To identify independent risk factors for myopia onset in schoolchildren, with a focus on binocular visual function.
MethodsWe conducted a school-based prospective cohort study in Wenzhou, China. Schoolchildren in grades 2 and 3 were recruited in 2014 and followed until graduation at grade 6. Myopia was defined as a spherical equivalent refraction (SER) of ≤ -0.50 diopters. The risk factors assessed included monocular uncorrected visual acuity (UCVA), axial length (AL), corneal refractive power (CR), demographic characteristics, daily activities, parental myopia, parental education level, and routine clinical binocular visual function parameters such as phoria, accommodation, and convergence-related metrics.
ResultsMultivariable logistic regression analysis revealed that children with the following baseline characteristics had a significantly increased risk (OR;95% CI) of developing myopia before graduation: female sex (3.03;1.99–4.62;P<.001), having two myopic parents (2.36;1.29–4.31;P=.005), worse UCVA (19.99;2.24–178.44;P=.007), more negative SER values (0.15;0.07–0.31;P<.001), longer AL (7.28;4.30–12.31;P<.001), larger CR (2.20;1.75–2.76;P<.001), and lower magnitude of positive relative accommodation (PRA) (1.11;1.02–1.22;P=.02). Additional exploratory subgroup analyses indicated that the association between PRA and myopia incident remained consistent across various demographic characteristics (P-interaction>0.05). Receiver operating characteristic curves (AUC; 95% CI) demonstrated that PRA (0.59;0.55–0.63) exhibited predictive capability comparable to key ocular biometric parameters such as AL (0.57;0.53–0.62) and CR (0.58;0.53–0.62).
ConclusionsThe current study identifies PRA as a stable, independent risk factor for myopia onset, with predictive capability comparable to key ocular biometric parameters. This finding can be utilized in future studies to enhance the accuracy of myopia prediction and assist in making informed decisions regarding myopia interventions.
In recent decades, there has been a significant global increase in the severity of myopia among schoolchildren, particularly in East and Southeast Asia, where the condition has reached epidemic proportions.1–3 In China, the annual incidence of myopia among schoolchildren has been reported to range from 6.3 % to 31.7 %.4–11 Myopia and high myopia can lead to permanent pathological changes and result in both direct healthcare expenditures and indirect costs such as lost productivity and reduced quality of life.12–16 Therefore, a thorough investigation of risk factors for myopia is crucial for developing effective interventions in children, especially before the onset of myopia.
Several prospective cohort studies have evaluated potential independent risk factors for myopia onset among primary schoolchildren. These studies identified risk factors including age, sex, residential area, parental myopia, daily activities, refractive error, and ocular biometric parameters such as axial length (AL) and corneal refractive power.6–9,17–21 Routine clinical examinations typically include assessments of binocular vision to optimize visual clarity and minimize asthenopia, which should be managed if necessary. However, evidence regarding the role of binocular vision in myopia development and progression remains limited.22 In 1988, Goss et al. conducted a 3-year cohort study involving 87 emmetropic schoolchildren aged 8.5 to 14.3 years in the USA.23–24 Based on univariable analysis, they found that binocular visual function parameters such as positive relative accommodation (PRA), accommodative convergence to accommodation (AC/A) ratio, near lateral heterophoria, and near fusional vergence range might be informative for predicting myopia onset. However, it remains unclear whether these parameters remain significant after adjusting for confounders. Our previous report indicated that PRA could be a potential predictor of myopia onset over a relatively short follow-up period of 2 years,25 but this observation requires verification over a longer follow-up period. Such information would be valuable for enhancing the accuracy of myopia prediction in the future.
Thus, the aim of this study was to identify independent risk factors for myopia onset, with a focus on exploring various binocular visual function parameters, and to evaluate their potential value in predicting the occurrence of myopia.
MethodsStudy design and populationThe Wenzhou Medical University Essilor Progression and Onset of Myopia (WEPrOM) study was a school-based prospective cohort study conducted in Wenzhou, an eastern city in China. The study was approved by the ethics committee of the Eye Hospital of Wenzhou Medical University (KYK [2013]34) and adhered to the tenets of the Declaration of Helsinki.
The study involved two elementary schools in Wenzhou, one situated in the urban city center and the other in a rural area. During the baseline visit in November 2014, all 1118 s- and third-grade students were invited to participate, with 1103 (98.7 %) attending. We chose these two grades to focus on the critical ages for myopia onset while maximizing recruitment efficiency and follow-up rates. Of the 1103 screened children, 30 (2.7 %) were excluded due to reported histories of ocular diseases affecting vision, such as strabismus, amblyopia, or congenital glaucoma. Consequently, 1073 schoolchildren were enrolled in the study. Follow-up visits were conducted annually until graduation at grade 6, except for the last two visits, which were delayed by six months due to a severe flu outbreak and the subsequent winter vacation. Written informed consent was obtained from the parents of all participants.
Measurements and outcomesTrained investigators conducted comprehensive standardized ocular examinations at both schools using equipment calibrated at the start of each visit. Detailed descriptions of the measurement methods and outcomes are provided in the eMethods section of the Supplement. Specifically, we measured monocular uncorrected visual acuity (UCVA) and non-cycloplegic subjective refractive error for both eyes, as well as AL and corneal refractive power (CR) in the right eye. Routine clinical binocular visual function parameters were also assessed, including near lateral heterophoria, AC/A ratio, negative relative accommodation (NRA), PRA, and the base-in (BI) and base-out (BO) break points of horizontal fusional convergence range at near. Prior to each ocular examination, questionnaires were distributed to parents to collect data on demographic characteristics (age, gender, school, and grade), daily activities (average time spent on near work and outdoor activities per day), parental myopia status (parental myopia, parental early-onset myopia [<12 years old], and parental high myopia), and parental educational attainment (both paternal and maternal). Refractive errors were calculated as spherical equivalent refraction (SER), defined as the sphere power plus half of the cylindrical power. Myopia was defined as an SER ≤ −0.50 diopters (D) and further classified into low myopia (−3.00 D < SER ≤ −0.50 D), moderate myopia (−6.00 D < SER ≤ −3.00 D), and high myopia (SER ≤ −6.00 D).7,26–27
Statistical analysisThe right eye was selected for data analysis due to the high correlation in SER between the left and right eyes at each visit (Pearson correlation coefficient > 0.85, P < .001 for all visits; see eTable 1 in the Supplement). Paired t-tests and McNemar tests were utilized for comparisons. To examine factors associated with myopia onset before primary school graduation, we conducted multivariable logistic regression analysis on participants who did not have myopia at baseline. Variables with P-values < 0.10 in the univariable analysis were included as potential confounders. We also adjusted for grade because follow-up durations differed between baseline grade 2 and grade 3 participants. Additionally, exploratory subgroup analyses were performed for significant parameters related to binocular visual functions.28 To investigate possible modifications on the association between these parameters and myopia onset, we included demographic interaction terms in the logistic regression model and presented the results in a forest plot. P values for interaction were evaluated using interaction terms and likelihood ratio tests. To assess the predictive ability of factors associated with myopia onset before graduation, receiver operating characteristic (ROC) curves were plotted, and area under the curve (AUC) values were calculated. Statistical analyses were conducted using Stata/MP version 15.1 (Stata Corp LLC, TX, USA) and RStudio version 1.3 (The R Foundation for Statistical Computing, Vienna, Austria). Two-sided P values < 0.05 were considered statistically significant.
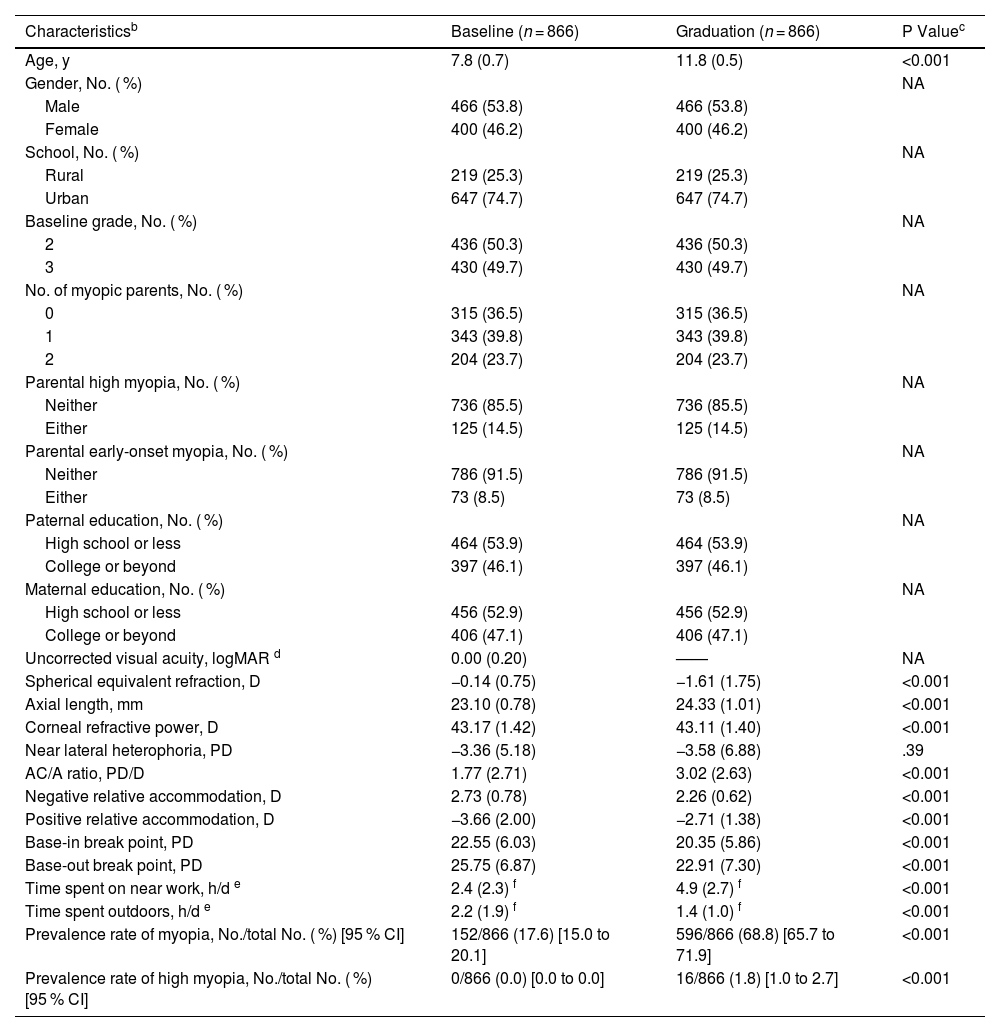
ResultsAfter excluding 207 schoolchildren who were lost to follow-up due to reasons such as school transfer, absence from examinations, or the use of orthokeratology lenses or atropine, a total of 866 participants (mean [SD] baseline age: 7.8 [0.7] years; 400 [46.2 %] female) with complete refraction data were included in the analysis. The characteristics of these 866 participants were compared between their baseline and graduation visits (Table 1). Compared to the baseline visit, significant increases were observed in age, AL, AC/A ratio, and time spent on near work; moreover, SER values became significantly more negative. However, at the graduation visit, there were significant decreases in CR, the magnitude of NRA and PRA, BI break point, BO break point, and time spent outdoors.
Characteristics of the Included Participants at Baseline and Graduation Visitsa.
| Characteristicsb | Baseline (n = 866) | Graduation (n = 866) | P Valuec |
|---|---|---|---|
| Age, y | 7.8 (0.7) | 11.8 (0.5) | <0.001 |
| Gender, No. ( %) | NA | ||
| Male | 466 (53.8) | 466 (53.8) | |
| Female | 400 (46.2) | 400 (46.2) | |
| School, No. ( %) | NA | ||
| Rural | 219 (25.3) | 219 (25.3) | |
| Urban | 647 (74.7) | 647 (74.7) | |
| Baseline grade, No. ( %) | NA | ||
| 2 | 436 (50.3) | 436 (50.3) | |
| 3 | 430 (49.7) | 430 (49.7) | |
| No. of myopic parents, No. ( %) | NA | ||
| 0 | 315 (36.5) | 315 (36.5) | |
| 1 | 343 (39.8) | 343 (39.8) | |
| 2 | 204 (23.7) | 204 (23.7) | |
| Parental high myopia, No. ( %) | NA | ||
| Neither | 736 (85.5) | 736 (85.5) | |
| Either | 125 (14.5) | 125 (14.5) | |
| Parental early-onset myopia, No. ( %) | NA | ||
| Neither | 786 (91.5) | 786 (91.5) | |
| Either | 73 (8.5) | 73 (8.5) | |
| Paternal education, No. ( %) | NA | ||
| High school or less | 464 (53.9) | 464 (53.9) | |
| College or beyond | 397 (46.1) | 397 (46.1) | |
| Maternal education, No. ( %) | NA | ||
| High school or less | 456 (52.9) | 456 (52.9) | |
| College or beyond | 406 (47.1) | 406 (47.1) | |
| Uncorrected visual acuity, logMAR d | 0.00 (0.20) | —— | NA |
| Spherical equivalent refraction, D | −0.14 (0.75) | −1.61 (1.75) | <0.001 |
| Axial length, mm | 23.10 (0.78) | 24.33 (1.01) | <0.001 |
| Corneal refractive power, D | 43.17 (1.42) | 43.11 (1.40) | <0.001 |
| Near lateral heterophoria, PD | −3.36 (5.18) | −3.58 (6.88) | .39 |
| AC/A ratio, PD/D | 1.77 (2.71) | 3.02 (2.63) | <0.001 |
| Negative relative accommodation, D | 2.73 (0.78) | 2.26 (0.62) | <0.001 |
| Positive relative accommodation, D | −3.66 (2.00) | −2.71 (1.38) | <0.001 |
| Base-in break point, PD | 22.55 (6.03) | 20.35 (5.86) | <0.001 |
| Base-out break point, PD | 25.75 (6.87) | 22.91 (7.30) | <0.001 |
| Time spent on near work, h/d e | 2.4 (2.3) f | 4.9 (2.7) f | <0.001 |
| Time spent outdoors, h/d e | 2.2 (1.9) f | 1.4 (1.0) f | <0.001 |
| Prevalence rate of myopia, No./total No. ( %) [95 % CI] | 152/866 (17.6) [15.0 to 20.1] | 596/866 (68.8) [65.7 to 71.9] | <0.001 |
| Prevalence rate of high myopia, No./total No. ( %) [95 % CI] | 0/866 (0.0) [0.0 to 0.0] | 16/866 (1.8) [1.0 to 2.7] | <0.001 |
Abbreviations: y, age in years; NA, not applicable; logMAR, logarithm of the minimum angle of resolution; D, diopter; PD, prism diopter; AC/A, accommodative convergence to accommodation; PD/D, prism diopter per diopter; h/d, hours per day; CI, confidence interval.
Data involved in the baseline visit were obtained in 2014 when children were in grade 2 or grade 3. Data from the graduation visit were collected in 2018 and 2019 successively when children were all in grade 6.
Uncorrected visual acuity was not evaluated among some myopic participants during follow-up visits; therefore, only baseline data are presented to avoid bias from non-random missing data.
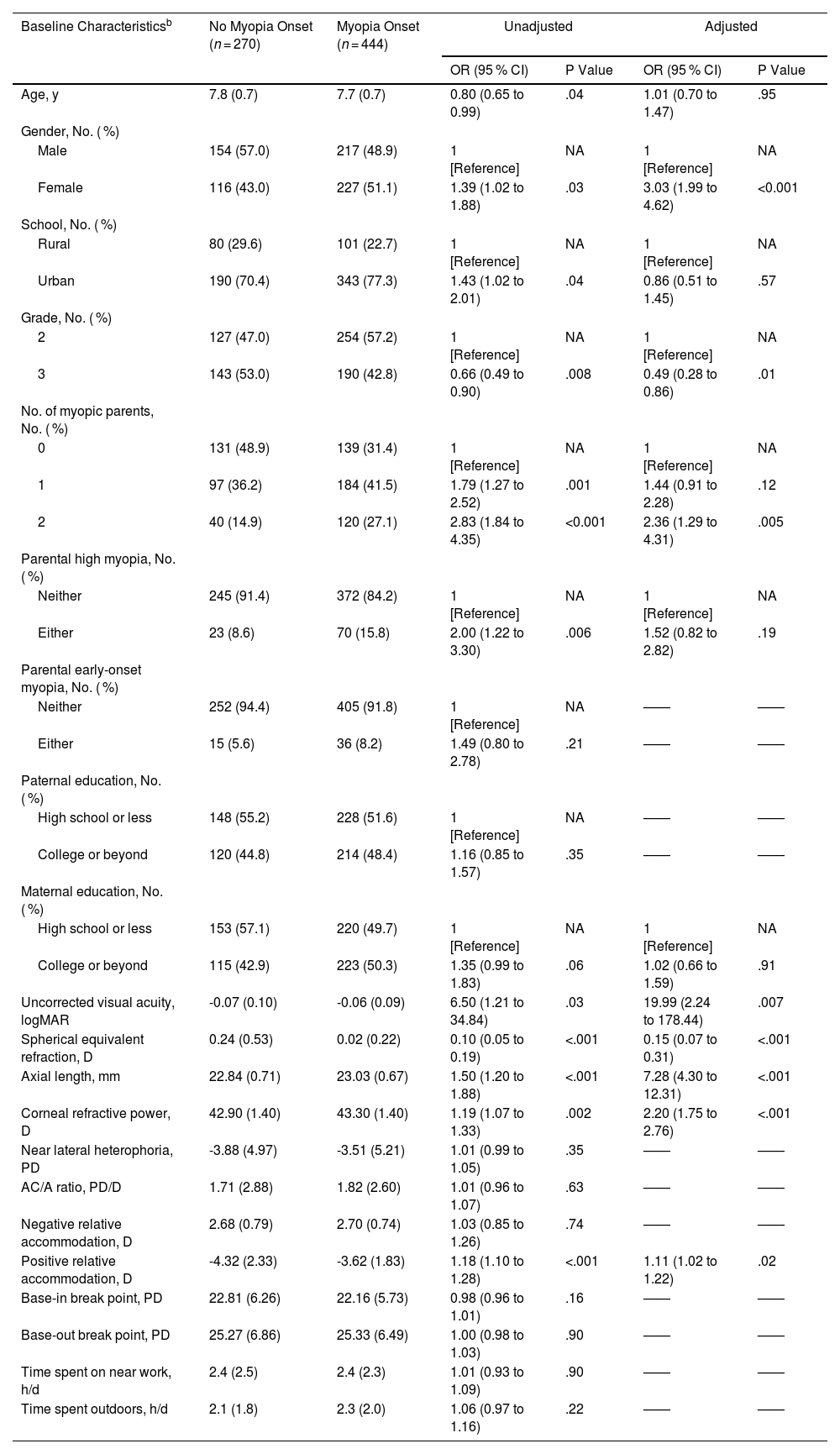
Among the 714 participants without myopia at baseline, 444 (62.2 %) developed myopia before graduation. After adjusting for confounders including baseline grade, children with the following baseline characteristics had a greater risk of myopia onset (Table 2): female sex (odds ratio [OR] = 3.03; P < .001), having two myopic parents (OR = 2.36; P = .005; compared to no myopic parents), worse UCVA (OR = 19.99; P = .007), more negative SER (OR = 0.15; P < .001), longer AL (OR = 7.28; P < .001), larger CR (OR = 2.20; P < .001), and lower magnitude of PRA (OR = 1.11; P = .02).
Multivariable Logistic Regression Analysis of Factors Associated with Myopia Onset before Graduationa.
| Baseline Characteristicsb | No Myopia Onset (n = 270) | Myopia Onset (n = 444) | Unadjusted | Adjusted | ||
|---|---|---|---|---|---|---|
| OR (95 % CI) | P Value | OR (95 % CI) | P Value | |||
| Age, y | 7.8 (0.7) | 7.7 (0.7) | 0.80 (0.65 to 0.99) | .04 | 1.01 (0.70 to 1.47) | .95 |
| Gender, No. ( %) | ||||||
| Male | 154 (57.0) | 217 (48.9) | 1 [Reference] | NA | 1 [Reference] | NA |
| Female | 116 (43.0) | 227 (51.1) | 1.39 (1.02 to 1.88) | .03 | 3.03 (1.99 to 4.62) | <0.001 |
| School, No. ( %) | ||||||
| Rural | 80 (29.6) | 101 (22.7) | 1 [Reference] | NA | 1 [Reference] | NA |
| Urban | 190 (70.4) | 343 (77.3) | 1.43 (1.02 to 2.01) | .04 | 0.86 (0.51 to 1.45) | .57 |
| Grade, No. ( %) | ||||||
| 2 | 127 (47.0) | 254 (57.2) | 1 [Reference] | NA | 1 [Reference] | NA |
| 3 | 143 (53.0) | 190 (42.8) | 0.66 (0.49 to 0.90) | .008 | 0.49 (0.28 to 0.86) | .01 |
| No. of myopic parents, No. ( %) | ||||||
| 0 | 131 (48.9) | 139 (31.4) | 1 [Reference] | NA | 1 [Reference] | NA |
| 1 | 97 (36.2) | 184 (41.5) | 1.79 (1.27 to 2.52) | .001 | 1.44 (0.91 to 2.28) | .12 |
| 2 | 40 (14.9) | 120 (27.1) | 2.83 (1.84 to 4.35) | <0.001 | 2.36 (1.29 to 4.31) | .005 |
| Parental high myopia, No. ( %) | ||||||
| Neither | 245 (91.4) | 372 (84.2) | 1 [Reference] | NA | 1 [Reference] | NA |
| Either | 23 (8.6) | 70 (15.8) | 2.00 (1.22 to 3.30) | .006 | 1.52 (0.82 to 2.82) | .19 |
| Parental early-onset myopia, No. ( %) | ||||||
| Neither | 252 (94.4) | 405 (91.8) | 1 [Reference] | NA | —— | —— |
| Either | 15 (5.6) | 36 (8.2) | 1.49 (0.80 to 2.78) | .21 | —— | —— |
| Paternal education, No. ( %) | ||||||
| High school or less | 148 (55.2) | 228 (51.6) | 1 [Reference] | NA | —— | —— |
| College or beyond | 120 (44.8) | 214 (48.4) | 1.16 (0.85 to 1.57) | .35 | —— | —— |
| Maternal education, No. ( %) | ||||||
| High school or less | 153 (57.1) | 220 (49.7) | 1 [Reference] | NA | 1 [Reference] | NA |
| College or beyond | 115 (42.9) | 223 (50.3) | 1.35 (0.99 to 1.83) | .06 | 1.02 (0.66 to 1.59) | .91 |
| Uncorrected visual acuity, logMAR | -0.07 (0.10) | -0.06 (0.09) | 6.50 (1.21 to 34.84) | .03 | 19.99 (2.24 to 178.44) | .007 |
| Spherical equivalent refraction, D | 0.24 (0.53) | 0.02 (0.22) | 0.10 (0.05 to 0.19) | <.001 | 0.15 (0.07 to 0.31) | <.001 |
| Axial length, mm | 22.84 (0.71) | 23.03 (0.67) | 1.50 (1.20 to 1.88) | <.001 | 7.28 (4.30 to 12.31) | <.001 |
| Corneal refractive power, D | 42.90 (1.40) | 43.30 (1.40) | 1.19 (1.07 to 1.33) | .002 | 2.20 (1.75 to 2.76) | <.001 |
| Near lateral heterophoria, PD | -3.88 (4.97) | -3.51 (5.21) | 1.01 (0.99 to 1.05) | .35 | —— | —— |
| AC/A ratio, PD/D | 1.71 (2.88) | 1.82 (2.60) | 1.01 (0.96 to 1.07) | .63 | —— | —— |
| Negative relative accommodation, D | 2.68 (0.79) | 2.70 (0.74) | 1.03 (0.85 to 1.26) | .74 | —— | —— |
| Positive relative accommodation, D | -4.32 (2.33) | -3.62 (1.83) | 1.18 (1.10 to 1.28) | <.001 | 1.11 (1.02 to 1.22) | .02 |
| Base-in break point, PD | 22.81 (6.26) | 22.16 (5.73) | 0.98 (0.96 to 1.01) | .16 | —— | —— |
| Base-out break point, PD | 25.27 (6.86) | 25.33 (6.49) | 1.00 (0.98 to 1.03) | .90 | —— | —— |
| Time spent on near work, h/d | 2.4 (2.5) | 2.4 (2.3) | 1.01 (0.93 to 1.09) | .90 | —— | —— |
| Time spent outdoors, h/d | 2.1 (1.8) | 2.3 (2.0) | 1.06 (0.97 to 1.16) | .22 | —— | —— |
Abbreviations: OR, odds ratio; CI, confidence interval; y, age in years; NA, not applicable; logMAR, logarithm of the minimum angle of resolution; D, diopter; PD, prism diopter; AC/A, accommodative convergence to accommodation; PD/D, prism diopter per diopter; h/d, hours per day.
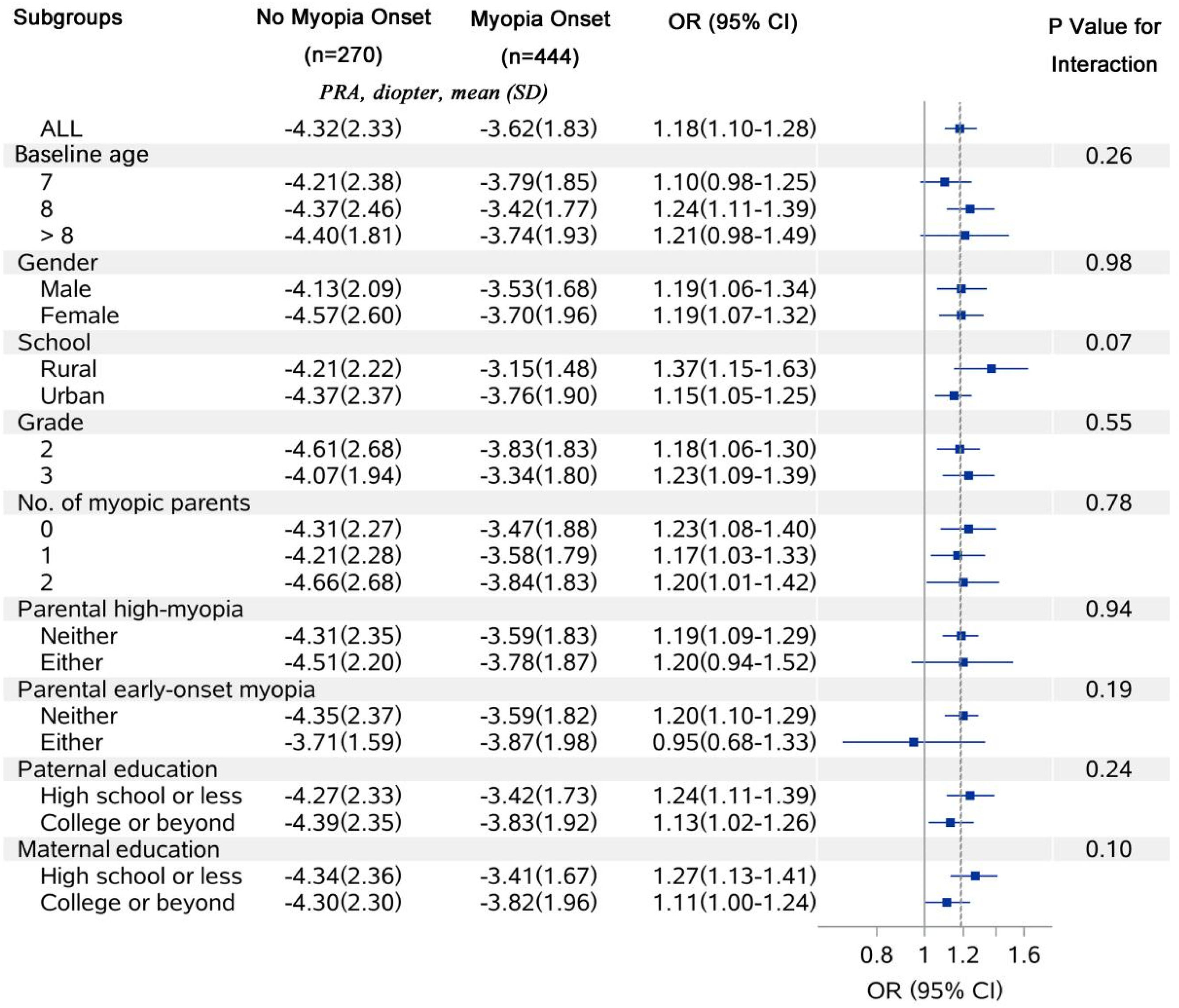
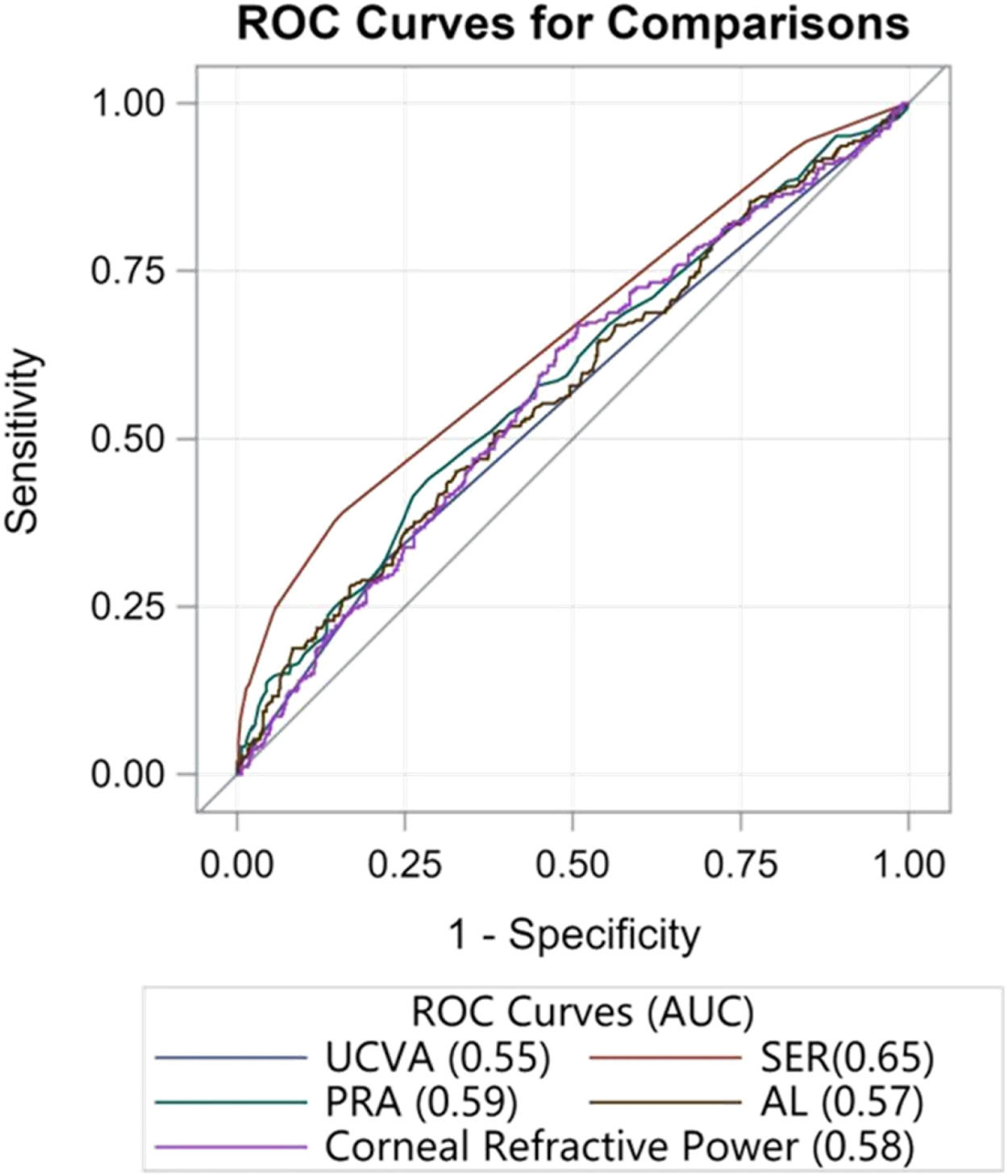
The correlation between baseline PRA and myopia onset before graduation remained consistent across all demographic subgroups (P-interaction > 0.05 for all; Figure 1). Consequently, the association between PRA and myopia onset did not exhibit significant variability. The ROC curves indicated that PRA had a moderate predictive capability for myopia onset before graduation, with an AUC of 0.59 (95 % CI: 0.55 to 0.63), which was less effective compared to SER (AUC = 0.65; 95 % CI: 0.61 to 0.69) but comparable to AL (AUC = 0.57; 95 % CI: 0.53 to 0.62) and CR (AUC = 0.58; 95 % CI: 0.53 to 0.62; Figure 2).
Receiver Operating Characteristic Curves of Risk Factors for Predicting Myopia Onset before Primary School Graduation. Abbreviations: ROC, receiver operating characteristic; AUC, area under the curve; UCVA, uncorrected visual acuity; SER, spherical equivalent refraction; PRA, positive relative accommodation; AL, axial length.
Our data revealed that myopia onset before elementary school graduation was associated with sex, parental myopia, UCVA, SER values, AL, CR, and notably, the magnitude of PRA at baseline. The association between PRA and myopia onset remained robust across various demographic characteristics. Moreover, PRA demonstrated a predictive capability comparable to key ocular biometric parameters such as AL and CR.
Consistent with prior studies, we found that female sex,7,17 having two myopic parents,8–9,17–18,21 more myopic refractive error,6–7,9,19,21 longer AL,20–21 and larger corneal refractive power21 at baseline were independently associated with myopia onset before primary school graduation. In our study, the myopia incidence did not differ significantly between rural and urban schools after multivariable adjustment. This finding contrasts with the one-year result reported in Taipei but aligns with the 4-year follow-up findings in Beijing.9,29 Such consistency may be attributable to urbanization driven by China's rapid economic development. Contrary to previous reports,17,19 age was not independently associated with myopia onset in our study, potentially due to the narrow age range of participants. Outdoor activities and near work were significantly associated with myopia onset in some studies,9,18,21 but not consistently across all studies.6,8 Notably, the lack of a significant association between outdoor activities and near work with myopia onset has been predominantly observed in studies involving Chinese children, consistent with our findings. This phenomenon may be explained by the increased time spent on near work, reduced outdoor exposure, and limited variability in environmental factors resulting from intense academic competition among Chinese students.
We identified that a lower magnitude of baseline PRA served as an independent risk factor for myopia onset. Our findings align with the 1996 study by Goss and colleagues, which reported that individuals who developed myopia exhibited a lower magnitude of PRA.23 This implies that a diminished capacity to sustain accommodative effort under prolonged binocular near-viewing conditions may be linked to myopia onset, potentially mediated through hyperopic retinal defocus.30–31 Notably, subgroup analyses revealed a consistent association between reduced PRA and myopia onset across various demographic and familial factors, including age, gender, school, grade, parental myopia status, and parental educational attainment. These results underscore the stability of PRA as a risk factor for myopia onset and highlight its importance in myopia prediction models and future investigative efforts.
As one of the pioneering studies investigating the independent association between binocular visual functions and myopia, our study possesses several unique strengths, including a large sample size, a relatively long follow-up period, and a high follow-up rate (4.5-year follow-up rate of 80.7 %). Nevertheless, this study also has certain limitations that warrant consideration. First, refraction measurements were conducted without cycloplegia, which might lead to an overestimation of myopic refractive error. However, we employed subjective refraction, utilizing a working lens of +2.00 D following retinoscopy performed by an experienced ophthalmologist. Compared with non-cycloplegic autorefraction, this method minimizes the impact of accommodation while maintaining operational efficiency and enhancing examination compliance. Furthermore, it facilitates the assessment of binocular visual functions, demonstrating practical value in large-scale epidemiological studies. Second, some questionnaire data were incomplete (baseline missing data: 32.8 % for near work; 23.0 % for outdoor activities). Considering the potential recall bias inherent in questionnaire-based assessments and discrepancies between reports from parents and children,32 future studies should incorporate objective and portable wearable devices to improve data accuracy.33
ConclusionsIn conclusion, this school-based 4.5-year cohort study conducted in Wenzhou initially identifies PRA as a stable and independent risk factor for myopia onset prior to elementary school graduation, with predictive capability comparable to key ocular biometric parameters. This finding can inform future studies to enhance the accuracy of myopia prediction, thereby assisting eye care professionals and health administrators in making more informed decisions before implementing interventions in children.
FundingThis work was supported by the Scientific Research Project of Zhejiang Provincial Department of Education [grant number Y202457210], the International S&T Cooperation Program of China [grant number 2014DFA30940], and the Wenzhou Medical University-Essilor International Research Center [WEIRC, grant numbers 95013006, 95016010]. The funders had no role in the conceptualization, design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Consent for publicationParental written informed consent were obtained from all enrolled participants.
Availability of data and materialsThe datasets generated and/or analysed during the current study are not publicly available due to privacy or ethical restrictions but are available from the corresponding author on reasonable request.
Author contributionsAll authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Drs. Yee Ling Wong, and Björn Drobe are employees of Essilor International, Singapore. No honorarium, grant, or other form of payment was given to anyone to produce the manuscript. The authors have no other potential conflicts of interest to disclose.
Not applicable.