Age-related Macular Degeneration (ARMD) patients often describe complaints from neck and scapula area muscles and a decreased postural control. In clinical assessment, these complaints are considered to be due to old age.
PurposeThis study focuses on low-vision patients with ARMD, comparing them to age-matched controls without any eye disease, in order to evaluate if the linkage between self-rated visual complaints and musculoskeletal complaints is more prominent when low vision is present.
MethodsIn a cross-sectional study, 24 ARMD patients, aged 65 to 85, were compared to a group of 24 controls without visual problems having a similar age distribution. Visual acuity, the need for magnification plus other optical and visual parameters were assessed. Visual, musculoskeletal and balance/proprioceptive complaints were collected by means of a self-rating questionnaire. The Visual Functioning Questionnaire - Near Activities Subscale (VFQ–NAS) was used to evaluate visual function and related complaints.
ResultsThe correlation between visual complaints and musculoskeletal complaints yielded significant values of the correlation coefficient when performed separately within each group, as well as when calculated on the entire data set [ARMD, Spearman's rho (ρ)=0.60, P=0.002; control group ρ=0.59, P=0.004; both groups together ρ=0.50 P<0.001]. Stepwise multiple regression analysis supported the hypothesized effect of vision (Visual complaints + Minimum readable typefaces) on musculoskeletal complaints, (r2=0.42, P<0.05).
ConclusionsThe results in this study support the hypothesis that a relationship exists between visual and musculoskeletal problems.
Los pacientes con degeneración macular asociada a la edad (DMAE) a menudo refieren dolores musculares en el cuello y en la zona escapular, así como un menor control postural. En la evaluación clínica, se suele considerar que estas dolencias son debidas a la edad avanzada del paciente.
ObjetivoEste estudio se centra en los pacientes con DMAE y con baja visión, comparándolos con pacientes de referencia sin patologías oculares y de edades similares, con el fin de analizar si la conexión entre las afecciones visuales y las dolencias musculares (que refiere el paciente mismo) es más estrecha cuando el paciente padece baja visión.
MétodosEn un estudio transversal, se comparó un grupo de 24 pacientes con DMAE de edades comprendidas entre 65 y 85 años, con un grupo de 24 sujetos de referencia (controles) sin problemas visuales que presentaba una distribución de edades similar. Se obtuvieron datos relativos a la agudeza visual, a la necesidad o no de utilizar instrumentos con aumentos, así como a otros parámetros ópticos y visuales. Se recogieron datos sobre problemas visuales, dolencias osteomusculares y problemas de equilibrio/propiocepción, utilizando para ello un cuestionario que habían de contestar los pacientes mismos. Se utilizó la subsección sobre actividades de visión cercana del Cuestionario de la Función Visual (en inglés, Visual Functioning Questionnaire -Near Activities Subscale, o sus siglas VFQ–NAS) para evaluar la función visual y los problemas asociados.
ResultadosEl coeficiente de correlación entre los problemas visuales y los problemas de tipo osteomuscular alcanzó valores significativos tanto cuando la correlación se realizó en cada grupo por separado, como cuando se llevó a cabo analizando juntos todos los sujetos participantes [DMAE, rho de Spearman (ρ)=0,60, P=0,002; grupo de referencia (controles) ρ=0,59, P=0,004; los dos grupos juntos ρ=0,50 P<0,001]. El análisis de regresión múltiple escalonada (paso a paso) respaldó la hipótesis de que la visión (problemas visuales + tamaño mínimo de letra legible) influye sobre las dolencias osteomusculares (r2=0,42, P<0,05).
ConclusionesLos resultados de este estudio respaldan la hipótesis de que existe una relación entre problemas visuales y problemas de tipo osteomuscular.
Vision is one of the most important senses, functionally affecting other senses and motor control, thereby exercising vital effects on many bodily systems which, in turn, crucially affects everyday functioning and comfort. During the aging process, the body is subject to neural changes and other common complications, resulting in a decline in visual function and increasing disorders and impairments. In this respect, it is of interest to note that age-related macular degeneration (ARMD) is the most common disease leading to low vision in the western world, where the prevalence is so high that it is thought to involve one in three people at the age of seventy.1-4
Observations from low-vision clinics indicate that ARMD patients, besides their visual deficits (e.g., central field scotomas), also report musculoskeletal complaints, such as stiffness, fatigue and muscular pain in the neck/scapular area along with nausea and dizziness.5-7 Most of these complaints are considered to be due to normal aging; however, with diminishing eyesight and increasing demand on visual attention, a decreased near-work distance, higher levels of oculomotor load, the use of optical and technical magnification aids and the adoption of fatiguing postures, ARMD patients and other people with low vision may be at increased risk of developing musculoskeletal problems in the neck/scapular area, regardless of their age.8-11
Furthermore, musculoskeletal problems may also arise due to disturbed eye-hand coordination.
For example, skilled reach-to-grasp movements will likely not be appropriately calibrated when vision is impoverished.12 In real-life tasks, the visuomotor consequences (feedback) about the outcome of a goal-directed arm and hand movement becomes less accurate in low vision. A constrained visuomotor control strategy, aggravated by muscle stiffness and co-contraction of muscles not directly involved in producing the desired reach-to-grasp movement, is likely to result as compensation.13 The result may be prolonged static load leading to the development of fatigue, stiffness, muscular pain, as well as to disturbed proprioception, balance problems and dizziness.14 Since the information from the muscle spindles (proprioception) is used by the central nervous system for direct feedback control of movement, a vicious cycle of chronic muscle pain could also be initiated this way in some low vision patients.12-18
The purpose of this study was, therefore, to explore the extent to which reduced vision is associated with neck/scapular area muscular dysfunction and/or discomfort. The relative impact of the different aspects of visual function on musculoskeletal functioning was of particular interest in this context. This objective was achieved by testing if subjects with low vision are more likely to suffer from musculoskeletal problems, as compared to age-matched controls. Although many different types of linkages between visual and musculoskeletal comfort and function (in the context of ARMD and low vision) seem plausible, to date they remain relatively unexplored. The hypothesis is that a reduced visual function is associated with neck/scapular area muscular complaints.
MethodsParticipantsTwenty-four ARMD patients (10 males and 14 females) aged 61-87 (Mean=76.5 years and SD=6.7) were compared with 24 age-matched controls with normal vision (13 males and 11 females) aged 65-83 (Mean=73.7 years and SD=6.0). Controls were included only if they had recently undergone an eye examination (less than two years before the study), confirming normal vision for their age and no known eye disease. Control subjects were relatives or companions of low vision patients visiting the clinic that happened to match our criteria.
The ARMD group consisted of patients who had first contacted the low-vision clinic between 1998 and 2007 and who had been seen at the low vision clinic at least twice, which meant that the patients to be included in the study were selected only among those who had adapted to their visual impairment.
The ARMD patients were consecutively selected from the queue system of patients who required a new appointment with the clinic. All ARMD patients who matched the inclusion criteria were asked to participate. Among those ARMD patients that were asked, all but two agreed to participate in the study: One of them had to cancel the set appointment due to illness and the other one due to problems with transportation. The enrolled ARMD patients had not to date been treated with surgery or injections to prevent further visual loss. Those individuals (from both groups) who had been diagnosed with a condition (such as Arthritis, Multiple Sclerosis or Parkinson's disease) that could be the cause of perceived muscular pain, were excluded. To test for age equivalence, a group (ARMD/controls) by gender (male/ female), factorial ANOVA was conducted, revealing no significant differences (all P's>0.10). Levene's test for equality of age variance was non-significant (P>0.96), as was the case for both groups when using the Kolgomorov-Smirnov test of normal age distribution (P's>0.40), thus indicating that the age distribution in the two groups was equal and normal.
The study was performed according to the tenets of the Declaration of Helsinki. The Regional Ethical Review Board in Uppsala (Sweden), gave its approval to the study.
Visual AssessmentsBinocular Visual Acuity was assessed by measuring bestcorrected distant acuity using the ETDRS logMAR by-letter chart, which is designed and recommended for use in clinical trials. The measurements are described here as decimal Visual Acuity.
Binocular Near Visual Acuity was estimated with ETDRS logMAR near charts placed at a distance of 40cm, and described as one decimal measure. Normal or best distance correction was used plus the near addition of +2.5 D to neutralize the distance. Illumination was set to be approximately 1000 lx, as recommended during normal reading.
Need for magnificationTheir need for enlargement when reading was estimated. The calculations were done considering the addition of diopters from all normally used assisting visual aids. In the calculation, each unit of magnification is equivalent to + 4.0 D. For example, if 12 D spectacle microscopes were used, the calculation yielded 12/4 = 3 X. If 8 D reading glasses were combined with a 20 D hand-held magnifying aid, the equivalent magnification was 8/4 +20/4 = 7X.
None of the ARMD patients were totally dependent on technical aids (i.e. closed circuit television - CCTV), which means that all measurements refer to optical aids such as reading glasses and hand-held magnifying aids. This is not the exact angular magnification, but it gives an approximate estimate of the magnification needed.
AidsThe types of visual aids were recorded. If the visit resulted in a new prescription, which they liked and which led to a better performance, this was from then on considered as their present aid(s). Aids could either consist of optical or technical devices. Optical aids included a) single-vision reading glasses, b) bifocals, c) progressive lenses d) spectacle microscopes, e) handheld magnifying aids, either combined or used on their own. Technical aids consisted of CCTV.
Minimum readable printThe estimate of the minimum print size that could be read, with the assistance of their normal aids, was recorded. Usually, print sizes are given in “points” = pt (1 pt = 1/72 of an inch, and refers to the body size of the letter, where “8 pt” refers to normal typeface size used in advertisements and newspapers). Eight pt is approximately equal to N8.
Reading distanceThe distance between the text and the eyes was estimated using a measuring tape, when the subject was reading with the assistance of their normal optical or technical aids.
All visual measurements refer to the best-possible visual performance, permitting binocular vision.
Thus, monocular acuity was not established, nor was the extent to which the patient relied on binocular or monocular vision.
Self-rated assessmentsVisual FunctionThe National Eye Institute's Visual Functioning Questionnaire - Near Activities Subscale (NEIVFQ-NAS) was used to assess the participants’ self-rated visual quality. The NEI VFQ-25 is often used, and is known to be a valid and reliable tool for assessing self-rated visual function.15,16 In this study, only the six questions related to the near activities subscale were used, thus avoiding fatiguing questions in areas of minor interest. Each question could be answered by picking one of the six available alternatives. The sixth alternative (“Stopped doing this for other reasons or not interested in doing this”) is not related to the quality of vision, and therefore does not contribute to the total score. The five remaining alternatives indicate the quality of vision, ranging from 0 up to 100 at equal steps (i.e. 0, 25, 50, 75 and 100). The scores from the six questions were added and then divided by the number of questions to probe the quality of vision (according to the manual). This results in a total near-activity score. Generally, a total score above 75 indicates minor visual problems, whereas a score below 50 indicates pronounced visual problems. Low scores on NEI VFQ-25 have been associated with marked problems related to near visual activities, general health issues and a reduced quality of life.16
ComplaintsTo obtain information regarding balance/proprioceptive, visual- and musculoskeletal complaints, a new questionnaire was prepared. For each of these areas, five questions were asked. Each question was answered using a visual analogue scale (VAS), ranging from 0 (no problem at all) to 10 (problems all the time), with verbal anchors set at 3 (occasionally) and at 7 (quite often). Those who found it difficult to estimate a precise value on their own could orally decide what they wanted to score on each question. The scores from the five questions asked corresponding to a given area of interest were added up; thus, the total score could vary between 0 and a maximum value of 50.
The following questions were asked with regard to visual complaints:
- 1)
Do you have problems with blurred or double vision when reading or performing near activities?
- 2)
Do you feel irritation or smarting pain in the eyes when reading or performing near activities?
- 3)
Do you find it difficult to focus on the text when reading a newspaper or a book?
- 4)
Do you get headaches when concentrating on a near activity?
- 5)
Do you get nausea or a sensation of illness when performing a prolonged near activity?
The following questions were asked dealing with balance/proprioception:
- 1)
Do you find it difficult to maintain your balance when you raise yourself up from a sitting position to a standing position?
- 2)
Do you find it difficult to estimate the distance to the ground when walking?
- 3)
Do you find it difficult to pour yourself a cup of coffee?
- 4)
Do you find it difficult to maintain your balance when standing without support?
- 5)
Do you find it difficult to maintain your balance when performing quick head movements, as for instance, when crossing the street?
The following questions were asked dealing with musculoskeletal complaints:
- 1)
Do you feel a sensation of burning, aching in your neck and shoulders when reading?
- 2)
Do you feel a sensation of burning or aching in your neck or shoulders when looking at a person who is giving a speech?
- 3)
Do you feel a sensation of burning or aching in your arms, back, neck or jaws when concentrating on a near activity?
- 4)
Do you have to rub or massage your neck in order to carry out a prolonged near activity?
- 5)
Do you ever have to quit a near activity because of a too strong sensation of burning, aching in your neck and shoulders?
All ARMD patients were recruited from the queue system established when they had contacted again the low vision clinic with the purpose of getting better spectacles or reading aids, after their first rehabilitation period finished. All patients, strictly following the order on the list, were asked to participate if they met the inclusion criteria. Informed consent was given. If they agreed to attend, they could either choose to receive the questionnaires in advance, or to wait until the set appointment, where the questionnaire could be completed with the help of the personnel at the low vision clinic. Although ARMD patients could use technical or optical aids to be able to complete the questionnaire on their own, nearly all of them chose to have an assistant reading the questionnaire for them. If the ARMD patients could perform better with the new aids, compared to their usual aids, the recorded visual measurements referred always to best-possible visual performance. Controls, prior to further assessments in the study, were tested to ensure that they were able to achieve normal visual acuity values (0.8-1.0, as corresponding to their age) with normal correction.
Statistical AnalysisTo test for age equivalence, a group (ARMD/controls) by gender (male/female), factorial ANOVA test was conducted. Moreover, Levene's test for equality of age variance was conducted, as well as the Kolgomorov-Smirnov test of normal age distribution.
All optical assessment results refer to the best-possible visual performance, permitting either binocular or monocular solutions. Independent samples of Mann-Whitney U-test were used in order to carry out intergroup comparisons for all optical, functional and symptom-related assessments included in the study. Spearman's rho (ρ) was used for the correlation analysis. In order to find out which are the most influential and impacting factors on musculoskeletal complaints and to evaluate the influence of optical and visual factors, three stepwise (forward) multiple regression analyses (with entry P<0.05 and removal P>0.10) were performed, using all the data from the optical and functional measurements and the remaining complaints. All statistical analyses were carried out using SPSS 15 for Windows (manufactured by SPSS Inc., Chicago, Illinois, USA). P-values below 0.05 were considered to be significant (2-tailed).
ResultsMean values and interquartile ranges corresponding to the different visual assessment variables are shown in table 1. The visual assessments confirmed that ARMD patients had reduced eyesight compared to age-matched controls. ARMD patients showed significantly lower visual acuity, both at a distance (4 m) and at shorter reading distances (40cm), compared to controls. ARMD patients needed significantly higher levels of magnification in terms of optical and technical supportive aids, had shorter reading distances and could only perform reading tasks when larger print size was used. The complaint questionnaire's reliability was tested and resulted in a Cronbach's alpha of 0.81 for those items related to visual complaints, an alpha of 0.85 for musculoskeletal complaints and an alpha of 0.88 for balance/ proprioception, which indicates that all sections show an adequate reliability.17
Mean (Mean) and standard deviations (SD) of visual assessments variables
| AMD'S | AMR'S | |||||
| Mean | SD | Mean | SD | Mean difference | P | |
| Visual acuity at 4 m | 0.18 | 0.12 | 1.10 | 0.25 | -0.92 | <0.001 |
| Visual acuity at 40 cm | 0.22 | 0.16 | 0.98 | 0.26 | -0.75 | <0.001 |
| Reading distance (cm) | 19.30 | 6.42 | 40.83 | 5.65 | -21.5 | <0.001 |
| Need of magnifying aid (X) | 6.02 | 1.38 | 0.62 | 0.07 | 5.40 | <0.001 |
| Minimal readable typeface-size (p) | 10.96 | 10.04 | 4.79 | 0.51 | 6.17 | <0.01 |
All assessments refer to best possible visual performance, permitting binocular vision if possible. Note: Near visual acuity at 40 cm was estimated with the additional optical aid of +2.5 D AMD= Age related Macular Degeneration patients. AMR= Age matched referents.
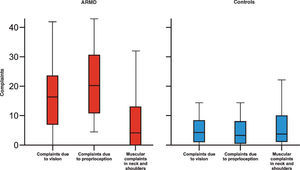
The assessment of near visual function (VFQ-NAS) revealed significant differences between the two groups. Mean VFQ-NAS score for the ARMD group was significantly lower than that obtained among controls. Compared to controls, ARMD patients scored significantly higher on all complaint categories, except for that regarding musculoskeletal complaints. Finally, in our study the VFQ - NAS gave a resulting Cronbach's alpha of 0.957(Table 2andFigure 1).
Results from questionnaires
| AMD | AMR | |||
| Mean (SD) | Mean (SD) | Difference | P-value | |
| VFQ-NAS | 35,70 (20,27) | 96.90 (3.89) | -61.20 | <0.001 |
| Visual complaints | 16,71 (11,98) | 4,71 (4,01) | 12,00 | <0.001 |
| Neck complaints | 8,98 (10,69) | 6,25 (6,55) | 2,73 | 0.290 |
| Complaints due to proprioception | 21,67 (11,63) | 4,48 (4,19) | 17,19 | <0.001 |
VFQ-NAS = Visual Functioning Questionnaire- Near Activities Subscale. AMD= Age related Macular Degeneration patients. AMR= Age matched referents.
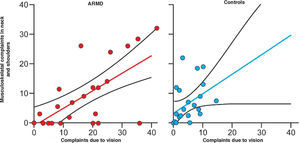
The correlation coefficient between visual complaints and musculoskeletal complaints yielded significant values when computed separately within each group as well as when calculated on the entire subject sample (ARMD: ρ=0.60, P=0.002; control group: ρ = 0.59, P=0.004; both groups together: ρ=0.50 P<0.001).
Since the relationship between visual complaints and musculoskeletal complaints was the only significant value within the two groups, this correlation was examined more closely. A scatter plot representing this correlation is shown in figure 2, where it becomes evident that a correlation between visual and muscular complaints does exist. Furthermore, several ARMD patients had prominent visual complaints compared to controls. Some ARMD patients reported severe visual complaints but, interestingly, no or very few muscular complaints. When applying a 99% confidence interval to the regression lines in figure 2, four ARMD patients were clearly below the lower limit of the confidence interval.
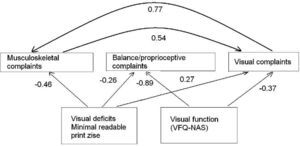
In order to more rigorously scrutinize the hypothesized impact of visual deficiencies on musculoskeletal complaints, three stepwise multiple regression analyses were performed. All variables (i.e. gender, age, group, optical assessment, VFQ-NAS, and symptomatic assessments) were regressed on the muscular complaints, balance/proprioceptive complaints, and visual complaints, respectively. The results of the three regression analyses are shown intable 3 and further significant relationships are illustrated in the path diagram infigure 3. Only two among the visual function and visual deficit variables had a significant impact on complaint variables. Minimum readable print size had a significant impact on all three complaint variables, whereas VFQ-NAS had a significant influence on two of them (balance/proprioception and visual complaints). Also, as shown in the path diagram, visual and musculoskeletal complaints are interrelated, though visual complaints seem to have a greater influence on musculoskeletal complaints than vice versa.
Resulting standardized coefficients obtained from stepwise multiple regression analysis
| Independent variables | Dependent variables Visual complaints β | Balance/proprioception complaints β | Musculosleletal complaints β |
| Group | -0.146 | -0.168 | 0.116 |
| Gender | -0.052 | 0.000 | -0.025 |
| Age | -0.026 | -0.028 | -0.003 |
| Visual acuity (distance) | -0.100 | -0.049 | 0.072 |
| Visual acuity (short distance) | 0.065 | -0.022 | -0.066 |
| Minimum readable font size | -0.372** | -0.888*** | -0.455*** |
| Binocular/Monocular | 0.063 | 0.120 | 0.121 |
| Type of Aids | -0.139 | -0.002 | 0.120 |
| Magnification | 0.047 | -0.024 | -0.016 |
| Reading distance | -0.060 | -0.047 | 0.129 |
| Pupil size | -0.103 | -0.131 | -0.023 |
| VFQ-NAS | 0.265* | -0.255* | 0.037 |
| Visual complaints | - - - | 0.186 | 0.771*** |
| Balance/proprioception complaints | 0.167 | - - - | -0.039 |
| Muscular complaints | 0.535*** | 0.083 | - - - |
| Model r2 | 0.660 | 0.570 | 0.498 |
β= standardized regression coefficient. All β are based on the final step in the regression analysis. β values in bold font are statistically significant. Non-significant β’s are excluded from model r2.
To our knowledge, this is one of the first studies that has investigated the existence of a linkage between visual and musculoskeletal complaints in old age. Despite the potentially large number of individuals affected, little is known about musculoskeletal health in people with low vision.
The results from this study suggest that visual and balance/proprioceptive complaints (but not musculoskeletal complaints) constitute age-independent effects of low vision. The ARMD patients reported that they occasionally suffer from blurred or double vision, asthenopia, nausea, headache, and reading problems. ARMD patients also reported occasional complaints related to balance, depth perception and eye-hand coordination tasks. Controls reported no such complains. Visual and balance/proprioceptive complaints were more pronounced relative to the musculoskeletal complaints, with the latter being, on average, rather modest and similar across groups.
The strong co-variation between visual and musculoskeletal complaints in the ARMD and in the control group confirms the hypothesis that a reduced visual function is associated with neck/scapular area muscular complaints. The linear stepwise regression analysis extended these findings further by indicating that visual complaints and minimum readable typefaces were both important predictive factors for musculoskeletal complaints. The stepwise linear regression analysis also identified self-rated visual quality to be the parameter with the highest impact on balance/proprioception. The combination of these results strongly suggests that individuals with low visual acuity, who require a larger print size, are more likely to experience disabling discomforts and complaints from muscles in the neck/scapular area.
These results are consistent with other published reports found in the literature and with clinical observations. High levels of oculomotor load have been associated with musculoskeletal complaints related to neck-scapular area muscles.10-12 Low vision does produce poor and insufficient visual information regarding the location of objects in the external environment and adversely influences motor control, thereby leading to muscle stiffness and pain.18,19 Balance/proprioception disturbances are also classical outcomes of musculoskeletal disorders.20
As more adults are extending their working life into old age, it may become progressively more important to prevent disorders in the neck/scapular area muscles that originate from low vision and prolonged exposure to mechanical loads in near-work conditions. More knowledge of the influence of risk factors could result in the possibility to offer a preventive treatment to those at risk,21-23 thereby improving the quality of life for people with low vision and muscular complaints.
The power analysis done prior to this study suggested a sample size of 16 participants in each group, in order to be able to identify statistical differences between the groups. Differences were noticed, but not all differences were significant, probably due to the limited number of participants. Therefore, a follow-up study including more ARMD patients and a broader range of measurements is warranted. In conclusion, more research is necessary in order to understand the eye-neck/scapular area linkages that exist in ARMD-patients as well as in age-matched controls.
This study was supported by grants from the Centre of Rehabilitation research, Örebro University Hospital, Sweden.
Financial disclosure: None of the authors has a financial interest in any of the devices described in the present work.