To determine whether the Melbourne Low Vision Index (MLVI) can be used to characterise the ability to carry out Activities of Daily Living (ADL) in a group of older people with age-related macular degeneration (AMD) which was reflective of actual day-to-day function according to in-depth interviews which encompassed questions about personal and environmental coping strategies.
MethodThirty-one individuals (23 females, 8 males, aged 79.1±5.6 years) with AMD (16 dry, 15 wet) and no other ocular diseases underwent tests of clinical visual function, the MLVI and a semi-structured interview intended to highlight functionality in the home environment.
ResultsParticipants’ clinical visual measures were correlated with MLVI score such that poorer visual function was associated with poorer functional ability for daily living activities (p<0.05). Moreover, part (a) of the MLVI, which is assessed by observation of task performance, has a significant correlation with the severity of AMD (p<0.05). Semi-structured interviews revealed a mismatch between MLVI part (a) and self-reported functionality in their own home environment.
ConclusionLow functionality score (total) with MLVI is associated with severity of AMD and poor clinical visual function. The disparity between observed measures of functional vision (MLVI part (a)) and self-reported measures in the MLVI and in the semi-structured interviews may be explained in part by individual participant coping and adaptation strategies. The MLVI is therefore reflective of function in unfamiliar environments where people with low vision may not have recourse to compensatory strategies.
Determinar si el Índice de Baja Visión de Melbourne (MLVI) podría utilizarse para calificar la capacidad de llevar a cabo actividades de la vida diaria en un grupo de personas mayores con degeneración macular asociada a la edad (DMAE) y su reflejo en la función diaria, mediante entrevistas detalladas y preguntas relativas a las estrategias de defensa ambientales y personales.
MétodoTreinta y un pacientes (23 mujeres, 8 varones, edad 79,1 ± 5,6 años) con DMAE (16 seca, 15 húmeda) y sin otras enfermedades oculares fueron sometidos a pruebas clínicas de la función visual, al MLVI y a una entrevista semi-estructurada de cara a caracterizar la funcionalidad en el entorno doméstico.
ResultadosLas mediciones clínicas visuales de los participantes guardaron una correlación con la puntuación del MLVI de modo que una función visual visual más pobre estaba asociada con una capacidad funcional más débil para las actividades de la vida diaria (p<0,05). Además, la parte (a) del MLVI, evaluada mediante observación de la ejecución de tareas, guardó una correlación con la severidad de la DMAE (p<0,05). Las entrevistas semi-estructuradas revelaron un desfase entre la parte (a) del MLVI y la funcionalidad auto-evaluada en el propio entorno doméstico de los participantes.
ConclusiónLa puntuación (total) de baja funcionalidad junto con el MLVI se asocia con la severidad de la DMAE y una débil función visual. La disparidad entre las mediciones observadas de la función visual (parte (a) del MLVI) y las mediciones auto-evaluadas en el MLVI y en las entrevistas semi-estructuradas pueden explicarse, en parte, por las estrategias de defensa y adaptación de los participantes. Por tanto, el MLVI es, por tanto, un reflejo de la funcionalidad en entornos desconocidos, en los que las personas con baja visión no poseen recursos en cuanto a estrategias compensatorias.
AMD causes progressive macular damage, resulting in loss of central vision which affects the ability to read, to recognise faces and objects, to drive and to write using fine detail.1,2 Other activities such as moving around, crossing streets and driving are also difficult for people with this visual impairment.3 Social isolation and depression are additional impacts of this vision loss.4,5 The risk of falling and fractures is a problem for the elderly with visual impairment.6,7 As a result, functional problems in performing daily living activities are a current and real challenge for people with AMD.8
It has been recognised that quantifying clinical visual function measures alone is not enough to characterise the ability of people with visual impairment to perform daily living activities.9 An appropriate assessment of visual impairment must include vision-related skills and abilities in performing daily living activities.10 Therefore the term ‘functional vision’ describes functions with regard to vision-related activities, and includes activities such as reading, writing, and face recognition and so on. These activities reflect “person” function, rather than just visual function. Many activity of daily living (ADL) instruments have been developed to measure functional vision and quality of life in people with visual impairment.11 The majority of these instruments employ a method of patient self-report regarding their vision impairment comprising general sets of questions about the individual's reported vision impairment. Instruments which employ both self-report and performance-based measures are expected to provide greater information about a person's ability to carry out daily living activities as these two kinds of measures are complementary.
The Melbourne Low Vision Index (MLVI) is one such instrument which incorporates both self-report and performance-based measures which aims to describe the ability to carry out ADLs by people with vision impairment.12 The MLVI instrument comprises two parts. In part (a), functional vision is quantified by evaluating the ability of the participant to perform 16 items of common daily living activities. In part (b), the participant answers nine questions, rating themselves on their ability to perform activities. The maximum score in part (a) is 64 and in part (b) is 36.
The aim of this research was to determine whether the MLVI could be used to characterise the ability to carry out ADL in a group of older people with AMD which was reflective of actual day-to-day function according to in-depth interviews which encompassed questions about personal and environmental coping strategies.
MethodParticipantsIn this study people with a diagnosis of AMD were recruited from the University of New South Wales (UNSW) School of Optometry and Vision Science low vision clinic and through the Macular Degeneration Foundation (Sydney, Australia) by mail out of invitation letters.
The inclusion criteria for the participants were a diagnosis of AMD and no other ocular or visual diseases, able to hear well enough (with or without hearing aid), and no cognitive problem. The Mini Mental State Examination (MMSE) was applied in order to assess current cognitive status.13 No one was excluded from the study on the basis of poor hearing or cognitive problems, although a few participants wore hearing aids. General health was assessed by self-report.
The method for this study was approved by the Human Research Ethics Advisory Panel, UNSW and all participants gave their informed consent.
ProcedureThe letter of invitation, information sheets, flyer and consent form were sent to the MD Foundation and then they sent all letters of invitation to eligible people who had already been recognised as people with MD. Data collection took place in the School of Optometry and Vision Science Clinic at UNSW over the period August–December 2008.
The first step was explaining the study, signing consent form and clinical measurements (visual acuity, contrast sensitivity, visual field). The MLVI instrument and semi-structured interview were then conducted. The final test was the retinal photograph. All data collection was by the first author.
Visual function measuresHabitual distance vision (McMonnies and Ho chart, UNSW, Sydney), near vision (logMAR word reading chart), static contrast sensitivity (Melbourne Edge Test), visual fields (Humphrey Visual Field Analyser, Carl Zeiss Group, Oberkochen) and confrontation visual fields were assessed. Retinal photographs were taken with a Kowa Nonmyd 7 camera (Kowa, Nagoya) for grading of AMD pathology according to AREDS criteria.14 Habitual vision was assessed in order to reflect the conditions under which the participants were currently living and carrying out their daily living activities. This study measured vision function monocularly and the correlation study was performed with average of both eye measures. The correlation study with better eye shows similar finding.
MLVI tests of functional visionThis instrument,12 compared with other currently available ADL instruments, has both performance-based and self-reported measures of ability to perform various daily living activities. MLVI part (a) measures functional vision by evaluating the ability of the participant to perform 16 items of common daily living activities, such as recognising faces; identifying money and supermarket labels; reading letters, an account, medicine labels, newspaper print size, headlines, and a digital alarm clock; finding telephone numbers in the telephone book; dialling the telephone; writing; telling the time with a wall clock and with wrist watches; pouring water; and threading a needle. MLVI part (b) comprises the participants’ self-reported functional impairment regarding daily activities. This part has nine questions where the participant was asked to rate his or her own ability to perform the following activities: shopping, preparing a meal, doing housework, taking medicine, dressing, grooming, going outdoors, eating, and bathing. Scores from part (a and b) are then transferred to a score sheet for data analysis. The maximum score in part (a) is 64 and in part (b) is 36. A score of 100 indicates no disability in performing daily living activities.
Firstly, the participants were asked to carry out the specific tasks of part (a) of the MLVI just as they would in everyday life. They were reminded that the test would be timed. It was emphasised that the test was not about how quickly they could do a task, but about how they would usually do a task. According to the scoring system of this test, there is a time limit for performing each task.12
The rated ability for all items in part (a) is between 0 and 4, where a score of 0 ‘shows very unsatisfactory result’, 1 ‘shows unsatisfactory result’, 2 ‘shows borderline result’, 3 ‘shows satisfactory result’ and 4 ‘shows very satisfactory result’. Whilst the other items each have their own instructions, time limit and specific answers, the ability rating for all 16 items is the same. Scores from each item are summed to obtain the part (a) score.
MLVI part (b) is a questionnaire and was designed to cover basic self-care ADL and was carried out after MLVI part (a). There are five possible scoring answers for each question. The best score is 4, which shows an ability to perform the task without help, quick and efficiently; score 3 means there is an ability to complete the task without help but a little slowly; score 2 shows that participant needs help or needs someone with him/her for all shopping; score 1 indicates the participant needs a great deal of help; and finally, score 0 reflects a complete inability in doing any of the tasks. All participants reported that their difficulties were entirely due to vision. Scores from individual items are summed to obtain the part (b) score. As the number of participants in the present study is too low to apply the Rasch model, the non-parametric approach of analysing the data during correlation analyses was used in recognition that the scale used was ordinal in the MLVI.
Semi-structured interviews were conducted individually and audio taped and analysed as to whether they did or did not support MLVI responses of individual items. Questions were asked about whether they had any difficulties in their daily living activities. The interview comprised a set of open-ended questions where the participants were asked to describe their current home environment and report any strategies or difficulties encountered when carrying out tasks. The interviewer asked about the home modifications that had been made using a room-by-room sequence starting with the approach to the home followed by the front door, hallway, bathroom and toilet, kitchen, stairs, windows, doors and bedroom. Questions regarding each room were structured to distinguish between those home modifications regarded as useful and which are related to their vision and those which are not. For example, when asking about the approach to the home, the following questions were asked: “Tell me about your vision problems when you enter your home from the street? What do you find easy to see and difficult to see in the walkways, steps and curb? How may they be a risk or hazard? What kind of modification would make it easier to remove or reduce the risk? What is your strategy to cope with this problem? What should be installed or removed from this area to make it more friendly to you?” The interview was designed to elicit responses specifically about what is easy and difficult to see and the changes which can be made in behaviour and the home environment which reduce the difficulties due to vision, rather than other reasons. The final question asked participants “Is there anything else that you would like to say about your point of view in respect of modification, which may be helpful for future provision of information for people with visual impairment?”
In this way, data about a participant's experiences with home modification and difficulties in performing daily living activities were obtained. The interviews were recorded and then transcribed into text using Microsoft Word. Professional transcribers were employed. All transcriptions were then entered into Qualitative Research Study (QSR) Nvivo 8 software for data analysis, which was performed with systematic examination of the transcription in order to find codes, themes and to develop categories. Similar themes, thoughts and points of view were identified with the Nvivo software. Furthermore, the interviews from individual participant were cross-checked with their MLVI part (a and b) responses to individual items for agreement or disagreement as to how functional they were for various daily living activities.
ResultsThirty-one participants (23 women and 8 men) with mean age 79.1 years (SD=5.6) participated in this study (N=31). The mean ages of females and males were 78.7 years (SD=6.00) and 80.5 years (SD=4.5), respectively. Demographic characteristics revealed that 60% of participants had primary and secondary levels of education and 40% of participants had no formal education. 70% of participants lived alone and 30% lived with a family member. 29% of participants were married, 32% were widow and 39% were divorced or single. Also, 52% of participants lived in house and 48% in unit. Finally, 52% of participants had dry macular degeneration (MD) whereas 48% had wet MD. All of the participants had no problems with cognition as indicated by the MMSE.
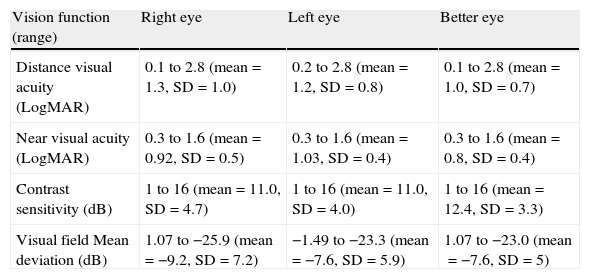
Visual function characteristics of the sampleHabitual distance and near visual acuity ranged from 0.1 to 2.8 logMAR. The results for better eye showed similar range. Table 1 indicates the details of these findings. The participants had visual impairment as defined by the World Health Organisation (WHO) due to reduced visual acuity.15 While 19.4% of participants were blind, AMD severities were level 1 (4 eyes), level two (18 eyes), level three (17 eyes) and advanced (14 eyes) using Age-Related Eye Disease Study AREDs (2001) criteria.
Results from vision function.
| Vision function (range) | Right eye | Left eye | Better eye |
| Distance visual acuity (LogMAR) | 0.1 to 2.8 (mean=1.3, SD=1.0) | 0.2 to 2.8 (mean=1.2, SD=0.8) | 0.1 to 2.8 (mean=1.0, SD=0.7) |
| Near visual acuity (LogMAR) | 0.3 to 1.6 (mean=0.92, SD=0.5) | 0.3 to 1.6 (mean=1.03, SD=0.4) | 0.3 to 1.6 (mean=0.8, SD=0.4) |
| Contrast sensitivity (dB) | 1 to 16 (mean=11.0, SD=4.7) | 1 to 16 (mean=11.0, SD=4.0) | 1 to 16 (mean=12.4, SD=3.3) |
| Visual field Mean deviation (dB) | 1.07 to −25.9 (mean=−9.2, SD=7.2) | −1.49 to −23.3 (mean=−7.6, SD=5.9) | 1.07 to −23.0 (mean=−7.6, SD=5) |
The results of the Melbourne Edge Test (MET) ranged from 1 to 16dB (Table 1). The normal value of MET for people younger than 65 years should be at least 18dB and for those over than 65 years should be at least 16–17dB.16,17 The results showed that 88.7% of participants had a reduction in contrast sensitivity. However, 11.3% of participants had contrast sensitivity within normal ranges.
Mean deviation of visual fields tested ranged from 1.07 to −25.9dB (Table 1). Peripheral visual fields, assessed using confrontation, showed no losses in all the participants.
Functional vision with MLVIThe results from the MLVI show relatively high performance scores among these participants with AMD. For example, more than 60% of participants achieved a test score of more than 70, indicating that participants were functional in performing many items of the MLVI instrument and according to self-report. For instance, the majority of participants had high performance scores (4 out of 4) in activities such as reading a digital alarm clock; reading newspaper headlines; dialling; identifying coins and supermarket labels; recognising faces; and pouring water. However, they had low scores (0 out of 4) in activities such as reading a telephone book; reading a newspaper; and threading a sewing needle. The total score for MLVI ranged from 36 to 100 (mean=72.7, SD=16.1), with the score for part (a) (observed items) ranging from 13 to 64 (mean=45.5, SD=14.0) and for part (b) (questionnaire) ranging from 18 to 36 (mean=27.3, SD=4.9).
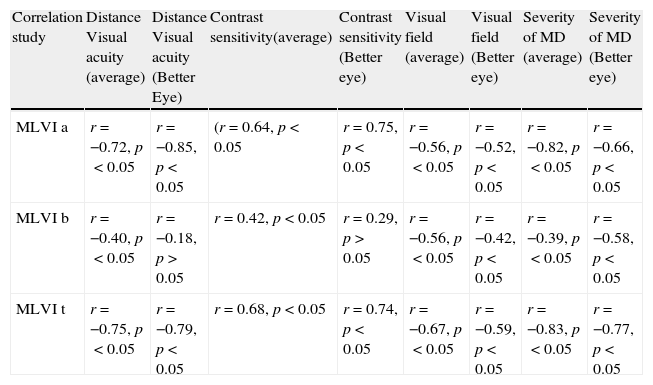
The MLVI scores demonstrate a significant correlation with distance habitual visual acuity, contrast sensitivity, mean deviation of visual field and the severity of the AMD indicating that inability in performing daily tasks is associated with visual impairment. The correlation study with better eye shows similar finding. The details of correlation study can be seen in Table 2.
Correlation between MLVI scores, vision function and severity of MD.
| Correlation study | Distance Visual acuity (average) | Distance Visual acuity (Better Eye) | Contrast sensitivity(average) | Contrast sensitivity (Better eye) | Visual field (average) | Visual field (Better eye) | Severity of MD (average) | Severity of MD (Better eye) |
| MLVI a | r=−0.72, p<0.05 | r=−0.85, p<0.05 | (r=0.64, p<0.05 | r=0.75, p<0.05 | r=−0.56, p<0.05 | r=−0.52, p<0.05 | r=−0.82, p<0.05 | r=−0.66, p<0.05 |
| MLVI b | r=−0.40, p<0.05 | r=−0.18, p>0.05 | r=0.42, p<0.05 | r=0.29, p>0.05 | r=−0.56, p<0.05 | r=−0.42, p<0.05 | r=−0.39, p<0.05 | r=−0.58, p<0.05 |
| MLVI t | r=−0.75, p<0.05 | r=−0.79, p<0.05 | r=0.68, p<0.05 | r=0.74, p<0.05 | r=−0.67, p<0.05 | r=−0.59, p<0.05 | r=−0.83, p<0.05 | r=−0.77, p<0.05 |
The semi-structured interviews reveal that the ADLs which were most problematic for nearly all participants were doing fine activities such as reading small print size materials and sewing. Other important problems were applying make-up, inserting plugs into sockets, inability to find an object within a cluttered environment, difficulty inserting keys into keyholes, difficulty in using elevators due to an inability to read the print material on the buttons and an inability to recognise faces. The participants also had difficulties with use of remote controls of home appliance. As a result, items in part (a) were addressed by the MLVI with the exception of inserting plugs into sockets, finding objects in cluttered environments, using elevators and remote controls.
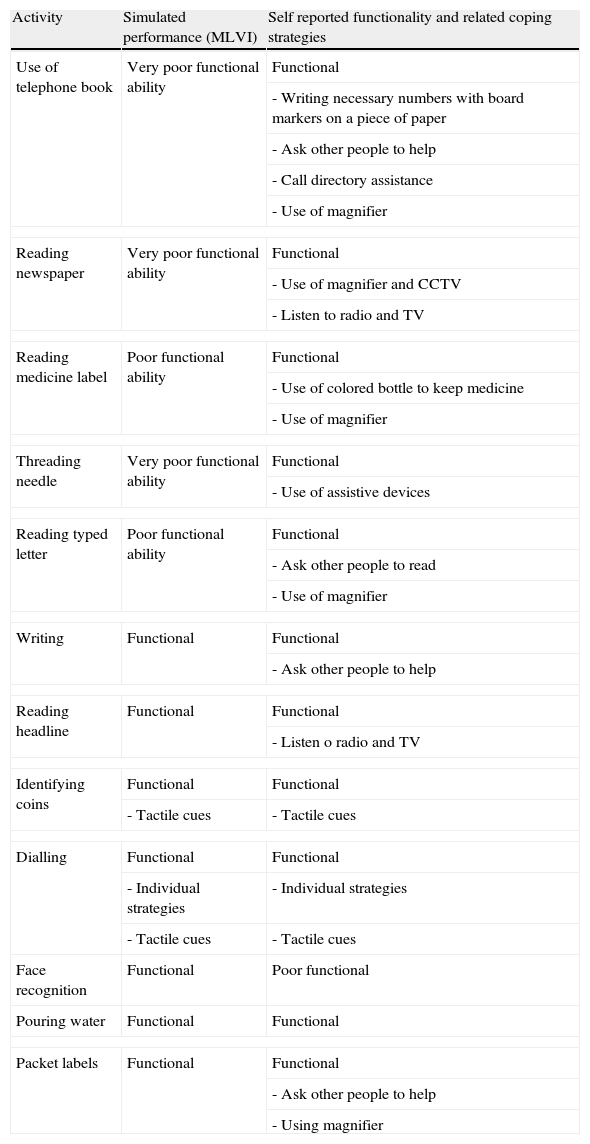
Cross-checking between the MLVI and semi-structured interview results indicated that there were many instances where the MLVI part (a) disagreed with the participant's self-report during the semi-structured interviews and during part (b) of the MLVI and a few instances where they agreed. These instances are listed in Table 3.
Examples of matches and mismatches in functionality in performance activity (simulated and self reported) of participants.
| Activity | Simulated performance (MLVI) | Self reported functionality and related coping strategies |
| Use of telephone book | Very poor functional ability | Functional |
| - Writing necessary numbers with board markers on a piece of paper | ||
| - Ask other people to help | ||
| - Call directory assistance | ||
| - Use of magnifier | ||
| Reading newspaper | Very poor functional ability | Functional |
| - Use of magnifier and CCTV | ||
| - Listen to radio and TV | ||
| Reading medicine label | Poor functional ability | Functional |
| - Use of colored bottle to keep medicine | ||
| - Use of magnifier | ||
| Threading needle | Very poor functional ability | Functional |
| - Use of assistive devices | ||
| Reading typed letter | Poor functional ability | Functional |
| - Ask other people to read | ||
| - Use of magnifier | ||
| Writing | Functional | Functional |
| - Ask other people to help | ||
| Reading headline | Functional | Functional |
| - Listen o radio and TV | ||
| Identifying coins | Functional | Functional |
| - Tactile cues | - Tactile cues | |
| Dialling | Functional | Functional |
| - Individual strategies | - Individual strategies | |
| - Tactile cues | - Tactile cues | |
| Face recognition | Functional | Poor functional |
| Pouring water | Functional | Functional |
| Packet labels | Functional | Functional |
| - Ask other people to help | ||
| - Using magnifier | ||
The results indicate that the participants had a wide range of severity of AMD as assessed using both AREDS criteria and clinical visual function measures. These measures were significantly correlated with MLVI scores such people with low severity AMD were more functional when using this test than those with high severity AMD. The results from the visual function tests correlate with the severity of AMD such that as AMD becomes more severe, by evaluation of fundus images, there is a greater reduction in the visual function.
The MLVI results are significantly correlated with decrease of visual acuity, contrast sensitivity and visual field and are consistent with the results from another study which used the MLVI to assess a mixed low vision population.18 Based on the results of that study, it was predicted that any reduction in visual acuity and contrast sensitivity may be associated with a low performance score. Our results indicate that there is a significant correlation between a low MLVI score and poor habitual visual acuity as few participants with poor visual acuity achieved relatively high-test scores with exceptions. For example, ADLs such as dialling the telephone, pouring water or identifying coins were found not to be problems for the participants. It is difficult to determine what minimum levels of visual acuity are needed to perform these tasks as other senses may assist. For example, the use of tactile strategies for identifying coins or dialling rather than using vision may lead to better functionality and, consequently, to better test scores. Pouring water to a desired level in a container such as a cup is a low contrast task but people may perform this activity using tactile or auditory strategies or make use of long-term experiences of water pouring to assist performance without significant problems despite the vision impairment. It should be noted that this strategy might be not applicable when pouring hot water because of safety issues. As expected, other items, such as threading a needle, finding telephone numbers in a telephone book and reading a newspaper, are assisted less by non-vision strategies.
In addition, the results indicated that a high level of visual acuity does not necessarily indicate a high level of ability to perform tasks such as reading documents, as scored by self-report in part (b) of the MLVI, which is likely to be due to differences in testing condition. For example, the ability to read documents may be reported as poor by the participants because their home lighting may not be adequate for these activities resulting in poorer self-reported performance than an MLVI task performance.19Table 3 shows that participants had poor function in the performance of some activities in the MLVI, but they reported themselves functional through interview. The reasons for the better functionality for these ADLs is given in Table 3 and ranged from using low vision aids, assistive devices, help from other people and alternative senses (e.g. listening to the radio, television, talking clocks). On the other hand, performance of some items of MLVI was easy for participants compared with the similar activities in daily life. For example recognizing faces in the MLVI was easy for participants, but many of participants reported themselves unable to recognize faces in their daily life perhaps being very close to the photograph may result in better recognition. Also photos have higher contrast than looking at real people under natural lighting and this may result in better recognition. The last reason may be the use of celebrity photographs in the MLVI who are easily recognizable people (Table 3). Moreover, the use of appropriate devices, such as using split-head needles when sewing, or exercising creativity to develop coping strategies, such as only buying food which needs to be reheated, was found to increase functionality.20
While there are a few tasks in daily activities, such as reading, that are highly vision-related, it should be kept in mind that MLVI part (a) is a performance-based section and the practitioners should rate the performance, while MLVI part (b) is a self-reported impairment section. The results from part (b) reflect that most of the participants self-reported high functionality in performing daily living activities. Although it was expected that the performance score from part (a) would work in association with the self-reported score (part b), for some ADLs, the participants report themselves more functional. One explanation for this finding may be related to adaptation strategies, for example, a participant may have been unable to read the medicine label in part (a) of the MLVI, but reports themselves as functional with reading their medicine label in part (b) and in the interview as they had additional strategies such as using coloured bottles with large print labels to help them read their medication. In addition, mismatches between self-reported and measured functionality may be due to participants being inaccurate in the perception and/or reporting of their own ability. Another possible reason is that performing the specific ADL items of part (a) and making a self-report of functional vision may involve different skill sets. For instance some activities tested in part (a) such as reading, require visual skills while other activities tested in part (b), such as shopping, preparing a meal, grooming, dressing, need physical and mobility skills in addition to visual skills.21 Therefore participants reported themselves more functional in part (b) because they may have been physically able to do the tasks of shopping and preparing a meal, even though their vision was impaired. In this way, part (b)’s assessment of self-reported ability to perform daily living activities encompasses at the very least both vision and mobility skills while part (a) examines visual skills which do not require mobility.
The results from the individual interviews indicate that living long-term with vision loss provides experiences that lead to functional adaptations in daily life. Coping strategies with vision loss differ among the participants. Most of these strategies were invented individually and are used because they result in positive impacts on their daily living activities. Although visual function is related to functional vision, poor visual function does not necessarily lead to an inability of performing daily living activities in people with visual impairment. This study highlighted a case report regarding the positive impact of coping strategies and use of appropriate assistive devices on daily living activities.20 Unfortunately, these strategies may not be identified through functional vision assessment with currently available instruments such as the MLVI. Furthermore, participants had other difficulties in their life which cannot be measured by MLVI, such as difficulty in inserting plugs into sockets, inability to find something in the clutter difficulty in inserting keys into keyhole, difficulty in using lifts due to an inability to read the print material on the buttons and an inability to recognise faces. Participants had individual strategies to cope with these difficulties. In addition, the majority of participants had difficulties with use of remote controls of home appliance which was not addressed by the MLVI.
The results from the functional vision assessment indicate that the use of part (b) in the MLVI is the strength of the instrument as it provides information which includes participant coping strategies. Part (a) of the MLVI, as it was administered in this study without the use of low vision aids, provides an indication of functionality in ADLs in unfamiliar environments and without low vision aids. Researchers and clinicians who use this tool must take care to also ask participants whether they have any coping strategies in order to understand whether their patients with low vision are functional in their own home and other familiar environments.
ConclusionThere is a significant correlation between severity of AMD, reduced clinical visual function measures and inability in performing tasks with MLVI. However, self-reported functionality may disagree with performance measures of the MLVI as the simulated tests of ADL in part (a) are not reflective of adaptation and coping strategies which people with AMD may employ in their own home to improve functionality. These strategies are not limited to low vision aids.
Conflicts of interestBaqiyatallah University of Medical Sciences has given financial support for the first author.
The authors would like to thank the MD Foundation for assistance in recruiting participants, Vision Australia for assistance with transcribing of interviews, Dr. Sharon Haymes for a copy of the MLVI and Dr. Arthur Ho for the McMonnies-Ho visual acuity chart. Special thanks to Baqiyatallah University of Medical Sciences for their financial support of the first author.