Many school-going children experience physical, social, and academic challenges due to uncorrected refractive errors. This study aims to uncover the prevalence of spectacle compliance, identify factors that encourage regular use, and explore the barriers that lead to non-compliance.
MethodsA retrospective exploratory study assessed compliance with free spectacles provided through the REACH project after three months of spectacles being dispensed. Unannounced visits were conducted across schools to check the compliances of the spectacles. Additional variables influencing compliance were assessed through digitized questionnaires administered. The project targeted students of grade 1–12, ranging from 6 to 18 years of age.
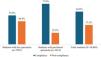
ResultsAmong the 18,205 children diagnosed with significant refractive error, most of them were myopic, 16,634 were provided with free spectacles, while the remaining children were advised to continue the same spectacles. A total of 10,469 children were present in the school, 62.8 % were compliant with spectacle use. Compliance was notably higher among students with purchased spectacles (77.8 %) compared to those provided free spectacles (55.6 %). Bivariate analysis showed that younger children (ages 6–10 years), private school students, and those with severe refractive errors (high myopia and hypermetropia) had significantly higher compliance rates (p < 0.001). Key barriers included broken lenses/frames (27.7 %), wearing spectacles occasionally (27.1 %), discomfort (10.7 %), forgetfulness (7.5 %), loss (5 %), disliking spectacles (4.1 %), teasing (2.1 %), and parental disapproval (1.7 %).
ConclusionThese findings underscore the need for durable, comfortable, and appealing spectacles, as well as targeted awareness programs for parents and students to address stigma and improve compliance, maximizing the benefits of vision correction for children’s educational and personal development.
Vision is the most powerful sense, shaping how we experience and interact with the world in every aspect of our lives. We often overlook the gift of sight, yet without it, life’s basics such as walking, reading, learning, and working become monumental challenges. Uncorrected Refractive Errors (UREs) are a major cause of avoidable blindness and vision impairment in both children and adults, worldwide and in Nepal.1–4 The prevalence of refractive error (RE) varies depending on factors such as ethnicity, geographic location, gender, age, educational level, outdoor activities, behavioral patterns, and parental education.5 It is estimated that at least 2.2 billion people globally are affected by visual impairment or blindness, with 1 billion cases being preventable or untreated, particularly in low- and middle-income countries.1 Nearly 18.9 million children under age 15 years suffer from visual impairment worldwide. The prevalence of RE is expected to rise with the increasing incidence of myopia, now considered an “epidemic” in the United States, Europe, and East Asia. Despite regional variations in RE prevalence, URE remains the leading cause of visual impairment among school-age children worldwide.6 RE has been emerged as an important cause of visual impairment and low vision.7 It is one of the most common causes of visual impairment (VI) and the second leading cause of preventable blindness.8
In developing countries, a significant portion of childhood blindness; 7 % to 31 % is avoidable, 10 % to 58 % can be treated, and 3 % to 28 % is entirely preventable.9 In developing countries like Nepal, a significant portion of childhood blindness and VI is avoidable (7 %−31 %), treatable (10 %−58 %), and preventable (3 %−28 %).10–12 Findings from the Refractive Error Study in India, children validate that RE stands as the primary cause of visual impairment in children aged 5 to 15 globally, accounting for 63 % to 77 % of cases of blindness and severe visual impairment (SVI).13
Reported prevalence rates of RE among school-going children vary across regions, with figs. from Kathmandu (8.60 %), Sunsari (19.8 %), Pokhara (6.4 %), and Jhapa (8.5 %).12,14,A study on visual impairment in schoolchildren from upper-middle socio-economic status in Kathmandu, found that 18.6 % had uncorrected visual impairment, with refractive error being the cause in 93.3 % of cases,15 while a more recent publication from Narayani Zone, Nepal reported a combined prevalence of Blindness (BL), Severe Visual Impairment (SVI), Moderate Visual Impairment (ModVI), and Mild Visual Impairment (MildVI) at 175 per 100,000.16
Unaddressed vision impairment from refractive errors profoundly affects a child’s physical, emotional, and social well-being, leading to poor academic performance and diminishing their overall quality of life, while also placing a significant burden on society.17,18 Effective strategies are essential to combat avoidable blindness in children caused by UREs. Implementing school screening programs is crucial for the early diagnosis of vision impairment and ensuring timely treatment with spectacles.19 Spectacles remain the most widely used and cost-effective method worldwide for correcting refractive errors.18,20 Common reasons for wearing spectacles include myopia, hypermetropia, astigmatism, and frequent headaches that worsen with focused tasks, especially reading. Additional indicators are difficulty in seeing clearly at certain distances, double vision, halos around lights, and the frequent need to squint.21
WHO advocates for screening children in communities and schools and encourages integrating vision screening into school health programs.22 These efforts are effective only if children wear spectacles consistently. In Nepal, the Nepal Netra Jyoti Sangh (NNJS), with support from various organizations, conducts school-based vision screening campaigns. However, most studies on spectacle-use compliance reveal that only one-third or fewer children with visual impairment due to refractive error regularly use corrective spectacles.17,23–25 Reasons for non-compliance with spectacle use vary widely across different regions and it is essential to identify these factors and implement targeted interventions to improve compliance and enhance the success of school vision screening campaigns. This study aims to uncover the prevalence of spectacle compliance, identify factors that encourage regular use, and explore the barriers that lead to non-compliance.
Materials and methods study design and settingA retrospective exploratory study was conducted on the database captured in the Refractive Error Among School going Children (REACH) project from 2018 to 2022. The project was done across five districts: Jhapa, Morang, and Sunsari in Koshi Province, and Siraha and Parsa in Madhesh Province. The project was implemented by the Nepal Netra Jyoti Sangh (NNJS)/Orbis, which involved the eye screening of students at the school level. It was initially piloted in Jhapa, Morang, and Sunsari of Koshi Province, later expanding to Siraha and Parsa in Madhesh Province. These Terai districts, where refractive error prevalence was high, previously benefited from Orbis's Comprehensive National Program for Control of Childhood Blindness (2010–2017). A total of 2738 schools were included in the initial program, and spectacles were distributed to students from these schools. Of these, 2206 (80.6 %) schools, regardless of category (public or private) or type, provided formal approval and participated in compliance assessment study. . Nepal has seven provinces, created to enhance local governance and development. The country is divided into three geographic regions: the Mountain region in the north, known as the Himalayas; the central Hill region, with a moderate climate; and the Terai region in the south, a fertile, densely populated agricultural area.
Each screening team consisted of an optometrist, an ophthalmic assistant (a three-year certificate-level course in Ophthalmic Science in Nepal), eye health workers, an optician/optical dispenser, and public health graduates. The team was trained according to the project’s clinical guidelines by subject experts from Sankara Netralaya, India, as well as pediatric ophthalmologists and senior optometrists from respective eye hospitals in Nepal. The initial training course lasted four days, followed by annual refresher training.
Furthermore, a Lead Optometrist (a senior optometrist from the hospital, not affiliated with the project team) conducted random school visits. During these visits, the Lead Optometrist selected 10 % of the children screened by the project team to verify the accuracy of examinations, prescriptions, and other procedures using a handheld refractometer. These measures helped ensure the quality of screening and provided a rationale (basis) for assessing compliance, confirming that both screening and spectacle dispensing were conducted accurately. Project conducted school vision screenings using standard clinical guidelines. Initial screening was conducted by trained ophthalmic assistants. Children who failed the initial screening were referred for detailed evaluations, including refraction, and were prescribed and provided with medicine or spectacles on-site by a team led by an optometrist. Those requiring cycloplegic refraction and more sophisticated evaluations were referred to base hospitals accompanied by their parents or teachers. Throughout this process, parents were kept informed via phone calls or messages relayed through the school authorities (Fig. 1).
Study population and sample sizeThe project targeted students from grades one through twelve, ranging from 6 to 18 years of age. For the compliance assessment, all students who had received spectacles, along with those who were already using them outside the screening program, were eligible. Among the 18,205 children diagnosed with significant refractive error (RE), 16,634 were provided with free spectacles, while the remaining children continued using their existing spectacles. By the end of the project, compliance checks were not completed in all schools due to various circumstances. In schools where compliance checks were conducted, only 10,469 students were present on the day of the compliance visit. Of these, 7055 students received spectacles through the REACH project following a detailed refraction.
Conditions for dispensing spectaclesThe students aged 6 to 18 years were considered to have significant refractive error if they could not read 0.2 Log MAR (6/9.6 Snellen’s) or could read 0.2 Log MAR (6/9.6 Snellen’s) of the pocket vision screener (PVS) card with +1.50 Diopter (D). Cycloplegic refraction was performed under the following circumstances: for children under 10 years of age, those with esotropia, hyperopia accompanied by asthenopia, a sudden shift or difference in refractive error exceeding 2 Diopter (D) from the existing prescription, fluctuating visual acuity with retinoscopy findings that did not correlate with uncorrected visual acuity, and a gross discrepancy between retinoscopy and subjective acceptance of >0.75 Diopter Spherical (DS) in myopia. Additionally, a dynamic retinoscopy lag greater than 1.00 D warranted cycloplegic refraction.
Spectacles were prescribed based on age-specific guidelines. For children under 11 years, prescriptions were given for myopia of −0.75 DS or more, hyperopia greater than +3.00 DS, and astigmatism of −1.00 diopter cylindrical (DC) or higher, regardless of axis (with the rule, against the rule, or oblique). For those aged 11 and above, myopia was treated similarly, while hyperopia was addressed if it exceeded +2.50 DS, and astigmatism prescriptions remained the same.
The above-mentioned guidelines are only applicable for those children who do not have any asthenopia symptoms, squint, or any visual discomfort specific to academic-related activities. These guidelines were meant to serve as a framework, and subjective acceptance (the power of spectacle needed, through which patient is comfortable and get adequate vision), along with correlation with clinical tests, was mandatory to finalize the prescription. The values used for the spectacles were net retinoscopy values obtained after cycloplegic refraction, with 1D deducted from the hyperopic value for cycloplegic retinoscopy.
Data collection techniquesTo evaluate compliance with spectacle use, a team of ophthalmic personnel conducted unannounced visit to each school 3 months ±1 month after the date of dispensing, carrying a digital list of children who had received free spectacles. Each participating school was visited only once for an unannounced follow-up assessment. During these visits, students' names were discreetly called, and their spectacles use was observed and recorded, ensuring that other students were unaware of the inspection. Students not wearing their spectacles at that moment, even if carrying them in pockets, head or bags, were classified as non-compliant. Additional data were collected through face-to-face interviews using a validated, digitized, semi-structured questionnaire in the local language, administered outside the classroom setting. The questionnaire gathered information on students' age, gender, school level, type of school (private/public), condition of lenses and frames, and reasons for wearing or not wearing spectacles. All responses were recorded offline in the field using the REACH Soft mobile-based scientific tool and later synced to a double cloud server when internet access was available.
Data processing and statistical analysisProject database and other information were readily available in REACH Software. Data was fetched to the SQL server and exported to Excel spreadsheets to ensure consistency and check for any missing data before carrying out the analysis. The cleaned dataset was then imported into SPSS version 22 for further analysis. Descriptive statistics, including frequencies and percentages, were calculated. To assess the association between dependent and independent variables, a chi-square test was conducted. Variables with a p-value of <0.05 at 95 % confidence interval were considered statistically significant.
ResultsCompliance to spectacles wear in childrenOut of 10,469 students, 6,577 were found wearing spectacles during an unannounced visit 3 months ±1 month after the date of dispensing, indicating an overall compliance rate of 62.8 %. However, compliance varied between groups: among students who received free spectacles under the REACH project, the compliance rate was 55.6 %. For students who had already purchased spectacles from hospitals outside the screening campaign, compliance rate was 77.8 % (Fig. 2).
Distribution of students according to compliance to spectacle wearA significant portion of the students (67.9 %) were between 11 and 15 years old, with female students making up 52 % of the participants. Most were in grades 6–8 (42.7 %), followed by grades 1–5 (29.3 %) and grades 9–12 (27.9 %). A significant portion, 81.5 %, attended private schools; primarily the students were from secondary level schools (64.2 %) and higher secondary level school (31 %), while only 1.4 % were from primary schools. Among districts, Jhapa had the largest representation with 38.8 %, while Siraha had the smallest at 7.6 %. Over three-quarters (75.8 %) of students were from Koshi Province, with the remaining 24.2 % from Madhesh Province.
The bivariate analysis of background characteristics and compliance with spectacle wear revealed significant associations with age, education level, school category, district, province and levels of refractive errors and types of refractive errors, while gender and type of school had no significant relation. Compliance was highest (60 %) in the 6–10 years age group in comparison to the other age groups, indicating association with age (p < 0.001). Gender showed no significant association, with compliance rates similar for males (55.2 %) and females (56 %) (p = 0.527). Grades of the students had significant association with compliance as students in grades 9–12 had higher compliance (58.4 %) compared to other grades (p < 0.001). Private school students had an 8.9 % higher compliance rate than government school students (p < 0.001). Morang (71 %) and Sunsari (68 %) had higher compliance rates compared to other districts (p < 0.001). Koshi Province had a 3.3 % higher compliance rate than Madhesh Province, showing a significant difference (p < 0.001) (Table 1).
Distribution of students according to compliance to spectacles wear (n = 7,055).
| Variables | Compliance | No compliance | Total | χ2 (P-value) |
|---|---|---|---|---|
| Age | 18.171(p < 0.001)* | |||
| 6–10 years | 1,023 (60.0 %) | 683 (40.0 %) | 1,706 (24.8 %) | |
| 11–15 years | 2,603 (54.4 %) | 2,187 (45.7 %) | 4,790 (67.9 %) | |
| 16–18 years | 294 (52.6 %) | 265 (47.4 %) | 559 (7.9 %) | |
| Gender | 0.399(p = 0.527) | |||
| Male | 2,026 (55.20 %) | 1,644 (44.80 %) | 3,670 (52 %) | |
| Female | 1,894 (56 %) | 1,491 (44 %) | 3,385 (48 %) | |
| Educational level | 15.466(p < 0.001)* | |||
| 1–5 class | 1172 (56.7 %) | 897 (43.4 %) | 2069 (29.3 %) | |
| 6–8 class | 1598 (53.0 %) | 1417 (47.0 %) | 3015 (42.7 %) | |
| 9–12 class | 1150 (58.4 %) | 821 (41.7 %) | 1971 (27.9 %) | |
| School category | 34.681(p < 0.001)* | |||
| Government | 629 (48.3 %) | 674 (51.7 %) | 1303 (18.5 %) | |
| Private | 3291 (57.2 %) | 2461 (42.8 %) | 5752 (81.5 %) | |
| Type of school | ||||
| Higher Secondary | 1227 (56.0 %) | 962 (44.0 %) | 2189 (31.0 %) | 0.775(p = 0.855) |
| Secondary School | 2500 (55.2 %) | 2028 (44.8 %) | 4528 (64.2 %) | |
| Basic School | 136 (56.9 %) | 103 (43.1 %) | 239 (3.4 %) | |
| Primary School | 57 (57.6 %) | 42 (42.4 %) | 99 (1.4 %) | |
| District | 382.215(p < 0.001)* | |||
| Jhapa | 1201 (43.9 %) | 1534 (56.1 %) | 2735 (38.8 %) | |
| Morang | 862 (71.0 %) | 353 (29.1 %) | 1215 (17.2 %) | |
| Sunsari | 951 (68.0 %) | 448 (32.0 %) | 1399 (19.8 %) | |
| Parsa | 592 (49.3 %) | 609 (50.7 %) | 1201 (17.0 %) | |
| Siraha | 314 (62.9 %) | 191 (37.8 %) | 505 (7.6 %) | |
| Province | 18.842 (p < 0.001)* | |||
| Koshi | 3014 (56.4 %) | 2335 (43.7 %) | 5349 (75.8 %) | |
| Madhesh | 906 (53.1 %) | 800 (46.9 %) | 1706 (24.2 %) | |
| Total | 3920 (55.6 %) | 3135 (44.4 %) | 7055 (100.0 %) |
This reduced sample size includes only those students who received spectacles following refractive error assessments conducted under the REACH project.
Among the students who were prescribed spectacles, most students exhibited low myopia in both eyes (Right eye: 80.8 %, Left eye: 80 %). Students with high or medium hypermetropia (RE: 87.5 %, 63.9 %; LE: 73.3 %, 56.7 %) and high or medium myopia (RE: 92 %, 81.2 %; LE: 96.8 %, 82.4 %) showed greater compliance than those with low myopia or hypermetropia. Spectacle wear compliance was significantly associated with severity of refractive error (p < 0.001) (Table 2).
Compliance to spectacles wear according to severity of refractive error (n = 7055).
The criteria for refractive errors were as follows: Hypermetropia: ≥+0.5D, categorized as High (>+6.0D), Medium (+3.0D to <+6.0D), and Low. Myopia: ≤−0.5D, categorized as High (>−6.0D), Medium (−3.0D to <−6.0D), and Low (−0.5D to −3.0D).
Simple myopic astigmatism was the most common condition (Right Eye (RE): 53.4 %, Left Eye (LE): 51.6 %), followed by various types of astigmatism. Compliance was higher in students with myopia (RE: 58.3 %, LE: 58.6 %), compound myopic astigmatism (RE: 63.7 %, LE: 64.3 %), and compound hyperopic astigmatism (RE: 53 %, LE: 57.6 %), indicating a significant association between refractive error type and compliance (p < 0.001) (Table 3).
Compliance to spectacles wear according to type of refractive error (n = 7,055).
The major reasons for not wearing spectacles include broken lenses or frames (27.7 %) and wearing them only on special occasions (27.1 %), followed by discomfort (10.7 %) (Table 4).
Reasons for non-compliance with spectacle use.
The enabling factors for using spectacles among students who were observed wearing them during compliance visits, as mentioned by the students, include clearer/improved vision (95.2 %), followed by relief from headaches or watering (8.0 %), Good academic performance and encouragement (4.1 %), Good looking (3.7 %), Good perfromance in sport (1.7 %) and Others reason (2.5 %).
Conditions of spectacles among compliant and non-compliant studentsAmong compliant students, 97.4 % maintained their spectacles in good condition. In contrast, 46.7 % of non-compliant students kept their spectacles in good condition but were not wearing them. Additionally, 20.2 % of non-compliant students had broken their spectacles, with only 3 % seeking repairs (Fig. 3).
Non-compliant student but having the spectacles (n = 3892)Out of the non-compliant students, 21 % said they had spectacles in their bags or at home, while 79 % said they did not have the provided spectacles at all. Most of the time students are not using spectacles due to cosmetic purposes when the power is low and not affect the vision significantly.
DiscussionThe present study assessed the prevalence of spectacles-wearing compliance among school-aged children (6–18 years) across five selected districts in Koshi and Madhesh provinces, Nepal, and investigated the underlying reasons for both non-compliance and compliance to spectacles wear. Key findings revealed differences between students who purchased spectacles and those who received them free of charge, also highlighting issues such as spectacles quality, aesthetic concerns, and social stigmas that directly influence compliance. As a school-based study covering a large sample of students across five districts, the findings of this research are broadly generalizable.
In this study, the compliance rate for spectacles wear was found to be 62.8 % following a surprise visit conducted three months after screening and providing spectacles to students. Globally, compliance rates show considerable variation, as highlighted by a 2020 meta-analysis covering 20 studies from 14 countries, which reported compliance rates ranging from as low as 9.84 % (95 % CI, 2.36–17.31 %) to as high as 78.57 % (95 % CI, 68.96–88.18 %).26 The compliance rate of 62.8 % in this study is notably higher than findings from other studies in Nepal, where compliance rates were reported at 28 %23 and 51 %27but slightly lower than the study done in eastern Nepal where compliance rate was 76 %.10 This higher compliance rate may be attributed to increased awareness among students or possibly the greater severity of refractive errors.
The notable difference in compliance rates between students who received free spectacles (55.6 %) and those who purchased them (77.8 %) suggests that payment status might influence how students perceive the value of their spectacles and their commitment to wearing them. When students or their families pay for spectacles, they may view them as a valued investment, increasing their sense of responsibility and motivation to wear them regularly. In contrast, free spectacles might be seen as less valuable, possibly reducing the perceived need for consistent use. Additionally, paid spectacles may come with options for personalized choices, potentially improving satisfaction with aspects like fit, comfort, or style-factors that can also impact compliance. Likewise, families who are able to purchase spectacles may possess higher health literacy, stronger engagement with their child's healthcare, or better access to services for repairing or replacing damaged spectacles. These households may also demonstrate greater follow-through with health-related advice and fewer structural barriers to compliance.
This study revealed higher compliance with spectacles wear among younger children aged 6–10 years, a finding consistent with studies conducted in India28 and Mexico.29 However, this contrasts with the other studies from India,30 Pakistan,11 and Chile,31 where compliance was found to be greater in older age groups. These mixed findings suggest that age may interact with other contextual or behavioral factors that influence spectacle wear. One possible reason for higher compliance among younger children in our setting might be the greater influence of parental monitoring and guidance at earlier ages. Younger children are often more dependent on their caregivers and may be more likely to follow instructions regarding health-related behaviors, including consistent spectacle use. Additionally, younger children may be less self-conscious about their appearance and less affected by peer opinions, which can often influence children's willingness to wear spectacles. In contrast, adolescents may experience increased social pressure, stigma, or aesthetic concerns that negatively impact compliance. In this study, we found no significant gender differences regarding compliance with spectacles wear, consistent with findings from South India.5However, one study from Nepal found that girls were more likely to wear spectacles than boys.23
In this study, students in grades 9–12 demonstrated slightly higher compliance with spectacle use compared to younger grade levels. This observation appears contradictory to our finding that younger children (ages 6–10) were more compliant, highlighting a potential discrepancy based on age versus academic grade. The inconsistency between age-related compliance patterns and those based on academic grade suggests the need for further investigation to clarify this gap. Our findings indicate that compliance with spectacles use was higher among students from private schools compared to those from public schools, aligning with the trend observed in previous study.23
This study found an association between the severity of refractive error and adherence to spectacles use, with students exhibiting high degrees of hypermetropia and myopia showing higher compliance than those with milder refractive errors. This finding is consistent with a meta-analysis indicating that the severity of refractive error is a key factor in spectacles-use compliance.32 Studies from rural China33 and Oman34 similarly identified severity of refractive error as a strong predictor of adherence, with high myopic students in particular demonstrating higher compliance. This trend may be explained by the more noticeable impact of severe refractive errors on daily activities, including reading and classroom learning, which may prompt students to wear spectacles more consistently to improve vision quality.
A major reason cited by students for non-compliance with spectacles use in our study was broken lenses or frames, a barrier corroborated by findings in multiple other studies.23,27,28,30 Broken or damaged spectacles can disrupt consistent use, especially in cases where repair or replacement is delayed due to cost or accessibility issues. Another reason for non-compliance reported by students was their tendency to use spectacles only on special occasions or when they deemed it necessary, rather than consistently. This selective use is echoed in findings from studies in India, where students reported wearing spectacles only when required.35,36 Uncomfortable spectacles and a general dislike of wearing them were also common reasons for inconsistent spectacles use among students in our study, a trend observed in other studies as well. Discomfort may arise from poor fit, weight, or pressure from the frames, which can make prolonged wear unappealing, particularly for younger students. Additionally, a dislike for the appearance of spectacles, often influenced by aesthetic or social preferences, can discourage consistent wear.26,30,37 Teasing from peers and disapproval from parents emerged as significant factors influencing students' choices to use spectacles, mirroring findings in other studies.28,34,35 Peer teasing can create a social stigma around spectacles use, particularly among children and adolescents, who may feel self-conscious about their appearance. Parental disapproval, whether due to cultural perceptions or misconceptions about spectacles, can further discourage students from consistent use.
The strength of the study was the project was managed paperless using a custom IT solution for efficient data handling. Project was locally implemented by the dedicated team of eye hospitals under NNJS in the respective districts. Data quality was maintained under the lead optometrist’s supervision, with ophthalmologists guiding clinical decisions. Clear guidelines ensured high standards. Children received free spectacles, medications, and surgeries. Major eye hospitals were key to its success. The project was approved by the Social Welfare Council (SWC), and was monitored by Orbis and NNJS, ensuring alignment with national health goals. The study offered valuable insights into disparities in compliance, particularly between students who received spectacles free of cost and those who purchased them, pointing to potential perceptions of quality or value. The findings also contribute to the broader understanding of spectacles wear compliance among school children in Nepal, informing future strategies for vision correction programs. As a school-based study covering a large sample across five districts, the results are broadly generalizable within similar settings. This study has few limitations. It did not fully explore parental involvement or the socio-cultural dimensions influencing spectacle use, which could provide deeper insights into non-compliance behaviors. Further qualitative research is recommended to better understand these factors. Since the unannounced visit was conducted only once per school, it may not accurately capture the compliance of all students who received spectacles but were absent during the visit. Information on compliance longitudinally has not been investigated. This limitation could have affected the compliance prevalence. Therefore, future programming should consider incorporating periodic follow-up visits rather than relying on a single assessment to better track usage trends and intervene as needed.
In conclusion, this study found that more than one-third of students were non-compliant with spectacles use, highlighting key factors influencing compliance among school children in Nepal’s Koshi and Madhesh provinces. Compliance was higher among younger children, private school students, and those with severe refractive errors. Common barriers include broken or uncomfortable spectacles, selective use on special occasions, and social concerns like teasing and parental disapproval.
Based on the findings of this study, several programmatic improvements can be recommended to enhance spectacle compliance among school children. First, a dedicated provision for the repair or replacement of broken spectacles—particularly frames and lenses—should be incorporated into program budgets to address one of the most common barriers to compliance. Second, implementing structured parental engagement sessions as part of the school screening workflow could foster greater awareness of the importance of spectacle use and help address social stigma, particularly among younger children. Third, efforts to provide comfortable, durable, and visually appealing frame designs—especially those acceptable to both students and parents—should be prioritized to reduce non-compliance due to discomfort or aesthetics.
Authors contributionsRS and SKM conceptualized the study. RS, AS, and AP conducted formal data analysis. The Methodological section was developed by RS, AP, PRS, and PRA. Supervision and validation were performed by RRB, SS, YDS, RDG, AKS, and RS. Findings, analysis, presentation and visualization were completed by RS, AKS, and PRS. The initial manuscript draft was prepared by RS, AP, SKM, AKS, AS, PRA, and PRS. Critical revisions of the draft were done by PRS, SS, SKM, and RRB.
Ethical approval and consent to participateThe study obtained informed consent from individual students and written consent from school principals before screenings. Throughout the referral journey, parents were kept informed via phone calls or messages relayed through the school authorities. Ethical approval was granted by the Institutional Review Committee (IRC) of NNJS (Ref. No. 91/081/082), adhering to the Declaration of Helsinki. Approval for project execution was secured from the SWC, under Nepal's Ministry of Women, Children, and Senior Citizen. Subsequently, written agreements were established with local municipalities, followed by written approvals from individual schools to conduct the screening program comprehensively.
Availability of data and materialsThe datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request or can be accessed from the figshare.
Shankar, P Ravi; Shah, Ranjan; Mishra, Sailesh K; Ray, Pankaj; Kumar Singh, Amit (2024). Compliance of spectacle wear among school-going children in selected districts of Nepal. Dataset. https://doi.org/10.6084/m9.figshare.27800241.v1
Consent for publicationAll authors reviewed and approved the final version for submission.
The author(s) report there are no competing interests to declare.