To examine the biometric characteristics of the anterior segment in a group of Sahrawi children.
MethodsA total of 66 children (33 male and 33 female, aged between 8 and 13 years) participated in this prospective, observational study. The non-invasive Pentacam Scheimpflug imaging device was used to measure corneal thickness (CT) (at the thinnest corneal point), mean anterior (Km Ant) and posterior (Km Post) corneal radii, corneal volume (CVol), anterior chamber depth (ACD) and anterior chamber volume (ACVol). The contribution of age and gender to the various parameters was investigated.
ResultsCT values of the present group of Sahrawi children were 521.70±3.92μm. Boys had thicker corneas than girls, although this difference was not significant. Strong correlations were revealed between CT and CVol (r=0.835; p<0.001), as well as between anterior and posterior corneal radii (r=0.916; p<0.001) and between ACD and ACVol (r=0.845; p<0.001). Weaker, but significant correlations were encountered between several other pairs of ocular parameters. Age and gender were found to influence ACD and ACVol values.
ConclusionsDifferent measurement procedures and ethnic background preclude any direct comparison of the present results with published data, although CT in Sahrawi children was found to be lower than previously reported in children of similar age but different ethnicity.
Examinar las características biométricas del segmento anterior en un grupo de niños Saharauis.
MétodosEn este estudio prospectivo y observacional participaron un total de 66 niños (33 varones y 33 hembras, con edades comprendidas entre 8 y 13 años). Se utilizó el dispositivo no invasivo de imagen Scheimpflug Pentacam para la medición del grosor corneal (en el punto corneal más delgado), los radios corneales medios anterior (Km Ant) y posterior (Km Post), el volumen corneal (CVol), la profundidad de la cámara anterior (ACD) y el volumen de la cámara anterior (ACVol). Se investigó la contribución de la edad y el sexo a los diversos parámetros.
ResultadosLos valores del grosor corneal del presente grupo de niños Saharauis fueron de 521,70±3,92μm. Los niños tenían unas córneas más gruesas que las niñas, aunque la diferencia no era significativa. Se hallaron unas fuertes correlaciones entre el grosor corneal y el volumen corneal (r=0,835; p<0,001), así como entre los radios corneales anterior y posterior (r=0,916; p<0,001), y entre la profundidad y el volumen de la cámara anterior (r=0,845; p<0,001). Se hallaron unas correlaciones más débiles, aunque significativas, entre otros pares de parámetros oculares. Se comprobó que la edad y el sexo influían en los valores de la profundidad y el volumen de la cámara anterior.
ConclusionesLos diferentes procedimientos de medición y los orígenes étnicos descartan cualquier comparación directa de los presentes resultados con los datos publicados, aunque se comprobó que el grosor corneal en los niños Saharauis era menor que el anteriormente reportado en niños de edades similares pero de diferente etnia.
For many years, ultrasound techniques have been considered the gold standard for ocular biometry. However, some limitations of ultrasound pachymetry have been described, mainly arising from inaccuracies in the calibration of sound transmittance of the ocular media and from diverse possible measurement errors associated with corneal indentation and probe placement, as well as with the need to use corneal anesthetic.1–3 Imaging techniques based on Scheimpflug photography allow for the point by point non-invasive exploration of CT, ACD and corneal and ACVol, in addition to the topographical assessment of anterior and posterior corneal surfaces,4 thus providing an excellent opportunity for precise characterization of the anterior ocular segment.
CT evaluation is important, particularly for the diagnosis and management of glaucoma, as it has been shown to modulate applanation tonometry measurements.5,6 Besides, there is a growing interest in laser refractive surgery in the pediatric population, both for amblyopia management in children with spectacle and contact lens intolerance7 and for the treatment of hyperopia, with or without hyperopic anisometropic amblyopia.8
Several studies have investigated the variations in central corneal thickness (CCT) among children from various ethnic groups and the influence of age and gender within the same group. Indeed, African American children were found to have thinner CCT values than Caucasians9,10 or Hispanics.11 Similarly, the average central corneas of Japanese children were encountered to be thinner than in Caucasians but thicker than in African American children,12 whereas Chinese children were found to have thicker corneas than Malayan or Indian Children.13 Other authors failed to discover any significant difference among racial subgroups.14 The effect of age on CCT is still uncertain. Thus, while some studies fail to demonstrate any effect of age on CCT,11,15,16 others describe an increase in CCT values until the age of 59 or 9,14 with either a decrease between the ages of 10 and 1414 or an approximation to adult values after the age of 5.12 Finally, most authors agree that CCT is not influenced by gender,11,16,17 although some studies have reported a small, albeit statistically significant interaction of gender and CCT, with boys having thicker corneas than girls.13,15
To the best of our knowledge, there are no published studies offering a complete biometric description of the anterior ocular segment in Sahrawi children. With this aim in mind, a prospective, observational study was designed to investigate CT, Km Ant and Km Post corneal curvature, CVol, ACD and ACVol in a Sahrawi pediatric population.
Materials and methodsPatientsThe present study was carried out on a group of Sahrawi children hosted for summer holidays in Alicante, Spain, and as part of the ongoing FUNCAVIS project (Fundación para la Calidad Visual). A total of 66 children (50% males, 50% females) between the ages of 8 and 13 years (mean age 10.63 years; SD=1.66 years) were enrolled in the study. Participants with a previous history of ocular surgery, ocular trauma and ocular pathology, as well as those under topical medication, were excluded from the investigation. None of the participants was born prematurely nor had any present or past history of contact lens wear. All participants showed good cooperation during the study.
Full explanation of the research was provided, including Pentacam measurement procedures, and written informed consent was obtained from a parent or legal guardian of each of the participants. The Declaration of Helsinki tenets of 1975 (as revised in Tokyo in 2004) was followed throughout the study and the study was given clearance by the Ethics Committee of the Hospital International Medimar Alicante.
The Pentacam systemThe Pentacam Oculus, Inc. GmbH, Wetzlar, Germany imaging device, which has been employed in ophthalmic practice since 2004, employs the Scheimpflug photographic technique to acquire multiple images of the anterior ocular segment. Its characteristics and operational principles have been extensively described in the literature.4 In essence, it utilizes a rotating monochromatic slit-light source (blue LED at 475nm) to capture 50 sectional images yielding 138,000 true elevation points, thus constructing a 3-dimensional view of the anterior segment of the eye, as well as allowing for the complete anterior and posterior topographic analysis of the cornea.
CT, Km Ant and posterior corneal curvature, CVol, ACD and ACVol were assessed. Corneal pachymetry was recorded at the thinnest point of the cornea. Mean corneal curvature (Km) is calculated by averaging the radii of the flat and steep meridians in a central 3.0mm zone. CVol is defined by the anterior and posterior corneal surface boundaries and a 10.0mm diameter around the corneal vertex. ACD is determined by the distance between the corneal endothelium, in line with the corneal vertex, and the anterior surface of the lens. Finally, ACVol is calculated similarly to CVol, with the posterior surface of the cornea and the anterior surface of the iris and lens acting as anatomical boundaries.
ProcedureAll participants underwent a complete ophthalmological and optometric examination, including visual acuity evaluation, slit-lamp exploration, non-cycloplegic autorefraction and ocular fundus inspection. No previously undiagnosed abnormalities were detected upon slit-lamp observation of the anterior segment.
Testing took place with natural pupils and under the same conditions in ambient illumination. Participants were instructed to keep both eyes open and to look at the fixation target for the duration of the scan, which was adjusted at 2seconds. Eyes were randomly examined. In order to avoid the documented daily changes in CT and other parameters, all measurements were conducted between 11:00AM and 14:00PM, after all participants had been awake for at least 4hours.18
Three consecutive Pentacam measurements were taken by an experimented investigator and the mean of the three readings was used for analysis. In order to avoid inter-examiner variability, all measurements were conducted by the same investigator (R.P.C.). The imaging device was calibrated prior to the start of each new set of measurements.
Data analysisStatistical analysis of the data was performed with the SPSS software (version 17.0, SPSS Inc., Chicago, IL, USA) for Windows. All data were analyzed for normality using the Kolmogorov–Smirnov test. No statistical difference could be found between right and left eyes. Therefore, data from right eyes was arbitrarily chosen for statistical purposes. A between-subjects analysis of variance (ANOVA) was used to investigate the interaction of gender on the various ocular parameters under examination. Pearson correlation test was employed to evaluate the relationship between ocular parameters. A p-value of 0.05 or less was considered to denote statistical significance throughout the study.
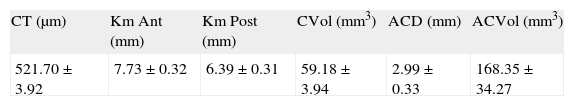
ResultsA total of 66 eyes from 66 children (33 males and 33 females) were included in the study. All data were found to follow a normal distribution. All eyes were found to have a refractive error ranging from emmetropia to +1.00 D, with the exception of two eyes presenting moderate myopia and three eyes with moderate hyperopic astigmatism. Mean and standard deviation (SD) values for CT, Km Ant and posterior corneal curvature, CVol, ACD and ACVol are displayed in Table 1. A between-subjects ANOVA revealed a statistically significant effect of gender on ACD (p=0.010) and ACVol (p=0.030). No other statistically significant contributions of gender were discovered, although for both Km Ant (7.80±0.36mm in males; 7.66±0.28mm in females) and Km Post (6.47±0.34mm in males; 6.32±0.28mm in females), differences approached statistical significance (p=0.076 and p=0.065 respectively). Males (526.70±31.18μm) were found to have slightly thicker corneas than females (516.30±31.72μm), albeit this difference failed to reach statistical significance (p=0.205).
Mean±SD values for corneal thickness (CT), mean anterior (Km Ant) and posterior (Km Post) corneal curvature, corneal volume (CVol), anterior chamber depth (ACD) and anterior chamber volume (ACVol).
| CT (μm) | Km Ant (mm) | Km Post (mm) | CVol (mm3) | ACD (mm) | ACVol (mm3) |
| 521.70±3.92 | 7.73±0.32 | 6.39±0.31 | 59.18±3.94 | 2.99±0.33 | 168.35±34.27 |
Analysis with the Pearson's correlation coefficient revealed significant and relatively strong correlations between Km Ant and Km Post (r=0.916; p<0.001), Km Ant and CVol (r=−0.406; p=0.001) and ACVol (r=0.369; p=0.002), Km Post and CVol (r=−0.552; p<0.001) and ACVol (r=0.318; p=0.009), ACD and ACVol (r=0.845; p<0.001) and between CT and CVol (r=0.835; p<0.001). Age was found to be weakly correlated with ACD (r=0.245; p=0.047) and ACVol (r=0.239; p=0.053). No correlation between age and CT was disclosed.
DiscussionAs far as a literature review has exposed, this study is one of the first to aim at a global non-invasive characterization of the anterior ocular segment in a group of children of Sahrawi ethnicity. Several previous researchers have explored various isolated ocular parameters, mainly central CT by means of ultrasound pachymetry. The present study evaluated CT, anterior and posterior corneal curvature, CVol, ACD and ACVol, and also examined the relationship between these parameters and the possible contribution of age and gender to the results.
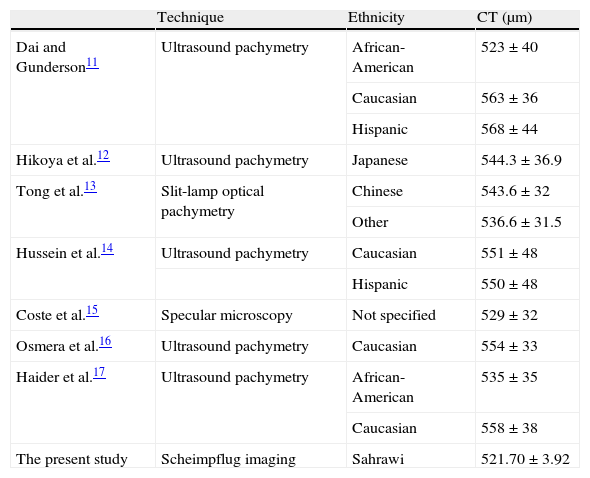
The mean CT of the group under study was of 521.70±31.92μm, with males having slight, but not statistically significant thicker corneas than females. These values are lower than previously reported11–17 and can only be considered comparable to those of a sample of African-American children of similar age11 (see Table 2). The negligible effect of age and the probably very weak contribution of gender are in agreement with earlier studies.
Mean±SD values for corneal thickness (CT) as compared with previous studies, with indication of the ethnic characteristics of the study sample and pachymetry technique.
| Technique | Ethnicity | CT (μm) | |
| Dai and Gunderson11 | Ultrasound pachymetry | African-American | 523±40 |
| Caucasian | 563±36 | ||
| Hispanic | 568±44 | ||
| Hikoya et al.12 | Ultrasound pachymetry | Japanese | 544.3±36.9 |
| Tong et al.13 | Slit-lamp optical pachymetry | Chinese | 543.6±32 |
| Other | 536.6±31.5 | ||
| Hussein et al.14 | Ultrasound pachymetry | Caucasian | 551±48 |
| Hispanic | 550±48 | ||
| Coste et al.15 | Specular microscopy | Not specified | 529±32 |
| Osmera et al.16 | Ultrasound pachymetry | Caucasian | 554±33 |
| Haider et al.17 | Ultrasound pachymetry | African-American | 535±35 |
| Caucasian | 558±38 | ||
| The present study | Scheimpflug imaging | Sahrawi | 521.70±3.92 |
Three different factors may account for the discrepancies in CT values. Firstly, ethnicity has been shown to be a determinant factor when measuring CT. The Sahrawi population originates from a mixed heritage, mainly Arab and Berber, thus presenting a different ethnic background to the groups previously studied. The relative geographical proximity to the African ethnicity may help to explain the mentioned similarities between the present group and the African-American group.
Secondly, it is prudent to admit the difficulties encountered in comparing outcomes from different instruments. Indeed, previous studies have compared the Pentacam system with other methods for measuring CT. Fujioka et al. examined the Pentacam, ultrasound pachymetry and non-contact specular microscopy, finding a good agreement between the three methods of measurement, although pairwise comparisons revealed statistically significant differences between them.19 Similarly, Barkana et al. compared the Pentacam, ultrasound and optical low-coherence reflectometry pachymeters, failing to discover any statistically significant difference between these devices and reporting excellent intraoperator repeatability and interoperator reproducibility for the Pentacam system.20 The same authors, however, advocated for further studies before these instruments could be used interchangeably.
Finally, the present method for the evaluation of CT was based on the identification of the thinnest point of the cornea. Previous research by Rüfer et al. disclosed that the thinnest point of the cornea is rarely located at its exact geometrical center, with an actual position mostly inferior and temporal from that point.21,22 The difference between the central thickness and the thickness at the thinnest point of the cornea was found by these authors to be statistically significant, and of the order of 10–12μm. The Pentacam system, like other imaging devices, determines both the location of the thinnest point of the cornea and its value. This information could be very relevant for the calculation of the residual CT when planning for refractive surgery procedures and for the precise measurement of intraocular pressure in glaucoma screening and management.
Previous authors have addressed possible differences in CT between children of different refractive status.15 Thus, myopic children were found to have thinner corneas than both emmetropic and hyperopic children, albeit statistically significant differences were only revealed between the emmetropic and hyperopic and between the hyperopic and myopic groups.15 The present limited sample of children had a refractive status ranging from emmetropia to +1.00D, with only two eyes with moderate myopia and three eyes with moderate hyperopic astigmatism. Therefore, the characteristics of this study sample precluded any statistical analysis of the possible associations between refractive status and ocular parameters.
Corneal radius values were similar to those reported by previous authors.23 It may be relevant to note that the measurement of mean K values offers a better repeatability than individual measures of flat and steep radii, an effect that has been suggested to result from the noise-reducing benefit of averaging two values.24
CT was not found to correlate with Km Ant. This finding is in disagreement with published research by Tong et al., where a weak (r=0.19) but statistically significant correlation was encountered between these paramenters,13 although other researchers failed to replicate this correlation.23 A positive, strong correlation was discovered between CT and CVol. The relationship between CT and CVol, as well as the other strong and statistically significant reported correlations between pairs of ocular parameters, are easily explainable from a simple geometrical standpoint. Thus, for example, it is to be expected that, in healthy subjects, a flatter Km Ant would be generally associated with a flatter Km Post or that an increase in ACD would result in a subsequent increase in ACVol values. In fact, a purist mathematical approach may consider a certain degree of dependence between some of these variables, thus precluding the statistical analysis of correlation.
Gender was found to be a contributing factor to both ACD and ACVol and a weak correlation was discovered between age and ACD. However, sample size should be considered an important limitation of the study when interpreting these findings. Further research on a larger sample, within the same ethnic group, including an equal number of males and females and presenting a greater range of ages would permit a more robust statistical approach and lead to more conclusive evidence.
In summary, the characteristics of the Pentacam system imaging methodology allow for a fast (less than 2seconds), non-invasive procedure, which ensures patient collaboration. This is particularly important when patients are of a young age or displaying a restive or anxious behavior. The precise biometric characterization of the anterior segment of the eye is of crucial importance to establishing baseline criteria whereupon anomalies can be judged, diagnosed and managed.
Conflict of interestsThe authors have no conflicts of interest to declare.