To determine the inter-examiner agreement of the manual values of central and peripheral corneal thickness as measured by optical coherence tomography (AS-OCT Visante) and to assess the agreement between AS-OCT Visante pachymetry, Orbscan II and ultrasound pachymetry (USP).
MethodsCentral and peripheral (4.0mm from the corneal centre to the superior, inferior, nasal and temporal areas) corneal thickness was analyzed in 30 eyes of 15 patients (mean age, 26.8±6.8 years), with the AS-OCT Visante both automatically (Global-Pachymetry Map) and manually (Flap Tool). The Orbscan II and USP (Corneo-Gage Plus) pachymetry were also assessed. Inter-examiner reproducibility for the manual values of the AS-OCT Visante was calculated. Automatic and manual AS-OCT pachymetries were compared for all corneal locations.
ResultsGood inter-examiner agreement was obtained for the manual values of the AS-OCT Visante for all locations studied (p=1.00). The automatic value was significantly different from the manual value for both central and inferior pachymetry (37±10μm and 27±11μm respectively; p<0.05). Good linear correlation was found between the automatic AS-OCT Visante, the Orbscan II and USP, although there were statistically significant differences (p<0.01) between all of the corneal locations, with the exception of the manual values of the AS-OCT Visante and the Orbscan II for the central corneal thickness (CCT) measures.
ConclusionsThe AS-OCT Visante has high inter-examiner agreement for manual values (Flap Tool). The automatic analysis (Global-Pachymetry Map) provides different corneal thickness values (centrally and peripherally) than those obtained manually for the same corneal scan.
Determinar el acuerdo interexaminador de los valores manuales del espesor corneal central y periférico según la medición por tomografía de coherencia óptica (AS-OCT Visante) y evaluar el acuerdo entre paquimetría con AS-OCT Visante, Orbscan II y paquimetría ultrasónica (PUS).
MétodosSe analizó el espesor corneal central y periférico (4mm del centro de la córnea a las áreas superior, inferior, nasal y temporal) en 30 ojos de 15 pacientes (media de edad, 26,8±6,8 años) con el instrumento AS-OCT Visante, tanto de manera automática (Global-Pachymetry Map) como manual (Flap Tool). También se evaluó la paquimetría con Orbscan II y PUS (Corneo-Gage Plus). Se calculó la reproducibilidad interexaminador para los valores manuales del AS-OCT Visante. Se compararon las paquimetrías AS-OCT manuales y automáticas de todas las zonas de la córnea.
ResultadosSe obtuvo buena concordancia interexaminador de los valores manuales del AS-OCT Visante en todas las zonas examinadas (p=1). El valor automático fue significativamente diferente del valor manual para la paquimetría central y para la inferior (37±10μm y 27±11μm respectivamente; p<0,05). Se observó una buena correlación lineal entre el AS-OCT Visante automático, el Orbscan II y la PUS, aunque hubo diferencias estadísticamente significativas (p<0,01) entre todas las zonas de la córnea, excepto los valores manuales del AS-OCT Visante y el Orbscan II de las mediciones del espesor corneal central (ECC).
ConclusionesEl AS-OCT Visante presenta alta concordancia interexaminador para valores manuales (Flap Tool). El análisis automático (Global-Pachymetry Map) proporciona valores de espesor corneal (céntricos y periféricos) diferentes de los obtenidos manualmente en el mismo examen corneal.
Corneal thickness is an indirect measure of the physiological functioning of the cornea. Indeed, the alteration of this parameter may be indicative of various pathologies.1 It is for this reason that corneal thickness is critical for the diagnosis, treatment, and monitoring of certain diseases of the anterior segment of the eye. There are many devices currently available for the determination of corneal thickness, although the focus of this paper is just on three of them: ultrasound pachymetry (USP), anterior segment-optical coherence tomography (AS-OCT Visante) and a corneal topography system (Orbscan II).
USP is one of the most popular techniques used to measure corneal thickness and is currently considered the gold standard.2–5 Its advantages include its ease of use, portability, and low cost. However, it has some disadvantages that may affect the accuracy of the values obtained,2,5 including: the need for topical anesthesia, direct contact with the corneal surface which could induce epithelial damage, patient discomfort, possible probe indentation in the cornea during measurement, repeatability conditioned to the placement of the probe judged visually, and possible non-perpendicular placement of the probe to the corneal surface. All this drawbacks make the USP to have lower reliability compared with other pachymetry techniques such as optical coherence tomography or elevation topography.6–8
Anterior Segment-Optical Coherence Tomography Visante (AS-OCT Visante, Carl Zeiss Meditec Inc, Dublin, Calif.) is a computerized instrument that acquires and analyses cross-sectional scans of the anterior segment of the eye without contact. AS-OCT Visante uses low coherence interferometry to compare the delay of light reflections across tissues against a reference reflection. To construct a 2-dimensional OCT image, multiple single axial scans (A-scans) are combined. AS-OCT Visante is able to acquire 2,000 A-scans per second, although the standard imaging mode uses fewer scans to get a wider view and provides high-quality cross-sectional corneal images with 17μm of axial resolution.9 AS-OCT Visante is a time-domain system, and despite of being the fastest commercial device in its category, it is still slower than the fourier-domain OCT. In contrast, AS-OCT Visante has a longer wavelength (1310nm) that penetrates more deeply through the sclera and iris;10 and it is also able to show all anterior segment structures in a single image. The AS-OCT Visante assesses the thickness of the cornea along its entire surface. The software program is accompanied by a caliper (Flap tool) that allows for manual analysis of corneal thickness at any desired point. This tool is very useful for measuring the thickness of the flap in LASIK procedures.11
Orbscan II provides anterior segment data in the form of topographic surfaces, including full corneal pachymetry, by analyzing images of the anterior and posterior corneal reflecting surfaces based on slit-scanning technology and videokeratography.12,13
The purpose of this study was to determine the inter-examiner agreement of the manual values on central and peripheral areas of the cornea using the Flap tool provided by AS-OCT Visante and assessing the agreement between AS-OCT Visante pachymetry with other reliable devices and techniques, such as the Orbscan II and USP.
Patients and methodsSubjectsThirty eyes from 15 volunteers were included in this study (13 women; 2 men). The mean age was 26.8±6.8 years (range: 20 to 41 years). The mean refractive error (spherical equivalent) was −1.8±1.9 D (range, −5.00 to +1.75 D). Subjects were excluded if they had active anterior segment disease that might cause an alteration in corneal thickness, a history of ocular surgery, or a prior history of wearing contact lenses. Informed consent was obtained from each subject, and all of the subjects were treated in accordance with the tenets of the Declaration of Helsinki.
InstrumentationCorneal thickness was assessed using the AS-OCT Visante (Carl Zeiss Meditec Inc, Dublin, Calif.), the Orbscan II (Bausch & Lomb, Rochester, NY, version 3.12), and USP (Sonogage, Sonogage Inc., Cleveland, Ohio; calibrated by the manufacturer).
AS-OCT Visante is a non-contact imaging technique that uses infrared light to obtain high-resolution, cross-sectional images in vivo of the cornea and anterior eye (anterior chamber, iris and lens). The use of the AS-OCT Visante has been described previously.14,15 Its software can measure corneal thickness at any desired point. One single scan was performed for each eye using the scan profile protocol (selecting A-scan, which is a particular setting of the AS-OCT Visante software).
Corneal thickness was analyzed in five different corneal locations: at the center of the cornea and at the superior, inferior, nasal, and temporal regions of the tissue 4.0mm from the centre. Two different analyses were conducted for every single scan (one single scan was performed for each eye). First, an automatic analysis was conducted using the Global-Pachymetry Map, which provides the thickness of a patient's cornea automatically, and a second manual analysis of the scan was conducted by three different masked examiners who collected corneal thickness values using the Flap Tool option by placing the cursors of the caliper at the limits of the anterior and posterior corneal surfaces.
The procedure involving the use of the Orbscan II has been described previously.12,13 An experienced operator conducted the Orbscan exploration to obtain central and peripheral (4.0mm from the corneal centre at the superior, inferior, nasal and temporal areas of the tissue) corneal pachymetry (with 95% acoustic factor). One scan was performed for each eye.
Central corneal thickness (CCT) was measured using USP after analyses with the AS-OCT Visante and Orbscan II had been conducted to avoid corneal changes resulting from the direct contact of the probe with the cornea or topical anesthesia. To perform USP, the cornea was anesthetized with a drop of proparacaine hydrochloride (0.5%). The probe was applied at an angle perpendicular to the corneal surface (standard clinical conditions). The same experienced and blinded operator performed all of the USP procedures. Seven measurements were obtained for the central cornea, and the highest and lowest were discarded. The mean of the five remaining measurements was used as the final value.
All of the tests were performed between 14.00 and 20.00 hours to avoid the edematous cornea as well as sleep-induced alterations in corneal thickness. This is the time of day when the eye is most physiologically stable.1
Data analysisThe data were analyzed using the Statistical Package for the Social Sciences (SPSS for Windows software, version 14.0, SPSS, Inc., Chicago, Illinois, USA).
Inter-examiner agreement of the manual values of the AS-OCT Visante was determined using multiple analysis of variance (ANOVA) with Bonferroni correction. A p-value <0.05 was considered statistically significant. The manual and automatic pachymetry obtained from the AS-OCT Visante were compared for central, superior, inferior, nasal, and temporal corneal thickness using multiple analysis of variance (ANOVA) with Bonferroni correction. A p-value <0.05 was considered statistically significant.
The manual and automatic values from the AS-OCT Visante were also compared with the Orbscan II and USP using Student's paired t-test. A p-value <0.05 was considered statistically significant. Limits of agreement were calculated (mean±two standard deviations) as suggested by Bland and Altman.15 Correlations between the automatic values of the AS-OCT Visante, the Orbscan II and USP were determined by linear correlation analysis. The correlation coefficient (r2) was also calculated. A p-value <0.05 was considered statistically significant.
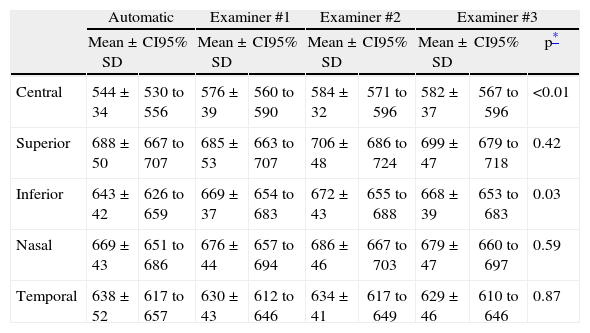
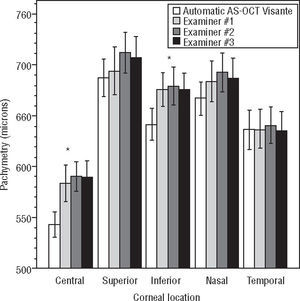
ResultsThe central corneal thickness as measured by USP was 555±30μm. The CCT as measured by Orbscan II was 588±42μm, while in the peripheral locations, it was 639±44μm, 626±39μm, 652±44μm, and 607±48μm for the superior, inferior, nasal, and temporal corneal locations, respectively. The automatic CCT obtained using the AS-OCT Visante was 544±34μm. The CCT measured manually with the AS-OCT Visante was 576±39μm, 584±32μm, and 582±37μm for examiners #1, #2, and #3, respectively. Table 1 summarizes the AS-OCT Visante central and peripheral corneal thickness measurements obtained using automatic and manual analysis.
Automatic and manual AS-OCT Visante pachymetry
| Automatic | Examiner #1 | Examiner #2 | Examiner #3 | ||||||
| Mean±SD | CI95% | Mean±SD | CI95% | Mean±SD | CI95% | Mean±SD | CI95% | p* | |
| Central | 544±34 | 530 to 556 | 576±39 | 560 to 590 | 584±32 | 571 to 596 | 582±37 | 567 to 596 | <0.01 |
| Superior | 688±50 | 667 to 707 | 685±53 | 663 to 707 | 706±48 | 686 to 724 | 699±47 | 679 to 718 | 0.42 |
| Inferior | 643±42 | 626 to 659 | 669±37 | 654 to 683 | 672±43 | 655 to 688 | 668±39 | 653 to 683 | 0.03 |
| Nasal | 669±43 | 651 to 686 | 676±44 | 657 to 694 | 686±46 | 667 to 703 | 679±47 | 660 to 697 | 0.59 |
| Temporal | 638±52 | 617 to 657 | 630±43 | 612 to 646 | 634±41 | 617 to 649 | 629±46 | 610 to 646 | 0.87 |
Central and peripheral AS-OCT Visante pachymetry for the automatic and manual values (examiners #1, #2 and #3). Diff: Mean difference (μm); SD=standard deviation; IC95%: 95% interval of confidence.
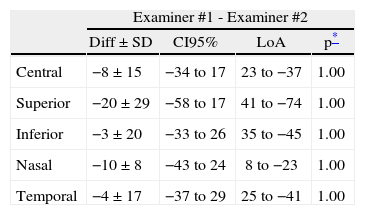
High inter-examiner agreement, without statistically significant differences (p=1.00 ANOVA with Bonferroni correction), was found between the AS-OCT Visante manual values obtained by each one of the three examiners in all of the corneal locations studied (Table 2).
Inter-examiner agreement for the manual values from the AS-OCT Visante
| Examiner #1 - Examiner #2 | ||||
| Diff±SD | CI95% | LoA | p* | |
| Central | −8±15 | −34 to 17 | 23 to −37 | 1.00 |
| Superior | −20±29 | −58 to 17 | 41 to −74 | 1.00 |
| Inferior | −3±20 | −33 to 26 | 35 to −45 | 1.00 |
| Nasal | −10±8 | −43 to 24 | 8 to −23 | 1.00 |
| Temporal | −4±17 | −37 to 29 | 25 to −41 | 1.00 |
| Examiner #1 - Examiner #3 | ||||
| Diff±SD | CI95% | LoA | p* | |
| Central | −6±13 | −32 to 19 | 19 to −31 | 1.00 |
| Superior | −14±17 | −52 to 24 | 26 to −40 | 1.00 |
| Inferior | 0.5±19 | −29 to 30 | 37 to −35 | 1.00 |
| Nasal | −3±7 | −37 to 30 | 11 to −16 | 1.00 |
| Temporal | 1±7 | −32 to 34 | 14 to −19 | 1.00 |
| Examiner #2 - Examiner #3 | ||||
| Diff±SD | CI95% | LoA | p* | |
| Central | 2±9 | −24 to 28 | 19 to −18 | 1.00 |
| Superior | 7±15 | −31 to 44 | 32 to −26 | 1.00 |
| Inferior | 4±13 | −25 to 33 | 31 to −20 | 1.00 |
| Nasal | 6±7 | −27 to 39 | 19 to −10 | 1.00 |
| Temporal | 5±14 | −28 to 38 | 34 to −23 | 1.00 |
Corneal pachymetry differences for the manual values of the AS-OCT Visante between the three different examiners for all corneal locations. Diff: Mean difference (μm); SD: standard deviation; IC95%: 95% interval of confidence; LoA: Limits of agreement (Mean±2SD).
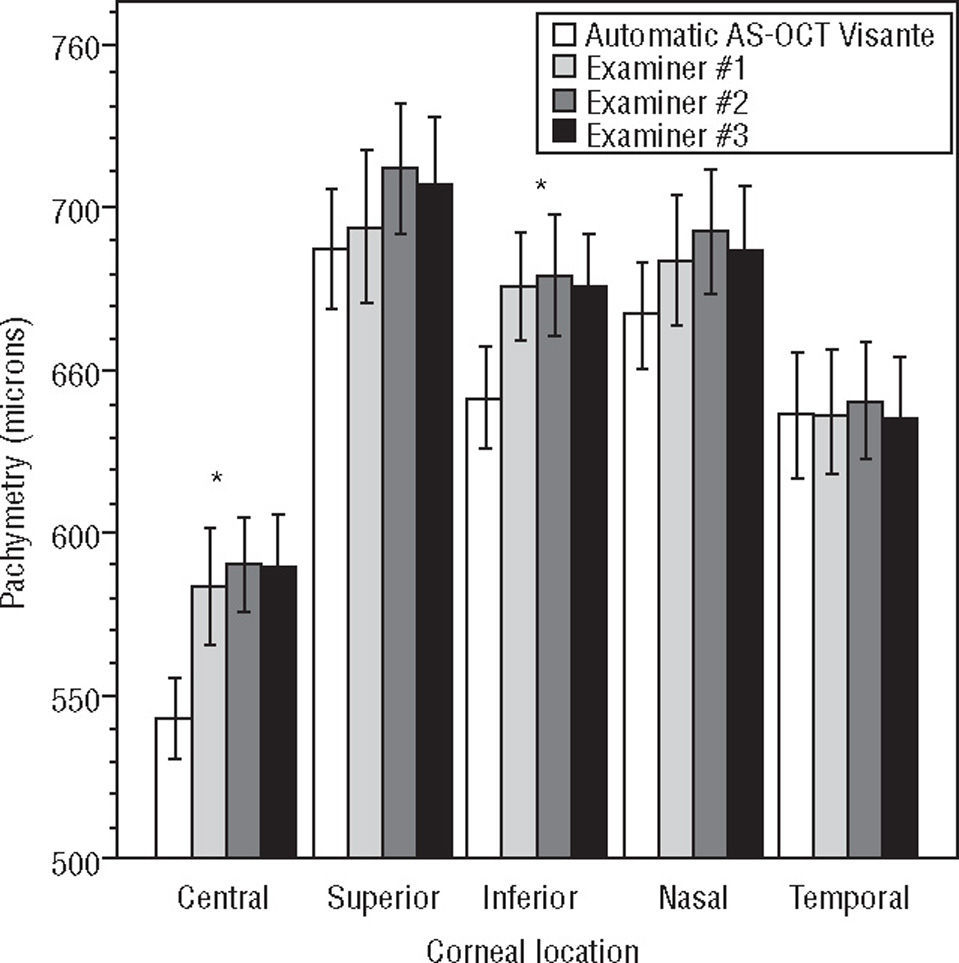
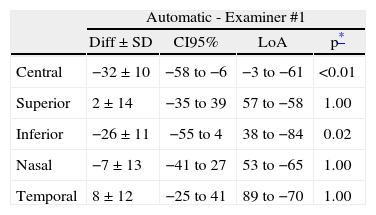
Good agreement between the automatic and the manual values (obtained by each one of the three examiners) from the AS-OCT Visante were found for the superior, nasal, and temporal corneal locations (p>0.05 multiple ANOVA). However, statistically significant differences were found for the CCT and inferior corneal thickness between both (automatic and manual) AS-OCT Visante analyses (p<0.05 ANOVA with Bonferroni correction). The difference between the automatic and the mean manual analyses was 37±10μm for CCT and 27±11μm for inferior corneal thickness. Figure 1 and Table 3 show the difference between the manual and automatic values of the AS-OCT Visante.
Agreement between manual (examiners #1, #2 and #3) and automatic values from the AS-OCT Visante pachymetry. *Statistically significant differences (p<0.05 multiple ANOVA) were found between manual and automatic values for the central and inferior corneal locations. However, non-statistically significant differences were found between the manual values of the three blinded examiners (p>0.05 multiple ANOVA with Bonferroni correction) in all of the corneal locations. Non-statistically significant differences were found (p>0.05 multiple ANOVA) between the manual and automatic values for the remaining locations.
Agreement between automatic and manual AS-OCT Visante pachymetry
| Automatic - Examiner #1 | ||||
| Diff ± SD | CI95% | LoA | p* | |
| Central | −32±10 | −58 to −6 | −3 to −61 | <0.01 |
| Superior | 2±14 | −35 to 39 | 57 to −58 | 1.00 |
| Inferior | −26±11 | −55 to 4 | 38 to −84 | 0.02 |
| Nasal | −7±13 | −41 to 27 | 53 to −65 | 1.00 |
| Temporal | 8±12 | −25 to 41 | 89 to −70 | 1.00 |
| Automatic - Examiner #2 | ||||
| Diff±SD | CI95% | LoA | p* | |
| Central | −40±10 | −66 to −15 | −25 to −56 | <0.01 |
| Superior | −18±14 | −54 to 19 | 27 to −69 | 1.00 |
| Inferior | −29±11 | −58 to 0.03 | 35 to −93 | <0.01 |
| Nasal | −17±12 | −49 to 16 | 42 to −71 | 1.00 |
| Temporal | 4±12 | −29 to 37 | 76 to −67 | 1.00 |
| Automatic - Examiner #3 | ||||
| Diff ± SD | CI95% | LoA | p* | |
| Central | −38±10 | −58 to −6 | −17 to −60 | <0.01 |
| Superior | −11±14 | −49 to 26 | 27 to −56 | 1.00 |
| Inferior | −25±11 | −55 to 4 | 31 to −77 | 0.03 |
| Nasal | −10±12 | −43 to 23 | 47 to −65 | 1.00 |
| Temporal | 9±12 | −24 to 42 | 87 to −69 | 1.00 |
Corneal pachymetry differences between the automatic and the manual values of the AS-OCT Visante for the three different examiners and for all corneal locations. Diff: Mean difference (μm); SD: standard deviation; IC95%: 95% interval of confidence; LoA: Limits of agreement (Mean±2 SD).
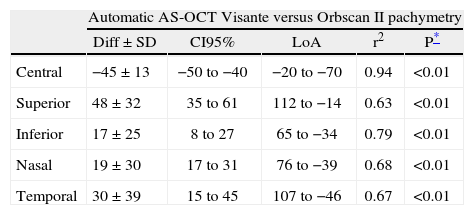
Good linear correlation (r2>0.62) was found for all corneal locations between the AS-OCT Visante automatic values and the values from the Orbscan II and USP; there were statistically significant differences (p<0.01 on Student's paired t-test) for all corneal locations (Table 4).
Agreement between automatic AS-OCT Visante, Orbscan II and USP
| Automatic AS-OCT Visante versus Orbscan II pachymetry | |||||
| Diff±SD | CI95% | LoA | r2 | P* | |
| Central | −45±13 | −50 to −40 | −20 to −70 | 0.94 | <0.01 |
| Superior | 48±32 | 35 to 61 | 112 to −14 | 0.63 | <0.01 |
| Inferior | 17±25 | 8 to 27 | 65 to −34 | 0.79 | <0.01 |
| Nasal | 19±30 | 17 to 31 | 76 to −39 | 0.68 | <0.01 |
| Temporal | 30±39 | 15 to 45 | 107 to −46 | 0.67 | <0.01 |
| Automatic AS-OCT Visante versus US pachymetry | |||||
| Diff±SD | CI95% | LoA | r2 | p* | |
| Central | −12±7 | −15 to −9 | 2 to −26 | 0.95 | <0.01 |
Corneal pachymetry differences for comparisons between the automatic values from the AS-OCT Visante, the Orbscan II and USP for all corneal locations. Diff: Mean difference (μm); SD: standard deviation; IC95%: 95% interval of confidence; LoA: Limits of agreement (Mean±2 SD).
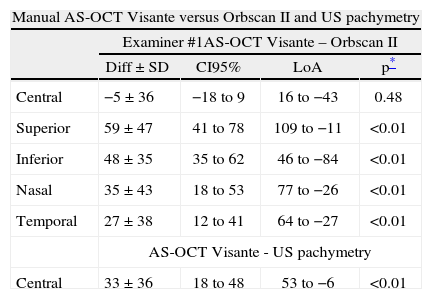
The manual CCT obtained with the AS-OCT Visante was significantly different (p<0.01 Student's paired t-test) from that obtained with USP. However, no significant differences were found for the Orbscan II CCT (p>0.05 Student's paired t-test). The results of the Orbscan II peripheral pachymetry were significantly different than all of the AS-OCT Visante manual values (p<0.01 Student's paired t-test) (Table 5).
Agreement between the manual AS-OCT Visante, Orbscan II and USP values
| Manual AS-OCT Visante versus Orbscan II and US pachymetry | ||||
| Examiner #1AS-OCT Visante – Orbscan II | ||||
| Diff±SD | CI95% | LoA | p* | |
| Central | −5±36 | −18 to 9 | 16 to −43 | 0.48 |
| Superior | 59±47 | 41 to 78 | 109 to −11 | <0.01 |
| Inferior | 48±35 | 35 to 62 | 46 to −84 | <0.01 |
| Nasal | 35±43 | 18 to 53 | 77 to −26 | <0.01 |
| Temporal | 27±38 | 12 to 41 | 64 to −27 | <0.01 |
| AS-OCT Visante - US pachymetry | ||||
| Central | 33±36 | 18 to 48 | 53 to −6 | <0.01 |
| Examiner #2AS-OCT Visante – Orbscan II | ||||
| Diff±SD | CI95% | LoA | p* | |
| Central | 3±32 | −9 to 4 | 26 to −36 | 0.67 |
| Superior | 77±38 | 62 to 92 | 118 to 20 | <0.01 |
| Inferior | 53±35 | 40 to 66 | 90 to 2 | <0.01 |
| Nasal | 43±41 | 27 to 58 | 83 to −15 | <0.01 |
| Temporal | 34±37 | 20 to 48 | 63 to −12 | <0.01 |
| AS-OCT Visante – US pachymetry | ||||
| Central | 36±31 | 23 to 50 | 48 to 7 | <0.01 |
| Examiner #3AS-OCT Visante – Orbscan II | ||||
| Diff±SD | CI95% | LoA | p* | |
| Central | 1±34 | −11 to 14 | 20 to −34 | 0.84 |
| Superior | 72±40 | 56 to 88 | 103 to 22 | <0.01 |
| Inferior | 49±31 | 37 to 61 | 75 to 8 | <0.01 |
| Nasal | 39±41 | 23 to 54 | 80 to −20 | <0.01 |
| Temporal | 29±35 | 16 to 42 | 59 to −17 | <0.01 |
| AS-OCT Visante – US pachymetry | ||||
| Central | 36±35 | 21 to 51 | 55 to −2 | <0.01 |
Corneal pachymetry differences for the comparison between the manual values from the AS-OCT Visante (examiners #1, #2 and #3), Orbscan II and USP for all corneal locations. Diff: Mean difference (μm); SD: standard deviation; IC95%: 95% interval of confidence; LoA: Limits of agreement (Mean±2SD).
Many studies have supported the effectiveness of the AS-OCT Visante as a promising tool for the assessment of the anterior segment of the eye in clinical practice, including its use for the measurement of corneal thickness.19–21 Most of these reports have assessed the repeatability and reproducibility of the manual values (Flap tool) of the AS-OCT Visante in corneas after LASIK surgery. In all cases, this instrument was found to have good repeatability and reproducibility.18,22,23 In the case of corneas that had not undergone any kind of previous surgery, we must highlight the study conducted by Li et al.,24 who found good repeatability and reproducibility for both manual and automatic pachymetric values of the CCT. Li et al.,24 found statistically significant differences between manual and automatic values, which is in line with our results. Moreover, we studied peripheral pachymetry, the data from which had been not previously reported, and found statistically significant differences when compared the automatic and manual values for the inferior pachymetry.
Huang et al.12 described good intra-examiner repeatability for central and peripheral corneal pachymetry when one single scan was automatically analyzed. However, they did not include manual analysis in their work, although a manual tool may be necessary in the evaluation of some patients to measure flap thickness 11 or contact lens induced corneal swelling,15 for example.
The present work is the first to determine inter-examiner agreement for both central and peripheral corneal thickness of the manual corneal measures using the Flap Tool. We also compared data obtained from the same corneal AS-OCT Visante scan analyzed automatically (Global-Pachymetry Map) and manually (from three masked examiners with the Flap Tool provided by the AS-OCT Visante software). These results are critical for clinical and research practice, as they may facilitate the standardization of corneal thickness analysis. The differences found between the manual and automatic results could be of paramount importance in the follow-up of patients in refractive surgery, contact lens wear and corneal pathologies.
Inter-examiner agreement for the manual valuesGood inter-examiner agreement was found with no statistically significant differences between the manual values of the AS-OCT Visante (p=1.00 ANOVA with Bonferroni correction) for the three masked examiners. This result is in accordance with previous reports that examined CCT 18,22–24 and are the first to describe the agreement of the manual values in the periphery of the cornea. The inter-examiner agreement obtained in this study suggests that the device is acceptable for clinical use.
Agreement between automatic and manual valuesThe differences between the automatic and the manual values for the central24 and inferior corneal location suggest that automatic and manual analyses cannot be used interchangeably. However, the superior, nasal, and temporal areas did not show significant differences between the automatic and manual values, although the manual values were higher than the automatic values, with the exception of the temporal corneal location (all examiners) and the superior location (only the examiner #1 values). Li et al.24 noticed that the anterior corneal limit delineated by the AS-OCT Visante software was positioned slightly under the anterior corneal surface, which could lead to the underestimation of corneal thickness when measured automatically. Furthermore, Dunne et al.25 have presented improved formulas for the AS-OCT Visante software in order to get better measures for axial distances and surface curvature. We agree that one of the reasons for these differences could be related to the software, which analyzes the pachymetry automatically (Global-Pachymetry Map), as we used the same scan and it was found to have good agreement with no differences between the manual values of the three masked examiners for each one of the five corneal locations studied.
Agreement between AS-OCT Visante, USP and Orbscan IIThe differences in the CCT between the AS-OCT Visante (both manual and automatic analysis) and USP found in this study are consistent with previous studies in the literature,2,5,10,20,24,25 although there was no discrimination between the manual or automatic values in those reports. Automatic values for the AS-OCT Visante were significantly lower than those for USP; however, the manual values (collected by three different examiners) were significantly higher than those from USP (Tables 4 and 5).
We found a similar trend with Orbscan II pachymetry, with significant differences both in central (in accordance with the previous studies focused on CCT27) and peripheral locations (i.e., superior, inferior, nasal and temporal). The automatic values of the AS-OCT Visante were significantly lower than those taken with the Orbscan II in the central area, but higher in the peripheral locations (Table 4). Between the manual values of the AS-OCT Visante and the Orbscan II, no statistically significant differences were found for CCT (p>0.05 multiple ANOVA); however, values for peripheral pachymetry were always higher (p<0.05 multiple ANOVA) when measured with the AS-OCT Visante than with the Orbscan II (Table 5).
One of the main limitations of this study could be related with the use of both eyes of the same subject to assess agreement between the manual and the automatic analysis of AS-OCT Visante; although it has been previously reported several studies where both eyes of the same subject have been used to determine agreement between different devices.28–30 Another possible limitation is the fact that we have performed one single scan when using the Orbscan II, although it has been widely reported the high repeatability of this device.14,31 The small sample data suggest that these results should be interpreted with caution. More studies in non-healthy corneas should also be conducted to determine the agreement between the manual and the automatic analysis.
Clinical implicationsWe found the AS-OCT Visante to be a device with good inter-examiner agreement when used for the assessment of corneal thickness18,22–24 although special attention is required when using this device, mainly because it does not provide the same values for the same scan when it is automatically or manually analyzed. These results confirm that AS-OCT Visante, USP and Orbscan II are not interchangeable devices.
The overestimation of corneal thickness in clinical practice (especially in the central area) can be of paramount importance for certain diagnostic and therapeutic decisions. It can lead to serious complications, for example, in pre-LASIK (Laser In Situ Keratomileusis) evaluation. More studies with larger sample sizes and a standardized measurement and analysis protocol for determining corneal thickness using the AS-OCT Visante device are needed to confirm these results.
In conclusion, this study demonstrates that automatic analysis with the AS-OCT Visante (Global-Pachymetry Map) provides different corneal thickness values than those obtained manually with the Flap Tool (a software program of the AS-OCT Visante) for the same corneal scan, which finally means that the same device is not giving the same data for the same tissue. However, focusing just on the Flap Tool option, it has been found a high inter-examiner agreement when used both for central and peripheral corneal thickness assessment.
Conflicts of interestsThe authors have no conflicts of interests to declare.
American Journal Experts reviewed the English grammar of this manuscript.