This study aimed to determine the changes in binocular vision (BV) and accommodation in Malay myopic children following long-term wear of Defocus Incorporated Multiple Segments (DIMS) spectacle lenses for 24 months.
MethodsTwenty-three Malay myopic children aged 7–12 years were enrolled in this prospective, self-controlled study. DIMS spectacle lenses were prescribed, and analyses were conducted at baseline, 12, and 24 months. Assessments included stereopsis, near point of convergence (NPC), phoria, positive/negative fusional vergence (PFV/NFV), amplitude of accommodation (AA), accommodative lag, positive/negative relative accommodation (PRA/NRA), and accommodative convergence to accommodation (AC/A) ratio. Visual acuity (VA), cycloplegic refraction (SER) and axial length (AL) were monitored. Data were analyzed using repeated-measures analysis of variance (ANOVA) within-subject or the Friedman test, with Bonferroni correction applied. p < 0.05 was considered statistically significant.
ResultsStatistically significant changes were observed after 24 months, including median changes in NPC (receded by 2 cm, p < 0.001), AA (reduced by 1.67D, p = 0.002), distance PFV break (increased by 8Δ, p = 0.026) and recovery (increased by 6Δ, p = 0.033), distance NFV break (no change, p = 0.043), stereopsis (improved by 10″, p < 0.001), accommodative lag (reduced by 0.25D, p = 0.002), and AC/A ratio (increased by 1Δ/D, p < 0.001). Additionally, distance and near VA improved (p < 0.001), while SER and AL increased (p < 0.001).
Conclusion: Wearing DIMS spectacle lenses for 24 months resulted in changes in BV and accommodation while slowing myopia progression. Regular NPC monitoring is recommended to maintain optimal BV function and visual comfort in children wearing DIMS lenses.
Myopia is a global public health concern, and its prevalence is steadily increasing, particularly in East and Southeast Asia.1,2 It is projected that myopia will affect 50 % of the world's population by 2050.2 Beyond solely contributing to refractive error, high myopia has been linked with an increased risk of sight-threatening conditions, which are associated with ocular morbidity and visual disability.3 These complications are not only increased in high myopia but also in low and moderate myopia.4 The mechanisms underlying myopia progression involve hyperopic defocus caused by a high accommodative lag during near work, which accelerates axial length (AL) elongation.5 Furthermore, ciliary-choroidal tension restricts equatorial expansion of the eye, promoting AL elongation and resulting in the more prolate shape of the myopic eye.6
In recent years, various designs of myopia control spectacle lenses have emerged, providing a safe and comfortable option for children while effectively slowing myopia progression.7 Defocus incorporated multiple segments (DIMS) lenses aim to induce peripheral myopic defocus while simultaneously maintaining clear vision. These lenses are designed with a 9 mm diameter central zone to correct the distance correction and are surrounded by 33 mm concentric multiple small segments (lenslets) in the mid-peripheral zone. Each lenslet provides an addition power of +3.50 Diopters (D) to induce myopic defocus in the mid-peripheral retina.8 DIMS spectacle lenses have been reported to reduce AL elongation by 62 % and myopia progression by 52 % among the Chinese population compared to children wearing single-vision spectacle (SVS) lenses over two years,8 with sustained myopia control effects over six years.9 Recently, Syed Mohd Dardin et al.10 reported that DIMS spectacle lenses effectively controlled myopia progression compared to SVS lenses over one year among the Malay population, reducing AL elongation by 65 % and myopia progression by 63.6 %.
A complex relationship exists between binocular vision (BV) function and myopia progression. The accuracy of BV and accommodation plays a crucial role, with factors such as near work and retinal blur potentially driving AL elongation.11 Research on optical myopia control interventions has shown that wearing such lenses can induce changes in BV function.12–14 After a year of wearing orthokeratology lenses, myopic children experience exophoric shifts at both distance and near, accompanied by improvements in accommodative function and stereopsis. However, a reduction in the fusional vergence range has also been observed during this period.13 Alteration of BV and accommodation measures may lead to BV dysfunction, significantly impacting childhood academic performance.15
Myopic children commonly exhibit high accommodative lag, a high accommodative convergence to accommodation (AC/A) ratio, and near esophoria.16 Additionally, positive relative accommodation (PRA) is lower in myopes compared to emmetropes.17 The dual power features of DIMS lenses could potentially interfere with BV and accommodation, as myopic children might under-accommodate when viewing through the lenslets.11 The long-term effects of wearing DIMS spectacle lenses on BV and accommodation remain unclear, as limited studies have explored this factor. Research has shown that BV dysfunction influences myopia progression in children wearing DIMS spectacle lenses. After one year of lens wear, children with divergence excess exhibited the most effective myopia control, while those with convergence excess experienced the greatest myopia progression.18 Lam et al.9 reported that post-wear visual function after six years of wearing DIMS spectacle lenses showed no adverse effects. Another study found no significant differences in visual function between the DIMS and SVS lenses.19 However, the interaction and changes between all measures of BV and accommodation have not been thoroughly investigated. This study aimed to investigate changes in BV and accommodation after 24 months of wearing DIMS spectacle lenses among Malay primary schoolchildren. The findings contribute to our understanding of the effectiveness of DIMS spectacle lenses and their impact on BV function, which aids in myopia control.
MethodsThis prospective, self-controlled study was conducted from August 2021 to August 2024 at the Optometry Clinic, Faculty of Health Sciences, Universiti Kebangsaan Malaysia, Kuala Lumpur Campus. It is part of the Myopia Control Study in Kuala Lumpur (MyCOSKL), which was designed to evaluate changes in BV and accommodation with DIMS spectacle lenses.20 This 24-month follow-up study invited 24 myopic children who had completed the initial 12-month study. Measurement of BV, accommodation, cycloplegic refraction, AL, and visual acuity (VA) were repeated at baseline, 12, and 24 months. Previous myopia progression status was not quantified nor considered a criterion for study participation. Based on previous studies on test repeatability, a clinically significant change was defined as >2PD for mean phoria21 and fusional vergence ranges,22 while >0.50 D for mean accommodative response.23 Sample size calculation was performed using G*Power software (version 3.1.9.4). A repeated-measures ANOVA (within-subject factors) with an alpha level of 0.05 determined that a minimum of 11 subjects was required to achieve 90 % power to detect a 0.50D difference in accommodation measurements. For vergence measurements, a minimum of 3 subjects was required to achieve 90 % power to detect a 2PD difference. As the accommodation calculation required a larger sample size, we used this value and accounted for a 20 % dropout rate, resulting in a final requirement of at least 13 subjects for this study. This study adhered to the principles of the Declaration of Helsinki and was approved by The Research Ethics Committee of the Universiti Kebangsaan Malaysia (UKM PPI/111/8/JEP-2020–667 and UKM PPI/111/8/JEP-2024–209). All subjects and their parents were informed about the study and signed the informed consent forms before the study commenced.
The inclusion criteria included Malay children aged between 7 and 12 years old, with spherical equivalent refraction (SER) ranging from −0.50 D to −5.00 D, astigmatism and anisometropia <1.50 D, and monocular best-corrected VA of 6/6 or better. Before enrolment, none of the children had received myopia control treatment, and they were free from any ocular or systemic abnormalities or BV issues. All subjects underwent cycloplegic refraction, and DIMS spectacle lenses were prescribed. They were instructed to wear the spectacles throughout waking hours, except while showering. The lenses were replaced with a new pair at any visit if the change in SER was >0.50 D All assessments were conducted with subjects wearing the DIMS spectacle lenses during the procedures. Participation in the study was voluntary, and the DIMS spectacle lenses were prescribed for free.
Visual acuityDistance and near visual acuity (VA) were measured using the LogMAR ETDRS charts (Precision Vision Inc., Woodstock, IL, USA). The distance chart was positioned on an illuminated cabinet at 4 m, and the near chart at 40 cm. The subject was encouraged to read the smallest line they could see, until four or more consecutive letters were misread. Each letter had a value of 0.02 log of the minimal angle of resolution (logMAR).24
Binocular vision and accommodationAccommodative response (AR) was measured using an open-field autorefractor (Shin-Nippon NVision-WAM 5500; Ajinomoto Trading Inc., Tokyo, Japan) while the subjects viewed a 6/9 letter target binocularly at 40 cm. Accommodative lag was calculated as the difference between the measured AR and the actual accommodative stimulus (2.50 D).20 Stereopsis was assessed using the Frisby stereotest (Clement Clarke International Ltd., Haag Streit UK Ltd., Harlow, Essex). The test does not require special glasses and it consists of three transparent plates of different thickness to create “real depth”. Subjects identify the square where a circular target appears to “pop out” from the background, with results recorded in seconds of arc (“).25
The Royal Air Force (RAF) rule was used to measure NPC and AA subjectively. For Near point of convergence (NPC), subjects focused on a small circle target while the examiner slowly moved it toward their nose.26 Three NPC measurements (in cm) were taken, and the average was recorded when subjects reported diplopia or when the examiner observed eye deviation. Amplitude of accommodation (AA) was measured monocularly and binocularly using the push-up method, where subjects kept an N5 word target clear as the examiner gradually moved the RAF rule closer.27 Three measurements were taken, and the average AA was recorded in diopters (D) when the subjects first reported sustained blur.
Horizontal distance and near phoria were measured objectively using alternate cover test. Distance phoria was assessed at 6 m while near phoria at 40 cm using a 0.2 logMAR fixation target. The eyes were alternately covered and eye movements were observed. The prism diopters (PD) needed to neutralize the eye movement using the prism bar were recorded as the phoria measurement.27 Then, +2.00 D lens was added to both eyes, and the alternate cover test was repeated. The AC/A ratio was calculated using the gradient method, based on the difference between the near phoria and near phoria with the +2.00 D lens, with exophoria values being negative and esophoria positive. Fusional vergences were measured with the prism bar in free space, using a base-out prism to assess positive fusional vergence (PFV), and a base-in prism for negative fusional vergence (NFV). The prism bar was gradually increased, and subjects identified the “break point” where they could no longer see a single image and the “recovery point“ where single vision returned. Measurements were taken while viewing a 0.2 logMAR target at 6 m and 40 cm, first at distance and then near.27 NFV was measured before PFV to prevent prism adaptation.28 “Blur point” measurements were not taken due to the young age of the subjects, as their results may not be reliable.29 The unequal prism bar measures 1, 2, 4–20PD in 2PD increments, while 25–40PD increases in 5PD increments. Therefore, although changes beyond 20PD are small, they are still recorded as 5PD increments. The procedure was repeated three times, and the average measurements were recorded in PD.
Negative relative accommodation (NRA) was assessed by gradually adding plus lenses in 0.25 D increments binocularly until the subject reported sustained blur while viewing a 0.2 logMAR target at 40 cm. The total amount of plus lenses added was recorded. Positive relative accommodation (PRA) was tested the same way, but with minus lenses, and the total minus lenses added were recorded. NRA was tested before PRA to prevent any influence on accommodation.27
Refractive and ocular biometryBefore cycloplegic refraction, two drops of 1 % cyclopentolate were administered 5 min apart. After a 30-minute interval, cycloplegic autorefraction was performed using the Shin-Nippon NVision-WAM 5500 open-field autorefractor (Ajinomoto Trading Inc., Tokyo, Japan), followed by subjective refraction to determine the refractive correction. The spherical equivalent refraction (SER) was calculated based on a sphere and a half-cylinder. Axial length (AL) was measured using the Lenstar LS900 (Haag-Streit AG, Switzerland), averaging five measurements for each eye.
Statistical analysisSPSS (IBM, Version 29.0.2.0, Armonk, NY, USA) was used for statistical analysis. The monocular data for the two eyes showed no statistically significant differences (p > 0.05) and were highly correlated with the SER (r = 0.939, p < 0.001) and AL (r = 0.981, p < 0.001). Therefore, only data from the right eye were used for the statistical analysis. Data normality was assessed using the Shapiro-Wilk test. For normally distributed data, repeated measures analysis of variance (RM-ANOVA) was used to analyze differences over time, with post hoc pairwise comparisons conducted using the Bonferroni correction. For non-normally distributed data, the Friedman test was applied, and pairwise comparisons were performed using the Wilcoxon signed-rank test with Bonferroni correction. A p-value of <0.05 was considered statistically significant, while a Bonferroni-adjusted p < 0.025 was applied for multiple comparisons.
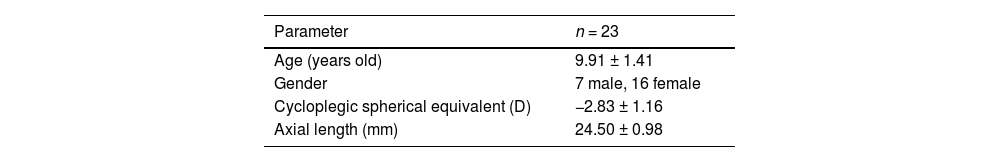
ResultsBaseline demographic dataBaseline demographics are described in Table 1. Of the 24 subjects prescribed DIMS spectacle lenses (age range: 7–12 years old), one was excluded from the analysis due to unusual increases in SE and AL elongation (annual rate of SE: −1.31 D/year and AL: 0.56 mm/year), and was referred to an ophthalmologist. The mean age of the 23 subjects who completed the study was 9.91 ± 1.41 years.
Baseline demographic data who completed the 24 months of wearing DIMS spectacle lenses.
| Parameter | n = 23 |
|---|---|
| Age (years old) | 9.91 ± 1.41 |
| Gender | 7 male, 16 female |
| Cycloplegic spherical equivalent (D) | −2.83 ± 1.16 |
| Axial length (mm) | 24.50 ± 0.98 |
Parameters are given as mean± standard deviations (SD).
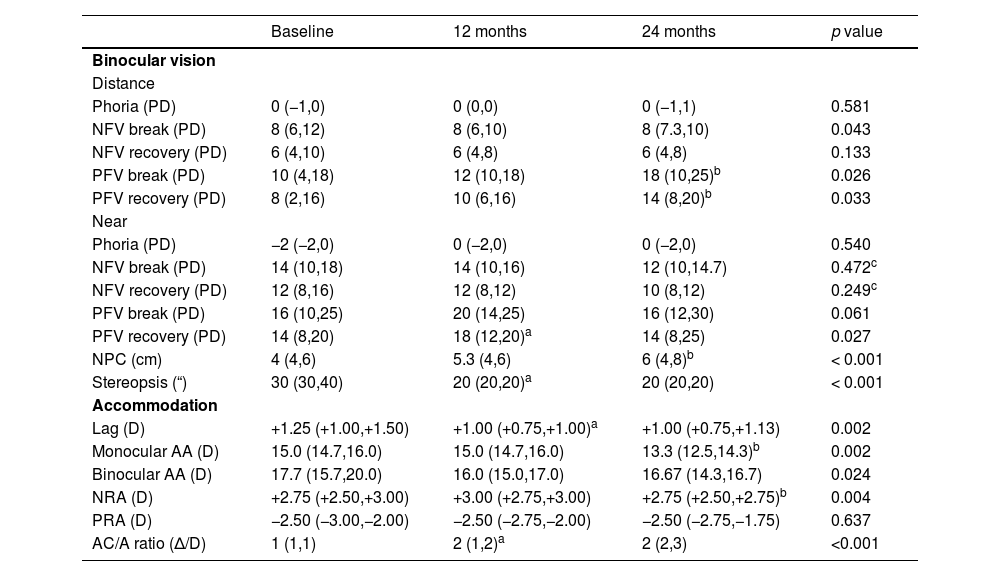
Table 2 showed the changes in BV and accommodation over 24 months. No significant differences were observed in distance (p = 0.581) and near (p = 0.540) phoria over time. Distance NFV break showed significant changes (W = 0.14, χ22=6.28, p = 0.043), but no significant differences between visits. No significant changes were found in distance NFV recovery (p = 0.133). Distance PFV showed significant changes in both break (W = 0.16, χ22 = 7.27, p = 0.026) and recovery (W = 0.15, χ22 = 6.85, p = 0.033), with a significant increase observed between 12 and 24 months for distance PFV break (Z = −2.84, p = 0.004) and recovery (Z = −2.62, p = 0.009). No significant changes were found in near NFV for both break (p = 0.472) and recovery (p = 0.249). Near PFV break showed no significant changes (p = 0.061), while near PFV recovery exhibited significant changes (W = 0.16, χ22 = 7.26, p = 0.027), with a significant increase observed between baseline and 12 months (Z = −2.28, p = 0.022). NPC significantly receded over time (W = 0.33, χ22 = 14.98, p < 0.001), with a significant recession observed between 12 and 24 months (Z = −2.55, p = 0.011). Additionally, stereopsis changed over time (W = 0.57, χ22 = 26.32, p < 0.001), with significant improvement observed between baseline and 12 months (Z = −3.84, p < 0.001).
Binocular vision and accommodation over 24 months wearing DIMS spectacle lenses (n = 23).
| Baseline | 12 months | 24 months | p value | |
|---|---|---|---|---|
| Binocular vision | ||||
| Distance | ||||
| Phoria (PD) | 0 (−1,0) | 0 (0,0) | 0 (−1,1) | 0.581 |
| NFV break (PD) | 8 (6,12) | 8 (6,10) | 8 (7.3,10) | 0.043 |
| NFV recovery (PD) | 6 (4,10) | 6 (4,8) | 6 (4,8) | 0.133 |
| PFV break (PD) | 10 (4,18) | 12 (10,18) | 18 (10,25)b | 0.026 |
| PFV recovery (PD) | 8 (2,16) | 10 (6,16) | 14 (8,20)b | 0.033 |
| Near | ||||
| Phoria (PD) | −2 (−2,0) | 0 (−2,0) | 0 (−2,0) | 0.540 |
| NFV break (PD) | 14 (10,18) | 14 (10,16) | 12 (10,14.7) | 0.472c |
| NFV recovery (PD) | 12 (8,16) | 12 (8,12) | 10 (8,12) | 0.249c |
| PFV break (PD) | 16 (10,25) | 20 (14,25) | 16 (12,30) | 0.061 |
| PFV recovery (PD) | 14 (8,20) | 18 (12,20)a | 14 (8,25) | 0.027 |
| NPC (cm) | 4 (4,6) | 5.3 (4,6) | 6 (4,8)b | < 0.001 |
| Stereopsis (“) | 30 (30,40) | 20 (20,20)a | 20 (20,20) | < 0.001 |
| Accommodation | ||||
| Lag (D) | +1.25 (+1.00,+1.50) | +1.00 (+0.75,+1.00)a | +1.00 (+0.75,+1.13) | 0.002 |
| Monocular AA (D) | 15.0 (14.7,16.0) | 15.0 (14.7,16.0) | 13.3 (12.5,14.3)b | 0.002 |
| Binocular AA (D) | 17.7 (15.7,20.0) | 16.0 (15.0,17.0) | 16.67 (14.3,16.7) | 0.024 |
| NRA (D) | +2.75 (+2.50,+3.00) | +3.00 (+2.75,+3.00) | +2.75 (+2.50,+2.75)b | 0.004 |
| PRA (D) | −2.50 (−3.00,−2.00) | −2.50 (−2.75,−2.00) | −2.50 (−2.75,−1.75) | 0.637 |
| AC/A ratio (Δ/D) | 1 (1,1) | 2 (1,2)a | 2 (2,3) | <0.001 |
All data presented as median (IQR).
NFV, negative fusional vergence; PFV, positive fusional vergence; NPC, near point of convergence, AA, amplitude of accommodation; NRA, negative relative accommodation; PRA, positive relative accommodation; AC/A, accommodative convergence to accommodation.
All examined accommodation measures showed changes except for PRA. Accommodative lag decreased over time (W = 0.27, χ22 = 12.02, p = 0.002), with a statistically significant difference in the first 12 months (Z = −3.13, p = 0.002). Both monocular and binocular AA significantly reduced over time: monocular (W = 0.26, χ22 = 12.02, p = 0.002) and binocular (W = 0.16, χ22 = 7.47, p = 0.024). Monocular AA showed a statistically significant reduction between 12 and 24 months (Z = −3.23, p = 0.001), while binocular AA showed no significant differences between visits. NRA changed significantly (W = 0.24, χ22 = 11.03, p = 0.004), with a significant reduction between 12 and 24 months (Z = −3.04, p = 0.002). PRA did not change over time (p = 0.637). The gradient AC/A ratio revealed a significant increase (W = 0.30, χ22 = 13.87, p < 0.001), with a statistically significant increase in the first 12 months (Z = −2.28, p = 0.023) (Table 2).
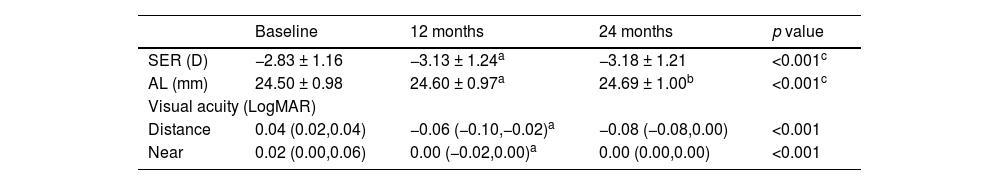
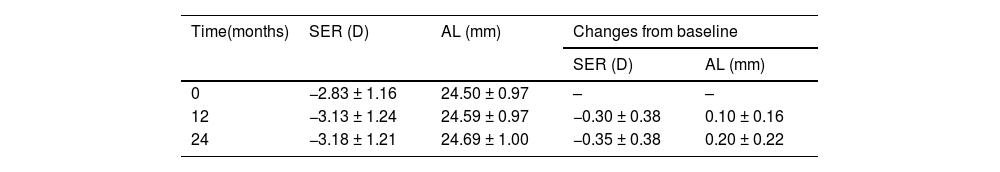
Changes in myopia progressionComparing the data from the three visits, significant changes were observed in SER (F2,44=11.82, p < 0.001) and AL (F1.1,23.9 = 16.92, p < 0.001) over time (Table 3). SER increased significantly during the first 12 months (p = 0.003), with no further significant changes by 24 months. AL exhibited a statistically significant increase between baseline and 12 months (p = 0.024) and between 12 and 24 months (p < 0.001). Over 24 months, SER changes was −0.35 ± 0.38 D and AL elongation was 0.20 ± 0.22 mm (Table 4).
Myopia progression and visual acuity over 24 months wearing DIMS spectacle lenses (n = 23).
| Baseline | 12 months | 24 months | p value | |
|---|---|---|---|---|
| SER (D) | −2.83 ± 1.16 | −3.13 ± 1.24a | −3.18 ± 1.21 | <0.001c |
| AL (mm) | 24.50 ± 0.98 | 24.60 ± 0.97a | 24.69 ± 1.00b | <0.001c |
| Visual acuity (LogMAR) | ||||
| Distance | 0.04 (0.02,0.04) | −0.06 (−0.10,−0.02)a | −0.08 (−0.08,0.00) | <0.001 |
| Near | 0.02 (0.00,0.06) | 0.00 (−0.02,0.00)a | 0.00 (0.00,0.00) | <0.001 |
SER, spherical equivalent; AL, axial length.
Mean and cumulative changes in the cycloplegic SER and AL from baseline to 24 months (n = 23).
Parameters are given as mean ± SD.
SER, spherical equivalent; AL, axial length.
Significant changes in both distance and near VA were observed over time, with distance VA (χ22=27.0, p < 0.001) and near (χ22=18.90, p < 0.001) showing improvement (Table 3). An improvement occurred between baseline and 12 months for both distance (Z=−4.03, p < 0.001) and near (Z=−2.95, p = 0.003) VA.
DiscussionThis study aimed to determine changes in BV and accommodation following long-term wear of DIMS spectacle lenses. Results showed that wearing DIMS spectacle lenses for 24 months led to several changes in BV and accommodation, including receded NPC, reduced AA, increased in distance PFV (break and recovery), distance NFV (break), and near PFV (recovery), and improvement in accommodative lag, NRA, stereopsis, and AC/A ratio. A study by Lam et al.9 concluded that long-term wear of DIMS spectacle lenses did not negatively affect visual functions over six years; VA, phoria, stereopsis, and AA. However, their study only assessed visual function at the last visit. Thus, the underlying mechanisms of changes in BV function with DIMS spectacle lenses remain unclear. Another two-year study by Lam et al.19 reported similar changes in accommodative lag, monocular and binocular AA, and stereopsis in children using DIMS and SVS lenses. In their study, single-vision correction was placed on a trial frame during measurements to avoid the effects of the DIMS lens. In contrast, this study evaluated the DIMS lens effect by having subjects wear the lenses as they would during their daily activities.
Menjivar et al.30 identified the NPC break as a reliable measure for detecting convergence insufficiency (CI), with a break of 6 cm or greater indicating general CI and 7.5 cm or greater indicating symptomatic CI. In this study, NPC receded by 2 cm over time, exceeding the clinically significant threshold of >1 cm based on test repeatability studies.31 This recession highlights the importance of annual NPC monitoring in children wearing DIMS spectacle lenses to support sustained BV function and visual comfort over long-term wear.
The results of this study also demonstrated that stereopsis improved after 12 months and remained stable, consistent with previous findings from studies comparing DIMS with SVS lenses.8,19 However, these changes were not clinically significant. There were no significant changes in distance and near phoria, indicating that DIMS spectacle lenses provided stable binocular alignment, as observed in another 24-month study.19 Unlike a longitudinal study on myopic children without myopia control intervention, which reported a near exophoric shift,29 our findings demonstrate stability in both distance and near phoria over 24 months.
In this study, we observed an increase in distance PFV for both break and recovery. Clinically, this suggests an improvement in the ability to sustain BV without diplopia and to regain fusion after diplopia. Thiagarajan et al.32 reported that PFV can improve through vergence adaptation, where the eyes adapt more effectively to sustained vergence demands, maintaining single vision without blur or diplopia. Although DIMS lenses primarily affect the peripheral retina, rapid eye movements may cause intermittent viewing through the lenslets, momentarily shifting the image to the fovea.33 Viewing through the lenslets probably induces exophoria, as the eyes tend to become more exophoric when binocularly viewing through plus lenses.34 However, vergence adaptation helps stabilize phoria by increasing PFV, effectively managing the additional visual demand imposed by DIMS lenses and supporting sustained BV over time. This mechanism may explain the observed increase in PFV in children wearing DIMS lenses, though further research is needed to confirm the underlying adaptation processes. For distance NFV break and near PFV recovery, the changes were statistically but not clinically significant, as the median remained unchanged from baseline to 24 months.
Progressive myopes often exhibit high accommodative lags that increase with demand.35 In this study, accommodative lag improved from +1.25 D at baseline to +1.00 D at 24 months, indicating a shift toward the normal range. Similarly, previous study reported a reduction in accommodative lag with comparable changes between DIMS and SVS lenses, suggesting that myopic defocus did not influence accommodative lag.19 Myopia progression cannot be solely attributed to accommodative lag, as it results from the interaction of multiple factors.36
Age-related changes in the anatomy of the accommodative apparatus can influence the reduction in AA over time.37 The decrease in monocular and binocular AA observed in this study is consistent with findings from a previous study involving 79 subjects wearing DIMS spectacle lenses for 24 months, which reported an annual reduction of 0.75 D19 Present study found an annual reduction of 0.84 D in AA, with the values remaining within the normative range.27 While NRA showed statistically significant changes, the difference was not clinically significant. PRA, which stimulates accommodation, remained stable over time. Monitoring increases in PRA is more important than NRA, as high PRA is associated with clinical signs of accommodative excess.38 This study found an increase in the AC/A ratio, indicating improved accommodation-convergence coordination in children. Typically, myopes exhibit a higher AC/A ratio that decreases as myopia stabilizes.39,40 However, in this study, the AC/A ratio started at a lower value and gradually increased toward normative ranges.
Another important observation in this study was myopia progression. The mean changes in SER and AL over 24 months of wearing DIMS spectacle lenses were −0.35 ± 0.38 D and 0.20 ± 0.22 mm, respectively. The greater changes in SER during the first year may be due to the initial prescription of DIMS spectacle lenses, with the myopia control effect gradually taking effect, while more stabilized progression was observed in the second year. Additionally, the initial enrolment was in 2021 during COVID-19 pandemic, characterized by online learning and increased screen time which may have accelerated myopia progression.41 The findings are similar to previous studies on DIMS lenses.8 After two years of wearing DIMS spectacle lenses, SER was observed to be −0.38 ± 0.06 D, with AL elongation of 0.21 ± 0.02 mm.8 Despite differences in study populations, with ours focusing on Malays in Malaysia and theirs on Chinese in Hong Kong, the effectiveness of myopia control treatments does not appear to be influenced by race.42 DIMS spectacle lenses demonstrated more favorable outcomes after two years of wear compared to other myopia control spectacle lenses.7 After two years of wearing highly aspherical and slightly aspherical lenslets spectacle, greater SER changes of −0.66 D and −1.04 D were observed, with AL elongation of 0.34 mm and 0.51 mm, respectively.43 Alongside changes in BV and accommodation, both distance and near VA improved with DIMS spectacle lenses, as observed in a previous study.19 This improvement appeared at 12 months and remained stable for 24 months. The improvement in VA is due to the higher contrast generated by the DIMS design, which provides clear central vision and better visual performance when viewing through the central zone.44
To our knowledge, this is the first study to evaluate long-term changes in BV and accommodation in children wearing DIMS spectacle lenses. While several changes were observed, only NPC recession, increased distance PFV (break and recovery), and an increased AC/A ratio were clinically significant. Given the observed NPC recession, regular monitoring is recommended to ensure visual comfort and maintain optimal BV function with long-term DIMS lens wear. Proper frame selection and precise lens centration are essential for optimizing both myopia control efficacy and BV function.
A limitation of this study is the absence of a control group, which restricts direct comparisons of the impact of DIMS spectacle lenses on BV and accommodation with other corrective treatments. However, comparisons with the normative range were used to support the results. Future studies could address this limitation by incorporating a control group, allowing for more direct comparisons and further validation of the findings.
ConclusionWearing DIMS spectacle lenses for 24 months resulted in changes in BV and accommodation while effectively slowing myopia progression in myopic children. Notable findings included NPC recession, increased distance PFV, and an increased AC/A ratio. These changes suggest potential adaptations in BV function associated with prolonged DIMS lens wear. Therefore, regular NPC monitoring is recommended to maintain optimal BV function and visual comfort in children wearing DIMS spectacle lenses.
Author contributionNur Adibah Yahaya: data collection, data analysis, writing draft of manuscript; Bariah Mohd-Ali: secure funds, project manager, data analysis and review draft of manuscript; Fatin Nur Najwa Norazman: screening of subjects, data collection and analysis; Syarifah Faiza Syed Mohd Dardin: screening of subjects, data collection and analysis; Mizhanim Mohamad Shahimin: data analysis and reviewing manuscript; Norliza Momad Fadzil: data collection and analysis.
FundingThe study was supported by grant GUP-2020–054 from Universiti Kebangsaan Malaysia.
The authors have no conflicts of interest to declare.
The authors thank the children and their families for cooperation in this study.