To investigate the binocular summation ratio (BSR) in intermittent exotropia (IXT) before and after vision training under varying light conditions, and to evaluate its association with the control of deviation.
MethodsTwenty IXT patients were included in the study. Patients were divided into three groups based on their control of deviation: poor, fair, and good control. Contrast sensitivity was assessed using the CSV1000-HGT chart at four spatial frequencies, evaluated both monocularly and binocularly from a distance of 2.5 meters. This evaluation occurred under both photopic and mesopic lighting conditions, with and without glare. Additionally, the BSR for each patient was calculated before and after the vision training process.
ResultsThe mesopic BSR under glare-free conditions demonstrated a significant increase following vision training. In the presence of glare, the mesopic BSR significantly increased across all spatial frequencies: 3, 6, 12, and 18 cycles/degree. Additionally, after vision training, the photopic BSR in glare-free conditions also showed an increase at all frequencies. However, under glare conditions, the photopic BSR only increased at the frequencies of 3, 12, and 18 cycles/degree, but this increase was not statistically significant. A significant increase in the BSR was observed only at the frequency of 6 cycles/degree. Furthermore, following vision training, the degree of control over deviation improved significantly.
ConclusionThe BSR and deviation control scores in patients diagnosed with IXT demonstrated significant improvement following vision training, underscoring the efficacy of this treatment method in the management of IXT.
Key Points
• Patients with intermittent exotropia demonstrate a significant decrease in binocular summation ratio. This ratio can be significantly improved by enhancing binocular vision through vision training.
• In patients with intermittent exotropia, binocular inhibition may be observed instead of binocular summation. This can be remedied by enhancing the deviation control and facilitating a more efficient form of binocular vision.
• The binocular summation ratio could be a useful criterion for assessing the enhancement of binocular vision following the stabilization of binocular vision in individuals with intermittent exotropia.
Intermittent exotropia (IXT) is a prevalent eye deviation, particularly observed during the first decade of life and more frequently in individuals of Asian descent.1,2 This condition is characterized by the outward deviation of one eye, notably occurring when the individual focuses on distant objects or is inattentive.3
Contrast sensitivity is defined as the ability to perceive subtle differences in shades and patterns. This ability is essential for detecting objects that do not have distinct borders, enabling individuals to differentiate these objects from their backgrounds based on levels of contrast.4
Binocular summation refers to the improved performance achieved when both eyes work together, as opposed to when each eye functions independently. Research indicates that binocular performance can be enhanced by approximately 40% compared to monocular performance.5 However, in patients with intermittent exotropia, the binocular summation ratio (BSR) is considerably lower than that of individuals without this condition.6
Evaluating binocular vision status primarily depends on assessing stereopsis, which has inherent limitations. However, unlike stereopsis, binocular summation is not influenced by monocular cues.7
The subnormal summation ratio of binocular contrast sensitivity in patients with IXT is significantly associated with both stereopsis and the control of deviation. Therefore, it is proposed that the binocular contrast sensitivity test could serve as a valuable tool for assessing binocular vision performance in patients with IXT.6 Furthermore, binocular summation markedly decreases in patients with poor control but can improve following surgical intervention.8,9
Accommodation and convergence exercises performed in the clinic, in conjunction with home-based vision training, significantly enhance the control of exotropia deviation at both far and near distances in patients with exotropia, regardless of their surgical history.10
To the best of our knowledge, no other study has explored how vision training impacts binocular summation in patients with IXT. This study aims to investigate the effects of vision training on both binocular summation and the control of deviation.
Material and methodStudy design and settingThis prospective cohort pilot study was conducted at the optometry clinic of the Mashhad University of Medical Sciences from February 2023 to February 2024.
Ethical approvalThe study protocol received approval from the Ethics Committee of Mashhad University of Medical Sciences (IR.MUMS.MEDICAL.REC.1401.642). Written informed consent was obtained from all IXT patients or their parents. The study methods adhered to the principles outlined in the Declaration of Helsinki.
Eligibility criteriaWe included the participants aged over 7 years (to ensure adequate cooperation), those with corrected monocular and binocular visual acuity of 10/10 or better, and individuals without a history of prior eye surgery. Patients were excluded from the study if they had any underlying systemic or ocular diseases, a history of eye surgery, or were using medications associated with visual blurring. Additional exclusion criteria included amblyopia, anisometropia greater than 2 diopters, refractive errors exceeding 3 diopters, astigmatism over 2 diopters, vertical deviation greater than 5 prism diopters, developmental or neurological disorders, and ocular mechanical or paralytic limitations. Patients demonstrating deep sensory adaptations (e.g., sensory adaptation in complete darkness, indicating profound adaptation) were also excluded, as well as those with convergence insufficiency, defined as a near deviation exceeding a 10-prism diopter difference compared to distance deviation.
ProcedureAt the beginning of the study, all assessments, including visual acuity, cover test, Worth four-dot test, and contrast sensitivity, were conducted with optimal optical correction. Prior to exposing the patient to high-light conditions, deviation at both near and far distances was measured and recorded using the alternate cover test method. Vision training was administered through 10–15 sessions of office-based therapy, each lasting 60 min, supplemented by home-based orthoptic exercises.
The Worth four-dot test was conducted to assess sensory dominance at a distance of 2.5 meters. A red filter was placed in front of the patient's right eye and a green filter in front of the left eye. Patients were instructed to focus on the bottom circle of the Worth four-dot test for a 15-second period and report the color observed. If the patient reported either red or green for more than 10 s, the eye with the corresponding filter was designated as the sensory-dominant eye. If a mixture of both colors was reported, no strong sensory dominance was considered present. This process was repeated three times.11 Deviation control was subsequently rated into three categories: good, fair, and poor.12
Contrast sensitivity was evaluated and recorded using the CSV1000-HGT chart (Vector Vision, Inc., Greenville, OH, USA) at four spatial frequencies (3, 6, 12, and 18 cycles/degree) for both monocular and binocular vision at a distance of 2.5 meters. Testing was conducted under photopic (85 cd/m²) and mesopic (3 cd/m²) lighting conditions, both with and without glare. The BSR for each patient was then calculated using the following method:
Vision training was administered through 10 to 15 office-based sessions, each lasting 60 min, and supplemented by home-based orthoptic exercises. The vision training protocol, detailed in Table 1 of the supplementary file, was followed throughout the study, with exercises continued until satisfactory deviation control was achieved.12
Statistical analysisData normality was evaluated using the Shapiro-Wilk test, histograms, box plots, and kurtosis and skewness indices. Since the data was not normally distributed, we used the Wilcoxon signed-rank test (a non-parametric alternative to the paired t-test) to compare BSR and before and after vision training. A significance threshold of p < 0.05 was applied to all tests. Statistical analyses were carried out using SPSS software, version 23.0.
ResultsTwenty patients (6 men and 14 women) were enrolled in the study, with a median age of 14 years (interquartile range [IQR] = 10–19). Half of the patients were right-eye dominant. None of the patients had a good control score, while 13 (65%) had a fair control score and seven (35%) of them had a poor control score. The participants' baseline characteristics are summarized in Table 1.
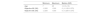
Following vision training, the mesopic BSR without glare showed a significant increase at spatial frequencies of 6 and 18 cycles per degree (p = 0.007, and 0.009, respectively). At frequencies 3 and 12, although an increase in BSR was observed post-training, this change was not statistically significant (p = 0.063 and 0.051, respectively). Under glare conditions, the mesopic BSR significantly increased across all frequencies (3, 6, 12, and 18 cycles per degree), with p < 0.005 in all (Table 2).
Changes in binocular summation ratio (in log contrast), in mesopic and photopic conditions.
| Condition | SF (Cycles/Degree) | Before vision training | After vision training | p-valuea | |
|---|---|---|---|---|---|
| Mesopic | Without glare | 3 | 0.97 | 1.02 | 0.063 |
| 6 | 0.99 | 1.06 | 0.007 | ||
| 12 | 1.01 | 1.07 | 0.051 | ||
| 18 | 0.97 | 1.08 | 0.009 | ||
| With glare | 3 | 0.95 | 1.08 | 0.001 | |
| 6 | 0.89 | 1.08 | < 0.001 | ||
| 12 | 0.81 | 1.16 | < 0.001 | ||
| 18 | 0.73 | 1.12 | 0.005 | ||
| Photopic | Without glare | 3 | 1.02 | 1.05 | 0.314 |
| 6 | 1.02 | 1.04 | 0.203 | ||
| 12 | 1.01 | 1.09 | 0.010 | ||
| 18 | 1.07 | 1.10 | 0.560 | ||
| With glare | 3 | 1.02 | 1.06 | 0.295 | |
| 6 | 1.01 | 1.07 | 0.010 | ||
| 12 | 1.07 | 1.07 | 0.722 | ||
| 18 | 1.05 | 1.11 | 0.201 |
SF, spatial frequency.
Under photopic conditions without glare, the BSR increased at frequencies of 3, 6, and 18 cycles per degree, although these increases were not statistically significant (p = 0.314, 0.203, and 0.560, respectively). At frequency 12, however, the increase in BSR following vision training was statistically significant (p = 0.010) In photopic conditions with glare, increases were observed at frequencies of 3, 12, and 18, though these were not significant (p = 0.2295, 0.722, and 0.201, respectively). A significant increase in binocular summation was noted only at frequency 6 (p = 0.010), as shown in Table 2.
The degree of deviation control improved significantly following vision training and all of the participants reached a good control score. The magnitude of both far and near deviation was also significantly reduced post-training (p < 0.001) (Table 3).
Changes in far and near deviation.
| Type | Before vision training | After vision training | p-valueb | |
|---|---|---|---|---|
| Deviation | Far | 23.2 | 11.8 | < 0.001 |
| Near | 15.2 | 4.8 | < 0.001 |
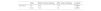
Comparison of changes in binocular summation ratio, in glare and without glare conditions showed a significant difference between photopic and mesopic in glare conditions at 3, 6, and 12 CPDs (p = 0.004, 0.036, and <0.001, respectively), while this difference was not significant in without glare condition and glare condition at 18 CPD (Table 4).
Comparison of changes in binocular summation ratio (in Log contrast), in glare and without glare conditions.
| SF (Cycles/Degree) | Photopic | Mesopic | p-valuea | |
|---|---|---|---|---|
| Without glare | 3 | 0.029 | 0.048 | 0.625 |
| 6 | 0.025 | 0.067 | 0.178 | |
| 12 | 0.071 | 0.055 | 0.970 | |
| 18 | 0.027 | 0.105 | 0.758 | |
| With glare | 3 | 0.039 | 0.135 | 0.004 |
| 6 | 0.061 | 0.189 | 0.036 | |
| 12 | −0.004 | 0.346 | < 0.001 | |
| 18 | 0.069 | 0.383 | 0.052 |
SF, spatial frequency; BSR, binocular summation ratio.
A significant decrease in binocular summation under low contrast sensitivity in patients with IXT who had higher deviation control scores may suggest a link between reduced binocular summation and poor deviation control.9 In our study, a notable reduction in binocular summation was observed before vision training, corresponding with weaker deviation control. However, following vision training, a marked improvement in deviation control was accompanied by a significant enhancement in binocular summation.
Strabismic patients exhibit subnormal binocular summation or even binocular inhibition at low contrast acuity levels, suggesting a more extensive impairment in strabismus than previously recognized.13 In the present study, binocular summation ratios decreased across all lighting conditions, with a particularly notable reduction under mesopic conditions. Ratios below 1 were observed, indicating a state of binocular inhibition rather than summation.
Kwon et al. found that reduced stereopsis was associated with lower contrast sensitivity, while improved fusional stability corresponded with better contrast sensitivity under mesopic light conditions. Consequently, contrast sensitivity testing may serve as a valuable tool for assessing sensory function in patients with IXT.14 Similar findings were observed in our study: under mesopic lighting and with glare across all frequencies, IXT patients exhibited significant reductions in binocular contrast sensitivity and binocular summation ratio, effectively indicating binocular inhibition rather than summation. However, after enhanced deviation control and strengthened fusional reserves, significant improvements in binocular contrast sensitivity and binocular summation were observed under both photopic and, notably, mesopic conditions.
In patients with IXT, subnormal binocular contrast sensitivity summation ratios were correlated with deviation control scores, suggesting that binocular contrast sensitivity testing may be an effective tool for assessing binocular vision performance in IXT patients.3 The present study demonstrated that poorer deviation control is associated with a reduced binocular summation ratio, while improved deviation control corresponds with an increased ratio.
Formerly Kwon et al. showed that in IXT patients contrast sensitivity is lower than normal levels in glare conditions and patients with photophobia showed worse contrast sensitivity under mesopic conditions with glare.14 In our study, we observed that contrast sensitivity and consequently BSR significantly improved at low and medium spatial frequencies under glare conditions after vision training. However, under no-glare conditions, the changes were not significant. Therefore, it seems that this vision training would be beneficial for improving binocular contrast sensitivity and consequently BSR.
Office-based vergence and accommodation exercises, when combined with home-based orthoptic exercises, significantly enhance both near and far exodeviation control in patients with IXT, regardless of surgical history.10 In the present study, regular clinic-based exercises, supplemented by at-home orthoptic exercises, significantly reduced deviation magnitude and markedly improved deviation control in IXT patients.
In the study by Martin Ming-Leung Ma et al.,15 children aged 6 to 18 years with IXT, underwent a 12-week vergence/accommodation therapy program, both in the clinic and at home, resulting in statistically and clinically significant improvements in distance control and deviation magnitude. In our study, 15 sessions of combined clinic-based and home orthoptic exercises similarly produced substantial improvement in near and far deviation control, alongside a significant reduction in the near and far deviation angles.
A normal BSR observed in post-surgical patients with IXT suggests that the visual cortex remains functionally intact at the threshold level of contrast sensitivity for binocular information processing.16 In the present study, following vision training and enhanced deviation control, binocular vision efficiency showed a significant increase in the binocular summation ratio, particularly in conditions that had previously exhibited a marked decline. Binocular inhibition was effectively replaced by binocular summation, indicating that the visual cortex retained its capacity for binocular processing and restored it to a normal or near-normal level.
A significant correlation was found between photophobia reported by parents of children with IXT and photophobia (measured as binocular contrast sensitivity) at a spatial frequency of 6 cycles per degree (CPD) under mesopic conditions (p = 0.002, r = 0.622). This sensitivity significantly improved following strabismus surgery (p = 0.003 at 6 CPD).17 In the present study, similar findings were observed under glare conditions in both mesopic and photopic lighting. After vision training, improvements in binocular contrast sensitivity were accompanied by a significant increase in the BSR at 6 CPD. This suggests that the reduction in the BSR at 6 CPD may be linked to the transient eye closure in IXT patients, and the improvement in this ratio may correspond with a reduction in photophobia symptoms.
As a proposed approach, the correlation between transient eye closure in patients with IXT and the BSR could be systematically assessed both before and after vision training or strabismus surgery.
This study has several strengths. First, it addresses a novel aspect of binocular vision by investigating the effects of vision training on binocular summation in patients with IXT, an area that has not been extensively explored. Second, the study has significant clinical relevance, as the findings suggest that vision training can improve both binocular summation and deviation control, offering a potential non-surgical treatment option for IXT patients. Third, utilizing objective and quantitative measurements, such as contrast sensitivity testing with the CSV1000-HGT chart, enhances the reliability and reproducibility of the results. Additionally, the study design includes a comprehensive evaluation of BSR under varying lighting conditions (photopic vs. mesopic) and glare settings, providing a thorough assessment of binocular vision performance. Moreover, the combination of office-based and home-based vision training enhances the practical applicability of the findings in real-world clinical settings. However, some limitations should be considered. The small sample size (n = 20) limits the generalizability of the findings, and a larger cohort is needed to confirm these results. Additionally, the lack of a control group prevents direct comparisons between the natural progression of IXT and the effects of vision training. Another limitation is the relatively short follow-up period, which does not provide insight into the long-term stability of the improvements in BSR and deviation control.
ConclusionThis study demonstrates that vision training significantly improves the BSR and deviation control in patients with IXT, suggesting its potential as a non-surgical intervention to enhance binocular function. Given its clinical applicability, vision training may be integrated into treatment plans to improve contrast sensitivity and fusion stability, particularly in patients with poor deviation control. However, as our study focused on short-term outcomes, future research with larger sample sizes, control groups, and long-term follow-up is needed to confirm the persistence of these improvements.
DeclarationsAvailability of data and materialsThe datasets used and/or analyzed during the current study will be available from the corresponding author upon reasonable request.
FundingThis study was funded by the Mashhad University of Medical Sciences (Grant number: 4,010,533).
Consent for publicationNot applicable.
Declaration of generative AI and AI-assisted technologies in the writing processDuring the preparation of this work the authors used ChatGPT (developed by OpenAI, 2025) in order to improve the readability and language of this paper. After using this tool, the authors reviewed and edited the content as needed and take full responsibility for the content of the published article.
The authors would like to thank the optometry clinic of the Mashhad University of Medical Sciences staff for their help.