To investigate which baseline factors are predictive for success in controlling myopia progression in a group of children wearing MiSight Contact Lens (CLs).
MethodsMyopic patients (n=41) fitted with MiSight CLs and followed up two years were included in this study. Bivariate analysis, a logistic regression analysis (LG) and a decision tree (DT) approach were used to screen for the factors influencing the success of the treatment. To assess the response, axial length (AL) changes were considered as main variable. Patients were classified based on a specific range of change of axial length at the end of each year of treatment as “responders” (R) (AL change <0.11mm/per year) and “non-responders” (NR) (AL change ≥0.11mm/per year).
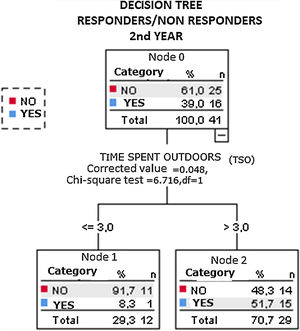
ResultsOf a total of forty-one Caucasian patients treated with MiSight CLs, 21 and 16 were considered responders in the first and the second year of follow-up, respectively. LG analysis showed that the only factor associated with smaller axial length growth was more time spent outdoors (p=0.0079) in the first year of treatment. The decision tree analysis showed that in the responding group spending more than 3 and 4h outdoors per week was associated with the best response in the first year and in the second year of treatment respectively.
ConclusionsThe LR and the DT approach of this pilot study identifies time spent outdoors as a main factor in controlling axial eye growth in children treated with MiSight CLs.
There is evidence that, in addition to genetics,1–3 there are environmental factors4 that play an important role in the onset of myopia, such as time spent outdoors,5,6 prolonged higher education,7,8 occupational and socioeconomic status, and sustained near vision.9–11 Once myopia has started in a child, the rate of progression is estimated to be around −1D average per year in East Asians and around −0.5D per year in Caucasians. 12,13
There is also strong evidence that myopia progression can be significantly reduced by a range of interventions, the most effective being the use of atropine, 14–19 followed by orthokeratology (OK)20–23 and peripheral defocus modifying CLs.24–30 Despite the good results reported for these treatments, not all study participants responded in the same way. Some children show progressive myopia despite treatment. Also, researchers and clinicians dedicated to methods to control the progression of the myopia, such as orthokeratology or peripheral defocus modifying soft contact lenses, had observed that the response to these different treatments is not equally effective in all the children. Some of the participants responded in a very positive way to the treatment and others did not so much. This fact has been also noticed in daily clinical practice. It would be useful to identify factors that contribute to the predictability of the response of subjects wearing different methods to control the progression of the myopia. The number of possible factors related to myopia progression represents a challenge to interpret all this data in a different way. The aim of this study was to investigate the risk factors in children who presented with myopia progression despite treatment with MiSight CLs, and in this regard we analyzed the predictive factors related to the best response to treatment. MiSight CL is a soft (hydrophilic) CL with a concentric design. It contains a large central correction zone surrounded by a series of treatment and correction concentric zones of alternating distant and near powers, which together produce two focal planes. The optical power of the correction zones corrects the refractive error while the treatment zones produce 2.00 diopters (D) of simultaneous myopic retinal defocus during both distance and near viewing, maintaining good visual acuity.29
We carried out a bivariate and logistic regression analysis and a decision tree (DT) approach to establish the main factors involved in the response to treatment with MiSight CLs. Decision trees consist of nodes that specify a particular attribute of the data, branches that represent a test of each attribute value, and leaves that correspond to the terminal decision of class assignment for an instance in the data set. DT models are emerging as reliable and effective analytical tools to screen a large number of variables linked to a condition, and to identify specific variables that indicate predicting factors of a condition [31]. The computer-generated model is represented in tree structure form, which provides easily interpretable and accurate predictions.32
To the authors’ knowledge, this is the first study to assess the main factors involved in the response to the treatment with MiSight CLs. In this sense we report pilot data on predicting factors for success wearing MiSight CLs.
MethodsThis study is part of the MiSight® Assessment Study Spain (MASS) that was designed to assess the efficacy of MiSight® CLs versus distance single vision (SV) spectacles in myopic children. The goal of the present study was to investigate which parameters may be considered as predictive factor of success in terms of response or not to the myopic progression. The protocol adhered to the tenets of the Declaration of Helsinki and was approved by the CEI-R (Regional Research Ethics Committee of the Community of Madrid, Spain). After receiving an explanation of the nature and possible consequences of the study, informed consent was obtained from all individual participants. The clinical trial was registered in Clinical Trials (ClinicalTrials.gov Identifier: NCT01917110). Eligibility criteria, methods and results can be consulted in previous publications.29 The study group (MiSight CLs), at the Baseline visit, 12 and 24 follow-up visits, underwent a full clinical history, anterior and posterior segment examination, binocular and accommodative function assessment, refractive evaluation, and measurement of ocular and corneal aberrations. Progression of myopia was defined as the magnitude of change in the spherical equivalent refractive error and as the change in axial length relative to baseline.29 Binocular and accommodative procedures can be consulted in a previous article.30 The wavefront evaluation was measured and collected by the same examiner using the I-Profiler plus (Carl Zeiss) without any optical compensation, in a dark room to guarantee wide pupil sizes. Therefore, the subjects from study group were instructed to remove CLs 30min before the evaluation and were instructed to fix the apparatus stimulus (that was the image of a balloon), while the infrared light beam generate a point of light in subject´s retina, then the light will cross the optic system of the subject’s eye between retina and corneal surface generating a wavefront captured by a Hartmann Shack sensor. The quadratic value of all aberrations (RMS) was registered, also the average of quadratic value of high order (HO_RMS) and low order (LO_RMS) aberrations at ocular and corneal level, in microns. Total and corneal spherical aberration (SA) also was obtained.
At each visit the subject and the subject’s parent/guardian were asked to fill out a questionnaire designed to collect information related to time spent outdoors (TSO), time spent on near work (TN), and time spent playing sports (TS).
In order to carry out an analysis of the possible predicting factors for success of the MiSight CLs in controlling myopia progression, the subjects of the study group, MiSight CLs users, were divided into two subgroups: responders (R) and non-responders (NR) in the first and in the second year of treatment. To assess response to treatment to the CLs, we considered the growth of axial length each year of contact lens wear less than 0.11mm. “Responders” (R) were defined as being those subjects with an axial elongation of less than 0.11 the first year and 0.22mm after two years of follow-up, and “non-responders” (NR) as those subjects with an axial elongation of 0.11mm the first year and 0.22mm or more after two years of follow-up. The value of 0.22 was chosen according to the MASS study29 where, to calculate the sample size, it was considered 0.22mm as the axial length change during two years of follow-up, so this value will be the cut-off point to divide subjects into responders versus non-responders.
Statistical analysisBivariate analysisAll measurements were expressed as mean and standard deviation. A total of 22 independent variables: age at the initiation of MiSight CLS, ocular and visual parameters (axial length; anterior chamber depth; equivalent spherical error; J0 and J45 vector values; mean keratometry; far and near visual acuity; distance and near phoria; stereopsis; stimulus AC/A ratio; accommodative response; low and high ocular and corneal RMS; ocular and corneal spherical aberration); time spent outdoors per week, time spent on near work per week and time spent playing sports per week, were included in a bivariate analysis in order to find statistically significant differences on a p<0.05 of the three period time evaluated (baseline, 12th and 24th months). A dichotomic qualitative variable was named as “responder (R)” or “non-responder(N)” based on the previously described axial length increase criteria. The paired sample t test was used for comparison within the groups. This variable was considered as the dependent variable for the Decision Tree Approach and Logistic Regression Analyses.
Decision tree approachA Chi square Automatic Interaction Detection (CHIAD) analysis works based on the minimum p value found was used to develop the DT. The Automatic Analysis works identifying the factor with strongest association with the dependent variable, and build the tree structure with the first node, that divide into two branches until the next best variable is reached. The CHIAD algorithm continues with the third most important variable and again divides the node into two branches. The sequence stops when no remaining independent variable could yield a statistically significant difference (p<0.05) or when no further split could be made due to the stooping rules defined previously. For each of the nodes generated, the DT analysis computed the probabilities of the risk expressed as percentages.31,32 All the variables included in the bivariate analysis that were statistically significant based on a p<0.05 level constituted the DT analysis.
Logistic regression analysisAll the variables included in the bivariate analysis that were statistically significant based on a p<0.05 level constituted also the database used in a Logistic Regression model to assess the factors associated to the dependent variable. The regression analysis model used the stepwise method. Inclusion criteria α≤0.15, elimination criteria β≥0.05 and step back screening p<0.05 were regarded as meaningful in the statistical analysis. The same statistical analysis was performed for two periods of time: baseline vs. 12 and baseline vs. 24 months.
IBM SPSS Statistics for Windows, Version 22 (IBM Corp. Release 2013, Armonk, NY, USA) and SAS software, version 9.4 (SAS Institute, Inc., Cary, NC, USA) were used for decision tree and logistic regression analyses respectively.
ResultsThe first year of treatment, twenty (49%) children were classified as responders (axial length increase less than 0.11mm) and twenty-one (51%) as non-responders (axial length increase greater than or equal to 0.11mm). And the second year sixteen children (39 %) were responders and twenty- five children (61 %) non-responders.
A post hoc analysis of the sample size of this pilot study showed that taking a statistical power of 0.90 and assuming a standard deviation of the change in axial length over a 2-year period of 0.10mm, a sample size of 8 subjects per group was needed to detect a difference in axial length variation equal to 0.22mm at P=0.05.
Bivariate analysis of response effectBivariate analysis showed that the responding group in the first year of treatment was associated with worse near visual acuity, distance horizontal phoria with more endophoric values, more time spent outdoors TSO and more time spent playing sports and in the second year of treatment with less myopia and better distance visual acuity. Responders had a mean myopic progression of -0.23 D and an axial elongation of 0.13mm over the two-year period of treatment and non-responders had a mean myopic progression of -0.6 D and an axial elongation of 0.38mm over the two-year period of treatment. Table 1 includes the two subgroups formed in this study: responders and non-responders in the first and in the second year of wearing MiSight CLs and show average values for demographic and visual parameters (Table 1A), binocular and accommodative data (Table 1B), time spent outdoors, playing sports and near work per week (Table 1C) and corneal and ocular wavefront data (Table 1D) of these subgroups at baseline, 12-month and 24-month follow-up visits.
Demographic and visual parameter for responders and non-responders.
| Parameter | Baseline(mean±SD) | P value | 1st Yearfollow-upn= (R:20, N:21)(mean±SD) | P value | 2nd YearFollow-upn= (R:16, N:25)(mean±SD) | P value | |
|---|---|---|---|---|---|---|---|
| Age (years) | R | 11.41±1.18 | 0.8901 | ||||
| N | 10.75±1.22 | ||||||
| Axial length (mm) | R | 24.05±0.54 | 0.7731 | 24.01±0.50 | 0.3902 | 24.18±0.53 | 0.1007 |
| N | 24.11±0.57 | 24.16±0.60 | 24.49±0.61 | ||||
| Anterior chamber (mm) | R | 3.77±0.22 | 0.9622 | 3.76±0.21 | 0.9340 | 3.80±0.25 | 0.9898 |
| N | 3.76±0.16 | 3.77±0.17 | 3.80±0.15 | ||||
| Spherical equivalent (D) | R | −1.91±0.95 | 0.1787 | −1.87±0.88 | 0.0620 | −2.14±1.13 | 0.0441* |
| N | −2.31±0.92 | −2.42±0.93 | −2.91±1.17 | ||||
| Mean keratometry (D) | R | 44.28±1.22 | 0.8486 | 44.31±1.15 | 0.7050 | 44.24±1.22 | 0.9018 |
| N | 44.21±1.29 | 44.17±1.36 | 44.19±1.26 | ||||
| J0 | R | 0.05±0.17 | 0.6778 | 0.07±0.18 | 0.7169 | 0.10±0.19 | 0.6505 |
| N | 0.08±0.19 | 0.062±0.18 | 0.12±0.18 | ||||
| J45 | R | 0.01±0.04 | 0.5986 | −0.007±0.09 | 0.8090 | −0.003±0.08 | 0.4574 |
| N | −0.04±0.15 | −0.03±0.15 | −0.03±0.12 | ||||
| BCDVA (LogMar) | R | −0.06±0.07 | 0.8085 | −0.05±0.06 | 0.3607 | −0.10±0.04 | 0.0300* |
| N | −0.06±0.05 | −0.07±0.05 | −0.06±0.05 | ||||
| BCNVA (LogMar) | R | 0.04± 0.08 | 0.0023* | 0.02±0.08 | 0.0068* | −0.02±0.03 | 0.4253 |
| N | −0.04±0.04 | −0.03±0.04 | 0.00±0.03 | ||||
R: responders, N: non-responders.
1st year: responders and non-responders in the first year of follow-up.
2nd year: responders and non-responders in the second year of follow-up.
D: diopters; J0 and J45 vectorial components for astigmatism; BCDVA: Monocular Best-corrected distance visual acuity measured in LogMar notation; BCNAV: Best-corrected near visual acuity measured in LogMar notation.
Binocular and accommodative data for responders and non- responders.
| Parameter | Baseline(mean±SD) | P value | 1st Yearfollow-upn= (R:20, N:21)(mean±SD) | P value | 2nd Yearfollow-upn= (R:20, N:21)(mean±SD) | P value | |
|---|---|---|---|---|---|---|---|
| Distance horizontal phoria (Δ) ** | R | 0.25±1.00 | 0.0689 | 0.20±0.89 | 0.0482* | 0±0 | 0.1703 |
| N | −0.56±1.58 | −0.67±1.71 | −0.42±1.44 | ||||
| NPC break (cm) | R | 3.25±2.37 | 0.8321 | 2.83±2.35 | 0.7594 | 3.67±3.39 | 0.6455 |
| N | 3.49±4.13 | 3.94±4.34 | 3.17±3.28 | ||||
| NPC recovery (cm) | R | 6.04±4.05 | 0.7753 | 5.37±4.18 | 0.7899 | 5.69±5.22 | 0.4036 |
| N | 6.61±8.55 | 7.36±9.03 | 4.37±4.62 | ||||
| Near horizontal phoria (Δ)** | R | 1.19±2.17 | 0.4253 | 1.45±3.10 | 0.1458 | 0±0.75 | 0.3815 |
| N | 0.04±4.97 | −0.43±4.78 | −0.84±4.61 | ||||
| Stereopsis (sec. of arc) | R | 31.56±12.21 | 0.2839 | 30.00±11.35 | 0.7073 | 32.00±14.24 | 0.9493 |
| N | 29.40±12.19 | 30.48±13.03 | 31.60±25.24 | ||||
| AC/A Ratio | R | 6.22±0.74 | 0.7731 | 6.32±1.19 | 0.2673 | 6.01±0.34 | 0.4562 |
| N | 5.94±1.81 | 5.80±1.71 | 5.74±1.73 | ||||
| Amplitude of accommodation (D) | R | 13.35±3.56 | 0.4552 | 13.65±3.31 | 0.6936 | 13.98±2.19 | 0.0945 |
| N | 14.22±3.63 | 14.10±3.89 | 12.40±3.10 | ||||
| Accommodative response 33cm (D) | R | 1.16±0.48 | 0.4800 | 1.10±0.46 | 0.8449 | 0.90±0.70 | 0.7878 |
| N | 1.02±0.68 | 1.06±0.73 | 0.83±0.72 | ||||
| Accommodative response 25cm (D) | R | 1.25±0.62 | 0.9122 | 1.2±0.60 | 0.8762 | 1.06±0.50 | 0.5679 |
| N | 1.23±0.69 | 1.26±0.72 | 1.17±0.63 | ||||
| Accommodative response 20cm (D) | R | 1.39±0.63 | 0.6694 | 1.32±0.59 | 0.8881 | 1.20±0.62 | 0.4115 |
| N | 1.30±0.65 | 1.35±0.69 | 1.38±0.70 |
R: responders, N: non-responders.
1st year: responders and non-responders in the first year of follow-up.
2nd year: responders and non-responders in the second year of follow-up.
NPC: near point of convergence, AC/A Ratio: accommodative convergence/accommodation ratio.
Time spent outdoors, playing sports and near work per week for responders and non-responders.
| Parameter | Baseline(mean±SD) | P value | 1st Yearfollow-upn= (R:20, N:21)(mean±SD) | P value | 2nd Yearfollow-upn= (R:20, N:21)(mean±SD) | P value | |
|---|---|---|---|---|---|---|---|
| Time spent outdoors TSO (hours) per week | R | 4.94±0.93 | 0.0162* | 4.90±1.12 | 0.0035* | 3.25±2.51 | 0.1520 |
| N | 3.68±1.70 | 3.48±1.63 | 4.56±1.76 | ||||
| Time spent playing sports (hours) per week | R | 8.59±4.73 | 0.0197* | 14.75±4.69 | 0.3994 | 5.83±3.64 | 0.7200 |
| N | 5.50±3.41 | 16.05±5.04 | 5.39±3.34 | ||||
| Time spent on near work (hours) per week | R | 14.44±4.44 | 0.3088 | 8.15±4.88 | 0.0305* | 16.50±5.85 | 0.4390 |
| N | 16.04±5.09 | 5.34±2.94 | 17.91±4.62 |
R: responders, N: non-responders.
1st year: responders and non-responders in the first year of follow-up.
2nd year: responders and non-responders in the second year of follow-up.
Corneal and ocular wavefront data for responders and non-responders.
| Parameter | Baseline(mean±SD) | P value | 1st Yearfollow-upn= (R:20, N:21)(mean±SD) | P value | 2nd Yearfollow-upn= (R:20, N:21)(mean±SD) | P value | |
|---|---|---|---|---|---|---|---|
| Pupil diameter (mm) | R | 5.75±0.41 | 0.8364 | 5.90±0.7 0 | 0.2803 | 5.87±0.51 | 0.6066 |
| N | 5.74±0.85 | 5.59±0.70 | 5.98±0.74 | ||||
| Total RMS (μm) | R | 2.36±1.01 | 0.2727 | 2.28±0.97 | 0.0740 | 2.67±1.08 | 0.2429 |
| N | 2.73±1.00 | 2.86±0.98 | 3.12±1.15 | ||||
| Total Low order RMS (μm) | R | 2.35±1.01 | 0.2739 | 2.27±0.97 | 0.0749 | 2.66±1.08 | 0.2497 |
| N | 2.71±1.00 | 2.85±0.99 | 3.10±1.15 | ||||
| Total High order RMS (μm) | R | 0.19±0.09 | 0.1889 | 0.19±0.09 | 0.0315* | 0.19±0.07 | 0.4796 |
| N | 0.24±0.11 | 0.25±0.11 | 0.21±0.078 | ||||
| Corneal RMS (μm) | R | 0.63±0.29 | 0.2720 | 0.63±0.27 | 0.1987 | 0.73±0.24 | 0.3987 |
| N | 0.76±0.39 | 0.78±0.41 | 0.82±0.37 | ||||
| Corneal Low order RMS (μm) | R | 0.56±0.33 | 0.3867 | 0.57±0.30 | 0.3757 | 0.69±0.24 | 0.4613 |
| N | 0.65±0.31 | 0.66±0.33 | 0.76±0.30 | ||||
| Corneal High order RMS (μm) | R | 0.23±0.05 | 0.2425 | 0.22±0.05 | 0.0364* | 0.22±0.05 | 0.2219 |
| N | 0.31±0.32 | 0.33±0.34 | 0.29±0.25 | ||||
| Total Spherical Aberration (μm) | R | 0.04±0.05 | 0.0760 | 0.03±0.05 | 0.0102* | 0.06±0.06 | 0.9283 |
| N | 0.08±0.08 | 0.09±0.08 | 0.06±0.10 | ||||
| Corneal Spherical Aberration (μm) | R | 0.10±0.04 | 0.0385* | 0.11±0.03 | 0.0319* | 0.12±0.03 | 0.4865 |
| N | 0.13±0.03 | 0.13±0.03 | 0.11±0.06 |
R: responders, N: non-responders.
1st year: responders and non-responders in the first year of follow-up.
2nd year: responders and non-responders in the second year of follow-up.
RMS: root mean square.
According to the LR analysis, only the time spend outdoors (TSO) during the first period of time (baseline vs. 12 month) is the independent variable with effect on the axial length growth (p=0.0079, ODD ratio=2.11 and AUC of the ROC curve of 0.7619) (Table 2).
Logistic regression analysis. Odds Ratio Estimates.
| Parameter | Standard Estimate | Wald Error | Chi-Square | Pr>ChiSq | Odds Ratio Estimate | 95% Wald confidence limits |
|---|---|---|---|---|---|---|
| Time Spent Outoors (TSO) | 0.7465 | 0.2810 | 7.0544 | 0.0079* | 2.11 | 1.216- 3.659 |
According to the model the log of the odds of a child to be “responder” to the treatment was positive related to “time spend outdoors” (p>0.05). In fact, the odd of child to be responder per unit of the variable is 2.110 greater than those children who do not spend time outdoors.
The inferential Goodness of fit test is the Hosmer–Lemeshow (H–L) test that yielded a DF4 of 3.9156 and was non-significant (p=0.4175), suggesting that the model was fit to the data well. In other words, the null hypothesis of a good model fit to data is tenable.
Decision treeThe DT resulting from Automatic Interaction Detection analysis is displayed in Figs. 1 and 2. DT results are relative to baseline factors. Fig. 1 has a dept of three levels from the root node and there is only one node. 49% of the patients (n=20) treated with MiSight CLs were responders according to the criteria. In these patients, the treatment was more effective in those who spent more than four hours a week outdoors and were more myopic than −2. 6D. Fig. 2 has a depth of two levels from the root node and there is a total of two nodes. 39% of patients (n=16) were responders. In these patients, the treatment was more effective in those who spent more than three hours a week outdoors (51.7% of responders). The decision tree analysis showed that in the “responding group” spending more than 3h outdoors per week was associated with the best response in the first year and spending more than 4h in the second year of treatment. Both Figs. (1 and 2) show time spent outdoors being a protection factor.
DiscussionThe MASS study29 confirmed that wearing MiSight CLS results in a significant reduction of myopia and axial length in children from 8 to 12 years old, compared with children wearing single vision spectacles. However, not all children had the same amount of response to the CLs treatment.
There are different ways to argue about the response to a treatment of myopia control. Previous reports use the terms “progressors” or “non-progressors”,17,18 “poor responders”,19 while other authors talk about “good or bad response” or “success” or “failure” in the treatment.16 All authors refer to the amount of response to the different treatments. Shih et al. defined17 progressors as those who had had an increase of >1D/year after an atropine treatment with different doses, while Loh K et al.18 defined progressors as those with myopia progression of more than 0.50D at 1year in the atropine-treated eye. Similarly, Wu et al.19 referred to poor responders to 0.05% atropine as those whose myopia continued progressing by >0.5D over 6 months, and Diaz-Llopis et al.,16 in their study with 0.01% atropine, defined “success” as an average progression of less than 0.25D per year, and “failure” as an average annual progression of more than -0.50D per year.
In addition to these studies, other authors such as Kong33 and Wang34 have studied the factors influencing the therapeutic effect of orthokeratology on controlling juvenile myopia progression. Both studies used axial length growth as primary outcome.
In the same way, we have also chosen axial elongation as the main variable to divide subjects into responders or non-responders, because it is generally accepted that axial elongation is the primary ocular component in myopia progression and its stabilization.35,36
Although some studies17–19,33,34 have analyzed the factors that influence a better or worse response for the control of myopia, to the best of our knowledge there are no previous studies that analyze the factors that can influence the success of soft peripheral defocus modifying CLs.
In the Atom 1 analysis,18 compared with non-progressors, progressors were younger (8.5±1.4 years vs. 9.3±1.5years; P=0.023), started to wear spectacles at a younger age (6.7±1.2 years vs. 7.3±1.5years; P=0.066), had two myopic parents and were more myopic at baseline (−3.6±1.3 D vs.−2.8±1.4 D; P=0.015). In our study, although responders and non-responders did not have significant differences in the amount of myopia at baseline, responders became less myopic at the end of 2 years of wearing MiSight CLs, as it was expected since axial length and amount of myopia are the two variables that determine the progression of myopia.
Kong Q et al.,33 showed that the factors related with the efficacy of the OK treatment were shorter myopia time, smaller diopter and corneal curvature, high proportion of overnight wear and longer wearing times among others. However, Wang B et al.34 showed that the factors associated with smaller axial length growth were older age at the onset of OK lens wear (p<0.0001) and greater baseline spherical equivalent myopic refractive error (p=0.0046). As can be seen in Table 1A, in our study at baseline responders and non-responders did not show significant differences in age, nor in the amount of myopia and axial length.
In relation with the time spent outdoors, there are no studies with contact lenses for myopia control that show data in this regard. The Atom 1 didn´t find any significant differences between the progressors and the non-progressors (6.1±4.1h per week vs. 5.9±4.9h per week; P=0.877), while our results of the bivariate and the Regression Analysis show that responders spent more time outdoors at baseline and in the first year of treatment.
Although both groups had good distance and near visual acuity, it seems that the responders had worse near visual acuity in the first year of follow-up and better distance visual acuity than non-responders at the end of the treatment. These differences in the visual acuity are modest and clinically non-significant. It is well within the normal test-retest variability in visual acuity testing and hence cannot be considered a real difference.
Here, we report pilot data on the predictive factors of success of MiSight CLs in controlling the progression of myopia. Our decision tree results show that time spent outdoors could be a protective factor for success wearing MiSight CLs, three or four hours per week being the cutoff in the first and in the second year of treatment respectively. There is strong evidence of a link between less time spent outdoors and myopia onset,7,37–40 but it is not clear if time spent outdoors is associated with myopia progression, a few studies having reached different conclusions. In the Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error Study,41 time spent outdoors was not associated with less myopia progression. This finding agrees with the results of the meta-analysis carried out by Xiong S et al.,42 whose pooled results demonstrated that outdoor time was not effective in slowing progression in eyes that were already myopic. In contrast, other studies found an increase in myopia progression associated with less time spent outdoors43,44 and, similarly, Read SA et al.45 suggested that children who had experienced less than 40min’ exposure to bright light per day had more axial eye growth. In the same way, our results of the Decision Tree show that spending more than 180min outdoors per a week could be associated with those children who responded better to the treatment with MiSight CLs, although these data should be confirmed with studies with larger sample sizes. Another important consideration is that there are no previous studies that analyze whether outdoor time is a predictor of success in the progression of myopia in children treated with contact lens for myopia control.
Previous studies40,46,47 have shown other factors that could be related to the progression of myopia in addition to time spent outdoors, such as accommodation, binocular vision, pupillary diameter and aberrations. Our results do not show significant differences in any of the accommodative measures between the group of responders and non-responders, in any of the statistical analyzes performed. Pupil diameter and aberrations are also related to myopia control methods. There is evidence that there is a negative correlation between pupil diameter and increased LAX in children treated with orthokeratology. Santodomingo-Rubido et al.47 showed that children with larger pupils have less myopia progression than those with smaller pupils, but our results did not find that pupil diameter could be a factor related to treatment success. In relation with aberrations, only the bivariate analysis (Table 1D) showed significant differences between responders and non-responders, being the responding group associated with less corneal high order aberration and less corneal and total spherical aberration in the first year of treatment. Despite these differences, the results of the two groups, measured without CLs, are within the values considered normal,48,49 so we do not consider it clinically relevant.
To date, several studies about myopia control have used regression analysis to describe the association between risk factors and the progression using adjusted odds ratio.33,34 In contrast, a DT approach has not been yet used. DT models are playing an increasingly important role in healthcare,31,32,50,51 one advantage being their ability to describe associations in the data by revealing important interactions among variables.31
Our results can be considered as a pilot study due to the sample itself is not large. In this sense, the results of the decision tree can indicate that there could be a required threshold of time spent outdoors in children treated with MiSight CLs in order to slow their axial eye growth.
To define more precisely this threshold of time spent outdoors, it would be necessary to carry out additional research with larger samples of children wearing MiSight CLs and longer follow-up periods. Proposed strategies could involve a combination of wearing MiSight CLs with increased outdoor time.
ConclusionsThe LR analysis and DT approach identifies time spent outdoors as a main factor in controlling axial eye growth in children treated with MiSight CLs. Our results can contribute to better and more appropriate advice about spending more time outdoors. Time spent outdoors is not only a risk factor involved in myopia onset, but also could be a risk factor for controlling myopia progression with MiSight CLs treatment.
Conflict of interestThe authors have no conflicts of interest to declare.
FundingCooperVision S.L. provided the study contact lenses and the funding to carry out the clinical trial (MASS Study) but had no role in the design of the research nor the analysis of the results.
The authors would like to thank Peter Bonney for proofreading the article.