To understand the pattern of visual development in preterm children attending a primary eye care centre in Malaysia. To improve the knowledge and management of preterm children in the South East Asian region.
MethodsClinical records of preterm babies born from 2000 to 2008 were reviewed retrospectively. Follow-up data from 1 to 6 years were also reviewed. Data collected included; gender, race, age at birth, current age, birth weight, and current weight, record of fundus examination, visual acuity (VA), refraction and strabismus.
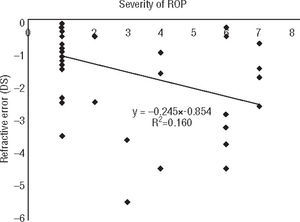
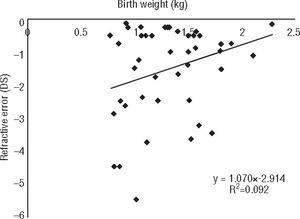
ResultsA total of 102 records were reviewed. Of these, 48 (47.1%) were males and 54 (52.9) were females, with 60 (58.8%) Malays, 20 (19.6%) Chinese, 21 (20.6%) Indian and 1 (1%) Caucasian. The average gestational age was 30.83±2.42 weeks and average birth weight was 1.37±0.36kg. Around 38 (37.3%) of them had retinopathy of premature (ROP) and 64 (62.7%) were without ROP. Improvement of VA was observed with age. Children with ROP developed myopia with age and those without ROP became mostly hyperopic. Linear regression analysis indicated that degree of myopia is significantly associated with severity of ROP and birth weight. No significant increment of astigmatism was noted with age. Only 13.7% of them had strabismus.
ConclusionsThis study concludes that children with ROP developed myopia with age and those without ROP became more hyperopic. Degree of myopia is associated with severity of ROP and birth weight. These factors should be considered during screening of vision and refractive error in children.
Comprender el modelo de desarrollo visual en niños prematuros atendidos en un centro de atención oftalmológica primaria de Malasia. Mejorar el conocimiento y el tratamiento de los niños prematuros en la región del sudeste asiático.
MétodosSe revisaron retrospectivamente las historias clínicas de niños prematuros nacidos entre 2000 y 2008. También se revisaron datos de seguimiento de 1 a 6 años. Los datos recopilados inclu-yen sexo, raza, edad al nacer, edad actual, peso al nacer y peso actual, registro de la exploración del fondo, agudeza visual (AV), refracción y estrabismo.
ResultadosEn total se revisaron 102 historias clínicas. De estas, 48 (47,1%) eran varones y 54 (52,9), mujeres, 60 (58,8%) malayos, 20 (19,6%) chinos, 21 (20,6%) indios y 1 (1%) caucásico. La edad gestacional media fue 30,83±2,42 semanas y el peso medio al nacer fue 1,37±0,36kg. Alrededor de 38 (37,3%) de ellos tenían retinopatía del prematuro (ROP) y 64 (62,7%), no. Con los años, se observó una mejora de la AV. Los niños con ROP desarrollaron miopía con la edad y los que no tenían ROP desarrollaron hipermetropía. El análisis de regresión lineal mostró que el grado de miopía está asociado significativamente con la gravedad de la ROP y el peso al nacer. Con la edad no se observó ningún aumento significativo del astigmatismo. Solamente un 13,7% de ellos tenían estrabismo.
ConclusionesEste estudio concluye que los niños con ROP desarrollaron miopía con la edad y los que no tenían ROP desarrollaron más hipermetropía. El grado de miopía está asociado con la gravedad de la ROP y el peso al nacer. Estos factores deben considerarse durante la evaluación de la visión y del error de refracción en niños.
Prematurely born children are at a high risk group for various visual problems.1,2 In the neonatal period, they may develop retinopathy of prematurity (ROP), whereas later they may develop other visual dysfunctions. It has been shown that ROP caused an increase in all types of refractive error later in life including myopia, hyperopia, anisometropia and astigmatism.3,4 Holmstroma et al. conducted long term ophthalmological follow up of 248 preterm infants for 2.5 years and found that the incidence of myopia and astigmatism was 10% and 26% respectively at the age of 30 months.5 Astigmatism was found to be associated with ROP, but not with cryotreated ROP. Their results also showed that anisometropia occurred in 8.4% of the babies at 30 months of age and the incidence of anisometropia was higher in eyes with ROP, particularly in cryotreated eyes.5
O’Connor et al. conducted a prospective longitudinal study of ROP in 505 preterm children at 10 to 12 years of age.6 In this study, ophthalmic morbidity was defined as visual acuity poorer than 6/6 or the presence of strabismus, myopia, colour vision defect or visual field defect. The rate of ophthalmic morbidity found in this study at 10 to 12 years of age was 50.8% compared to 19.5% in the control group and the highest rate of ophthalmic morbidity was found to be associated with severe ROP. Their analysis also showed a higher percentage of preterm children without ROP developing visual dysfunctions than the control group which indicates that preterm children are at increased risk of visual impairments compared to children who are born full term.
In a more recent study, Cook et al. examined the ocular growth and refractive error development in premature infants (32 and 52 weeks postmenstrual age babies with or without ROP).7 Their results showed linear growth of corneal curvature of babies with ROP that correlated well with refractive state. The myopic babies found at the beginning of the study became emmetropic around term and were hyperopic toward 52 weeks of postmenstrual age. Verma et al. determined the refractive status of 50 preterm neonates at birth and at the age of 6 months and 1 year using cycloplegic refraction.8 The refractive error however was not quantified by the examiner. Myopia over 1 D was determined based on the shadow movement against the mirror during retinoscopy. Hyperopia and myopia lower than 1 D were differentiated using different lenses. Their results showed that at 1 year, hyperopia was found in 20% of the examined eyes while myopia was present in 16%. Myopia was seen exclusively among infants with birth weight of 2000g or less.
This retrospective study was planned to better understand the pattern of visual function development in preterm children attending a primary eye clinic in one of the states in Malaysia. To our knowledge there are very few reports available in the literature describing the ophthalmic findings among preterm children in Asian populations. In a study conducted in India, Varghese et al. investigated the relationship between refractive error and physical parameters at birth in preterm and full term babies.9 Their results showed that the incidence of myopia increased with decreasing weight and concluded that birth weight should be used as criteria for screening for refractive error. Other studies carried out on normal birth pre-school children showed higher incidence of myopia among Asian, than Caucasian children.10,11 It is possible that there are some ethnic variations in the development of visual functions in the preterm children. Understanding ethnic differences is important in the management in these children so that early intervention can be provided and their quality of life can be improved. As Malaysia is a multicultural country, the results will enable us to improve the current optometric management of prematurely born children in this country.
MethodsThis is a retrospective study involving data from clinical records of preterm babies in the eye clinic, Hospital Tuanku Ja’afar, Seremban, Negeri Sembilan. All the preterm babies files listed in the eye clinic's registration book from year 2000 to year 2008 were traced. Data collected include: gender, race, age at birth, current gestation age, birth weight, current weight and record of clinical findings such as; fundus examination diagnosis, stage of ROP, zone of ROP, treatment given (i.e. laser therapy), visual acuity, refraction and strabismus assessment. In the current system, the first ophthalmic follow up examination should be conducted at 6 months after birth, 1 year and every year after that until 6 years old. However, due to schedule issues in the hospital, most of the first follow up appointments were given at one year after birth.
All patients remained anonymous. The inclusion criteria included: all clinic records of neonates born earlier than 37 weeks gestational age between 2000 to 2008 and complete clinical records with information during birth such as; date of birth, age at birth, current gestation age and birth weight. The clinical records must contain the record of the first two preterm visits (at first and second year after birth), including fundus examination, diagnosis and results of visual evaluation. This study was approved by the ethical committee of the faculty and followed the tenets of the Declaration of Helsinki.
Fundus examination was conducted on all patients 4 weeks after birth using binocular indirect ophthalmoscope to detect the presence of ROP. Pupils were dilated using topical cyclopentolate 0.5% and phenylephrine 2.5% prior to examination. ROP was classified in all patients according to the International Classification of Retinopathy of Prematurity (ICROP).12 This system classifies ROP by four parameters: location, stage, extent or clock hours of involvement, and the absence or presence of “plus disease”. The disease is described as being located in one of three zones; Zone I, Zone II or Zone III. Zone I is the most posterior and generally most severe location for ROP, Zone II is the most common, intermediate zone for ROP to develop and Zone III is the most peripheral and benign location for ROP to occur.
Several methods were used to measure VA, depending on the patient's age and response. The methods were as follow: Catford drum for babies aged between 6 months and 1 year old, Cardiff acuity test for children from 1 to 2 years old, Sheridan Gardiner for children aged 3 to 4 years old and Sheridan Gardiner or Snellen chart for children aged from 5 to 6 years old. Refraction was determined using retinoscopy. Cycloplegic refraction (with 2 drops of 0.5% cyclopentolate) was performed on all patients during follow-up examination. Myopia was defined as −0.50 dioptres sphere or worse. Hyperopia was defined as + 1.00 dioptres sphere or worse and astigmatism was defined as −1.00 dioptres cylinder or worse. Strabismus was assessed using Hirschberg test followed by cover test. Cover-uncover test was performed to detect manifest deviation of the eye.
The development of visual functions in both groups were analysed using Repeated Measures ANOVA. Parametric (t-test) and non-parametric analysis (Pearson Chi-Square test) were used to compare the difference in visual acuity, refractive status and squint assessment for each year between preterm babies with ROP and without ROP from 1 to 6 years old. Linear regression was performed to analyse the relationship between refractive error and birth weight and severity of ROP.
ResultsA total of 102 preterm babies records were reviewed at the Eye clinic, Hospital Tuanku Jaafar Seremban from January 2000 to Dec 2008. Of these, 48 (47.1%) were males and 54 (52.9) were females. The racial distribution was 60 (58.8%) Malays, 20 (19.6%) Chinese, 21 (20.6%) Indian and 1 (1%) Caucasian. The average gestational age was 30.83±2.42 weeks, ranging from 26 weeks to 36 weeks. The average birth weight was 1.37±0.36 kilograms, ranging from 0.55kg to 2.28kg. The characteristics of the study population are shown in Table 1.
Characteristics of the study population
| Group AWith ROP (n=38) | Group BWithout ROP (n=64) | ||||
| n | % | n | % | ||
| Gender | Gender | ||||
| Male | 17 | 44.7 | Male | 30 | 46.9 |
| Female | 21 | 55.3 | Female | 34 | 53.1 |
| Race | Race | ||||
| Malay | 19 | 50 | Malay | 41 | 64.1 |
| Chinese | 9 | 23.7 | Chinese | 11 | 17.2 |
| Indian | 10 | 26.3 | Indian | 11 | 17.2 |
| Others | − | − | Others | 1 | 1.6 |
| Gestational age | Gestational age | ||||
| < 28 weeks | 11 | 28.9 | < 28 weeks | 1 | 1.6 |
| 28–32 weeks | 23 | 60.6 | 28–32 weeks | 24 | 37.5 |
| > 32 weeks | 4 | 10.5 | > 32 weeks | 39 | 60.9 |
| Birth weight | Birth weight | ||||
| < 1kg | 13 | 34.2 | < 1kg | 3 | 4.7 |
| 1–1.5kg | 22 | 57.6 | 1–1.5kg | 31 | 48.4 |
| > 1.5kg | 3 | 7.9 | > 1.5kg | 30 | 46.9 |
Fundus examination revealed that 38 (37.3%) of the preterm children had ROP. Ten (9.8%) patients developed stage 1 ROP; with 9 (8.8%) patients at zone III and 1 (1%) at zone II. Seventeen (16.6%) patients developed stage 2 ROP with 4 (3.9%) had ROP at zone III and 13 (12.7%) at zone II. Another 11 (10.9%) patients developed stage 3 ROP where 4 (3.9%) of them were at zone III and 7 (6.9%) patients at zone II. The number of preterm children with ROP who required laser therapy was 22 (21.6%). Seventeen (44.7%) males and 21 (55.3%) females were diagnosed with ROP. Another 30 (46.9%) male and 34 (53.1%) female babies did not have ROP.
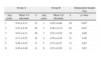
In this report preterm babies with ROP is referred to as Group A and preterm babies without ROP as Group B. Overall, the results showed improvement of the VA in both groups with age. Mean VA at 1 year old for Group A was 0.24±0.12 (6/24) and 0.29±0.09 (6/24) for Group B. At 6 years old, the VA improved to 0.48±0.40 (6/12) for Group A and 0.51±0.20 (6/12) for Group B. Statistical analysis using ANOVA showed no significant difference between both groups (p=0.87). However, significant difference was noted between mean VA of Group A and B for children at the age of 1 year (p=0.03) and 2 years old (p=0.01). Significantly higher VA was noted in 4 years old than other age groups. Mean VA of every age group for both groups is shown in Table 2.
Mean ± SD of VA as a function of age group for preterm children with ROP (Group A) and without ROP (Group B)
| Group A | Group B | Independent Sample Test | ||||
| Age (year) | Mean VA (decimal) | n | Age (year) | Mean VA (decimal) | n | p-value |
| 1 | 0.24±0.12 | 31 | 1 | 0.29±0.09 | 59 | 0.03* |
| 2 | 0.35±0.19 | 36 | 2 | 0.46±0.19 | 62 | 0.01* |
| 3 | 0.53±0.31 | 28 | 3 | 0.54±0.28 | 34 | 0.69 |
| 4 | 0.71±0.55 | 19 | 4 | 0.59±0.29 | 21 | 0.49 |
| 5 | 0.46±0.42 | 13 | 5 | 0.53±0.27 | 13 | 0.62 |
| 6 | 0.48±0.40 | 11 | 6 | 0.51±0.20 | 11 | 0.85 |
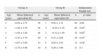
Refraction was recorded as sphere (DS) and astigmatism (DC). Mean spherical equivalent (MSE) at every age group for both groups of children is shown in Table 3. The children in Group A became more myopic as they became older. Their refractive error changed from −0.94 D±2.75 DS at 1 year (n=28) to −2.78 D±4.99 DS (n=10) at 6 years old. The children in Group B became slightly hyperopic as they became older. Their refractive error at 1 year was −0.12 D±1.95 (n=32) and at 6 years old was + 0.26 D ± 3.09 DS (n=11). Statistical analysis showed no significant difference between both groups (p=0.07) and between each age from 1 to 6 years old.
Mean ± SD of refractive error in spherical equivalent (MSE) as a function of age group for preterm children with ROP (Group A) and without ROP (Group B)
| Group A | Group B | Independent Sample test | ||||
| Age (year) | Mean Spherical equivalent (D) | n | Age (year) | Mean Spherical equivalent (D) | n | p-value |
| 1 | −0.94±2.75 | 38 | 1 | 0.01±1.31 | 64 | 0.06 |
| 2 | −1.40±2.79 | 38 | 2 | −0.24±1.45 | 64 | 0.02* |
| 3 | −1.84±3.20 | 28 | 3 | −0.12±1.95 | 32 | 0.02* |
| 4 | −2.45±3.79 | 20 | 4 | 0.21±2.08 | 20 | 0.01* |
| 5 | −4.07±5.69 | 12 | 5 | 0.02±2.83 | 12 | 0.04* |
| 6 | −2.78±4.99 | 10 | 6 | 0.26±3.09 | 11 | 0.1 |
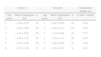
Mean astigmatism in every age group is shown in Table 4. There was no significant increment of astigmatism with age for both groups of children. At 1 year, mean astigmatism for Group A children was −1.20 D±0.79 and for Group B was −0.97 D±0.85. At 6 years old, mean astigmatism for 8 children in Group A was −1.53 D±1.20 and for 8 children in Group B was −1.03 D±0.52. Linear regression was used to evaluate the association between myopia and astigmatism with birth weight and severity of ROP. Degree of myopia was found to be significantly associated with birth weight (p=0.001) and severity of ROP (p=0.001) as shown in figure 1. However, no association was detected between astigmatism with the two factors.
Mean ± SD of astigmatism as a function of age group for preterm children with ROP(Group A) and without ROP (Group B)
| Group A | Group B | Independent Sample test | ||||
| Age (year) | Mean Astigmatism (D) | n | Age (year) | Mean Astigmatism (D) | n | p-value (2-tailed) |
| 1 | −1.20±0.79 | 38 | 1 | −0.97±0.85 | 59 | 0.18 |
| 2 | −1.16±0.96 | 38 | 2 | −0.92±0.71 | 59 | 0.16 |
| 3 | −1.19±0.92 | 28 | 3 | −1.10±0.86 | 24 | 0.77 |
| 4 | −1.36±1.10 | 18 | 4 | −1.39±1.13 | 16 | 0.95 |
| 5 | −1.23±0.98 | 10 | 5 | −1.05±0.92 | 10 | 0.68 |
| 6 | −1.53±1.20 | 8 | 6 | −1.03±0.52 | 8 | 0.31 |
Regarding strabismus, only 13.7% of the children were diagnosed with strabismus. Of those, 9 of them were having esotropia and another 5 exotropia. Statistical analysis showed no significant difference in percentage of strabismus between both groups. Summary of the results as a function of age is shown in Table 5.
DiscussionMalaysia is a multi racial country with predominantly 3 main races, Malay, Chinese and Indian. Data from Malaysia census population and housing reported in 2010 showed that around 49.74% of the population were Malays, 22.8% Chinese and 1.3% Indians.14 The results of this study report on numbers of Malays and Chinese having premature infants and subsequently ROP in comparison to the percentage of both races in Malaysia. The results however were disproportionately higher for the Indians. We were unable to determine the cause of this finding as the parents medical records were not available to us at the time of the study. Theng et al. noted larger percentage of Malays having premature infants than other races in Singapore and attributed the trend to the lower socioeconomic status of Malays in their country.13
Overall, the results of this study showed that VA of preterm children in both groups improved from 1 to 6 years of age. Around 44.2% of the preterm children reached normal vision at 1 year old. The present data also showed that VA among children with ROP was lower than children without ROP at 3, 4, 5 and 6 years. Erickson compared the VA of preterm (without ROP) and full term children at 3, 5 and 6 years old and found that the mean VA in preterm children without ROP in each age group was lower than full term children.15 Sebris et al. measured VA on 23 preterm and full term children at the age of 3 to 4 years old using preferential looking chart and found that the average acuity of the preterm children was slightly poorer than full term children of the same age, even when children with significant refractive errors were eliminated from the sample.16 Unfortunately, we were unable to compare our results with full term children as the data was not available in the clinic.
Myopia is a well known consequence of low birth weight, particularly in patients with ROP. Fledelius compared the refractive error between preterm and full term birth children and concluded that children who were born prematurely and had little or no ROP were likely to develop myopia due to arrested development of the anterior segment.3 O’Connor et al. demonstrated that the prevalence of myopia is higher in preterm children with severe than mild ROP.6 The degree of myopia in preterm children is probably associated with the disease process itself and not the treatment. In a study conducted on preterm infants with birth weights of less than 1251g, Quinn et al. demonstrated higher prevalence of myopia in preterm population compared to full term children.17 Their analysis showed that birth weight and severity of ROP were the predictive factors for the development of myopia in preterm children. Their results were supported by Varghese et al. who showed that the incidence of myopia increased with decreasing weight of preterm infants. The authors concluded that birth weight should be used as criteria for screening for refractive error.9 Results of the present study support these earlier findings. Degree of myopia was found to be inversely related to severity of ROP and birth weight. However, future studies with larger sample size are needed to confirm these findings.
There is another class of myopia associated with preterm birth that is infants born preterm are generally myopic before term but later becomes emmetropic secondary to changes in the ocular structures such as shorter axial length and steeper cornea. Fledelius measured the refractive and biometric status of preterm children at 7 to 10 years old and showed a more curved cornea and shorter axial length than expected from refractive values.18 Sharanjeet et al. compared similar measurements between preterm (without ROP) with full term children and demonstrated insignificant difference in the refractive status but significant difference in the measurements of axial length, corneal curvature and thickness of crystalline lens.19 Premature children were found to have shorter axial length, steeper corneal curvature and thicker crystalline lens than full term children. The authors hypothesized that the differences in the biometric measurements were probably due to the emmetropisation process. This theory was proposed earlier by Saunders et al. who demonstrated that premature babies without ROP achieve emmetropisation by 6 months of age.20 The authors suggested that the emmetropisation is able to correct the refractive error associated with preterm birth in the absence of ROP. Our results however, did not concur with the proposed theory which was probably due to the small number of subjects. Several children in our sample did not turn up for the scheduled follow up examination in the hospital.
Regarding astigmatism and strabismus, no significant difference was detected in the frequencies between preterm children with ROP and without ROP in all age groups. Atkinson et al. demonstrated higher percentage of astigmatism in preterm (21%) than full term children (4–9%).21 However, their results showed lower percentage of strabismus (10%) among preterm children than other reported studies. Other researchers have also found that the rate of strabismus increases with decreasing gestational age.22–24 Such an association was not obvious in this study. This result should be substantiated by future studies with larger samples.
This study describes and highlights the visual problems of preterm children attending a primary eye clinic in south Malaysia. Myopia was found to be associated with birth weight and severity of ROP in preterm children. These factors should be considered during screening of vision and refractive error so that early intervention can be provided to improve the quality of life of these children.
Conflicts of interestsThe authors have no conflicts of interests to declare.
We acknowledged Norlaila Mat Daud and the staff of Eye Clinic, Hospital Tuanku Jaafar, Seremban, Negeri Sembilan for their kind support throughout this study.