To evaluate myopia progression as assessed by changes in axial length (AL) and spherical equivalent (SE) from baseline in Caucasian children wearing multifocal soft contact lenses (MCL) compared to single-vision distance spectacles. Methods: Forty progressing (at least -0.75D increase in previous 12 months) myopic children (7–12 years old) with SE ranging from -0.75 to -4.50 D were recruited in a longitudinal prospective non-randomized study. 20 were fitted with MCL (+2.50D add), whereas 20 wore single-vision distance spectacles. Cycloplegic refraction was measured with an auto-refractometer (Topcon TRK-2P, Japan) and AL with IOLMaster 700 (Carl Zeiss, Germany). Subjective responses related to vision and comfort of MCL wear were determined with a questionnaire scaled from 0 (very poor) to 10 (excellent). Results: After 2 years, mean change in SE/AL in the MCL group was - 0.82±0.25D/0.51±0.02 mm and -1.12±0.14D/0.66±0.03 mm in the spectacles group (all p < 0.001). Cumulative Absolute Reduction in Axial Elongation (CARE) was 0.15 mm. Difference in SE change was 0.30D. 97.5 % of children in the spectacles group showed an AL increase of between 0.61 and 0.70, and 70 % of eyes showed an SE increase of −1.00 D. In the MCL group, there was no case with an elongation >0.60 mm, with 67.5 % of eyes being between 0.51 and 0.60 mm. In contrast, over half of the MCL group exhibited lower SE progression, from 0.50 to 0.75 D. Conclusion: A slower myopia progression rate was achieved with a centre distance MCL with +2.50D addition after two years of wear compared with the spectacles group.
Increasing levels of myopia impose a health, economic, and social burden, especially in East and Southeast Asia, where the prevalence of myopia in young adults is approximately 80–90 %, and that of high myopia is 10–20 %.1,2 A recent study in Spanish children aged five to seven years reported a myopia prevalence of 19 % between 2016 and 2021, with projections indicating an increase to 30.2 % by 2030.3 During the early stage of human life, axial length (AL) is considered to be driven by emmetropisation—a physiological process—from hyperopia to emmetropia. Children who develop myopia show excessive AL elongation, which tends to stabilise after the age of 15, although it continues to increase in the top 50th percentile.4-6
Presently, there are several options to delay myopia rather than simply correcting vision and improving the quality of life.7-10 These include changes in lifestyle, such as improving time spent outdoors,11 spectacle-based strategies,12-14 pharmacological treatments,15-17 low-level red-light therapy, overnight orthokeratology with rigid gas permeable (RGP) contact lenses (CL),18 and soft CL designed for myopia management.19-24 Moreover, combining strategies such as pharmacological and optical treatments improves treatment efficacy.25-27 Regarding soft CL, previous studies showed different power profiles, including multifocal with aspherical designs (MCL) for presbyopia,23,24 extended depth of focus (EDOF),20,22,28-30 multi-concentric with annular rings,19,21,31 non-coaxial toroidal,32 and also an asymmetrical power map.33 MCL present a central optic zone with distance correction surrounded by progressively positive power to generate a positive spherical aberration, which could prevent axial elongation.24,34-36 Interestingly, a recent study suggests no evidence of a loss of treatment effect after discontinuing centre-distance soft MCL with +2.50D addition in older teenagers.37 Previous studies used MCL designs with standard parameters,23,24 so little is known about MCL with customised parameters (different base curves and diameters) in myopia control, which could be helpful in cases where adaptation is unsatisfactory. The purpose of the current study was to evaluate the myopia progression rate in Caucasian children over a two-year follow-up—as assessed by changes in AL and cycloplegic refraction from baseline—using customised progressive MCL with an addition of +2.50 D compared to single-vision distance spectacles, and to determine possible differences between groups.
Material and methodsStudy design & participantsA total of 40 myopic children aged between 7 and 12 years old were recruited in this prospective, longitudinal clinical trial conducted at Clínica de Oftalmología Integral in Bilbao, Spain. All participants were of European (Caucasian) ethnicity, with normal ocular health that did not preclude contact lens wear. Inclusion criteria included myopia progression of at least −0.75 D in the past 12 months, determined after cycloplegic refraction; best-corrected visual acuity of at least 0.00 logMAR in both eyes; a cycloplegic spherical equivalent (SE) ranging from −0.75 to −4.50 D; and astigmatism of up to 0.75 D Children with a history of CL wear or any myopia control treatment, a history of systemic or ocular disease, or who were currently using any systemic or topical ocular medications were excluded.
Parents or legal guardians were informed about the different pharmacological or optical options to slow down myopia. Next, children were allocated to their preferred treatment group rather than randomised. Therefore, those interested in participating in the current trial and being fitted with soft MCL were screened for suitability according to the inclusion criteria and assigned to the MCL group if eligible. If they were interested in participating in the trial but not in myopia management or single-vision contact lens fitting, they were assigned to the control group to wear single-vision distance spectacles. A clinic secretary carried out patient allocation without the participation of the examiner. A total of 20 participants were assigned to wear MCL, and 20 were assigned to the control group to wear spectacles.
Ocular and visual outcomesAll trial-related measurements were conducted by a single optometrist (S. D-G) at baseline and six-monthly intervals. Ocular health was also evaluated by two ophthalmologists (A.U. and J. L-G) at baseline and every six months. Two drops of 1 % cyclopentolate hydrochloride (Alcon Cusí, Spain) were instilled into each of the participant's eyes 5 min apart. Twenty minutes after the installation, three refractive error measurements were taken with an auto-refractometer (Topcon-TRK-2P, Tokyo, Japan). The IOLMaster® 700 Biometer (Carl Zeiss, Jena, Germany) was used to assess AL. Corneal data were evaluated with the topographer-aberrometer OPD Scan III (Nidek, Gamagori, Japan)
Visual performance was measured under photopic conditions (≥85 cd/m2), with best spectacle correction or CL wear as the control and test groups, respectively. The SE was calculated as SE = Sphere + Cylinder/2. LogMAR High-contrast (96 %) corrected distance visual acuity (CDVA) was assessed using an OptoTab (SmartThings4vision, Zaragoza, Spain) placed at 5 m under normal room lighting (photopic luminance). Subjects were required to identify each letter on the chart until they incorrectly identified a whole row of letters; at this point, the test was terminated, and visual acuity was calculated. Subjects were encouraged to guess letters if they were unsure.
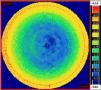
Contact lensesSaphir Rx Multifocal® (mark´ennovy, Spain) is a soft silicone hydrogel CL (Filcon 5B (60) [75 %]) designed to correct presbyopia, associated or not with myopia, hypermetropia, or astigmatism. The lens features a multifocal design over the optical zone, available in centre distance and centre near designs with additions of between 0.50 and 4 D to provide good distance, intermediate, and near vision. The study lenses are a non-toric centre-distance design with a + 2.50 D addition. The central area maintains a constant-power distance prescription, followed by a progressive transition to the near portion. Finally, the near power has constant refraction with a maximum relative positive power approximately 3 mm from the centre (Fig. 1).
The CL material has an oxygen permeability (DK) of 60, an elasticity modulus of 0.33 MPa, a coefficient of friction of 0.02, a blue handling tint, and a Class I ultraviolet (UV) filter (absorbs >90 % of UV A and >99 % of UV B). The lens is available in a monthly replacement for individual ocular parameters: total diameter from 13.00 to 16.00 mm in 0.50 mm steps, base curve from 6.80 to 9.80 mm in 0.30 mm steps, spheres ±30.00 D in 0.25 D steps, cylinders from −0.75 to −8.00 D in 0.25 D steps, and additions from 0.50 to 4.00 D in 0.50 D steps.
Initial customised lens parameters (base curve and diameter) were calculated by the manufacturer considering topographic anterior corneal outcomes (keratometry, horizontal visible iris diameter (HVID), and eccentricity) and the refraction obtained after referencing the corneal plane. After 15 minutes of fitting, a slit-lamp evaluation (Topcon SL-D4, Japan) was performed to check that each lens was acceptably positioned in terms of centration and movement. CLs were used on a daily wear basis, and participants were instructed to wear them during all waking hours and every day with a minimum wear time of six days per week and at least 10 h each day. Lenses and lens cases were replaced on a monthly basis. Alvera (Avizor, Spain) multipurpose solution was provided to CL wearers for use with the lenses. The composition of the solution includes aloe vera, poloxamer, polyvinylpyrrolidone (PVP), disodium edetate (EDTA), and polyhexanide (PHMB) 0.0002 %.
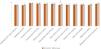
Subjective measurementsSubjective responses related to vision and lens wear comfort were determined using a questionnaire—ranked from 1 (very poor) to 10 (excellent) in one-unit steps—administered after one month and two years of CL wear. The categories comprised handling (upon insertion, after 5 min, and at removal), comfort (5 min after insertion and at the end of the day), clarity of vision (distance, intermediate, near, and night-time), vision stability (distance, near, and night-time), overall satisfaction, and willingness to continue wearing the lens.
Statistical analysisAll statistical tests were performed using Statgraphics 19 (Statgraphics Technologies, Inc, USA). Given that data was collected on both eyes, combined data was presented and analysed using a General Linear Model, including all the eyes. Descriptive statistics, including the mean and standard deviations of the quantitative data, were calculated. Changes in AL and SE were the primary outcome variables. The normality of all data samples was assessed using the Shapiro-Wilk test. The student’s t-test was used to compare outcomes between the spectacles and MCL groups at baseline, 6, 12, 18, and 24 months. AL, SE, and CDVA variations in the follow-up periods were compared between the spectacles and MCL groups using a repeated measures ANOVA with a Greenhouse-Geisser correction, followed by Bonferroni post-hoc test. Pearson or Spearman correlation analysis was performed to analyse the relationship between baseline outcomes and changes in AL or SE and between changes in AL and SE over the two-year study period. The efficacy of myopic control of CLs was determined by comparing differences in AL progression between test and control groups and was defined as Cumulative Absolute Reduction in axial Elongation (CARE).8 Similarly, differences in SE progression between test and control groups were also computed. Statistical significance was set at a level of 0.05 (*p < 0.05; ⁎⁎p < 0.01; ⁎⁎⁎p < 0.001).
ResultsTable 1 presents the baseline demographic data of the 40 participants assigned to the spectacles and MCL groups. There were no statistically significant differences in age, AL, or SE between groups. Most children (95 %) had at least one myopic parent in the MCL group; this percentage was lower (75 %) in the spectacles group. In the MCL group, there were six cases of mild corneal staining, which did not necessitate discontinuation of CL wear. No more adverse events were detected. There were no dropouts during the study period. Questionnaire responses after one month and two years of CL wear are represented in Fig. 2. All items showed a mean rating value ≥ 9. A statistically significant improvement was found in “near clarity of vision” at two years compared with one-month values.
Demographic outcomes measured in the control and experimental groups.
AL, axial length; SE, spherical equivalent. Age, AL and SE expressed as mean ± SD.
The AL and SE results at each visit are represented in Table 2. There were no differences in AL and SE progression with respect to right/left eyes, sex, or number of myopic parents, nor with the combined effect of these variables (p > 0.05).
Axial length and spherical equivalent in the control and experimental group measured at baseline, 6-. 12-, 18- and 24 months (Mean ± SD).
AL, axial Length; SE, spherical equivalent; M, months. Statistically significant difference: p < 0.05.
Repeated measures ANOVA (p < 0.001) and Bonferroni post hoc test indicates statistically significant differences in AL and SE changes between all measured times for both the MCL and spectacles groups. Over the two-year follow-up, significantly less axial elongation was observed in the MCL group than in the spectacles group (p < 0.001), as represented in Fig. 3. The total increase in AL was 0.66 ± 0.03 mm (from 0.60 to 0.77) in the spectacles group (p < 0.001) and 0.51 ± 0.02 mm (from 0.40 to 0.55) in the MCL group (p < 0.001), resulting in a CARE value of 0.15 mm. Similar to AL, changes in SE were significantly different between the MCL and spectacles groups (p < 0.001) at all measured times, being smaller in the MCL group. The total increase in SE was −1.12 ± 0.14 D (from −1.00 to −1.50 D) in the spectacles group (p < 0.001) and −0.82 ± 0.25 D (from −0.50 to −1.25 D) in the MCL group (p < 0.001). SE variations between the two groups exhibited a mean difference of –0.30 D.
Fig. 4 illustrates the distribution of AL and SE changes during the entire follow-up period. In the spectacles group, 97.5 % of the children presented an AL increase ranging from 0.61 to 0.70 mm. In the MCL group, no elongation exceeded 0.60 mm, with 67.5 % of eyes presenting an increase between 0.51 and 0.60 mm. Regarding SE, in the spectacles group, 70 % of eyes had an SE increase of −1.00 D; in contrast, over half of the MCL group presented lower SE progression, from 0.50 to 0.75 D.
There were no correlations between baseline AL and AL changes over time (p = 0.07 and p = 0.36 for the spectacles and MCL groups, respectively) nor between baseline SE and SE changes (p = 0.94 and p = 0.06 for the spectacles and MCL groups, respectively). When the relationship between changes in AL and SE for the entire period was analysed, a correlation was only found for the MCL group (rho=0.51/p = 0.01). Therefore, the greater the AL change, the larger the SE change after a two-year follow-up.
Binocular logMAR CDVA results at baseline, 12, and 24 months are represented in Table 3. There was no statistically significant change throughout the follow-up period. For CDVA, there was a statistically but not clinically significant difference lower than two letters at baseline and 24 months (p<0.05).
logMAR corrected distance visual acuity in the control and experimental groups measured at baseline,12- and 24 months (Mean ± SD).
| Baseline | 12M | 24M | p-value | |
|---|---|---|---|---|
| Spectacles | −0.04 ± 0.04 | −0.04 ± 0.04 | −0.04 ± 0.04 | >0.99 |
| Contact lens | −0.01 ± 0.03 | −0.02 ± 0.03 | −0.02 ± 0.02 | >0.99 |
| p-value | 0.01⁎ | 0.16 | 0.04⁎ |
M, months.
This study adds clinical data to the evidence indicating that the myopia progression rate can be slowed down using MCL with a + 2.50 D progressive addition compared with control single-distance vision spectacles in a Caucasian child population. In agreement with the study of Walline et al.,24 there was a low percentage of adverse events that did not lead to wear discontinuation, confirming the safety of the fitted MCL.24
The present study included Caucasian children; thus, a slower change in AL and SE than that observed in an Asian population was expected.38 On the other hand, the current study only included children with evidence of at least a −0.75 D increase over the previous year before the inclusion. Aller et al.23 studied bifocal soft CL (Acuvue bifocal, Vistakon) in multiracial children who progressed −0.50 D or more since their last examination, apart from near-point esophoria and/or accommodative dysfunctions. They reported an AL increase of only 0.05 mm after a one-year follow-up. In contrast, the control group, fitted with single-vision (SV)-CL, increased 0.24 mm, with a CARE value of 0.19 mm, higher than the current study (0.15 mm). The fitted CL presented a central optic zone <2 mm surrounded by two concentric addition rings with the maximum relative positive power.39 Walline et al.24 fitted two progressive centre distance MCL (Biofinity, CooperVision) with different additions (+2.50 and +1.50 D) and a refraction range of −0.75 to −4.00 D in 98 multiracial, mostly Caucasian, children aged 7 to 11 years. They reported a lower AL change than the present study with the +2.50 D Add (0.16 and 0.30 mm at 12 and 24 months, respectively), while the AL change was high in the +1.50 D Add group (0.26 and 0.44 mm at 12 and 24 months, respectively). The lower efficacy of Saphir Rx lens could be due to Biofinity presenting the maximum relative positive power at approximately 2 mm from the optical zone centre.
Interestingly, the efficacy in the studies of Aller et al.23 and Walline et al.,24 with smaller optic zones than the current study, could indicate that myopia control with MCL could be related both to high addition power and a more central location, similar to how a smaller back optic zone diameter in orthokeratology may be beneficial for retarding axial elongation.40
The cumulative variation in AL in the test group of the current study (0.51 mm) aligns with the paper published by Sankaridurg et al.,20 although conducted in an Asian population aged 7 to 13 years and including a spherical refractive error ranging from −0.75 to −3.50 D The authors fitted four hydrogel test CL, where test Lenses I and II had +2.50 and +1.50 D Add, respectively. Like Saphir Rx, the lenses presented the maximum relative positive power at approximately 3 mm. In addition, a stepped, relative positive power was incorporated centrally (up to 1.0 mm semi-chord) of up to +1.00 D. Comparing the results of lens I and the current study, the authors reported a slightly lower change in the same 2-year follow-up period (0.44 mm). Similar AL changes were found with test Lens II (0.45 mm).
Comparing the results of the present study with those previously obtained by the same authors with an EDOF CL (MYLO; mark´ennovy), also with a two-year follow-up and the same inclusion criteria, the efficacy of the analysed MCL was half that obtained with EDOF CL, with a CARE of 0.1 mm and 0.2 mm, respectively, at the two-year follow-up.22 On the other hand, in accordance with the current study, Ruiz-Pomeda et al.41 also conducted a study in Spanish children, mainly Caucasian, aged 8 to 12 years, ranging from −0.75 to −3.50 D, and fitted with Dual-focus CL (MiSight, CooperVision) vs Single-Vision spectacles. They found a CARE of 0.17 mm after a two-year follow-up. The authors did not have inclusion criteria of a minimum −0.75 D increase in the previous 12 months.
Regarding SE, the variation in the whole follow-up period (−0.82D) was lower than that reported by Sankaridurg et al.,20 with a mean increase of −0.92D. Theoretically, AL variation should correlate with the change in SE. However, various factors can influence the relationship between both variables. Ulaganathan et al.42 described that the mean amplitude of daily variations in AL is 0.029 ± 0.007 mm; thus, minor variations could be neglected when considering yearly AL changes. To minimise this influence, children were evaluated at the same time in the current study.
Concerning visual performance, in agreement with this study, Aller et al. found an HCVA of −0.04 logMAR with +2.50 D Add with no statistically significant difference compared to SV-CL. The satisfactory results in the subjective questionnaire were similar between one month and two years of MCL wear, agreeing with the previous ratings reported with soft CL. In a recent systematic review and meta-analysis, Ping et al.43 reported that subjective impression ratings for vision and comfort with myopia MCL were slightly lower than for single-vision lenses. Moreover, children rated their overall visual experience higher than young adults. Notably, all the subjects of the present study wished to continue wearing contact lenses.
The present study had some limitations that could be improved upon in future studies. First, the lack of randomisation is a limitation that could introduce unwanted confounding variables and bias. It is believed that this study is more representative of a real-life scenario where patient motivation plays an important role in myopia management and may result in a lower number of discontinuations from the control group (no dropout was found). However, masking was not possible, and it could inflate the perceived effectiveness of the intervention compared to real-world settings. Moreover, it would be necessary to increase the sample size. Additionally, visual function under photopic and mesopic conditions, as well as the influence of customised contact lens parameters regarding centration and movement, could be analysed, since previous studies with MCL used standard parameters.
ConclusionIn Caucasian children, a slower myopia progression rate was achieved with a centre distance multifocal contact lens fitting with +2.50 D addition after two years of wear compared with the single-vision distance spectacles group.
Ethics approval and consent to participateThis clinical trial was conducted in accordance with the tenets of the Declaration of Helsinki and was approved by the institutional review board of the Hospital Clínico San Carlos of Madrid (Code: 19/264/E). The children’s parents/carers signed the informed consent form, and all children assented to participate in the trial.
Fundingmark´ennovy manufactured and provided the contact lenses used in the study. Avizor provided the maintenance solutions.
CRediT authorship contribution statementSergio Díaz-Gómez: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. Amaia Urkia-Solorzano: Data curation, Investigation, Writing – review & editing. José A. López-Garrido: Data curation, Investigation, Writing – review & editing. Mercedes Burgos-Martínez: Conceptualization, Writing – review & editing. Jesús Carballo-Álvarez: Conceptualization, Data curation, Investigation, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing.
M.B-M. is an employee of mark´ennovy. This company has commercial interest in myopia control products. All of the other authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
The authors would like to thank Santiago Cano-Alsúa, Complutense University statistician, for collaborating on the statistical analysis and Laura Sáenz-Barrera for helping with participant management.