A novel protocol to improve long-term results in the treatment of amblyopia was proposed. The protocol combines active home-based therapy through perceptual learning activities (Gabor patch, dichoptic stimulation, and random dot stereograms) with conventional visual therapy in the clinic as an adjunct to patching occlusion in subjects with patch-resistant amblyopia
MethodsBetween 2018 and 2022, a group of patients received treatment for persistent strabismic and combined-mechanism amblyopia according to the novel treatment protocol, consisting of in-clinic orthoptics/visual therapy combined with the use of gamified PL software at home, as an adjunct to occlusion treatment.
ResultsA retrospective analysis of treatment outcomes was subsequently carried out for 53 patients aged 7.75±5.88. Eccentric fixation was present in 17 of the 53 subjects.
The distribution of patients presenting with combined-mechanism and strabismic amblyopia was 37 and 16, respectively. Eighteen patients (34 %) demonstrated measurable stereoacuity prior to treatment. Following treatment using the combined treatment protocol, forty-six (87 %) participants achieved a of logMAR 0.1 or better, mean BCVA was significantly improved, from logMAR 0.30±0.23 to logMAR 0.07±0.12 (p < 0.01). Eleven subjects (65 %) of seventeen participants with eccentric fixation achieved central fixation. In addition, stereoacuity was measurable in 43 patients (81 %). Mean stereoacuity improved, from 1200.00±258.69 arc seconds to 539.62±518.69 arc seconds (p < 0.01). These results remained stable six months after completion of the therapy.
ConclusionThe outcomes of the proposed novel treatment protocol were reduced angle of deviation, and improved BCVA and stereoacuity in patients with persistent strabismic and combined-mechanism amblyopia.
Disruption of normal visual development early in life may result in perceptual, oculomotor and clinical abnormalities such as instability of fixation, anomalous retinal correspondence, and lack of stereoacuity.1 The global prevalence of amblyopia is between 1.3 and 4 %.2,3 Amblyopia is associated with refractive error (anisometropia or isometropia) and strabismus.4
The gold standard treatment prescribed for this condition combines spectacle correction of the refractive error with penalization and/or occlusion of the dominant eye,5 known as passive therapy (i.e., requiring no action from the patient).6 The main outcomes can be summarized in three points:2 failure to achieve normal visual acuity in around 50 % of patients; little improvement in terms of stereoacuity; and reported recurrence of the condition in 25 % of successfully treated amblyopic children within the first year of treatment. For esotropic amblyopia, the recurrence ratio is even higher (recurrent amblyopia requiring retreatment was determined in 60 % of patients during the 5-year follow-up in one 2013 study).2
Buckle et al.7 analysed the results of occlusion therapy in amblyopic subjects in a hospital in order to determine a “real life” benchmark for treatment outcomes in clinical practice. Although the outcomes in terms of visual acuity were similar to those previously obtained by occlusion therapy, a “plateau” of no further improvement was observed at 32 weeks for mild, and 48 weeks for severe amblyopia.7
Active therapy requires the patient's active participation.6 Baker et al.8 proposed that the mechanisms responsible for integrating information received by both eyes remain intact but are suppressed in patients with amblyopia. To restore binocular vision, the contrast or luminance of the image perceived by the dominant eye is reduced. Subsequent studies have explored this concept, suggesting that the stimuli for the amblyopic eye are enhanced (e.g., increased contrast or brightness), while the stimuli for the dominant eye are diminished (e.g., reduced contrast). This adjustment creates a perceptual balance that promotes the active engagement of the amblyopic eye through dichoptic therapy.9 Dichoptic therapy uses dichoptic elements inserted in videogames10–16 or films.17,18 The results of dichoptic therapy in terms of visual acuity are inconsistent, producing similar or better than results to those obtained by spectacle correction alone14,15 and occlusion,11,17 in some cases, and inferior results in others,12,13,16,19 for reasons which are unclear.21 Regarding stereopsis, the results are poor in anisometropic amblyopia and anecdotal in strabismic amblyopia with both occlusion19 and dichoptic therapy.11,12,13,16,20
Notwithstanding, dichoptic therapy has never, to the authors’ knowledge, produced results superior to those obtained using a passive therapy protocol in isolation, according to clinical trial studies comparing the two strategies.9,21
Regarding the strabismic angle in amblyopia, dichoptic therapy studies included only strabismic subjects with microtropia (<12 prism diopters).10,11,15,16,18,19 The reviewed studies show no significant changes in deviation angles between pre- and post-treatment,12,16,21 with results similar to those obtained using occlusion or atropine.22
Recent studies have combined active and passive therapy in a single protocol, with promising results in anisometropic23 and strabismic amblyopia.24 In this study, patients with strabismic amblyopia underwent a combined treatment approach that included occlusion and prismatic correction of esotropic deviation, followed by fusional vergence therapy or surgery for larger angles (>12 prism diopters).
Recently, in a quasi-experimental multicentric study, subjects with persistent amblyopia treated with a combination of active and passive therapy obtained best outcomes than subjects with passive treatment alone.25 In this case, the active therapy consisted of dichoptic therapy, vergence therapy, and direct stimulation of stereopsis.
This study aims to analyze the outcomes of an amblyopia treatment protocol that combines active therapy (dichoptic therapy, vergence therapy, and direct stereopsis stimulation) with passive therapy (occlusion and prismatic correction of the deviation, when necessary).
MethodsStudy designThis study is a pseudo-experimental, pre-post, retrospective study. As a retrospective analysis, it did not include a control or placebo group, which limits causal inference regarding treatment efficacy. The present study analysis of treatment outcomes in patients who received treatment at Begira Clinic in Bilbao (Basque Country, Spain) between 2018 and 2022. These patients, both children and adults, presented with persistent strabismic and combined-mechanism (anisometropic and strabismic) amblyopia; all had previously undergone passive therapy that had failed to result in normal visual acuity. The study was approved by the Basque Country Ethical Committee of Clinical Research (CEIC-E22/34), Spain.
SubjectsThe patient inclusion criteria were as follows: persistent strabismic and combined-mechanism amblyopia (strabismus and anisometropia). Anisometropia was defined as a difference of 1 or more diopters in spherical equivalent.26 A subject had persistent amblyopia if, despite having been previously treated with optical correction and occlusion or penalty for >32 or 48 weeks, the difference in logMAR acuity between amblyopic and dominant eyes was ≥2 lines; and a BCVA of logMAR worse than 0.10 (equivalent to 0.8 decimal visual acuity).7 Mild amblyopia was classified as being logMAR BCVA visual acuity of 0.13 to 0.30, moderate amblyopia as being worse than 0.30 to 0.70, and severe amblyopia as being worse than 0.70.27 Patients with ocular pathology, paretic or paralytic strabismus, congenital strabismus, strabismic surgery, vertical deviations, nystagmus or cognitive delay were excluded from the study.
The study included 53 patients (34 males and 19 females) with a mean age of 7.75 ± 5.88 years (range: 4–42 years). Sixteen participants (30 %) had strabismic amblyopia, while 37 (70 %) were diagnosed with combined-mechanism amblyopia (the coexistence of anisometropia and strabismus). Central fixation was observed in 36 patients (68 %), whereas 17 (32 %) exhibited eccentric fixation. Eight patients (15 %) were classified as having anomalous sensory correspondence (ASC), while 45 (85 %) had normal sensory correspondence (NSC). Five participants (9 %) had severe amblyopia, 20 (39 %) had moderate amblyopia, and 28 (52 %) had mild amblyopia (as shown in Figure 2 and the supplementary material in Table 1).
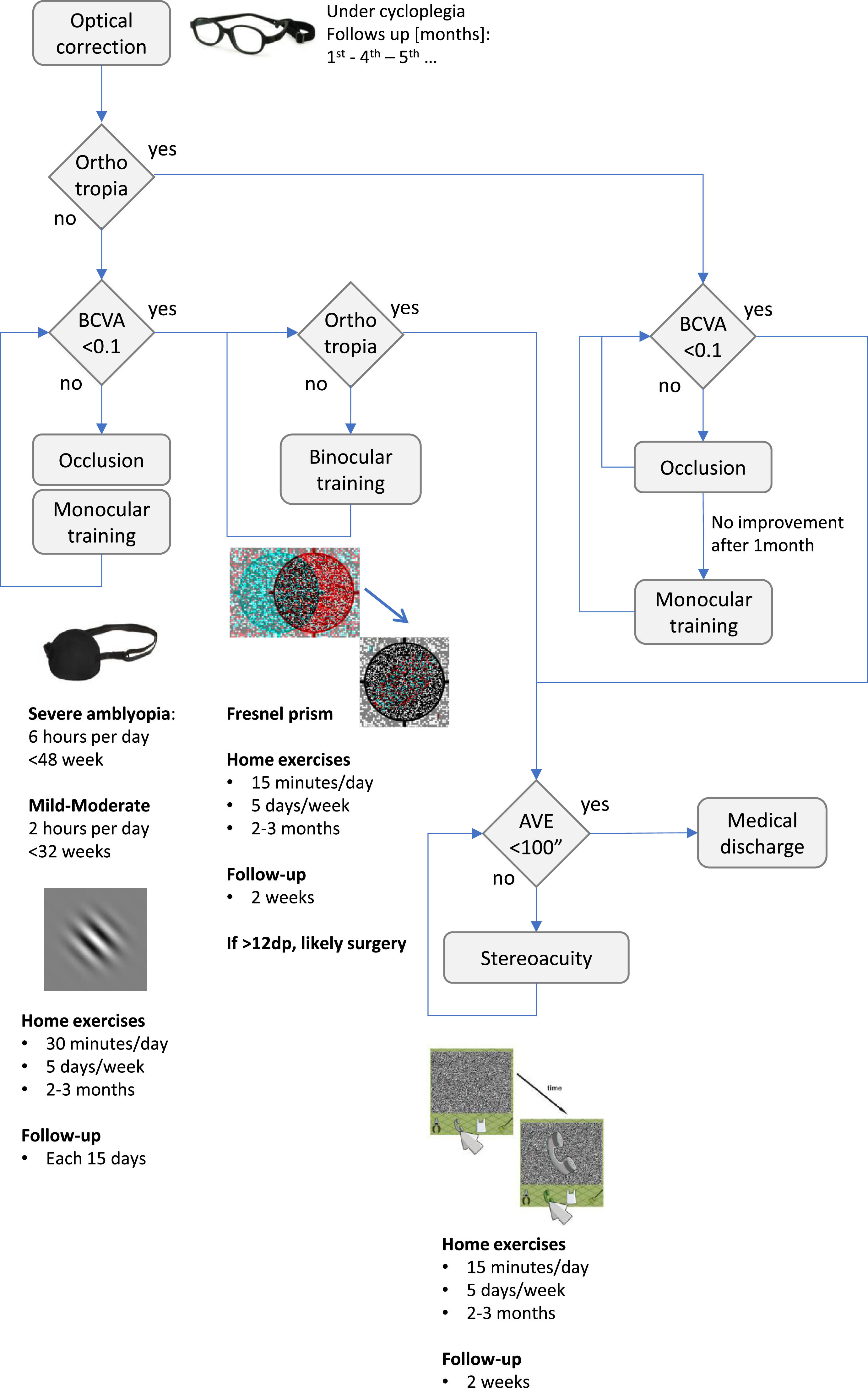
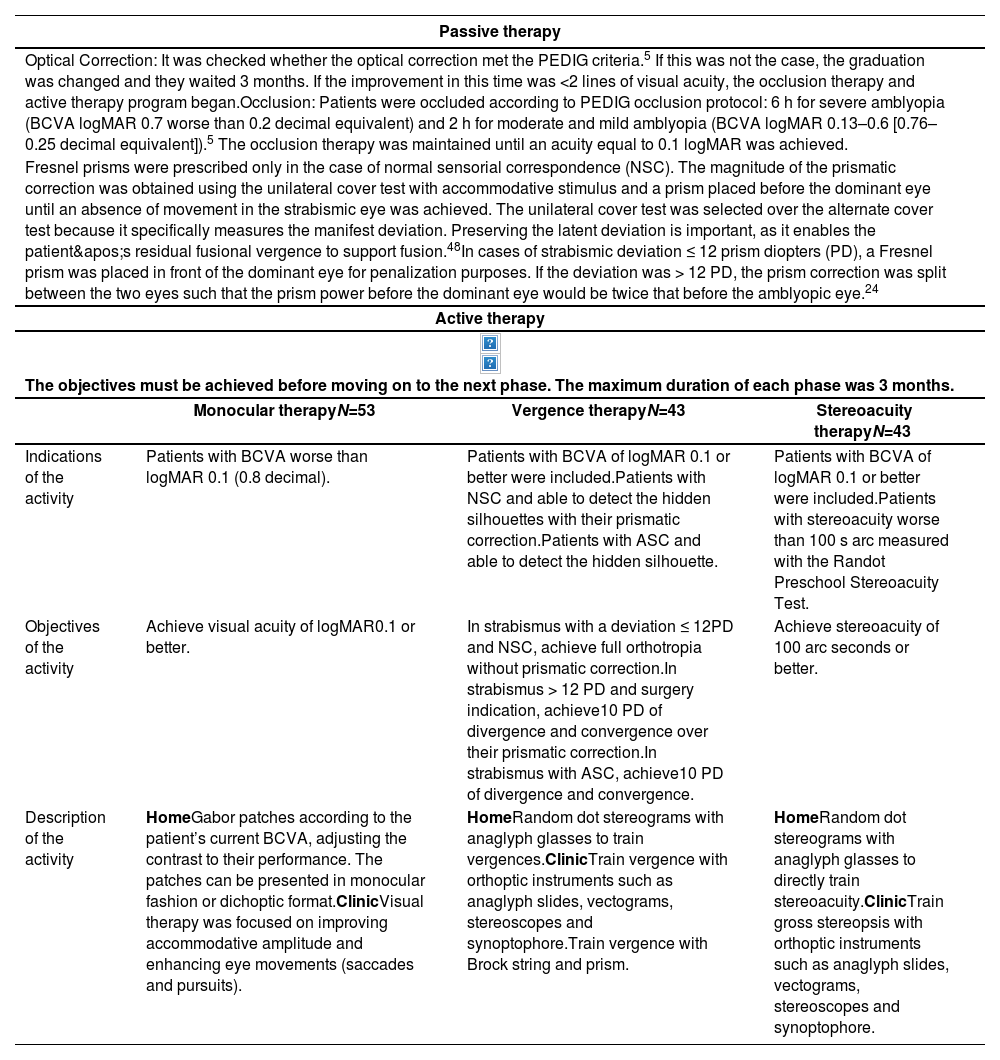
Passive therapy and active therapy strategies included in the study protocol.
| Passive therapy | |||
|---|---|---|---|
| Optical Correction: It was checked whether the optical correction met the PEDIG criteria.5 If this was not the case, the graduation was changed and they waited 3 months. If the improvement in this time was <2 lines of visual acuity, the occlusion therapy and active therapy program began.Occlusion: Patients were occluded according to PEDIG occlusion protocol: 6 h for severe amblyopia (BCVA logMAR 0.7 worse than 0.2 decimal equivalent) and 2 h for moderate and mild amblyopia (BCVA logMAR 0.13–0.6 [0.76–0.25 decimal equivalent]).5 The occlusion therapy was maintained until an acuity equal to 0.1 logMAR was achieved. | |||
| Fresnel prisms were prescribed only in the case of normal sensorial correspondence (NSC). The magnitude of the prismatic correction was obtained using the unilateral cover test with accommodative stimulus and a prism placed before the dominant eye until an absence of movement in the strabismic eye was achieved. The unilateral cover test was selected over the alternate cover test because it specifically measures the manifest deviation. Preserving the latent deviation is important, as it enables the patient's residual fusional vergence to support fusion.48In cases of strabismic deviation ≤ 12 prism diopters (PD), a Fresnel prism was placed in front of the dominant eye for penalization purposes. If the deviation was > 12 PD, the prism correction was split between the two eyes such that the prism power before the dominant eye would be twice that before the amblyopic eye.24 | |||
| Active therapy | |||
| The objectives must be achieved before moving on to the next phase. The maximum duration of each phase was 3 months. | |||
| Monocular therapyN=53 | Vergence therapyN=43 | Stereoacuity therapyN=43 | |
| Indications of the activity | Patients with BCVA worse than logMAR 0.1 (0.8 decimal). | Patients with BCVA of logMAR 0.1 or better were included.Patients with NSC and able to detect the hidden silhouettes with their prismatic correction.Patients with ASC and able to detect the hidden silhouette. | Patients with BCVA of logMAR 0.1 or better were included.Patients with stereoacuity worse than 100 s arc measured with the Randot Preschool Stereoacuity Test. |
| Objectives of the activity | Achieve visual acuity of logMAR0.1 or better. | In strabismus with a deviation ≤ 12PD and NSC, achieve full orthotropia without prismatic correction.In strabismus > 12 PD and surgery indication, achieve10 PD of divergence and convergence over their prismatic correction.In strabismus with ASC, achieve10 PD of divergence and convergence. | Achieve stereoacuity of 100 arc seconds or better. |
| Description of the activity | HomeGabor patches according to the patient’s current BCVA, adjusting the contrast to their performance. The patches can be presented in monocular fashion or dichoptic format.ClinicVisual therapy was focused on improving accommodative amplitude and enhancing eye movements (saccades and pursuits). | HomeRandom dot stereograms with anaglyph glasses to train vergences.ClinicTrain vergence with orthoptic instruments such as anaglyph slides, vectograms, stereoscopes and synoptophore.Train vergence with Brock string and prism. | HomeRandom dot stereograms with anaglyph glasses to directly train stereoacuity.ClinicTrain gross stereopsis with orthoptic instruments such as anaglyph slides, vectograms, stereoscopes and synoptophore. |
Visual evaluation included best-corrected visual acuity (BCVA) measured in logMAR using a single-letter Snellen E chart with crowding bars (OptoTab Polar; SmarThings4Vision, Spain). Central or eccentric fixation was assessed with a Visuscope (Beta 200, Heine, Germany). The Simultaneous Prism and Cover Test was used to measure tropia at distance (4 m) and near (1/3 m or 33 cm) with an accommodative target (an isolated letter two lines below the visual acuity of the amblyopic eye).
Refractive error was determined using an automated refractor (TRK 1P, Topcon, Japan) and/or retinoscopy under cycloplegia (cyclopentolate 1 %) following the Pediatric Eye Disease Investigator Group (PEDIG) guidelines.5 For esotropia, full cylinder and full myopia corrections were prescribed. In cases of hyperopia, to eliminate all accommodative components, full hyperopia correction was prescribed, allowing a reduction of −0.50 D in each eye. Simultaneously, an evaluation of the anterior and posterior segments was performed.
Binocular vision (fusion, suppression, or diplopia) was evaluated at four metres, using the Worth Four Dot test on a polarized screen (SmarThing4Vision, Spain) for two target sizes (visual angles of 1.5° and 5.0°). Patient responses were ordered according to the extent of their suppression scotoma. A scale of six categories from 0 to 5 was thus obtained, whereby 0 = suppression with both target sizes; 1 = suppression of 1.5º and diplopia 5º; 2 = diplopia of 1.5º and 5º; 3 = fusion of 5º and suppression 1.5º; 4 = fusion of 5º and diplopia 1.5º and 5 =fusion with both target sizes.28 A synoptophore (Wetzlar, Oculus, Germany) was used to evaluate fusion capacity at the objective and subjective angle of deviation. If the patient was able to fuse at the objective angle (the angle between the visual axes measured objectively using peripheral fusion cards), NSC was defined. Conversely, the subjective angle refers to the angle of strabismus as perceived by the patient. If the patient fused at the subjective angle, ASC was defined.29 Only patients who achieved fusion with the synoptophore at their target angle underwent dichoptic therapy.
Stereoacuity measurements were taken with the Randot Preschool Stereoacuity Test (Stereo Optical, USA). Patients whose responses indicated nil stereoacuity were then evaluated with the TNO test (Lameris Instrumenten, Netherlands), using qualitative Plates III, IV and V, assuming a quantifiable value of 1200 arc seconds.24 An arbitrary value of 1300 arc seconds (“ecological stereoblindness”) was assigned to patients with no measurable stereoacuity.30
Treatment fundamentalsThe treatment protocol comprised both passive and active therapeutic strategies, as detailed in Table 1.5,24,25,31 In summary, passive therapy involves optical correction, occlusion therapy, and prismatic correction (applied when necessary and exclusively in patients with NSC). Conversely, active therapy is conducted both at home and in the clinic. At home, it is carried out through dichoptic therapy, vergence training, and direct stereoacuity stimulation using a specialized computer program (https://www.visionarytool.com).25 In the clinical setting, traditional visual therapy and orthoptic exercises are implemented.31
Phases of treatmentFigure 1 summarizes the treatment received between baseline and final evaluation. Four phases are differentiated: (1) passive therapy; refractive correction, prismatic correction and occlusion, (2) monocular training, (3) vergence training, and (4) stereoacuity training.
Passive therapy The passive therapy data is summarized in Table 1. Briefly, based on optical correction and posterior occlusion of dominant eye following PEDIG criteria.5 Hourly occlusion was maintained until an acuity equal to 0.1 logMAR was achieved.
Active therapyTable 1 shows the indications, objectives, and activities performed by the participants.
Monocular training: in this active therapy phase, BCVA was the target function. The criteria for commencing monocular training were a BCVA worse than logMAR 0.1, and no improvement after three months of passive therapy.
The at-home visual therapy exercises were based on Gabor patches, using Visionary Tool software.25 The software selects the frequency of the Gabor patches according to the patient’s current BCVA and adapts the contrast to their performance. The patches can be presented in either monocular (with an occluder) or dichoptic format (with blue-red googles). Patients with eccentric fixation, or ASC, performed the Gabor patch with an occluder to avoid horror fusionis and potential diplopia.
The usual prescription consisted of a 30-minute session, five days per week, for two to three months. If no improvement was demonstrated at the end of three months, home therapy was discontinued. Clinical visual therapy exercises were carried out at follow-up visits every two weeks. Traditional visual therapy focused on improving accommodative amplitude and enhancing eye movements (saccades and smooth pursuits).31
Vergence training: the vergence training phase was exclusive to subjects with a BCVA of logMAR 0.1 or better and NSC. Patients with ASC were included if they were able to see the hidden silhouette in a random dot format.
The final goal of this phase was to obtain binocular correspondence in orthotropia without any prismatic correction. Active therapy made use of several orthoptic instruments such as anaglyph slides, vectograms and stereoscopes.
At-home visual therapy activities were based on random dot stereograms with anaglyph glasses to train vergences, using Visionary Tool.25 The usual prescription consisted of a 15-minute session, five days per week, for two to three months, with compliance checked via the Visionary server and patient confirmation.25
In patients presenting with esotropia ≤12 PD, prism power was progressively reduced. The amount of prismatic reduction was equal to half the divergence capacity with the computer software.24
Direct stimulation of stereoacuity: this phase was indicated for patients who either presented with stereoacuity worse than 100 arc seconds. Active therapy with Visionary Tool at-home visual therapy, involving activities based on random dot stimuli with anaglyph glasses, was prescribed. The average prescription consisted of a 15-minute session, five days per week, for two to three months. 25,32
ComplianceCompliance with treatment was calculated considering a frequency of at least five sessions per week (over 20 sessions per month). The following formula was used to determine percentage compliance. For example, in a 3-month treatment, 60 sessions would be 100 % compliance.
Statistical analysisStatistical analysis was performed using the SPSS 26.0 (SPSS, Chicago, IL, United States). A non-parametric distribution of data was verified with the Kolmogorov-Smirnov test (p < 0.05). The results are presented as a mean ± standard deviation (SD) with a 95 % confidence interval (CI). The Wilcoxon test was used to compare all the study parameters at different visits. Different groupings – according to the presence or otherwise of ASC, combined-mechanism or strabismic amblyopia, and central or eccentric fixation – were compared using the Mann-Whitney U test.
The effectiveness of the proposed treatment was evaluated by means of BCVA (amblyopic eye), binocular vision (suppression scotoma), deviation (near and far distances) and stereoacuity with the Wilcoxon rank sum test. The presence or absence of eccentric fixation, ASC, and anisometropia in addition to strabismus was taken into consideration when comparing results among patients across all study visits. BCVA is presented in logMAR and stereoacuity value was converted to a value of log10 for analysis.
In addition, an analysis was conducted to determine whether the observed improvement was clinically significant. An improvement in BCVA was defined as a final acuity equal to or better than 0.10 logMAR (equivalent to a decimal visual acuity of 0.8). Conversely, an improvement in stereoacuity was defined as an increase of two levels from the initial measurement.
ResultsThe results of the different groups will be presented based on the visits conducted, in order to facilitate the comparison of each group's progression.
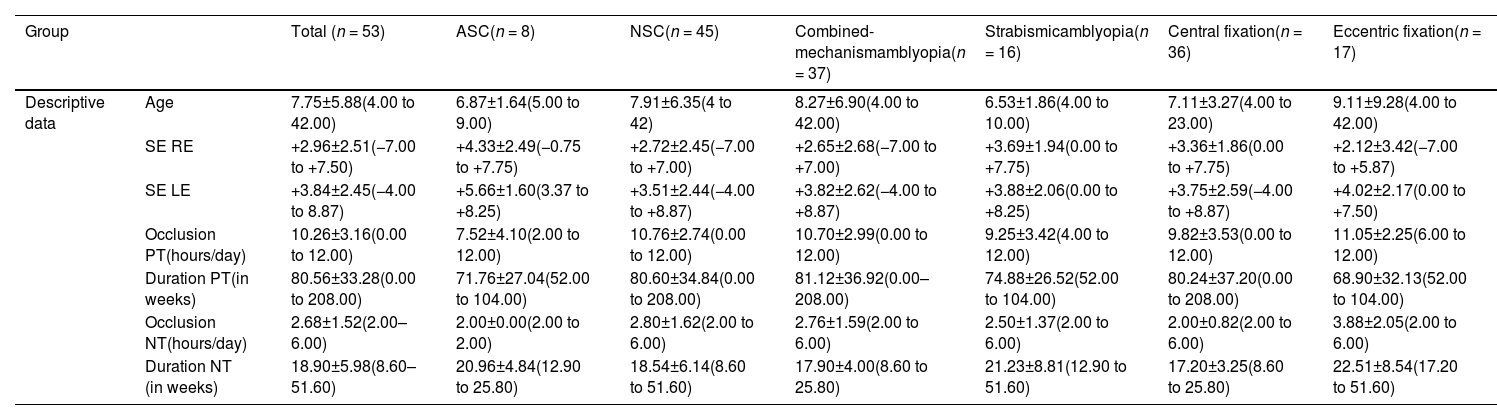
Baseline descriptive dataBaseline descriptive data are presented in Table 2. The mean best-corrected visual acuity (BCVA) in the amblyopic eye was 0.30 ± 0.23 logMAR (range: 0.15–1.30), compared to 0.02 ± 0.04 logMAR (range: 0.00–0.22) in the dominant eye. Notably, 17 participants exhibited eccentric fixation.
Descriptive data analysis of results across the total sample and different subgroups.
Abbreviations: n, sample size; ASC, anomalous sensorial correspondence; NSC, normal sensorial correspondence; SE, spherical equivalent; RE, right eye; LE, left eye; PT, previous treatment; NT, new treatment.
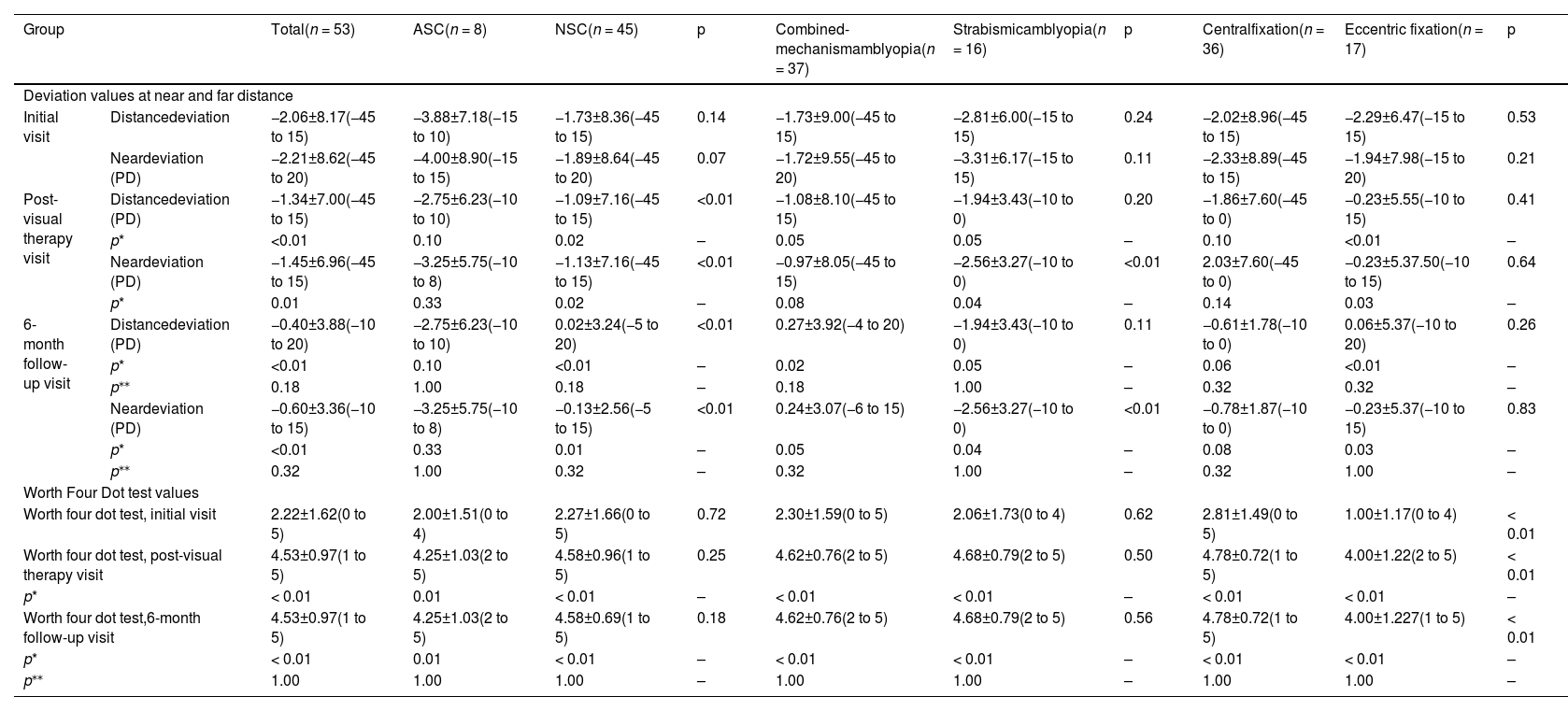
The mean angles of deviation at far and near distances were −2.06 ± 8.17 prism diopters (PD) (range: −45 to 15 PD) and −2.21 ± 8.62 PD (range: −45 to 20 PD), respectively (Table 3). Eight patients were fully orthotropic, while another eight presented with ASC.
Analysis of deviation values at near and far distance and worth four dot test values across all subgroups and follow-up visits.
p: Mann-Whitney U test comparing subgroups; p* Wilcoxon rank sum test comparing this visit with initial visit; p** Wilcoxon rank sum test comparing this visit with post-visual therapy visit.
Abbreviations: n, sample size; Rx, refraction in spherical equivalent; ASC, anomalous sensorial correspondence; NSC, normal sensorial correspondence. The deviation strabismus measurements are in prismatic diopters (PD).
Eighteen patients demonstrated measurable stereoacuity using random dot tests, with a mean stereoacuity of 1200.00 ± 258.69 arcseconds (range: 100–1300 arcseconds). Figures 2, Tables 2 and 3, and the supplementary material provide further information on the pre- and post-treatment clinical data.
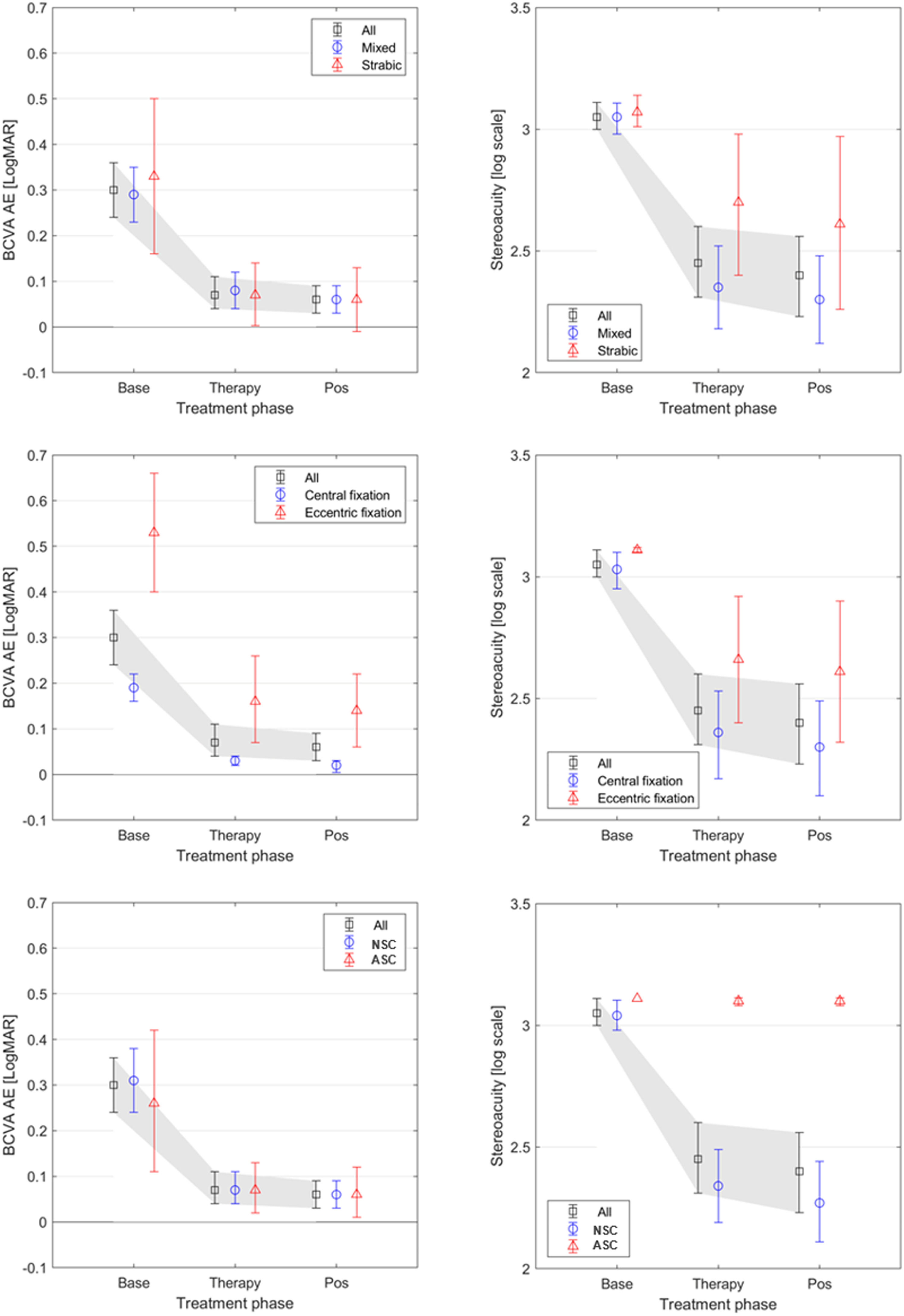
Graphical representation of BCVA values (on the left) and logarithmic stereopsis values (on the right) across different visits for different subgroups. The highest logarithmic stereopsis values are 3.11 equivalent to 1300 arc seconds, 2.50 equivalent to 600 arc seconds, and 2.00 equivalent to approximately 100 ′onds.
The combined treatment lasted 18.90 ± 5.98 weeks (range: 8.60–51.60), with an occlusion dose of 2.68 ± 1.52 h/day (range: 2.00–6.00) and an average compliance rate of 74 % ± 15 % (confidence interval: 68 %–79 %).
Twenty-six participants underwent monocular training using Gabor patches, with 17 having eccentric fixation and eight with ASC. The remaining participants performed training with dichoptic Gabor patches. The vergence therapy and direct stereoacuity stimulation phase were completed by 43 patients (81 %).
General resultsThe mean BCVA of the amblyopic eye improved significantly, from 0.30 ± 0.23 logMAR at baseline to 0.08 ± 0.11 logMAR post-treatment (p < 0.01). Forty-six patients (87 %) achieved a BCVA equal to or better than 0.01 logMAR, indicating successful treatment.
At baseline, 35 patients (66 %) demonstrated no measurable stereoacuity. Following treatment, only seven patients exhibited null stereoacuity, while 34 of 53 patients (64 %) improved their stereoacuity by at least two levels (successful treatment).
The Worth Four Dot test revealed that, prior to treatment, only one patient could fuse at two target sizes (visual angles of 1.5° and 5.0°). Post-treatment, 39 patients demonstrated fusion. Regarding strabismus deviation, near deviation improved from −2.20 ± 7.80 PD at baseline to −0.50 ± 4.20 PD post-treatment (p < 0.05), and distance deviation improved from −2.00 ± 6.50 PD to −0.30 ± 4.00 PD (p < 0.05).
Results by sensorial correspondenceComparative analysis based on sensorial correspondence (NSC vs. ASC) showed significant BCVA improvement in both subgroups, with no significant differences between them. However, significant differences were observed in the angle of deviation at both near and far distances (p < 0.01).
Regarding binocular vision, four patients (50 %) in the ASC group achieved fusion for both target sizes on the Worth Four Dot test and coarse stereoacuity (1200 arc seconds). The NSC group, however, demonstrated better overall fusion and stereoacuity (p < 0.01). Thirty-four of 45 patients (75 %) improved by at least two levels (successful treatment).
Results by fixation typeWhen stratified by fixation type (central vs. eccentric), the patients with central fixation showed significantly better improvement in BCVA (p < 0.01). Eleven of seventeen patients (65 %) achieved central fixation. Nine of seventeen patients (53 %) achieved a BCVA equal to or better than 0.01 logMAR. However, the lowest final BCVA was recorded for the eccentric fixation subgroup. Regardless of binocular vision, in both groups the changes in stereoacuity and fusion capacity were significant (p < 0.01). Among those with eccentric fixation, eight of seventeen (47 %) achieved fusion at both sizes and improved their stereoacuity by two steps from its initial level. The deviation angle improved significantly at both distances.
Results by amblyopia typeComparing amblyopia types (combined mechanism vs. strabismic amblyopia), BCVA improved significantly in both subgroups without significant differences. However, patients with combined-mechanism amblyopia demonstrated significantly greater reductions in near deviation compared to those with strabismic amblyopia (p = 0.03).
Binocular vision outcomes showed no significant differences in the Worth Four Dot test response. Nonetheless, stereoacuity was significantly better in patients with combined-mechanism amblyopia compared to those with strabismic amblyopia (p = 0.03).
StabilityAt the six-month follow-up, the angle of deviation and Worth Four Dot test results remained stable. The BCVA of the amblyopic eye showed statistically significant improvement (p < 0.04) across all subgroups except ASC (p = 0.29) and eccentric fixation (p = 0.59).
Stereoacuity improved significantly across the entire sample, from 539.62 ± 518.69 arcseconds at baseline to 523.77 ± 519.25 arcseconds (p < 0.01). Notably, the NSC subgroup also showed significant improvement (p = 0.01), as illustrated in Figure 2 and Table 1 of the supplementary material.
DiscussionIn the present study, the authors describe an active therapy protocol in cases where occlusion treatment alone has failed to achieve normal visual acuity. However, due to the pre- post study design without a control or placebo group, these findings do not establish the efficacy of the treatment.
Forty-six (87 %) participants achieved a BCVA of logMAR 0.1 or better and the stereoacuity was achieved in 43 participants (81 %). Furthermore, the results were stable six months later in a population highly susceptible to recurrence.2 The deviation angle, fixation status, and binocular vision remained stable. However, BCVA improved significantly without any maintenance treatment. The absence of suppression in the sample (74 % exhibited fusion at both sizes) could explain this improvement.
An important factor to consider is treatment adherence, which was 74 % in this study, indicating good compliance with the prescribed home-based therapy. Previous systematic reviews have highlighted the critical role of adherence in amblyopia treatment outcomes.33,34 Higher compliance rates are associated with better visual improvements, whereas poor adherence can significantly limit treatment efficacy.
The present study reports result comparable to those obtained by Hernández-Rodríguez CJ et al.25 using the same home-based computer program. Compliance, visual acuity, and stereoacuity outcomes were similar. However, a significant difference lies in the sample composition: while most participants in the previous study were anisometropic, the sample in the present study exclusively consisted of patients with strabismus.
The sample was divided in three categories: depend on the fixation (central or eccentric foveal fixation); the sensorial correspondence (anormal or normal) and the amblyogenic mechanism (strabismus or strabismus plus anisometropia) (Table 2 and 3 and supplementary material).
In participants belong to eccentric fixation subgroup, the 65 % of them achieved central fixation, however they got the lowest final BCVA recorded, although the improvement over the initial BCVA was statistically significant (p < 0.01) for this subgroup.
The influence of foveal fixation in amblyopia treatment has yet to be studied in depth. A recent study (Mehmed B et al., 2022)35 of amblyopic patients with eccentric fixation over a twelve-month period of occlusion treatment found that the efficacy of the occlusion decreased with age. Despite some improvement in patients under eight years, older patients showed significantly lower treatment efficacy. Although the sample size was small, we assessed the effect of age within this group (eccentric fixation) by dividing the sample into two subgroups: one consisting of amblyopic patients older than 8 years (n = 5) and the other comprising patients younger than 8 years (n = 12). Pre- and post-treatment visual acuity measurements were compared to determine whether the improvement was statistically significant using the Wilcoxon test. In subjects older than 8 years, changes in BCVA were not significant (p = 0.68), whereas in subjects younger than 8 years, changes in BCVA were statistically significant (p = 0.02).
In addition, no changes in BCVA were observed beyond the six-month stage. In the sample observed for the present study, the mean age was 8.47±8.31 years, with previous long-term treatment that had proved unsuccessful. It is possible, therefore, that patients with eccentric fixation tend to respond less positively than patients with adequate foveal fixation, as the present results show. However, the diagnosis of eccentric fixation was determined using the visuscope, a subjective method for assessing fixation. It is possible that some subjects diagnosed with eccentric fixation may have exhibited unstable fixation. To obtain more accurate measurements, it would be valuable to analyze fixation using objective methods, such as microperimetry,36 in future studies.
In addition to allowing for the nature of the fixation, the incorporation of a number of clinical methods recommended by other authors should be highlighted.37 Firstly, only patients who were able to achieve fusion with the synoptophore at their target angle underwent dichoptic therapy, to determine whether their binocular circuits were intact and avoid potential intractable diplopia. Secondly, the degree of suppression was assessed with a new version of the Four Worth dot test that determines suppression and fusion capacity in peripheral (5°) and central (1.5º) vision. This allows binocular vision to be clinically monitored throughout the treatment. Finally, stereoacuity outside the Panum area was measured with the first slides of the TNO test, allowing the presence of stereoacuity to be measured in subjects who recorded null stereoacuity with other tests, for example, the Random Dot Preschool Stereoacuity test.
The changes in the angle of deviation varied across subgroups, reflecting differing responses to treatment. Patients with NSC exhibited significantly greater reductions in angle deviation compared to those with ASC. This suggests that intact binocular sensory mechanisms in NSC patients enhance motor alignment outcomes. Similarly, patients with central fixation achieved greater alignment improvements than those with eccentric fixation. Furthermore, combined mechanism amblyopia was associated with greater reductions in near deviation compared to strabismic amblyopia.
Among subjects with NRC, the greatest reduction in angle deviation was observed, which explains their greater improvement in stereoacuity. For stereoacuity to be achieved, the images received by both eyes must fall in Panum’s fusional area with a fixation disparity between 0.6 and 0.1 PD.32
In the present study, a Worth Four Dot test indicated that patients in the ASC and eccentric subgroups improved their binocular vision with fusion and achieved near coarse stereoacuity. The post-treatment stereoacuity measurements in the ASC group (mean: 1250.00 ± 53.45 arcseconds) and the eccentric group (mean: 718.95 ± 508.95 arc seconds) indicate the persistent presence of microtropia or monofixation syndrome. Nevertheless, some degree of binocular collaboration remained achievable.38,39 Although a robust body of literature links stereopsis deficiency and difficulties with fine motor skill difficulties,40 the relationship between stereoacuity and motor skills is not linear, with a complete absence of stereoacuity having a much greater impact, suggesting that the presence of some stereoacuity is better than none at all.41
Several studies have compared BCVA results with respect to occlusion times (two versus six hours of occlusion of the dominant eye) in patients with residual amblyopia,42 finding a difference of 0.6 lines of visual acuity in 30 to 35 % of the patients studied. In addition, Buckle et al.7 determined that occlusion beyond the “plateau” in visual acuity improvement was not clinically relevant: although the patients in this study, having reached the plateau, continued to receive an occlusion dose, the increased duration of the occlusion did not appear to be advantageous.5 Since contemporary research indicates that dichoptic therapy is no more effective than occlusion when both strategies are implemented in isolation.9,21 The authors of the present study recommend active visual therapy as an adjuvant to occlusion. It should be noted that, for the patients in our sample – who presented with strabismic amblyopia resistant to occlusion – the combination of occlusion and active therapy achieved better results than those of occlusion in isolation, with a progressive reduction of the occlusion dose [10.26±3.16 hours (0.00 to 12.00) versus 2.68±1.52 hours (2.00 to 6.00)] each day.
The protocol proposed in this study consists of three different phases:
Monocular trainingGabor patches has shown efficacy in the treatment of amblyopia.43,44 Additionally, Gabor patches has been proposed as an adjunct to occlusion therapy.44 Gamified Gabor patches therapy may enhance engagement and compliance, addressing challenges noted in earlier studied.25
Vergence trainingIn previous studies, monocular and dichoptic therapy did not significantly reduce angle deviation.12,16,19,22 The proposed treatment reduces angle deviation by enabling compensation through fusional vergences. In earlier research, dichoptic therapy showed improvements in suppression scotoma rupture and simultaneous vision capability,45,46 but did not enhance stereoacuity.11–13,16,19,43,44 Correcting strabismus deviation with prisms enhances disparity receptor function by aligning foveal images within Panum's area, as demonstrated in previous studies on esotropia.24,47 Surgery is recommended for deviations >12 PD; in this study, one patient (45 PD esotropia) underwent surgery and achieved 200 arcseconds of stereoacuity, consistent with prior findings.24 For deviations ≤12 PD, vergence therapy progressively reduces the amount of prism needed to compensate for the strabismus until orthotropia is achieved.24
Direct stereoacuity stimulationPatients who achieved orthotropia without prism correction underwent gamified stereoacuity training using random dot stimuli with progressive demand. Recent studies have shown that, in patients with a history of strabismic amblyopia, direct stimulation of stereoacuity improves stereoacuity.20,32 Unlike passive therapies, which yield poor stereoacuity outcomes,20 or dichoptic stimuli, which provide only limited improvements,11–13,16,19,43,44 this protocol resulted in significant gains in stereoacuity.
Study limitationsThe main limitations of this study are its retrospective design and the absence of a control or placebo group. Without a control group, it is not possible to determine whether the observed improvements are attributable to the treatment itself or to other factors, such as improved adherence to occlusion therapy. While including a control group of patients undergoing prolonged occlusion therapy may raise ethical concerns, other studies have incorporated placebo treatments to address this limitation.33,34 Future prospective studies with appropriate control groups are necessary to accurately assess the effectiveness of each phase of this protocol.
In conclusion, gamified visual therapy software, used as an adjuvant to occlusion treatment, improved BCVA and stereoacuity in patients with persistent strabismic and combined-mechanism amblyopia. This improvement was observed across all subgroups, including those with ASC or eccentric fixation, for whom passive therapy had failed to achieve normal visual acuity. However, given the lack of a control group, these findings should be interpreted as preliminary observations rather than definitive evidence of treatment efficacy. Further research, including randomized controlled trials, is necessary to confirm these results.
Author contributions statementJP collected the data from his own records, SM documented the protocol, and IP statistically analyzed the results. Apart from this, all authors contribute to the writing of the manuscript.
In 2015 SM and JP promoted, with the support of the University of Oviedo, the creation of the startup VisionaryTool (www.visionarytool.com). VisionaryTool has not had any role (writing, analysis, or control over publication) in the production of the paper.
This research has not received any funding. JP works on his own clinic, whereas SM and IP are lecturers at University of Oviedo and University of Valladolid.