Evidence indicates the existence of an association between socioeconomic status (SES) and the prevalence of myopia in the adult population. In contrast, there are limited studies investigating this association in children. The purpose of this study was to investigate the association between the presence of myopia in 8-year-old children from southern Europe and SES defined as parental educational level and employment status.
MethodsParticipants aged 8 years old were recruited from 16 schools located in Terrassa, Spain (n = 813). Ten of these schools were classified as “high complexity” schools (low SES). Refractive error was assessed using non-cycloplegic retinoscopy. Parental questionnaires were used to gather socioeconomic information such as parental education level and employment status. Non-parametric Kruskal Wallis, Mann Whitney and Chi-square tests were used to evaluate the association between spherical equivalent (SE) and parental educational level and employment status as well as differences in the SE distribution between high-complexity and regular schools.
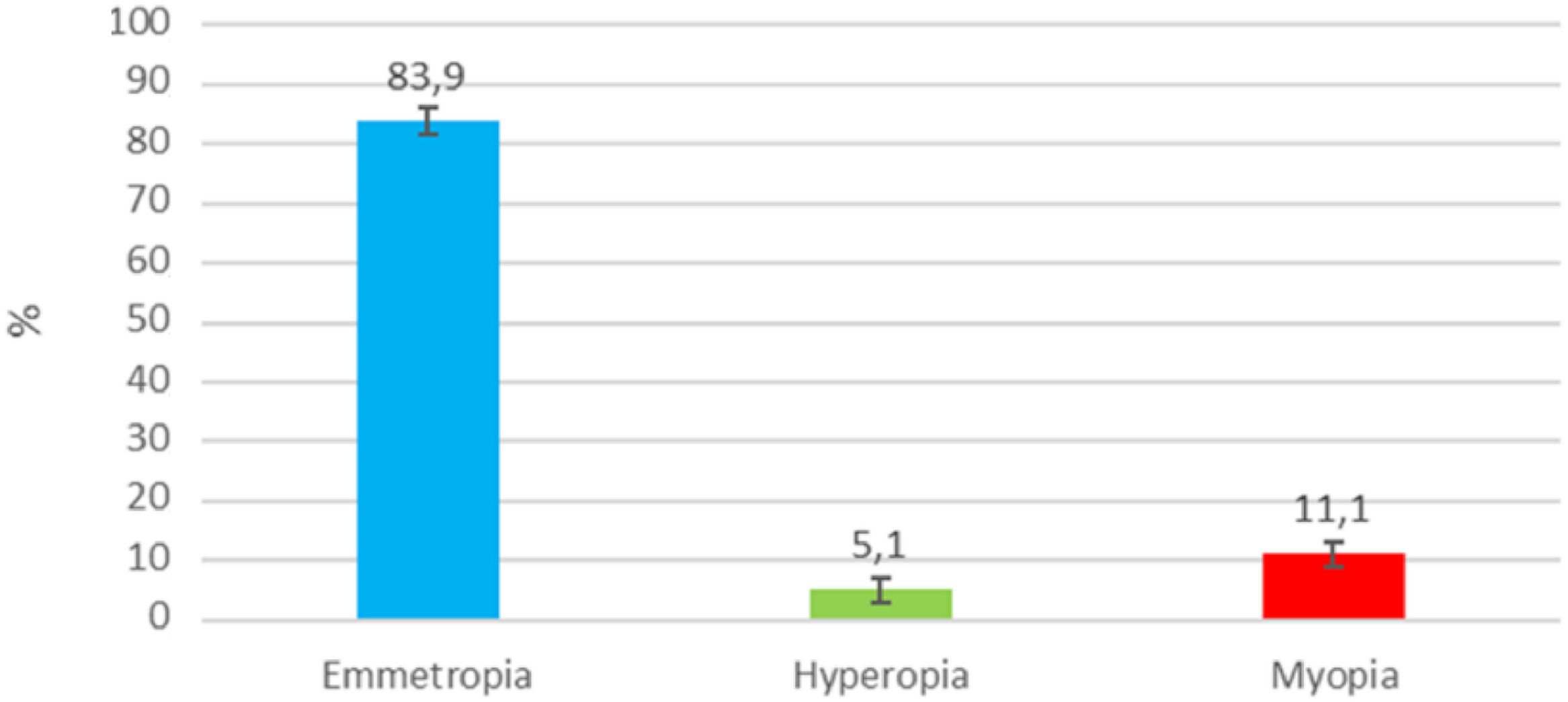
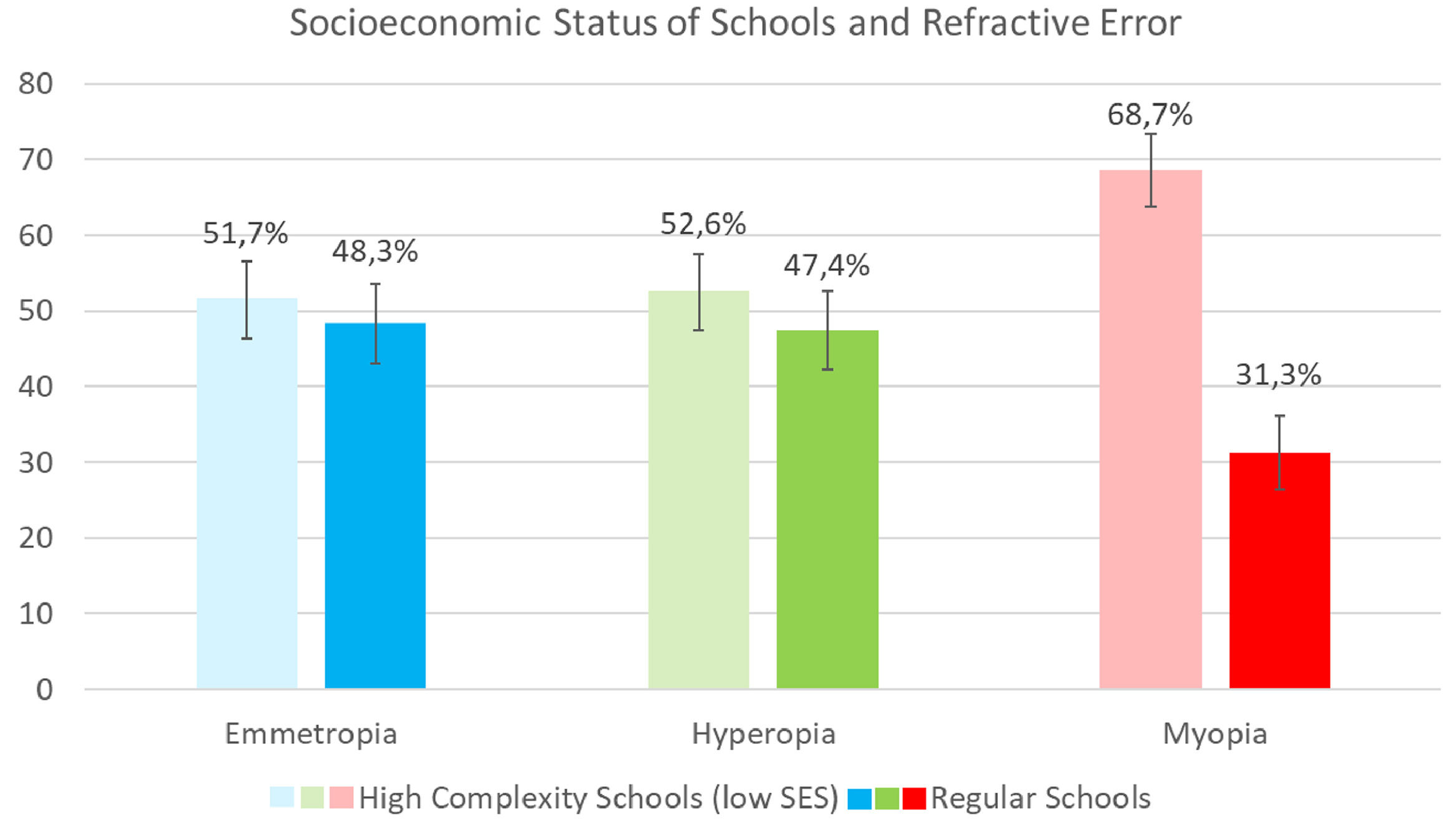
ResultsMyopia was more prevalent than hyperopia in the population sample (11.1% vs 5.1 %). Chi-square tests revealed a significant association between attending “high-complexity” schools and the presence of myopia (p = 0.014). In contrast, no significant associations were found between SE and SES. A trend for higher prevalence of myopia in children whose mothers had low educational level and were unemployed was observed.
ConclusionsWhile no significant associations are found between SE and parental education or employment status, myopia is more frequently found in schools with low SES (“high-complexity” schools), suggesting a potential link between SES and childhood myopia.
Uncorrected refractive error is the second leading cause of visual impairment globally and the main cause of visual impairment in children.1 The increased prevalence of refractive errors in the paediatric population and the cost associated to their correction with optical, surgical and pharmacological treatments pose a global economic burden and a public health concern.2,3 From a socio-economic point of view, uncorrected refractive errors can also have an impact on children's academic performance further impacting on their development, learning and quality of life.3
Myopia is the most common refractive error in the world with increasing concerns of becoming a pandemic, given the continuous global increase in its prevalence in recent decades.4,5 For instance, the global prevalence of myopia in 1993 was of 10.4 %,6 while in 2000 the prevalence had doubled (22.9 %),5 and projections indicate that the prevalence of myopia will reach 50 % of the population by 2050.5 Further, it has also been estimated and proposed that by 2050, 10 % of myopes will be high myopes,5 and therefore will suffer from the additional ocular changes and abnormalities that high myopia implies.7 In Europe, the current prevalence of myopia is variable across countries (ranging from 15 % to almost 50 %)8-11 and these discrepancies could arise from differences in participant recruitment and study design, but could also arise from genetic as well as environmental differences.
Besides genetics, multiple environmental risk factors for myopia have been proposed being education and time outdoors, the two major risk factors identified.12 In terms of education, there is extensive evidence to support the association between education level and myopia development in young adults. For instance, evidence from early studies suggests that myopia is less prevalent in societies with limited schooling.13 In addition, the prevalence of myopia has also been shown to increase for older children who spend more hours in education,14 and also for children attending more academically challenging schools or courses,15 as well as children with higher academic achievements.16 Similarly, solid evidence exists to support the view that time outdoors is an important protective factor for myopia development.12 A meta-analysis has demonstrated the effect of time outdoors for the onset of myopia,17 but there is still some controversy regarding the impact of time outdoors on myopia progression.
While higher risk of poor health has been shown in individuals with low socioeconomic status (SES),18,19 considering the associations between education and myopia, it could be reasonable to argue that the link between SES and myopia may be different. For instance, families of higher SES may prioritise education and academic achievements, over outdoor and physical activities. The impact of socioeconomic factors on myopia has already been investigated in some Asian countries suggesting an increased prevalence of myopia in children from families with high SES defined by household monthly income and parental home ownership.20 Having said this, the link between childhood myopia and socioeconomic factors is still unclear and some study results are conflicting. These could be explained by some arguments like the number of confounding factors that may play a role in the study of this relationship. Also, evidence from different studies may be difficult to integrate and collate given the differences between populations from different countries.12 Finally, the investigation of the relationship between childhood myopia and SES is complex because this is not directly related to the children, but to their families. Hence, while there are some studies investigating the associations between education, SES and myopia in adult European populations21,22 research investigating this link in paediatric European populations is limited. To the authors knowledge, there is currently one European paediatric cohort conducted in The Netherlands that has examined the prevalence of childhood myopia in different socioeconomic groups based on the parents’ ethnicity, the mother's education, and the household income.23
The aim of this study is to further investigate the association between the presence of myopia in children from southern Europe and SES defined by parental educational level and parental employment status. The association between myopia and attending “high-complexity” schools is also investigated.
Materials and methodsStudy population sampleThe study population sample consisted of 813 children aged 8 to 9 years attending primary schools in the city of Terrassa (Barcelona), Spain. A number of local schools (public/state maintained and private/independent schools) located across the city were invited to participate in the study. In addition, the Townhall and Council of the city of Terrassa were approached to support the recruitment of schools classified as “high-complexity” (i.e. low SES). In Catalunya, where the study was conducted, the Catalan government (“Generalitat de Catalunya”) is responsible for the classification of schools as being of “high-complexity”, and this is conducted considering the socioeconomic and administrative context of the area where the educational institution is located. Amongst others, the criteria for the classification of a school as being of “high-complexity” considers the parental educational level, the parental employment status, the percentage of pupils whose parents have migrated to Catalonia from other countries, and the percentage of pupils with special educational needs and disabilities.24 The objective of this classification is to take into account and compensate socioeconomic and cultural inequalities that may exist between educational institutions by providing support staff to improve the pupils’ academic achievements.24 A total of 16 schools were recruited: 10 schools that were classified as “high complexity schools” (low SES) and 6 schools that have not been classified as such (i.e. regular schools/non-high complexity schools).
The sample size was calculated with EpiData (EpiData Association, Odense. Denmark version 3.1) considering the reference population of 35,000 children of the city where the study was conducted and a confidence level of 95 %. According to such calculation the minimum sample size required for the study was of 245, which is lower than the 813 schoolchildren recruited in this study.
Study designThis is an epidemiological cross-sectional study to investigate the relationship between refractive error, SES (defined by parental educational level and employment status), and school classification (“high-complexity” vs. “non high-complexity/regular”). While currently this is a cross-sectional study, the long-term objective is for the study to become longitudinal in the framework of the CISViT project. Hence, the children of this study are also the first stage participants of a cohort study project named ‘Cohort Infantil de Salut Visual de Terrassa (CISViT)’ [Terrassa Infantile Visual Study Cohort].
Study information sheets and parental consent forms were provided to all schools participating and the teachers were responsible for their distribution to the parents of child participants. Children whose parents consented in participating, attended a single visit at the Centre Universitari de la Visió (University Vision Centre; the Universitat Politècnica de Catalunya optometry clinic) with their school group and accompanied by their teacher. Prior to taking any clinical measures, the teachers provided the signed parental consent forms to the researchers.
The protocol was approved by the Drug Research Ethics Committee of Mútua de Terrassa (P/22–090) and designed in accordance with the Declaration of Helsinki. Written informed consent was obtained from the participants’ parents or guardians.
Data collectionDuring the visit all data was collected by multiple clinical researchers that were trained to follow the same protocol and procedures which included the assessment of refractive error, visual acuity (VA) and ocular alignment.
Refractive error was assessed using objective refraction with non-cycloplegic retinoscopy while fogging the contralateral eye with positive lenses. The result was recorded in sphero-cylinder form and the SE was later calculated and used for the classification of the refractive error as emmetropia: −0.5D ≤ SE ≤ +1.50D; hyperopia: SE > +1.50D; and myopia: SE <−0.50D. Presenting (with refractive error correction, if any) distance VA was measured monocularly with the Snellen test. Distance and near cover test was conducted to ensure eye alignment was within normative values (distance 2e-2x, near 2e-8x).
Prior to attending the research visit, a questionnaire to assess the parental SES was provided to the parents of the participating children via the schools’ teachers. The parental SES was defined considering their employment status at the time of the study and their educational level. Parents were asked whether they were employed or not (no income) at the time of the study and their educational level was classified as: low education (level 1); primary education (level 2); secondary education (level 3), and higher education, university (level 4).
Statistical analysisThe data from the optometric vision screening and questionnaires were input into a Microsoft Excel (Microsoft Corporation, Washington, USA) spreadsheet and were later exported to JASP v15 (University of Amsterdam, Amsterdam, The Netherlands) for statistical analysis. Prior to the statistical analysis, the distribution of SE was assessed using Shapiro-Wilk test which revealed a non-normal distribution of the SE. Hence, non-parametric statistics were used to investigate the relationship between SE, parental SES and school type. Two different statistical analysis were conducted given that SE could be studied as a categorical as well as a continuous variable, therefore Chi-square and Mann-Whitney tests were used to assess the association between SE (dependent variable) and the other variables studied. A p value of ≤0.05 was considered to be significant for both statistical analyses. The prevalence was finally calculated with a 95 % confidence interval.
ResultsThe study data collection lasted 12 months. A total of 813 children were recruited, but data from 63 children were excluded as their parental questionnaires were not returned. Hence, data from 750 children (mean age 8.3±SD 0.9 years) were included in the analysis (46.5 % males and 53.5 % females; SE ranging from +6.50D to −10.50D (mean 0.27±SD1.15)). Given that there was a high correlation between the SE in the right and left eye (Pearson Correlation coefficient 0.83 p < 0.001), the following data analysis presents the SE of the right eye only.
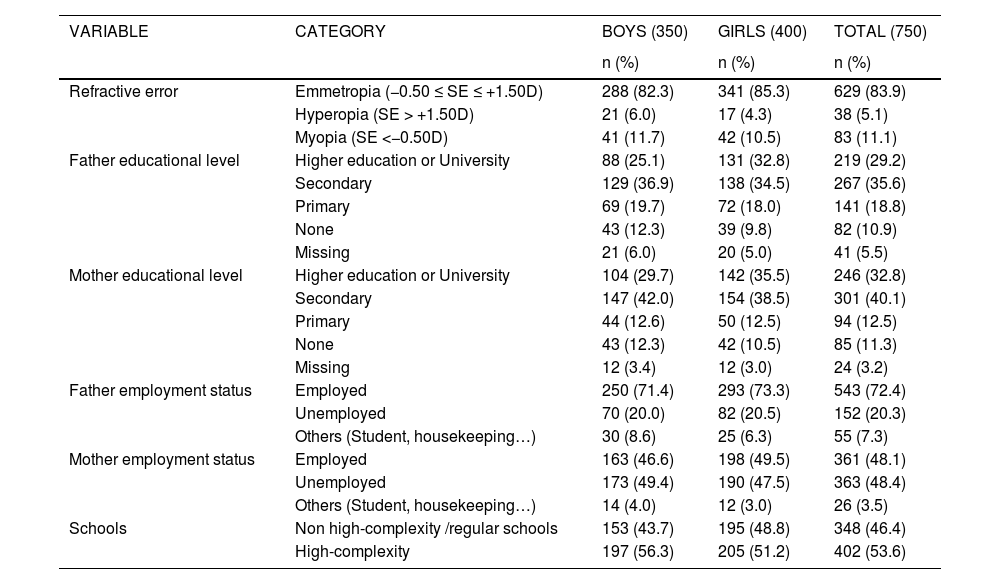
Table 1 presents the distribution of the different variables studied by gender. No significant gender differences were found in the distribution of the refractive error (p > 0.05).
Distribution of the different variables studied by gender.
The prevalence of myopia found in the population sample was of 11.1 % (95 % CI 8.9–13.3) and this was higher than the prevalence of hyperopia (5.1 %; 95 %CI 3.5–6.7) (Fig 1).
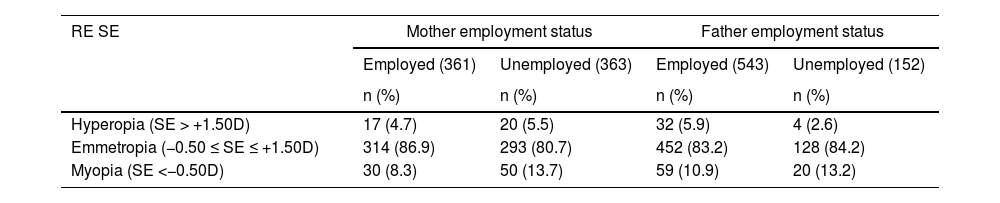
Table 2 presents the distribution of refractive errors in children according to their parental employment status. No differences were observed in the prevalence of refractive error according to the father's employment status, although myopia was slightly more prevalent in children whose fathers were unemployed (13.2 %) than in children whose parents were employed (10.9 %). Similarly, it was also observed that while the distribution of emmetropia was similar between children with different maternal employment status, myopia was more prevalent in children whose mothers were unemployed (13.7 %) than in children whose mothers were employed (8.3 %). Hence, a trend for a higher prevalence of myopia in children whose parents were unemployed was observed. Despite these observations, statistical analysis with chi-squared tests revealed no significant associations between SE or the presence of myopia and maternal (p = 0.051) or paternal employment status (p = 0.223).
Distribution of refractive errors in children according to their parental employment status.
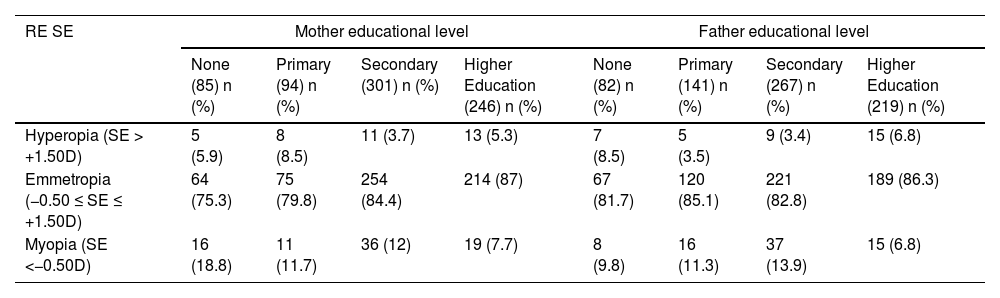
Table 3 presents the distribution of refractive errors in children according to their parental educational level. Although a higher prevalence of myopia in children whose mothers had low educational level was observed, chi-squared tests found no significant associations between SE or the presence of myopia and maternal (p = 0.064) or paternal educational status (p = 0.075).
Distribution of refractive errors in children according to their parental educational level.
To verify that the schools recruited were correctly classified as mainstream regular schools and “high complexity” schools according to the SES definitions, the number of children whose parents were employed and unemployed for each school was counted. It was confirmed that schools with low SES and classified by the local government as “high-complexity” schools comprised the higher proportion of children with unemployed fathers (27.9% vs. 15.0 %) and mothers (60.5% vs. 38.5 %). In addition, schools classified as being of “high complexity” also comprised a higher proportion of children whose parents had low education level. For instance, in “high-complexity” schools 15.4 % of fathers and 16 % of mothers reported to have low education level and this was only the case in 7 % of parents in “non-high complexity”/regular mainstream schools.
Fig 2 shows the prevalence emmetropia, hyperopia and myopia in the population sample considering the school they attended. While the prevalence of emmetropia and hyperopia was similar between schools, a higher prevalence of myopia (2x) was found in “high-complexity” schools compared to “non-high complexity” schools (68.7% vs 31.3 %). Chi-square tests confirmed that the association between “high-complexity” schools and myopic SE was statistically significant (p = 0.014).
DiscussionThe aim of this study was to investigate, for the first time, possible associations between the prevalence of myopia and SES in southern European children.
The prevalence of childhood myopia found in this study is of 11.1 %, and is lower than that recently found in younger children from the same country (20.1 % in children aged 5 to 7 years).9 However, the discrepancy in the prevalence reported in these two studies conducted in the same country is likely to arise from the difference in the population samples. While the recruitment of this study was conducted directly from schools and included all 8-year-old children attending the participating schools, Alvarez-Pelegrina et al.9 recruited child participants aged 5 to 7 years old through a campaign to support children's eye care. It could be argued that the recruitment via such campaign may have included more children with visual symptoms or ocular family history, and indirectly more myopes than a population sample directly recruited from primary schools. The prevalence found in the current study is very similar to that found in a cohort study involving children of similar age (11.5 % in children aged 9 years) in The Netherlands.25 While the recruitment process from both studies is largely different, the sample populations are likely to be similar given the unselected recruited.
While the investigation of SES and childhood refractive error has been studied in some Asian countries, European data are limited. To the authors knowledge, the only study investigating this in Europe showed a higher prevalence of myopia in children from families with low income, low maternal education status, and from non-European ethnicity.23 While no statistically significant associations were found between SE and parental employment, the data of the current study showed that myopia was also more frequently found in children whose mothers were unemployed and had low educational status. Following the same trend, the results obtained from the different schools showed a higher prevalence of childhood myopia in “high-complexity” schools (low SES) than in “non-high complexity” schools. This association was found to be statistically significant. Hence, taken all the study results together, these findings provide further evidence to support that low SES may be associated with a higher likelihood of myopia.
Given the relationship between myopia and education found in the adult population, it may appear surprising that this study findings show a tendency for higher frequency of myopia in children whose mothers were unemployed and had low educational level as well as in children attending “high-complexity” schools (low SES). These results imply that childhood myopia is more prevalent in families with low SES. A plausible explanation for this finding could be linked to the concept of health literacy, and therefore to the abilities that determine the capacity and motivation to access, assess, value, understand, and apply health related information. Health literacy has been shown to be linked to multiples variables including SES.26,27 Following this, individuals with low SES are more likely to experience difficulties to achieve a healthy lifestyle. While there are no studies investigating the impact of SES on visual health literacy level, it is reasonable to suggest that families with low SES have less tools to advise their children to limit the use of electronic devices and spend more time outdoors to reduce the likelihood of myopia development.
It is important to note that the study of SES in child populations is complex, because the variables used to assess SES do refer to their parents/family and not to the children themselves. For instance, to assess the SES of an adult based on their educational level, the number of years and/or hours of education is taken into consideration, and this is directly related to the time of near work conducted individually. In contrast, in the child population, parental educational level is used to assess the child's SES, and this variable does not relate to the number of hours the child spends conducting near work. In fact, all children within the same year group are considered to have the same educational level, and therefore this variable that is gathered from their parents/family does not provide any information about the children near habits. Hence, the study of the relationship between myopia and SES is different between the adult and the child population, and the impact of SES on childhood myopia is less understood.
The main strength of this study is that while the study reported here is cross-sectional, the population sample is the first stage of participants of a cohort study project (CISViT project). Hence, the study aims to become a prospective longitudinal cohort design that follows up a representative population sample of 8-year-olds from southern Europe. Further, this design will allow the research team to continue investigating myopia onset and development in this population and location in future years as well as collecting additional data of interest such as children's visual habits and time outdoors or parental myopia/refractive status by expanding the study questionnaires. In addition, during the course of the study, the vision deficits found in child participants with low SES will be managed accordingly at no cost thanks to “Mirades Solidàries” Project. While this is not a research outcome, it is still important given its public health impact and should also be considered a strength. A study limitation is the use of non-cycloplegic retinoscopy as the method to determine refractive error. While cycloplegia would have been more appropriate to ensure an accurate refractive error measurement and identify pseudomyopias, this was difficult as children attended the research visit in group (together with their entire school group) and the parents were not present during the procedure. It was felt that it was not appropriate to conduct this procedure without the presence of their families and only with the teachers support and supervision.
Given the likely differences in the impact of SES in myopia between adults and children, future studies to further understand refractive error development in school settings with different SES and the possible long-term impact of SES on myopia development are warranted.
We gratefully acknowledge the “Ajuntament de Terrassa”, “Centre Universitari de la Visió”, “Centre de Cooperació per al Desenvolupament de la UPC” and the “Col·legi Oficial d'Optics Optometristes de Catalunya” for their financial and logistic support. Vinuela-Navarro V is funded by “Ministerio de Universidades” and “European Union - NextGenerationEU”. We also want to acknowledge Mestre A, optometrist and teaching associate, as well as the following graduate and postgraduate students for their collaboration with the clinical measurements and analysis: Bonilla, N; Domínguez, L; El Gharbi, M; Fedelich, G; Lacroizette, L; Morera, A; Olives, M.