To analyze the differences in induced multifocality after LASIK surgery in myopic and hyperopic patients using conventional and aberration-free profiles.
SettingAugenlaserzentrum, Recklinghausen, Germany.
MethodsWe retrospectively evaluated four consecutive groups of 280 eyes treated by the ESIRIS laser platform: Group A myopic with conventional treatment (70 eyes), group B myopic with aspheric treatment (70 eyes), group C hyperopic eyes treated with conventional LASIK (70 eyes) and group D hyperopic eyes treated with aspheric profile (70 eyes). We used in all the cases the ESIRIS SCHWIND Laser Platform and the Carriazo Pendular Microkeratome. The Optikon Keratron Topographer obtained the measurement of change in corneal refractive power of the anterior surface at 3, 5, and 7mm meridionally and in the form of corneal wavefront analysis.
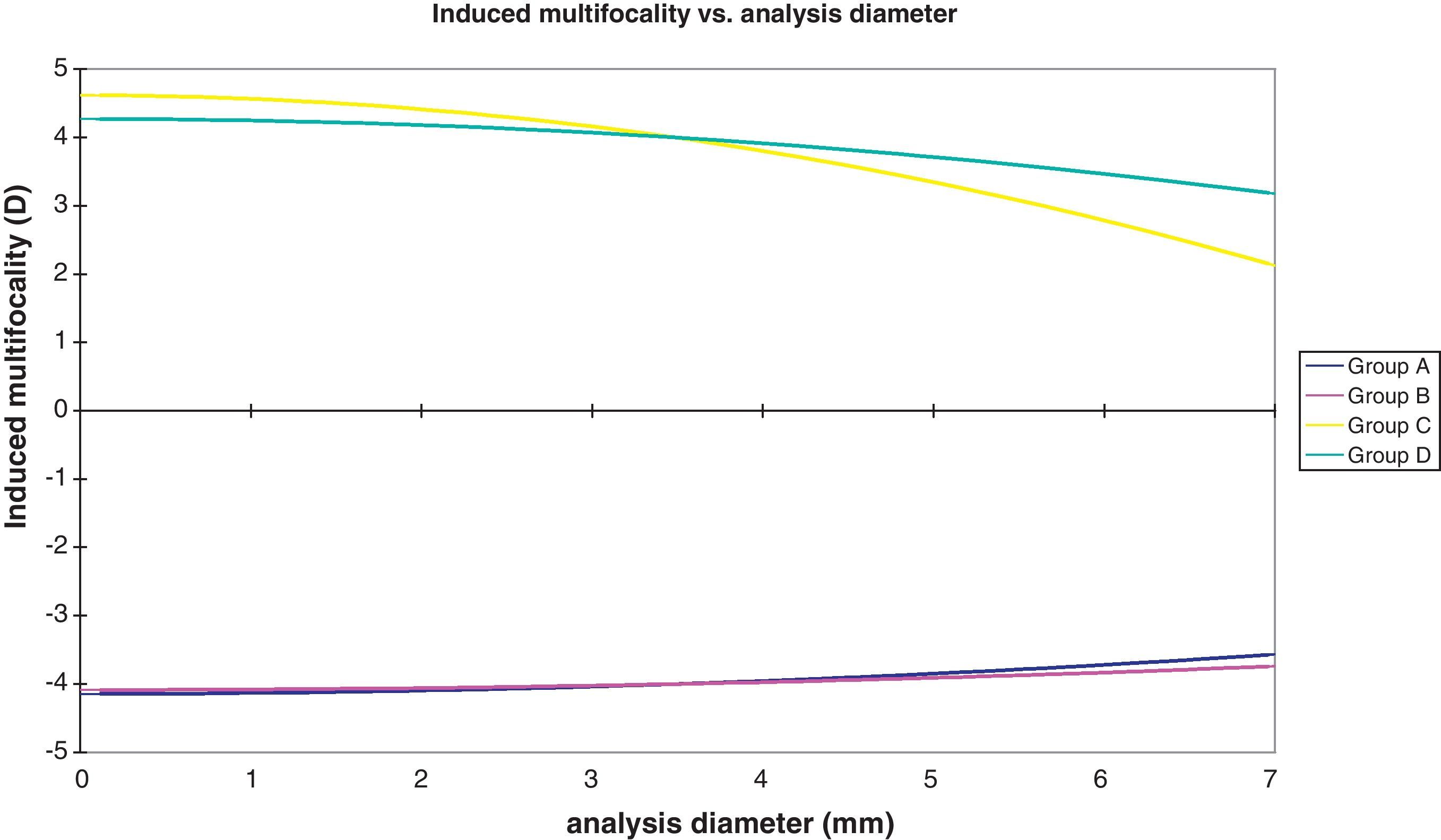
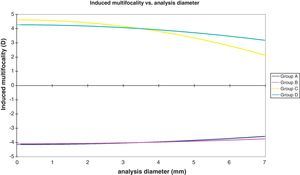
ResultsWe compared the preoperative multifocality with the created multifocality measured in diopters (D) per achieved diopter of defocus correction after LASIK treatment. The created multifocality was in the myopic group A +0.12D per achieved diopter of defocus correction, in group B +0.08D per achieved diopter of defocus correction, in the hyperopic group C −0.51D per achieved diopter of defocus correction and in group D −0.14D per achieved diopter of defocus correction.
ConclusionsAnalyzing the slope of the anterior corneal surface and the corneal wavefront the local refractive changes after LASIK can be characterized in the form of positive (relative central myopization) and negative multifocality (relative peripheral myopization). Less multifocality is created with the aberration-free pattern than with the classic pattern.
Analizar las diferencias relativas a la multifocalidad inducida tras la cirugía LASIK en pacientes miópicos e hiperópicos, utilizando perfiles convencionales y asféricos “aberration-free”.
DispositivoAugenlaserzentrum, Recklinghausen, Alemania.
MétodosEvaluamos retrospectivamente a cuatro grupos consecutivos de 280 ojos tratados con la plataforma láser ESIRIS: el grupo A miópico con tratamiento convencional (70 ojos), el grupo B miópico con tratamiento asférico (70 ojos), el grupo C de ojos hipermetrópicos tratados con LASIK convencional (70 ojos) y el grupo D de ojos hipermetrópicos tratados con perfil asférico (70 ojos). En todos los casos se empleó la Plataforma Láser ESIRIS SCHWIND y el microqueratomo Carriazo-Pendular. El Topógrafo Optikon Keratron obtuvo la medición del cambio en el poder refractivo corneal de la superficie anterior a 3, 5, y 7mm meridionalmente, así como el análisis del frente de onda corneal.
ResultadosComparamos la multifocalidad preoperatoria con la multifocalidad creada medida en dioptrías (D) por dioptría lograda de corrección de desenfoque tras el tratamiento con LASIK. Los valores de multifocalidad creada obtenidos fueron de +0,12D por dioptría lograda de corrección de desenfoque en el grupo miópico A, +0,08D por dioptría lograda de corrección de desenfoque en el grupo B, −0,51D por dioptría lograda de corrección de desenfoque en el grupo hipermetrópico C, y −0,14D por dioptría lograda de corrección de desenfoque en el grupo D.
ConclusionesAnalizando la pendiente de la superficie corneal anterior y el frente de onda corneal podemos caracterizar los cambios refractivos locales tras LASIK, pudiendo analizar, por tanto, la existencia de multifocalidad positiva (miopización central relativa) y negativa (miopización periferica relativa). Se induce menos multifocalidad con el perfil de ablación LASIK asférico “aberration-free” que con el convencional.
With the LASIK (Laser in situ Keratomileusis1) treatment, we have an accepted method to correct refractive errors such as myopia,2 hyperopia,3 and astigmatism.4 The goal of a laser refractive treatment is to obtain the best possible visual function without spectacle correction. Attempting to correct low order aberrations, sphere and cylinder, good results can be achieved in most of cases;5 however, in some cases the patients complain about halos or other impairing visual effects.6
The recent advances in excimer laser technology, such as the use of aspheric ablation profiles, incorporation of higher order aberration (HOA) treatments and eye trackers, have presumably led to better refractive outcomes and reduced HOA induction postoperatively that have been recently reported.7,8
In this study, we want to analyze the induced multifocality after LASIK surgery in myopic and hyperopic patients using the conventional and the aspheric profiles. This could explain some clinical changes, such as the more difficulty in reading in myopic LASIK patients and the opposite situation in hyperopic LASIK patients. The better knowledge of multifocality will help us to design better treatments for presbyopic patients.
We want to clarify the use of the term “multifocality” in this context. Here “spherical aberration” and “multifocality” are considered as “unwanted effects” and should not be mixed up with a multifocality generally sought as a compensation for presbyopia.
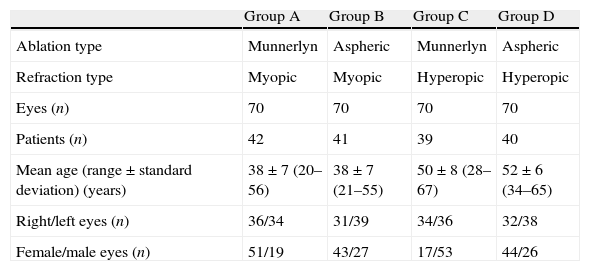
MaterialsPatientsWe retrospectively analyzed 280 eyes in four consecutive groups. The mean age was 45 years with a range from 28 to 67 years. Group A included patients treated with myopic LASIK using a classic Munnerlyn standard profile (70 eyes), group B including myopic eyes treated with aspheric ablation profiles (70 eyes), group C including hyperopic eyes treated with Munnerlyn standard profile (70 eyes) and group D including hyperopic eyes treated with aspheric profile (70 eyes). A follow-up of at least 3 months was completed in 100% of the cases. We analyzed the visual outcome, the corneal wavefront aberration9 and the topographic changes10 of these four consecutive groups of eyes. All patients were examined preoperatively at 1 day, 1 week, 1 month, and 3 months postoperatively.
MethodsIn all cases, standard LASIK surgery was performed with the profile described before.11 The same surgeon (D.O.) in the Augenlaserzentrum Recklinghausen, Germany carried out all operations. We used the Carriazo-Pendular microkeratome (SCHWIND Eye-tech-solutions, Kleinostheim, Germany), and the hinge was located superiorly.
In the case of the classic standard profile, we used our own nomogram calculated from previously treated eyes, which had resulted in some undercorrection. In the case of the aspheric aberration-free profile, we did not use any nomogram.
The conventional or classic profile is based on calculations of Munnerlyn. Aspheric aberration-free profiles are not based on the Munnerlyn proposed profiles, and go beyond that by adding some aspheric characteristics to balance the induction of spherical aberration (prolateness optimization).
The aspheric profile is based on an aberration free treatment. The goal of this treatment is not to induce aberrations in the treated optical zone. To compensate for the aberration induction observed with other types of profile definitions,12 some of the sources of aberrations, such as those related to the loss of efficiency of laser ablation for non-normal incidence are avoided as much as possible.13–15 Optimization is performed by taking into account the loss of efficiency at the periphery of the cornea in relation to the centre, as there is a tangential effect of the spot in relation to the curvature of the cornea (K (keratometry)-reading). The laser platform was the same in all the cases, the ESIRIS platform (SCHWIND Eye-tech-solutions, GmbH, Kleinostheim, Germany). The ESIRIS laser system works at a repetition rate of 200Hz, produces a spot size of 0.8mm (full width at half maximum or FWHM) with a paraGaussian ablative spot profile. High-speed eye-tracking with 330Hz acquisition rate is accomplished with a 5-ms latency period. In all myopic cases, we used an optical zone of 6.50mm and, in hyperopic, 6.25mm. In case of the classic profile, we used a transition zone of 0.50mm, whereas in the case of the aspheric aberration-free profile we used a variable transition zone, which was given automatically by the software in relation to the refraction to be corrected (range 0.2–2.5mm).
Main outcome measures included preoperative and postoperative findings, autorefractor measurements, manifest refraction, best spectacle-corrected visual acuity (BSCVA), uncorrected visual acuity (UCVA), topography and corneal aberrometry as well as complications. The topography and corneal aberrometry (up to the seventh Zernike order) were measured using a videokeratoscope (Keratron™, Optikon2000s.p.a., Italy).
We took the best-fit keratometry (K) readings (K readings) of Maloney index, the simulated K readings (Sim-K), and the K readings at 3, 5 and 7mm. The topographic changes and the differences were analyzed as described in previous studies.16–18
Optical errors, when represented by wavefront aberration, were described by Zernike polynomials19 and coefficients in OSA standard,20 and analyzed for a diameter of 6mm.
Multifocality was assessed in two ways:
- (1)
corneal aberrations16–18:
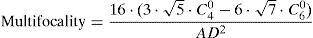
The equation to compute radial symmetric multifocality from Zernike primary and secondary spherical aberrations (in μm) to diopters of multifocality is the following21:
where C40 is primary Zernike spherical aberration; C60 is secondary Zernike spherical aberration; AD is Analysis diameter. - (2)
topographic multifocality16–18:
The topographic multifocality was determined as the progression of the topographic mean keratometric readings from the apical radius of curvature, 3, 5, and 7mm diameters.
For statistical analysis, unpaired t-tests were used to test statistical differences with p values of less than 0.05 being considered statistically significant.
All data were analyzed using the Datagraph-med 3.2 software (Pieger GmbH, Germany).
ResultsTable 1 shows the patients’ demographics comparing all four groups.
Patient demographics.
| Group A | Group B | Group C | Group D | |
| Ablation type | Munnerlyn | Aspheric | Munnerlyn | Aspheric |
| Refraction type | Myopic | Myopic | Hyperopic | Hyperopic |
| Eyes (n) | 70 | 70 | 70 | 70 |
| Patients (n) | 42 | 41 | 39 | 40 |
| Mean age (range±standard deviation) (years) | 38±7 (20–56) | 38±7 (21–55) | 50±8 (28–67) | 52±6 (34–65) |
| Right/left eyes (n) | 36/34 | 31/39 | 34/36 | 32/38 |
| Female/male eyes (n) | 51/19 | 43/27 | 17/53 | 44/26 |
At the 3 months postoperatively, all 280 eyes (100%) were examined.
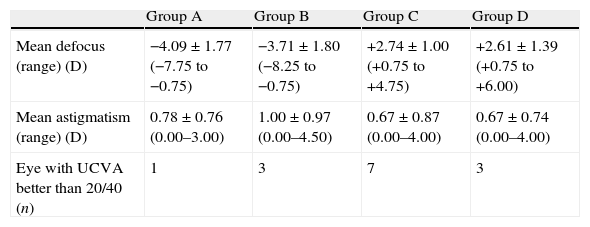
Table 2 summarizes the refractive corrections applied for each of the groups.
Preoperative refractive values.
| Group A | Group B | Group C | Group D | |
| Mean defocus (range) (D) | −4.09±1.77 (−7.75 to −0.75) | −3.71±1.80 (−8.25 to −0.75) | +2.74±1.00 (+0.75 to +4.75) | +2.61±1.39 (+0.75 to +6.00) |
| Mean astigmatism (range) (D) | 0.78±0.76 (0.00–3.00) | 1.00±0.97 (0.00–4.50) | 0.67±0.87 (0.00–4.00) | 0.67±0.74 (0.00–4.00) |
| Eye with UCVA better than 20/40 (n) | 1 | 3 | 7 | 3 |
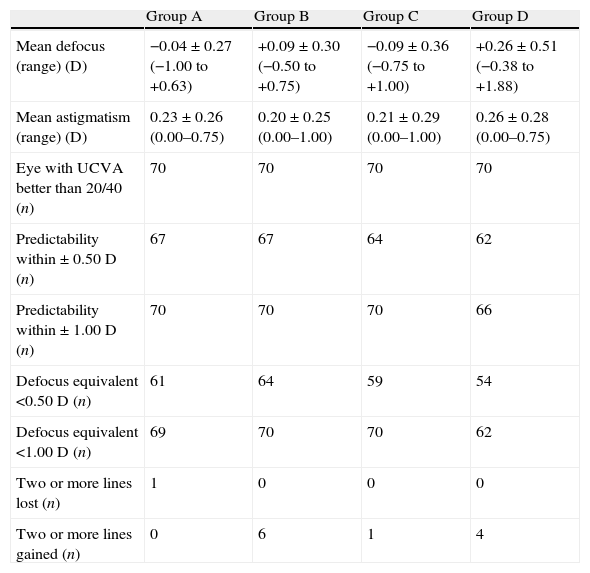
The defocus equivalent after 3 months was under half of a diopter in group A in 87% of the cases and in group B in 91% of eyes. For the hyperopic groups C and D, a defocus equivalent of half of a diopter or less was found in 82% of the cases. All groups had a defocus equivalent (SE+abs(Cyl)/2) of 1D or less in 100% of the cases.
Table 2 summarizes the refractive corrections applied and Table 3 the refractive outcomes achieved for each of the groups.
3 month postoperative refractive values.
| Group A | Group B | Group C | Group D | |
| Mean defocus (range) (D) | −0.04±0.27 (−1.00 to +0.63) | +0.09±0.30 (−0.50 to +0.75) | −0.09±0.36 (−0.75 to +1.00) | +0.26±0.51 (−0.38 to +1.88) |
| Mean astigmatism (range) (D) | 0.23±0.26 (0.00–0.75) | 0.20±0.25 (0.00–1.00) | 0.21±0.29 (0.00–1.00) | 0.26±0.28 (0.00–0.75) |
| Eye with UCVA better than 20/40 (n) | 70 | 70 | 70 | 70 |
| Predictability within±0.50D (n) | 67 | 67 | 64 | 62 |
| Predictability within±1.00D (n) | 70 | 70 | 70 | 66 |
| Defocus equivalent <0.50D (n) | 61 | 64 | 59 | 54 |
| Defocus equivalent <1.00D (n) | 69 | 70 | 70 | 62 |
| Two or more lines lost (n) | 1 | 0 | 0 | 0 |
| Two or more lines gained (n) | 0 | 6 | 1 | 4 |
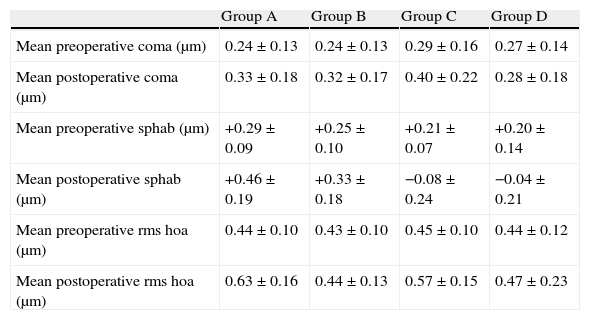
The preoperative and postoperative corneal aberrometry is shown in Table 4.
Comparison of corneal aberrations at 6-mm analysis diameter.
| Group A | Group B | Group C | Group D | |
| Mean preoperative coma (μm) | 0.24±0.13 | 0.24±0.13 | 0.29±0.16 | 0.27±0.14 |
| Mean postoperative coma (μm) | 0.33±0.18 | 0.32±0.17 | 0.40±0.22 | 0.28±0.18 |
| Mean preoperative sphab (μm) | +0.29±0.09 | +0.25±0.10 | +0.21±0.07 | +0.20±0.14 |
| Mean postoperative sphab (μm) | +0.46±0.19 | +0.33±0.18 | −0.08±0.24 | −0.04±0.21 |
| Mean preoperative rms hoa (μm) | 0.44±0.10 | 0.43±0.10 | 0.45±0.10 | 0.44±0.12 |
| Mean postoperative rms hoa (μm) | 0.63±0.16 | 0.44±0.13 | 0.57±0.15 | 0.47±0.23 |
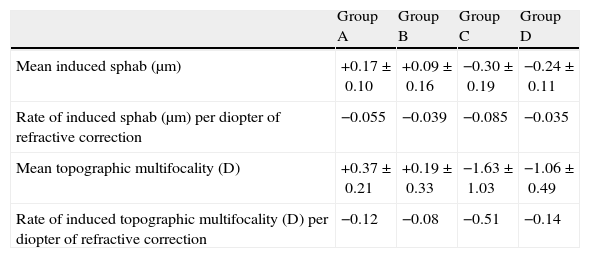
The induced spherical aberrations and the topographic multifocality are summarized in Table 5. Aspheric treatments induced less multifocality in a statistically significant amount (p<0.01 for myopia (group A vs. group B); p<0.05 for hyperopia (group C vs. group D)). Hyperopic treatments induced opposite corneal multifocality to myopic treatments. The difference in the magnitude of the induced multifocality was larger for hyperopic corrections (p<0.001 for conventional (group A vs. group C) and aspheric (group B vs. group D)).
Multifocality.
| Group A | Group B | Group C | Group D | |
| Mean induced sphab (μm) | +0.17±0.10 | +0.09±0.16 | −0.30±0.19 | −0.24±0.11 |
| Rate of induced sphab (μm) per diopter of refractive correction | −0.055 | −0.039 | −0.085 | −0.035 |
| Mean topographic multifocality (D) | +0.37±0.21 | +0.19±0.33 | −1.63±1.03 | −1.06±0.49 |
| Rate of induced topographic multifocality (D) per diopter of refractive correction | −0.12 | −0.08 | −0.51 | −0.14 |
The induction of positive asphericity in the myopic groups were also related to the achieved correction (r2=0.32 and p<0.001 for group A, and r2=0.38 and p<0.001 for group B) with 0.19 per diopter of achieved defocus correction in the classic group and 0.14 per diopter of achieved defocus correction in the aberration-free group. In hyperopic LASIK, there was an induction of negative asphericity also related to the achieved correction, which was higher for the classic group (r2=0.30 and p<0.001 for group C, and r2=0.36 and p<0.001 for group D) (Fig. 1).
Topographic changesFrom the topographic data at 3, 5, and 7mm, a map of multifocality at the different zones could be created. As explained in a previous study,16 the achieved correction can be calculated from the topographic changes after LASIK. We analyzed these data in all groups.
Analyzing the slope of the ablated cornea versus the considered diameter, multifocality could be observed within an area of 7mm diameter in the cornea, amounting to 0.50D in the classic group A and to 0.25D in the aspheric aberration-free group B.
In hyperopic LASIK, Maloney index and the Sim K correlated to the refractive power change. The achieved power change correlated at 5mm, but it was not correlated with the intended hyperopic corrections, as we had an optical zone of 6.5mm.
The achieved power change at 7mm, K readings, was not correlated with intended refractive correction. Furthermore, we found a myopic-like effect even for intended hyperopic corrections, as we had an optical zone of 6.5mm.
DiscussionAs published in previous studies,18,22–24 the induced spherical aberration is of positive sign in case of myopia and of negative sign in case of hyperopia.16,17,25,26 The refractive patient who is myopic before surgery has a “natural” focal point for the near distance. After refractive surgery and having induced positive spherical aberrations, two scenarios are possible: either the patient is centrally overcorrected and emmetropized at the periphery, which means that under mesopic conditions the visual acuity is good but under photopic conditions or when the pupil is miotic there will be difficulties when reading (miotic hyperopia); the other scenario is that the centre is emmetropized and the periphery is undercorrected, and once the pupil dilates, the patient will have difficulties in distance vision (mydriatic myopia). The problem becomes more obvious with an increase in multifocality. In our study, 0.5D with the classic profile myopic group versus 0.25D with the aspheric myopic profile.
In our study, multifocality has been assessed using two approaches (corneal aberrations and topographic zone analyses).16–18 Both approaches provide very similar results but differ in the details. Corneal aberrations multifocality is based on the radial terms of the Zernike expansion of the corneal wavefront aberrations. Thus, it is affected and limited by the number of coefficients used for the Zernike expansion of the corneal wavefront aberrations, it is referred to the pupil centre and provides a smooth radial multifocality change. Topographic multifocality is based on zonal analyses of the corneal refractive power at 0, 3, 5, and 7mm diameters. Thus, it is referred to the corneal vertex and provides a discrete multifocality change. In general the differences between both are minimal, but specially differences may be observed for large pupil-vertex offset27 (i.e. large angles kappa,28 lambda29 or alpha30) or for highly aberrated corneas not fitting accurately to the 7th order of the Zernike expansion.
In hyperopic LASIK patients, we created a positive multifocality higher with the classic profile than with the aspheric profile. This causes an overacted centre of the cornea, which gives a pseudoaccommodation once the pupil is smaller and when the pupil is bigger we a have a little undercorrection. This scenario is ideal in presbyopic patients, as long as the induced aberrations are not so high for inducing a worsening of the visual quality. The problem is that the induction is in relation to the laser settings and not to the specific needs of each patient. An optimization of the induced negative spherical aberration might allow us to treat presbyopic patients in a precalculated way.
Transition zones are used, so that multifocality is expected. However, multifocality is only expected outside the optical zone disc and within the transition zone ring. As the used optical zone was 6.5mm and the largest analysis diameter was 7mm, ideally a flat monofocal correction would be observed within the central 6.5mm diameter disc, and a multifocal effect only from the 6.5 to the 7mm radius ring. With the corneal topographic analysis, we can analyze the shape of the treated cornea and its natural multifocality. The ideal treatment shall preserve this multifocality and only brings the best focus closer to or further away from the retinal plane. For several reasons, including loss of efficiency in the periphery, biomechanical response of the cornea, etc., we modify the natural multifocality of the cornea. In the case of myopia treatment, proper correction of the centre means that the periphery is undercorrected, and this change of multifocality is lower with the aberration-free pattern.
For a pupil of 3mm, a small overcorrection is observed in hyperopic LASIK eyes, which is something good for facilitating reading. For a bigger pupil some degree of hyperopization is induced. This effect is due to a positive multifocality.
In case of myopia, the opposite situation occurs. The induction of positive spherical aberration with a large pupil induces a myopization resulting in poor distance vision. On the other hand, difficulties for reading will be observed for small pupils due to the overcorrection induced.
Multifocality can be something that we want or can be something we create, and we create less multifocality with the aberration-free pattern than with the classic pattern.
Financial disclosureThis work has been conducted without external financial support. Dr. Samuel Arba-Mosquera is employee of SCHWIND eye-tech-solutions. Dr. Diego de Ortueta is consultant for SCHWIND eye-tech-solutions.
Conflicts of interestThe authors have no conflicts of interest to declare.