Preterm birth is associated with an increased risk of abnormal refractive development, even without retinopathy of prematurity (ROP). This study aimed to evaluate the differences in refractive error between preterm infants without ROP and full-term infants, as well as to assess the relationship between physical parameters at birth and refractive status in preterm infants.
MethodsA total of 1205 infants aged 1–18 months participated in this cross-sectional study conducted at Tianjin Women’s and Children’s Health Center in China from March 2020 to September 2023. Following One-to-one propensity score matching (PSM), 230 pairs of infants were included. Refraction was examined by cycloplegic refraction, and the mean spherical equivalent (MSE) of both eyes was analyzed. A simple linear regression model was employed to determine the relationships between refractive state and gestational age (GA), birth weight (BW), and birth length (BL) in preterm infants.
ResultsAmong the 1205 infants, 230 were preterm infants without ROP, and 975 were full-term infants. After PSM, the MSE of preterm infants was lower than that of full-term infants during every period (t = −0.320, P = 0.749). Compared with full-term infants, preterm infants exhibited a significantly higher prevalence of refractive error (P = 0.014), particularly astigmatism (P = 0.040). Although the difference in myopia between the two groups was not significant (P = 0.500), preterm infants had more frequent emmetropia than full-term infants across all stages (P = 0.037). In addition, MSE was negatively correlated with both BW and BL (R2 = 0.260, P < 0.001; R2 = 0.035, P = 0.004); however, there was no correlation between MSE and GA (R2 = 0.048, P = 0.051).
ConclusionsCompared to full-term infants, preterm infants without ROP exhibit lower MSE values and a higher prevalence of refractive errors, particularly astigmatism, and a trend towards developing myopia was observed during early life. BW can be utilized as a parameter to predict the early refractive status of these preterm infants.
Globally, refractive error is an increasingly prevalent disease and a leading cause of visual impairment among children.1–3 Numerous researchers have found that preterm infants are particularly susceptible to refractive errors.4,5 Preterm infants manifest delayed eye development due to their departure from the intrauterine environment. Even in the absence of retinopathy of prematurity (ROP), conditions such as hypoxia, asphyxia, or intrauterine growth retardation may lead to atypical refractive development, resulting in a higher incidence of myopia, astigmatism, and anisometropia compared to healthy children.6,7 Numerous ocular health challenges are also associated with prematurity. An increased incidence of strabismus and amblyopia has also been reported in children born prematurely.8 Population-based studies suggest that ophthalmic impairments remain common in preterm infants, and even this visual impairment can persist into adulthood.9 The increasing risk of refractive error in premterm infants is nowadays urgent to be solved.
Previous studies have demonstrated that physical parameters, such as gestational age (GA), significantly impact the development of biological structures, as well as the development of the refractive states.10–13 Varghese10 suggested that birth weight (BW), rather than GA, should be used as a criterion for screening refractive errors in newborn preterm infants with ROP, especially in developing countries. However, Modrzejewska13 reported no correlation between myopia and either BW or GA among preterm infant without ROP. While most clinical research on refractive error in infancy has focused on preterm babies with varying degrees of ROP, it remains unclear whether prematurity itself contributes to the early development of refractive error.
In this study, we compared the differences in refractive distribution between preterm infants without ROP and full-term infants aged 1–18 months and further evaluated the relationship between refractive state and GA, BW and birth length (BL) in preterm infants.
Materials and methodsStudy populationThis was a cross-sectional study. A total of 1205 children were recruited on a voluntary basis at the Tianjin Women’s and Children’s Health Center from March 2020 to September 2023. The study protocol has been described elsewhere.14 Children with previous congenital cataract, glaucoma, eye tumor, strabismus, or ptosis, and those children who did not cooperate were excluded. Additionally, preterm infants with ROP were excluded to represent the relationship more accurately between refractive error and preterm birth itself, rather than ROP.
Refractive error screening procedureCycloplegic refraction was induced with three drops of tropicamide (1 %) administered 10 min apart. Cycloplegia was then evaluated after an additional 20 min. If a light reflex was still detected, another drop of tropicamide was administered. Refractive error was measured using a Spot Vision Screener ( Welch Allyn Spot, VS100, China). The average of the three measurements was taken as the final result.
Birth parameters and anthropometric measurementsFull-term infants was defined as GA ≥37 weeks and preterm infants as GA <37 weeks. Low birth weight (LBW) defined as BW≤2,500 g.15 The weight of the newborn at birth was measured on an electronic weighing machine accurate up to 10 g (Jinheng, TCS-60, China). Birth length was measured as infantometer accurate to 0.1 cm (Zhengda, SZG-180, China).
Definition of refractive errorRefraction was expressed as mean spherical equivalent (MSE), which was defined as the spherical power plus half of the negative cylinder in the diopter (D) unit. Hyperopia was defined as MSE ≥ +2.00 D, mild hyperopia was defined as +0.50 D ≤MSE ≤+1.75 D, emmetropia as −0.50 D < MSE < +0.50 D, and myopia as MSE ≤ −0.50 D Astigmatism was defined as absolute cylindrical refraction ≥ 1.50 DC, with classifications based on minus cylinder notation. Refractive error was defined as MSE ≥ +2.00 D, MSE ≤ −0.50 D or astigmatism ≥ −1.50 DC.
Statistical analysisPSM analysis was performed in this study with SPSS for Windows, version 26.0 (IBM-SPSS, USA), and conducted with the 1:1 nearest neighbor matching method. The covariates included number of infants by age group, age, gender, BW, BL, type of delivery (normal vaginal birth/cesarean birth), whether singleton or twin pregnancy, parental high myopia, and maternal age at birth.
Statistical analysis was performed using SPSS for Windows, version 26.0 (IBM-SPSS, USA). The Pearson correlation coefficient of MSE from the right eye and the left eye was 0.865. Only the right eye data were presented. The refraction distribution was expressed as mean refraction X‾±SD. A chi-square test or Fisher’s exact test (when the theoretical frequency for 20 % was < 5) was used to compare the prevalence of refractive errors. Analysis of variance (ANOVA) or the Kruskal-Wallis test was used for comparisons between more than two groups. Statistical significance was defined as P < 0.05.
ResultsIn this study, a total of 1205 infants were finally enrolled. Among them, 230 were preterm infants without ROP, consisting of 121 boys (52.6 %) and 109 girls (47.4 %). The GA at birth was 33.59 (±5.82) weeks, and the BW was 2369.82 (±706.47) g. The full-term group consisted of 975 infants, with 489 boys (50.2 %) and 486 girls (49.8 %). The mean GA at birth was 38.52 (±2.70) weeks, and the mean BW was 3313.76 (±588.48) g.
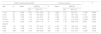
Comparison of general conditions between preterm infants without ROP and full-term infants before PSMWe used preterm infants as the group variable. The number of infants by age group, gender, BW, BL, type of delivery (normal vaginal birth/cesarean birth), whether singleton or twin pregnancy, parental history of high myopia, and maternal age at birth were used as observational covariates. Although there was no significant difference in the proportions of infants across age or gender groups between the two groups before PSM (P = 0.881, P = 0.305, P = 0.503), other variables showed statistically significant differences (all P < 0.05) (Table 1).
Characteristics of the individuals preterm infants without ROP and full-term infants before PSM.
| Parameters | Preterm infants n (%) | Full-term infants n (%) | χ2/Z | P |
|---|---|---|---|---|
| age (month) | 6 (3.0,11.6) | 6 (3.1,11.5) | 0.152 | 0.881a |
| N | 230 (100) | 975 (100) | 4.829 | 0.305 |
| 1–3m | 45 (19.6) | 216 (22.2) | ||
| 3–6m | 52 (22.6) | 189 (35.00) | ||
| 6–9m | 39 (17.0) | 178 (18.3) | ||
| 9–12m | 63 (27.4) | 224 (23.0) | ||
| 12–18m | 31 (13.5) | 168 (17.2) | ||
| Gender | 0.449 | 0.503 | ||
| Boys | 121 (52.6) | 489 (50.2) | ||
| Girls | 109 (47.4) | 486 (49.8) | ||
| BW (g) | 265.531 | <0.001 | ||
| <2,500 | 100 (69.0) | 45 (31.0) | ||
| ≥2,500 | 130 (12.3) | 930 (87.7) | ||
| BL (cm) | 92.80 | <0.001 | ||
| <45 | 51 (57.9) | 37 (42.1) | ||
| ≥45 | 189 (16.7) | 938 (83.3) | ||
| Type of delivery | 30.01 | <0.001 | ||
| Normal birth | 85 (36.9) | 444 (45.5) | ||
| Cesarean | 145 (63.1) | 531 (54.5) | ||
| Twins | 89.95 | <0.001 | ||
| Yes | 53 (23.0) | 80 (4.3) | ||
| No | 177 (77.0) | 895 (95.7) | ||
| Parental high myopia | 4.697 | 0.030 | ||
| Yes | 21 (9.1) | 299 (30.6) | ||
| No | 209 (90.9) | 676 (69.4) | ||
| Maternal age at birth (year) | 10.869 | 0.004 | ||
| ≤25y | 19 (8.3) | 64 (6.6) | ||
| 25–35y | 138 (60.0) | 693 (71.1) | ||
| ≥35y | 73 (31.7) | 218 (22.4) |
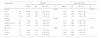
After PSM, 230 pairs were matched, and BW and BL still maintained statistically significant differences between the two groups (P < 0.001, P < 0.001); however, the test statistics were significantly reduced. Other variables showed the same tendency, with the two groups not differing in these indices (all P ≥ 0.05) (Table 2).
Characteristics of the individuals preterm infants without ROP and full-term infants after PSM.
| Parameters | Preterm infantsn (%) | Full-term infantsn (%) | χ2/Z | P |
|---|---|---|---|---|
| age (month) | 6 (3.0,11.6) | 6(3.4,11.1) | 0.201 | 0.840a |
| N | 230 (100) | 230 (100) | 0.267 | 0.992 |
| 1–3m | 45 (51.1) | 43 (48.9) | ||
| 3–6m | 52 (49.1) | 54 (50.9) | ||
| 6–9m | 39 (48.1) | 42 (51.9) | ||
| 9–12m | 63 (51.2) | 60 (48.8) | ||
| 12–18m | 31 (50.0) | 31 (50.0) | ||
| Gender | 0.000 | 1.000 | ||
| Boys | 121 (50.0) | 121 (50.0) | ||
| Girls | 109 (50.0) | 109 (50.0) | ||
| BW(g) | 30.465 | <0.001 | ||
| <2,500 | 100 (69.0) | 45 (19.5) | ||
| ≥2,500 | 130 (12.3) | 185 (80.5) | ||
| BL(cm) | 10.351 | <0.001 | ||
| <45 | 51 (57.9) | 37 (42.1) | ||
| ≥45 | 189 (16.7) | 938 (83.3) | ||
| Type of delivery | 0.291 | 0.587 | ||
| Normal birth | 85 (47.0) | 122 (53.0) | ||
| Cesarean | 145 (57.2) | 108 (42.8) | ||
| Twins | 0.157 | 0.690 | ||
| Yes | 53 (43.8) | 68 (56.2) | ||
| No | 177 (53.7) | 162 (47.7) | ||
| Parental high myopia | 0.803 | 0.370 | ||
| Yes | 21 (50.7) | 20 (49.3) | ||
| No | 209 (49.9) | 210 (50.1) | ||
| Maternal age at birth (year) | 0.442 | 0.800 | ||
| ≤25y | 19 (47.5) | 21 (52.5) | ||
| 25–35y | 138 (52.2) | 126 (47.8) | ||
| ≥35y | 73 (46.8) | 83 (53.2) |
Table 3 shows that after PSM, The initial MSE of infants was +2.82 D in the preterm group and +2.89 D in the full-term group; the final MSEs of the pemterm and full-term groups were +0.83 D and +1.43 D at 18 months, respectively. The MSE of preterm infants was less hypermetropic than that of full-term infants during every period (t = −0.320, P = 0.749). While there were statistically significant differences in the MSE between the two groups at 12–18 months of age (t = 2.283, P = 0.022). There were no significant differences in the MSE between boys and girls (P = 0.856; P = 0.849).
Comparison of refractive distribution of MSE between preterm infants without ROP and full-term infants.
Table 4 provides the overall prevalence of hyperopia, emmetropia, myopia, astigmatism and refractive error for both two groups. Compared to full-term infants, preterm infants without ROP exhibited a significantly higher prevalence of refractive error (69.1 % vs. 79.1 %, P = 0.014).
Comparison of refractive error between preterm infants without ROP and full-term infants.
As the most common refractive error, it can be seen that 26.4 % of preterm infants and 31.2 % of full-term infants was astigmatism in 3 to 6 months age group, which was higher than that in infants aged 12–18 months (7.8 %; 4.3 %, respectively). Astigmatism was more prevalent among preterm infants, this difference is statistically significant after adjustment for age (P = 0.040).
Hyperopia was present in 48.3 % of preterm infants and 40.0 % of full-term infants. The prevalence of mild hyperopia of the preterm and full-term groups were 30.4 % and 38.7 %, respectively. There was no significance difference in hyperopia or mild hyperopia (P = 0.074;P = 0.077).
Meanwhile, considerable more emmetropia took place between 9 and 12 months of age most significance (8.8 %). Compared to full-term infants, emmetropia was more prevalent among preterm infants at each age stage (8.3 % vs. 13.9 %, P = 0.037).
At birth, 3.3 % of the preterm infants had myopia, then higher in those with 9 – 12 months (4.7 %), and again lower in children aged 12–18 months (2.3 %). There was no statistical difference in myopia between the two groups (7.8 % vs. 7.4 %, P = 0.500).
Distribution of refractive of preterm infants without ROP in different GA, BW, and BLTable 5 shows that the MSE and the prevalence of astigmatism decreased as GA, BW, and BL increased in preterm infants without ROP. The MSE among preterm infants with varying BW was statistically significant (P = 0.049).
Distribution of refractive of preterm infants without ROP in different GA, BW, and BL.
Applying simple linear regression analysis (Fig. 1, Fig. 2), MSE showed a negative relationship with BW and BL in preterm infants (R2 = 0.260, P < 0.001; R2 = 0.035, P = 0.004). However, there was no significant correlation between MSE and GA (R2 = 0.048, P = 0.051).
In this study, the predominant refractive state of infants from 1 to 18 months in the two groups was hyperopia, the MSEs of the preterm without ROP and full-term groups were +1.88 D and +1.93 D , respectively. The refractive development patterns of preterm infants without ROP were found to be similar to those of full-term infants. Specifically, the refractive status among those aged 1–18 months reflected that hyperopia transitioned to mild hyperopia with age. As anticipated, the MSE of preterm infants was lower than that of full-term infants across age groups (P = 0.749), this finding is similar to the results of previous studies.16,17
Tian et al.18 reported that by the time full-term children reached emmetropia between ages 0–6 of age, the refractive status of most preterm infants of the same age had developed into myopia. This phenomenon may be attributed to anatomical differences in the eyes of premature, which are characterized by a spherical lens, shallow anterior chamber, and increased corneal curvature.19–21 Al Oum et al.22 conducted a comparative analysis on eyeball shape between preterm infants non-ROP and full-term infant, discovering minor pathologic changes or retinal traction occurred around the retina. They noted early optic nerve ischemia even in the absence of significant ROP, which exerted a detrimental effect on refractive development and emmetropization in these preterm infants. In the present study, a greater proportion of preterm infants without ROP manifested significant emmetropia compared to their full-term counterparts (62.7 % vs. 38.3 %, P = 0.037), it is also possible that the emmetropia was reached earlier in preterm infants than full-term infants. Moreover, the MSE in preterm infants non-ROP was significantly lower than that in full-term infants (P = 0.022) after one year of age. Therefore, preterm infants without ROP may retain potential for "catch-up growth" in refractive development after one year of age, in other words, the preterm group carries the risk of subsequent progression to myopia compared to full-term infants. Our findings, which are supported by those of some previous studies.16,23,24 Further longitudinal studies involving larger participant cohorts are necessary to comprehensively assess the refractive status at various postnatal ages.
Premature departure from the intrauterine environment may impact ocular development, leading to an imbalance in the maturation of various refractive parameters of the eye. Several researchers25–29 have reported a higher prevalence of refractive error in pre-term infants without ROP than that in full-term infants, this was confirmed by this study, in which refractive errors was more common in prematurely born infants than in full-term infants (69.1 % vs. 79.1 %, P = 0.014). The overall prevalence of astigmatism in the preterm group in this study was higher than that in the full-term group (56.1 % vs. 47.4 %, P = 0.040). Deng et al.29 compared ocular morphology between non-ROP preterm infants and mature infants aged 6 – 12months, finding shorter axial length, shallower anterior chamber, and higher curvature of the cornea in the preterm infants groups. Their study may elucidate the reasons for the elevated prevalence of astigmatism and myopia observed in the present study among preterm infants. In other words, premature delivery may serve as a risk factor leading to impaired development of the anterior segment of the eye, which subsequently affects orthokeratological processes and refractive status.23,30 However, preterm infants without ROP and full-term infants were equally likely to have a astigmatism in a previous study.31 Although the exact reasons for such discrepancy remain unclear, we speculate that the different ethnic sample population might be a contributing factor.
Our results showed that the overall prevalence of hyperopia was 48.3 % in preterm infants without ROP, which was lower prevalence than that reported in the study of children in Israel aged 6 months (76.7 %)32 and much higher than that reported by Sherief ST (13.1 %,).33 It is essential to emphasize that we found that the prevalence of hyperopia among children aged 9 to 18 months did not exhibit significant changes. According to Mayer 's34 research, hyperopia in children tends to remain relatively stable after the age of 12 months, which means that for some children, hyperopia does not decrease with age. Morgan35 suggested that mild hyperopia is the natural state of refractive development in children. This has important implications for the follow-up of early childhood hyperopia, since hyperopia in children is at risk of being accompanied by accommodative esotropia.
According to analysis by Fielder et al.,36 three types of myopia are associated with premature birth: (1) physiological and temporary myopia, Fletcher et al.37 and Pennie et al.38 emphasized that this type of myopia is a physiological finding postnatally and after the age of 1 or 2 years, neonatal hyperopia or myopia refractive error rapidly decreases and turn into emmetropia; (2) myopia without ROP, often rather high and static, the possibility of a shift from the myopia of prematurity towards a more ordinary childhood myopia type, this also implies a potential of progression; (3) myopia induced by severe ROP, numerous previous literatures confirm this result.39–42 Xie et al.39 in their study of preterm infants followed to the age of 8 years, myopia frequency was 7.69 % (5/65) in normal eyes, 18.18 % (20/10) in eyes that had shown non-ROP, and 27.66 % (13/47) in the subgroup with more marked ROP. In the present study, preterm infants with ROP were excluded. Preterm infants without ROP infants did not demonstrate a greater inclination toward myopia compared to their full-term infants counterparts (7.4 % vs.7.8 % P = 0.500). In addition, it is worth noting that reduction of hyperopia in preterm group could signal incidient earlier emmetropia or myopia. Some studies43,44 confirmed that a higher prevalence of myopia in prematurely born children without ROP than in those born at term by the time they reached school age.
The early refractive status of preterm infants is influenced by various factors, including GA, BW, corneal curvature, and axial length. Wood45 investigated the significant differences in ocular optical components between preterm infants and full-term infants, aiming to elucidate the disparities in refractive status from a biological perspective. The authors also identified that the refractive status of preterm infants was associated with physical parameters at birth. In 2009, Varghese10 enrolled 599 one-week-old infants for ophthalmologic examinations, their linear regression analysis determined that a positive correlation between the refractive status of preterm infants and both GA and BW; however, no relationship was found with BL or head circumference at birth. In this study, we assessed the refractive distribution among preterm infants with varying GA, BW, and BL. Notably, we observed statistically significant differences in MSE among preterm infants categorized by different BW; specifically, MSE decreased as BW increased (P = 0.049). Further linear regression analysis revealed that BW exhibited a negative correlation with MSE (R2= 26.01 %, P< 0.001), indicating that higher birth weights were associated with lower MSE. While we share a similar perspective with Varghese, who proposed that BW rather than gestational age (GA) should be considered as a criterion for screening refractive errors, it is important to note that BW was negatively correlated with MSE. Additionally, although BL also exhibited a negative correlation with MSE, the association was weak (R² = 3.54 %). Therefore, we conclude that BW is one of the most reliable physical parameters at birth reflecting the refractive status of infants aged 1–18 months.
There was no evidence supporting a significant correlation between MSE and GA in preterm infants without ROP (P = 0.227), which might have been related to the relatively high mean GA of our preterm babies. This found contrasts sharply with earlier studies which one eye size in preterm infants tends to be smaller with lower GA, one might expect a higher MSE in younger preterm infants.17 Additionally, an increase in axial length in preterm infants did not compensate for diminution in corneal curvature and lens refraction and tended to cause myopia and astigmatism.46,46 The disparities between our findings and those reported in the literature may stem from the fact that this study excluded preterm infants with ROP, as well as differences in GA and BW thresholds used for grouping, along with variations in the age at examination. We hypothesize that while GA is associated with early refractive status in preterm infants postnatally, this relationship may not persist as age increases, however, further validation through additional experiments is necessary.
Some potential limitations of the present study should be noted. First, we administered tropicamide (1 %) to achieve an adequate level of cycloplegia prior to conducting the Spot Vision Screener examination. While cyclopentolate (0.5 %) and atropine (0.5 %) are more potent cycloplegic agents compared to tropicamide (1 %), they are associated with a higher incidence of systemic and local adverse effects due to their muscarinic antagonist properties; for instance, there is an increased risk of gastric atony. Therefore, in consideration of patient safety, we opted for tropicamide in this study. Notably, no residual accommodation was observed during our investigation. Second, despite employing PSM analysis, inconsistencies and bias may still exist. Our data were collected from preterm infants without ROP, but some of these infants might have had undetected mild or regressed ROP that went unnoticed by clinicians. Finally, larger studies are warranted to further explore the impact of prematurity based on corrected GA, BW, and BL.
ConclusionsCompared to full-term infants, preterm infants without ROP exhibit lower MSE values and a higher prevalence of refractive errors, particularly astigmatism, and a trend towards developing myopia was observed during early life. BW can be used as a parameter to predict the early refractive status of these preterm infants. We recommend that clinicians conduct screenings for refractive conditions in preterm infants and pay close attention to neonates with low birth weight.
Author contributionsHL contributed to the design and conduct of the study, data collection and management, results interpretation, and writing the whole paper; JXY contributed to data collection and management of the study; LCM participated in the study design. All authors read and approved the final manuscript.
The authors have no conflicts of interest to declare.
Ethics approval and consent to participate The study adhered to the tenets of the Declaration of Helsinki and was approved by the Human Research Ethics Committee of Tianjin Medical University Eye Hospital, Tianjin Women’s and Children’s Health Center (Date:March 1, 2020/NO.hsy-2020030101).