the disease process, treatment involved and the success rate of surgery. Most of patients did not know what actually consent meant and why they were signing it. The success of the operation, the anaesthesia and a long list of complications tended to provoke anxiety. However, it must be recognized that most of patients want to know what their treatment involves. Although, some might be anxious, it should not mean that they do not need information. The information helps patients to cope with the treatment and helps to achieve better surgical outcome.
Conflict of interestsThe authors declare not to have any conflicts of interest.
We gratefully acknowledge the help of consultant ophthalmologists Dr Ranjana Sharma, Dr Purnima Raj Karnikar Sthapit and Dr Pooja Shrestha, ophthalmic assistant Mr Utsav Khoju and eye health worker Ms Urmila Nepal.
- 1.
Which statement best reflects your opinion regarding eye surgery?
- 1.
I will do what the doctor recommends
- 2.
I want to know what my treatment involves but will have it anyway as doctor knows best
- 3.
The treatment I have should be agreed after discussion of the pros and cons of the treatment and any alternatives
- 4.
I should make the final decision about my treatment
- 1.
- 2.
Which of the following statements best reflects your attitude when signing the consent form?
- 1.
It is a formality
- 2.
It is to protect the doctor against being sued
- 3.
It confirms that the operation and its effects have been explained to me
- 4.
It shows I have agreed to have the operation
- 1.
- 3.
Is the consent form a legal document
- 1.
Yes
- 2.
No
- 3.
Don’t know
- 1.
- 4.
Did you think you had to sign the consent form?
- 1.
Yes
- 2.
No
- 3.
Don’t know
- 1.
- 5.
Do you think you can change your mind once you have signed the consent forms?
- 1.
Yes
- 2.
No
- 3.
Don’t know
- 1.
- 6.
Do you think the preoperative interview and signing the consent form is important because:
- 1.
It gives me information
- 2.
It helps me make my mind up
- 3.
It protects the doctor medico-legally
- 4.
It is not important. I will do as the doctor says
- 5.
It is not important because I have decided to have the operation
- 1.
- 7.
Would you have an operation if there was risk of serious complication?
- a.
Yes
- b.
Depends of level of risk and need for operation
- c.
No
- a.
- 8.
Are you worried about these things?
- 1.
The anaesthetic
- 2.
Complications of the operation
- 3.
The operation being successful
- 1.
- 9.
Do you think that eye surgery:
- 1.
Is a harmless and easy procedure
- 2.
It is difficult or risk prone surgery?
- 1.
- 10.
Do you feel that you decided for this surgery or doctor decided it?
- 1.
Doctor
- 2.
Myself
- 3.
Both
- 1.
- 11.
Which of the following things would you want to be told before you have another operation? (multiple response)
- 1.
The nature of your ‘illness’
- 2.
The reason for the operation
- 3.
What will be done during the operation (in general terms)
- 4.
How you will feel after the operation?
- 5.
The important potential complications
- 6.
All complications
- 7.
No complications
- 8.
How long you should be off work
- 9.
The chances of a successful result of the operation
- 10.
Any special precautions you should take afterwards
- 1.
- 12.
Overall, are you satisfied with your surgical outcome? Yes/No
| 1. | How much are you satisfied with the preoperative information provided? | 1 | 2 | 3 | 4 | 5 |
| 2. | How much are you worried about the surgery? | 1 | 2 | 3 | 4 | 5 |
| 3. | How risky is the eye surgery? | 1 | 2 | 3 | 4 | 5 |
| 4. | How important is it for you to know the alternative treatments? | 1 | 2 | 3 | 4 | 5 |
| 5. | How much important is it for you to know about the improvement in vision after surgery? | 1 | 2 | 3 | 4 | 5 |
| 6. | How much necessary is it to give you the general details of the surgical procedure? | 1 | 2 | 3 | 4 | 5 |
| 7. | How much necessary is it to give you information about the anaesthetic? | 1 | 2 | 3 | 4 | 5 |
| 8. | How much necessary is it to know who is operating you? | 1 | 2 | 3 | 4 | 5 |