To investigate the relationship between age, gender, corneal diameter, central corneal curvature, central corneal thickness (CCT) and intraocular pressure in Nigerians with normal intraocular pressure.
MethodsOne hundred and thirty eyes from 130 subjects (mean age=47.8±16.8 years) including 77 males and 53 females were recruited. CCT was measured by ultrasound pachymetry, intraocular pressure was determined by non-contact tonometry, horizontal and vertical corneal diameters were measured with a ruler and central corneal curvature was measured by keratometry.
ResultsThe mean values obtained were as follows: CCT=548.97±34.28μm, IOP=15.61±2.69mmHg, average corneal curvature (AVK)=42.98±1.19 D, horizontal corneal diameter (HVID)=11.39±0.69mm and vertical corneal diameter (VVID)=10.51±0.50mm. There was a significant effect of age on CCT (r=−0.35, p<0.001). A 10-year-increase in age was associated with a 7.0μm decrease in CCT. Males had significantly wider HVID than females (p=0.03). Subjects in older age groups have narrower HVID and VVID. Corneal curvature, corneal diameter and gender did not significantly affect CCT.
ConclusionCCT of normotensive Nigerian adults decreases with increasing age. There was no correlation between CCT and IOP in normotensive subjects. CCT was not significantly influenced by gender, corneal curvature and corneal diameter.
investigar la relación entre la edad, el sexo, el diámetro corneal, la curvatura corneal central, el espesor corneal central (ECC) y la presión intraocular en nigerianos con presión intraocular normal.
Métodosse incluyeron 130 ojos derechos de 130 sujetos (media de edad=47,8±16,8 años), de los cuales 77 eran hombres y 53 mujeres. Se midió el ECC por paquimetría ultrasónica, la presión intraocular se determinó mediante tonometría sin contacto, el diámetro corneal vertical y horizontal se midió con una regla milimétrica y la curvatura corneal central se determinó por queratometría.
Resultadoslos valores medios obtenidos fueron los siguientes: ECC=548,97±34,28μm; PIO=15,61±2,69mmHg; curvatura corneal media (AVK)=42,98±1,19 D, diámetro corneal horizontal (HVID)=11,39±0,69mm y diámetro corneal vertical (VVID)=10,51±0,50mm. Hubo un efecto significativo de la edad sobre el ECC (r=-0,35, p<0,001). Un aumento de la edad en 10 años se asoció con una disminución del ECC de 7,0 μm. Los hombres presentaron un HVID más amplio que el de las mujeres (p=0,03). Los sujetos de mayor edad tenían HVID y VVID menores. La curvatura corneal, el diámetro corneal y el sexo no tuvieron un efecto significativo sobre el ECC.
Conclusiónel ECC de los adultos nigerianos normotensos disminuye con la edad. No se observó ninguna correlación entre el ECC y la PIO en los sujetos normotensos. El sexo, la curvatura corneal y el diámetro corneal no tuvieron un efecto significativo sobre el ECC.
Intra ocular pressure (IOP) is measured as part of the routine to diagnose, classify and monitor the progression of glaucoma.1 Goldmann applanation tonometry (GAT) is considered as the gold standard technique for the measurement of IOP. However, the validity of this procedure can be affected by the central corneal thickness (CCT). In general, a thin cornea leads to underestimation while a thick cornea results in overestimation of the actual IOP.2,3 However, this observation does not necessarily prove a causal relationship between thick CCT and glaucoma.
Clinic and population-based studies have demonstrated that African-Americans and other populations of African descent have thinner CCT than other races.3–9 The under diagnosis and treatment of African-Americans with glaucoma may be partly linked to their thinner corneas. Corneal thickness is an independent risk factor for the development as well as progression of glaucoma.5,10,11 Doughty and Zaman12 advised that a correction factor of 2.5mmHg should be made for every 50μm change in CCT.
Several factors affect CCT including race and ethnicity,3–6,9 gender,3,5,6,13–16 age,3,5,6,9,13–17 refractive error,3,5,9,17–19 corneal curvature,6,20,21 and genetic factors.18,22,23
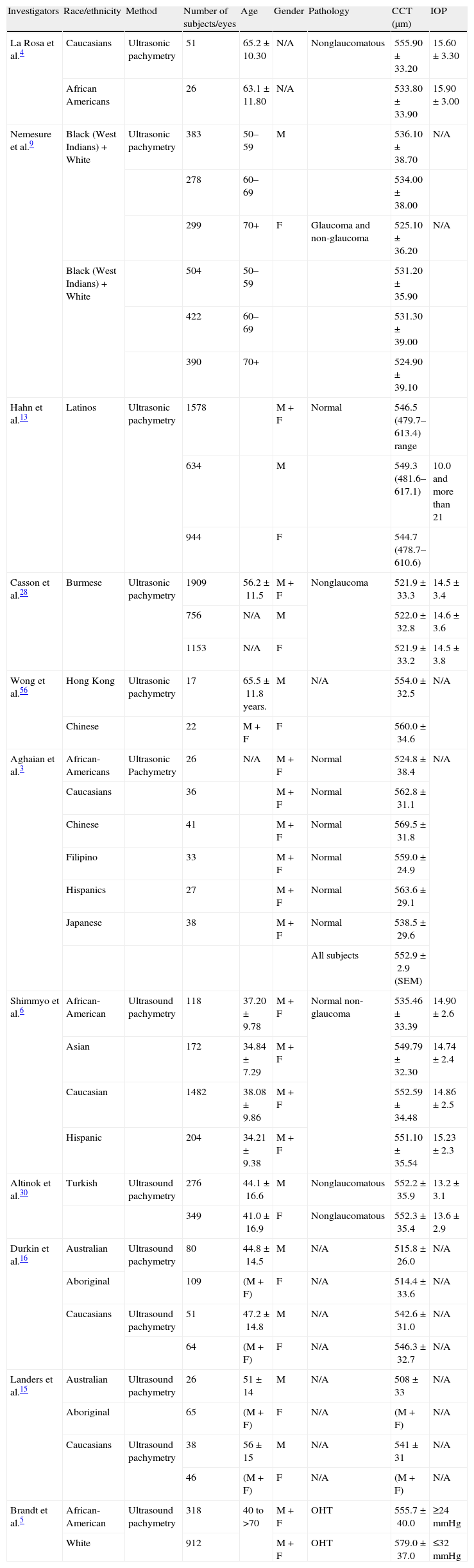
The differences in CCT between racial groups (Table 1) reflect strong genetic inheritance. La Rosa et al.,4 observed that self reported racial background in the United States is mainly inhomogeneous. Consequently, this may mask any racial differences in CCT. One implication of this observation is that average value of CCT of African-Americans may not be valid for populations of African descent outside of the United States.
Central corneal thickness (CCT) in subjects of different races and ethnicities.
| Investigators | Race/ethnicity | Method | Number of subjects/eyes | Age | Gender | Pathology | CCT (μm) | IOP |
| La Rosa et al.4 | Caucasians | Ultrasonic pachymetry | 51 | 65.2±10.30 | N/A | Nonglaucomatous | 555.90±33.20 | 15.60±3.30 |
| African Americans | 26 | 63.1±11.80 | N/A | 533.80±33.90 | 15.90±3.00 | |||
| Nemesure et al.9 | Black (West Indians)+White | Ultrasonic pachymetry | 383 | 50–59 | M | 536.10±38.70 | N/A | |
| 278 | 60–69 | 534.00±38.00 | ||||||
| 299 | 70+ | F | Glaucoma and non-glaucoma | 525.10±36.20 | N/A | |||
| Black (West Indians)+White | 504 | 50–59 | 531.20±35.90 | |||||
| 422 | 60–69 | 531.30±39.00 | ||||||
| 390 | 70+ | 524.90±39.10 | ||||||
| Hahn et al.13 | Latinos | Ultrasonic pachymetry | 1578 | M+F | Normal | 546.5 (479.7–613.4) range | ||
| 634 | M | 549.3 (481.6–617.1) | 10.0 and more than 21 | |||||
| 944 | F | 544.7 (478.7–610.6) | ||||||
| Casson et al.28 | Burmese | Ultrasonic pachymetry | 1909 | 56.2±11.5 | M+F | Nonglaucoma | 521.9±33.3 | 14.5±3.4 |
| 756 | N/A | M | 522.0±32.8 | 14.6±3.6 | ||||
| 1153 | N/A | F | 521.9±33.2 | 14.5±3.8 | ||||
| Wong et al.56 | Hong Kong | Ultrasonic pachymetry | 17 | 65.5±11.8 years. | M | N/A | 554.0±32.5 | N/A |
| Chinese | 22 | M+F | F | 560.0±34.6 | ||||
| Aghaian et al.3 | African-Americans | Ultrasonic Pachymetry | 26 | N/A | M+F | Normal | 524.8±38.4 | N/A |
| Caucasians | 36 | M+F | Normal | 562.8±31.1 | ||||
| Chinese | 41 | M+F | Normal | 569.5±31.8 | ||||
| Filipino | 33 | M+F | Normal | 559.0±24.9 | ||||
| Hispanics | 27 | M+F | Normal | 563.6±29.1 | ||||
| Japanese | 38 | M+F | Normal | 538.5±29.6 | ||||
| All subjects | 552.9±2.9 (SEM) | |||||||
| Shimmyo et al.6 | African-American | Ultrasound pachymetry | 118 | 37.20±9.78 | M+F | Normal non-glaucoma | 535.46±33.39 | 14.90±2.6 |
| Asian | 172 | 34.84±7.29 | M+F | 549.79±32.30 | 14.74±2.4 | |||
| Caucasian | 1482 | 38.08±9.86 | M+F | 552.59±34.48 | 14.86±2.5 | |||
| Hispanic | 204 | 34.21±9.38 | M+F | 551.10±35.54 | 15.23±2.3 | |||
| Altinok et al.30 | Turkish | Ultrasound pachymetry | 276 | 44.1±16.6 | M | Nonglaucomatous | 552.2±35.9 | 13.2±3.1 |
| 349 | 41.0±16.9 | F | Nonglaucomatous | 552.3±35.4 | 13.6±2.9 | |||
| Durkin et al.16 | Australian | Ultrasound pachymetry | 80 | 44.8±14.5 | M | N/A | 515.8±26.0 | N/A |
| Aboriginal | 109 | (M+F) | F | N/A | 514.4±33.6 | N/A | ||
| Caucasians | Ultrasound pachymetry | 51 | 47.2±14.8 | M | N/A | 542.6±31.0 | N/A | |
| 64 | (M+F) | F | N/A | 546.3±32.7 | N/A | |||
| Landers et al.15 | Australian | Ultrasound pachymetry | 26 | 51±14 | M | N/A | 508±33 | N/A |
| Aboriginal | 65 | (M+F) | F | N/A | (M+F) | N/A | ||
| Caucasians | Ultrasound pachymetry | 38 | 56±15 | M | N/A | 541±31 | N/A | |
| 46 | (M+F) | F | N/A | (M+F) | N/A | |||
| Brandt et al.5 | African-American | Ultrasound pachymetry | 318 | 40 to >70 | M+F | OHT | 555.7±40.0 | ≥24mmHg |
| White | 912 | M+F | OHT | 579.0±37.0 | ≤32mmHg |
N/A=not available, μm=micron meter, IOP=intra ocular pressure, mmHg=millimetre of mercury, M=males, F=females, M+F=males and females, OHT=ocular hypertension.
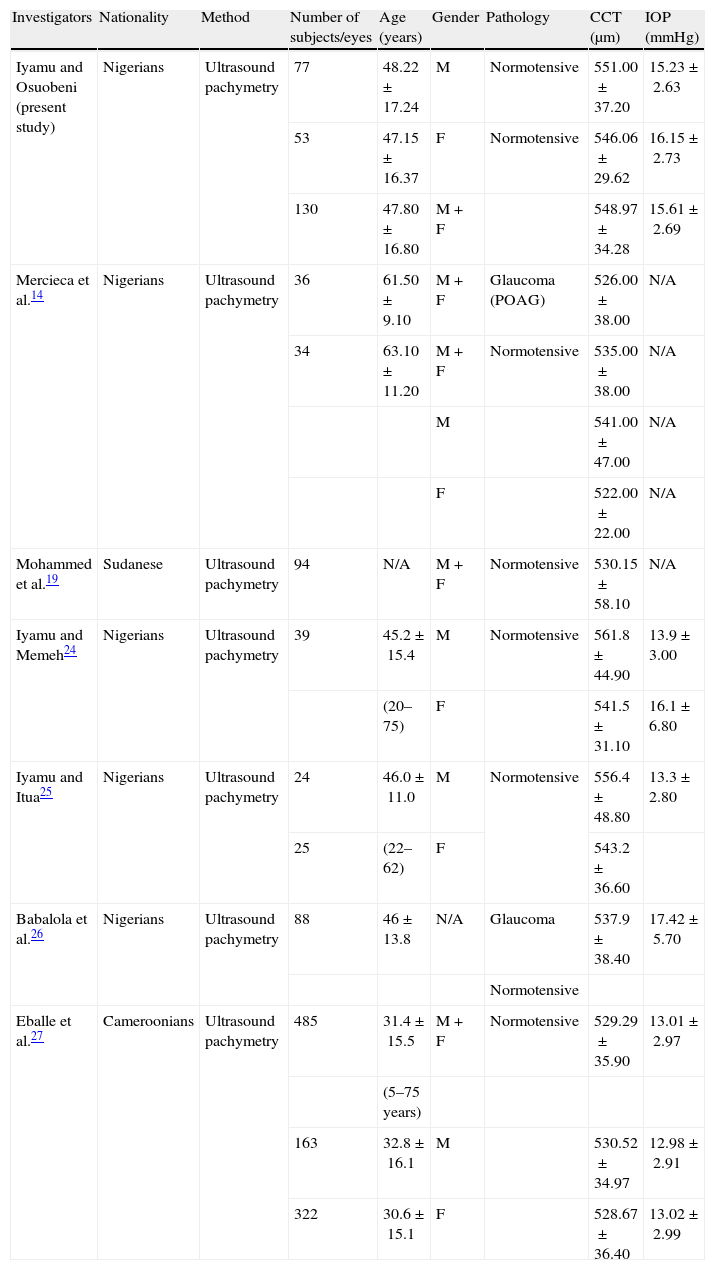
Several investigators (Table 2) have studied the CCT of indigenous African subjects.14,19,24–27 Mercieca et al.,14 reported that age was negatively correlated with CCT (p=0.0002) in Nigerian adults. However, the regression equation of CCT on age was not presented. This would have been helpful to predict the CCT of Nigerian adults. Similarly, gender had a significant effect on CCT (p=0.035) with men having thicker corneas (541±47μm) than women (522±22μm).
Central corneal thickness (CCT) in African subjects.
| Investigators | Nationality | Method | Number of subjects/eyes | Age (years) | Gender | Pathology | CCT (μm) | IOP (mmHg) |
| Iyamu and Osuobeni (present study) | Nigerians | Ultrasound pachymetry | 77 | 48.22±17.24 | M | Normotensive | 551.00±37.20 | 15.23±2.63 |
| 53 | 47.15±16.37 | F | Normotensive | 546.06±29.62 | 16.15±2.73 | |||
| 130 | 47.80±16.80 | M+F | 548.97±34.28 | 15.61±2.69 | ||||
| Mercieca et al.14 | Nigerians | Ultrasound pachymetry | 36 | 61.50±9.10 | M+F | Glaucoma (POAG) | 526.00±38.00 | N/A |
| 34 | 63.10±11.20 | M+F | Normotensive | 535.00±38.00 | N/A | |||
| M | 541.00±47.00 | N/A | ||||||
| F | 522.00±22.00 | N/A | ||||||
| Mohammed et al.19 | Sudanese | Ultrasound pachymetry | 94 | N/A | M+F | Normotensive | 530.15±58.10 | N/A |
| Iyamu and Memeh24 | Nigerians | Ultrasound pachymetry | 39 | 45.2±15.4 | M | Normotensive | 561.8±44.90 | 13.9±3.00 |
| (20–75) | F | 541.5±31.10 | 16.1±6.80 | |||||
| Iyamu and Itua25 | Nigerians | Ultrasound pachymetry | 24 | 46.0±11.0 | M | Normotensive | 556.4±48.80 | 13.3±2.80 |
| 25 | (22–62) | F | 543.2±36.60 | |||||
| Babalola et al.26 | Nigerians | Ultrasound pachymetry | 88 | 46±13.8 | N/A | Glaucoma | 537.9±38.40 | 17.42±5.70 |
| Normotensive | ||||||||
| Eballe et al.27 | Cameroonians | Ultrasound pachymetry | 485 | 31.4±15.5 | M+F | Normotensive | 529.29±35.90 | 13.01±2.97 |
| (5–75 years) | ||||||||
| 163 | 32.8±16.1 | M | 530.52±34.97 | 12.98±2.91 | ||||
| 322 | 30.6±15.1 | F | 528.67±36.40 | 13.02±2.99 |
N/A=not available, CCT=central corneal thickness, μm=micron, IOP=intraocular pressure, mmHg=millimetre of mercury, M=males, F=females, M+F=males and females.
Iyamu and Memeh24 established that refractive error and gender did not correlate with CCT in Nigerian adults with normal IOP. However, there was an indication that CCT decreases with age. The linear regression equation predicts approximately a 7.0μm decrease in CCT per decade increase in age.
Iyamu and Ituah25 evaluated CCT and intraocular pressure in Nigerian adults. They demonstrated that glaucoma subjects had significantly thinner corneas (508.4±33.8μm) than normotensive subjects (551.6±44.5μm). Ocular hypertensive subjects had the thickest corneas (604.5±14.4μm). They concluded that gender and age were not significantly associated with CCT.
Babalola et al.,26 noted that Nigerians have lower CCT (537.9μm) than Caucasians (550.4μm) but a higher value than African-Americans (521μm).3
The relationship between central corneal curvature, corneal diameter and CCT is ambiguous.6,20,21,28–32 Longer eyes are associated with flatter radius of curvature of the central cornea33,34 and wider corneal diameter.35 Chang et al.,36 reported that longer eyes are associated with thinner CCT. They argued that larger corneal area associated with longer axial length will result in a thinner stroma and subsequently thinner CCT. Henriques et al.,37 demonstrated a significant correlation between CCT and corneal diameter in children with congenital glaucoma. Price et al.,38 reported that CCT was not correlated with corneal diameter in myopic patients undergoing Laser In Situ Keratomileusis.
Any factor that affects the CCT could potentially influence the true value of the measured IOP. Consequently such factors would have to be factored into a regression equation in order to predict a more accurate IOP value. This is crucial for the clinical diagnosis, management and monitoring of glaucoma therapy. The CCT is also clinically important in patients contemplating photorefractive surgery. The reasons for carrying out this study were to investigate the effect of age, gender, corneal radius of curvature and the horizontal and vertical corneal diameter on CCT and ultimately on the IOP in normotensive Nigerian adults. We were also interested in reconciling some of the ambiguities in previous investigations of CCT in Nigerian adults.
MethodsThe experimental design was an observational, prospective cross-sectional study carried out in the Optometry clinic, Department of Optometry, University of Benin, Benin-City, Nigeria. The Departmental Research Ethics Committee (DREC) approved the research proposal. Informed consent was obtained from each subject after thorough explanation of the procedure and possible outcome. The experiment was conducted in accordance with the tenets of the Declaration of Helsinki. The subjects recruited for this study were healthy adult Nigerians. Inclusion criteria were as follows, at least 20 years of age and no history of the following: contact lens wear, systemic diseases associated with corneal pathology (rheumatoid arthritis), ocular hypertension, glaucoma (open- or closed-angle, normal tension) and corneal pathology (e.g., infection, encroached pterygium, dystrophy, ectasias). All measurements were taken only in the right eye by one of the authors who is a University lecturer and a registered Optometrist with special interest in Contact lenses.
Subjects were divided into five age groups: 20–39, 40–49, 50–59, 60–69 and 70 years and above. These groups were further qualitatively described as younger age group (20–49 years), middle age group (50–59 years) and older age group (60 years and above).
All prospective subjects completed a questionnaire to scrutinize their eligibility for the study. Next, a slit lamp examination of the anterior eye was conducted. The corneal curvature was determined with a Bausch & Lomb one position Keratometer (Bausch & Lomb Corp., USA). The instrument was calibrated by using a stainless steel ball bearing of 44.75D curvature. Measurements were made along the two major meridians. The average of both values represented the mean corneal curvature. Next, the vertical and horizontal corneal diameter was determined by measuring the visible iris diameter with a millimetre ruler. The distance between the nasal and temporal imaginary tangents to the corneal circumference, along the centre of the pupil, was recorded in millimetres as the horizontal corneal diameter (horizontal visible iris diameter, HVID). The vertical corneal diameter (vertical visible iris diameter, VVID) was the distance between the superior and inferior imaginary tangents to the corneal circumference. In measuring the VVID it was occasionally necessary to lift the eyelids with minimum pressure being applied to the globe. The intraocular pressure (IOP) was measured with a portable hand-held tonometer (Keeler Pulsair EasyEye, Keeler Instrument Inc., USA). Five measurements were obtained. The average value was recorded as the IOP. Finally, the central corneal thickness was measured with an ultrasound pachymeter (SW-1000P ultrasound pachymeter Tianji Suowei Electronic Technology, Co. Ltd., China). Probe frequency was 20MHz, and sound speed=1640m−1). The subject was comfortably seated with the head upright and eyes in the primary position of gaze. The probe was sterilized with 70% alcohol and allowed to air-dry. A drop of topical anaesthetic (Tetracaine HCl 0.1%) was instilled in the subject's eye. The probe was carefully aligned perpendicularly to and lightly touching the cornea. At least ten readings were continuously taken and the average calculated as the measured central corneal thickness (CCT). All measurements were taken by the same observer between 10.00 am and 12.00 pm to avoid diurnal variation.
Statistical analysesStatgraphics Plus39 version 5.1 (Statpoint Technologies, Inc., Warrenton, VA, USA.) and SPSS40 version 10.0 (SPSS Inc, Chicago, IL, USA) were employed for statistical analyses. Test for normality of distribution was performed with computed Chi-squared goodness-of-fit statistic. Relationship or association between variables was determined with correlation and regression analyses. Analysis of variance (ANOVA) and Student's t-test were employed to test for significance difference between groups. Statistical significance was reached when p-value was ≤0.05.
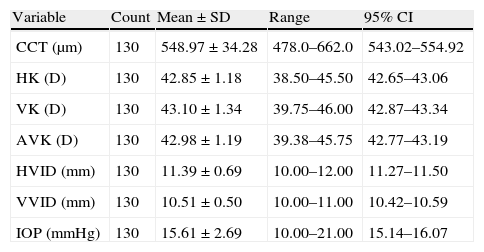
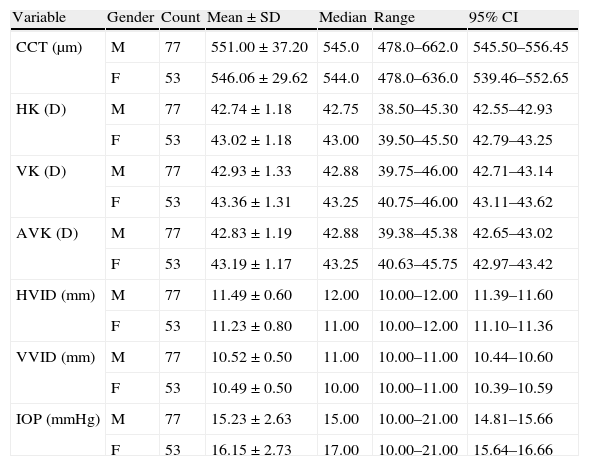
ResultsA total of one hundred and thirty subjects (n=130) comprising 77 males and 53 females took part in the study. The average age all subjects were 47.8±16.8 years (range 20–79 years). Table 3 shows the descriptive statistics of the measured variables.
Statistics of measured variables from all subjects.
| Variable | Count | Mean±SD | Range | 95% CI |
| CCT (μm) | 130 | 548.97±34.28 | 478.0–662.0 | 543.02–554.92 |
| HK (D) | 130 | 42.85±1.18 | 38.50–45.50 | 42.65–43.06 |
| VK (D) | 130 | 43.10±1.34 | 39.75–46.00 | 42.87–43.34 |
| AVK (D) | 130 | 42.98±1.19 | 39.38–45.75 | 42.77–43.19 |
| HVID (mm) | 130 | 11.39±0.69 | 10.00–12.00 | 11.27–11.50 |
| VVID (mm) | 130 | 10.51±0.50 | 10.00–11.00 | 10.42–10.59 |
| IOP (mmHg) | 130 | 15.61±2.69 | 10.00–21.00 | 15.14–16.07 |
CCT=central corneal thickness; HK=horizontal corneal curvature; VK=vertical corneal curvature; AVK=Average corneal curvature; HVID=horizontal visible iris diameter (horizontal corneal diameter); VVID=vertical visible iris diameter (vertical corneal diameter); IOP=intraocular pressure; SD=standard deviation; CI=confidence interval.
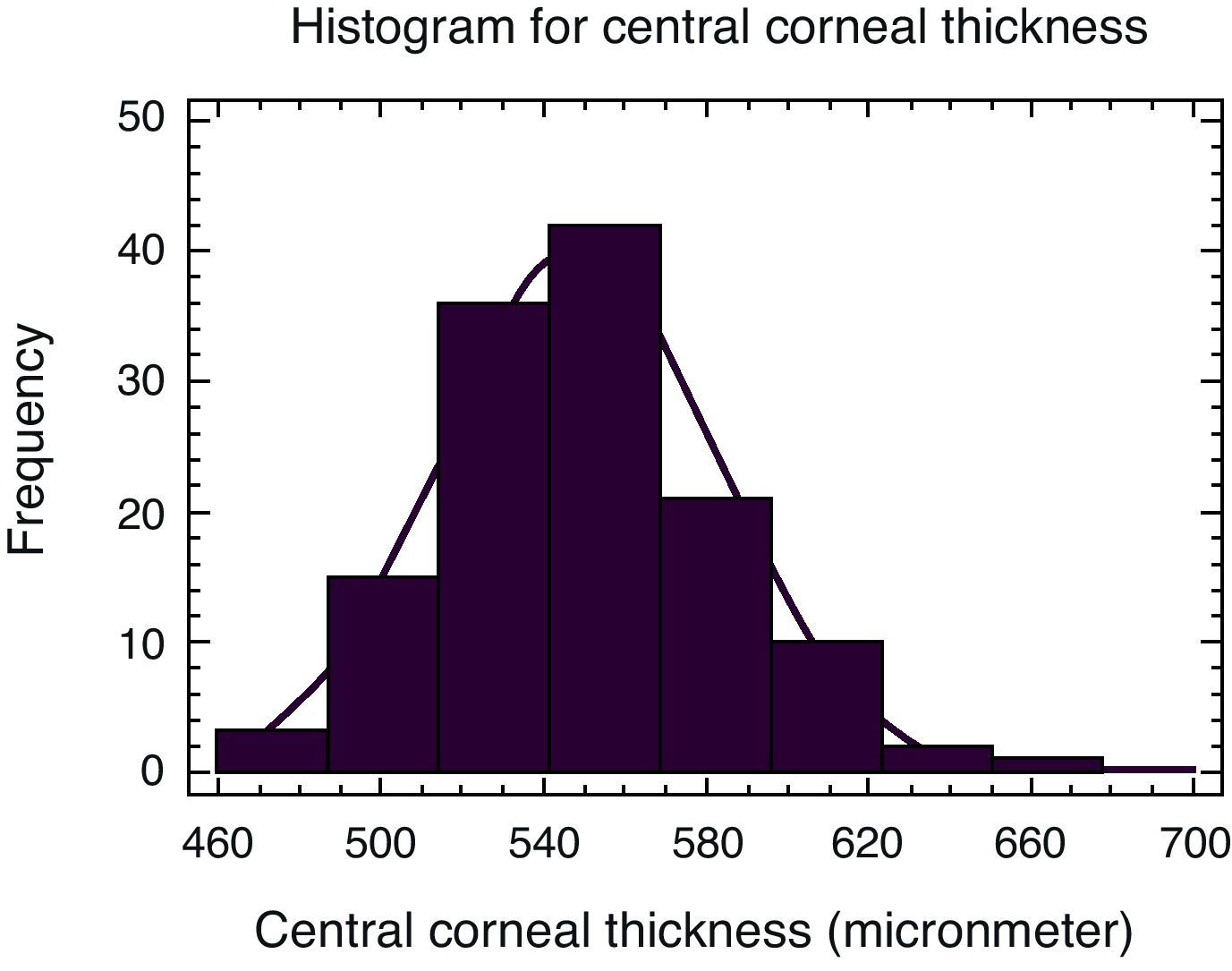
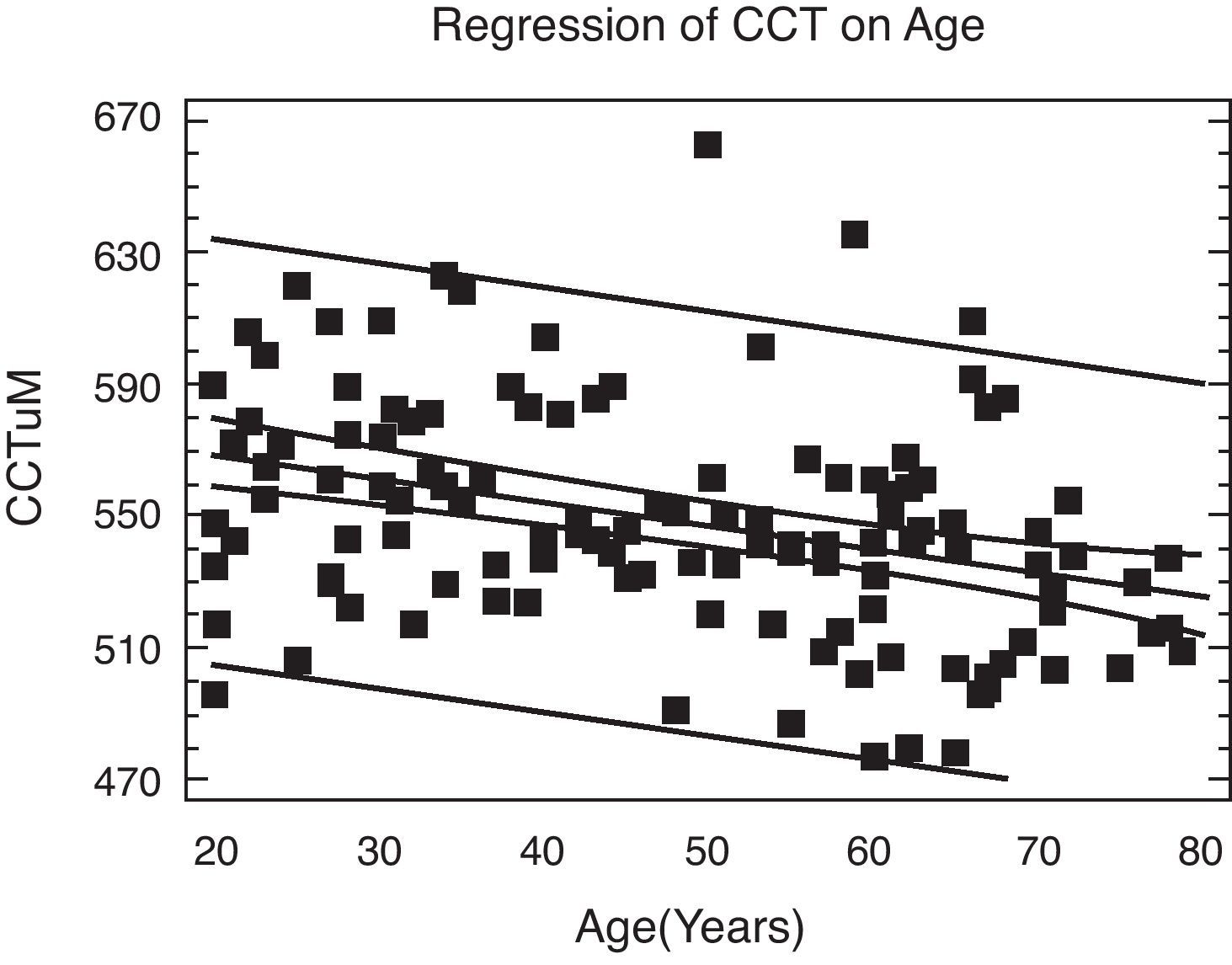
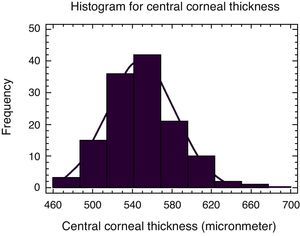
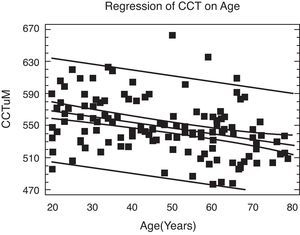
Fig. 1 shows the distribution of CCT. The Chi-square goodness-of-fit-statistic (p=0.15) shows that CCT was normally distributed. The mean CCT for the entire sample was 548.97±34.28μm. Fig. 2 is a graphical representation of the regression of CCT on age. A linear model best described this relationship, CCT (μm)=583.16–0.72* AGE (r=−0.35, p<0.001). According to this model, a 10-year increase in age leads to approximately a 7μm decrease in CCT.
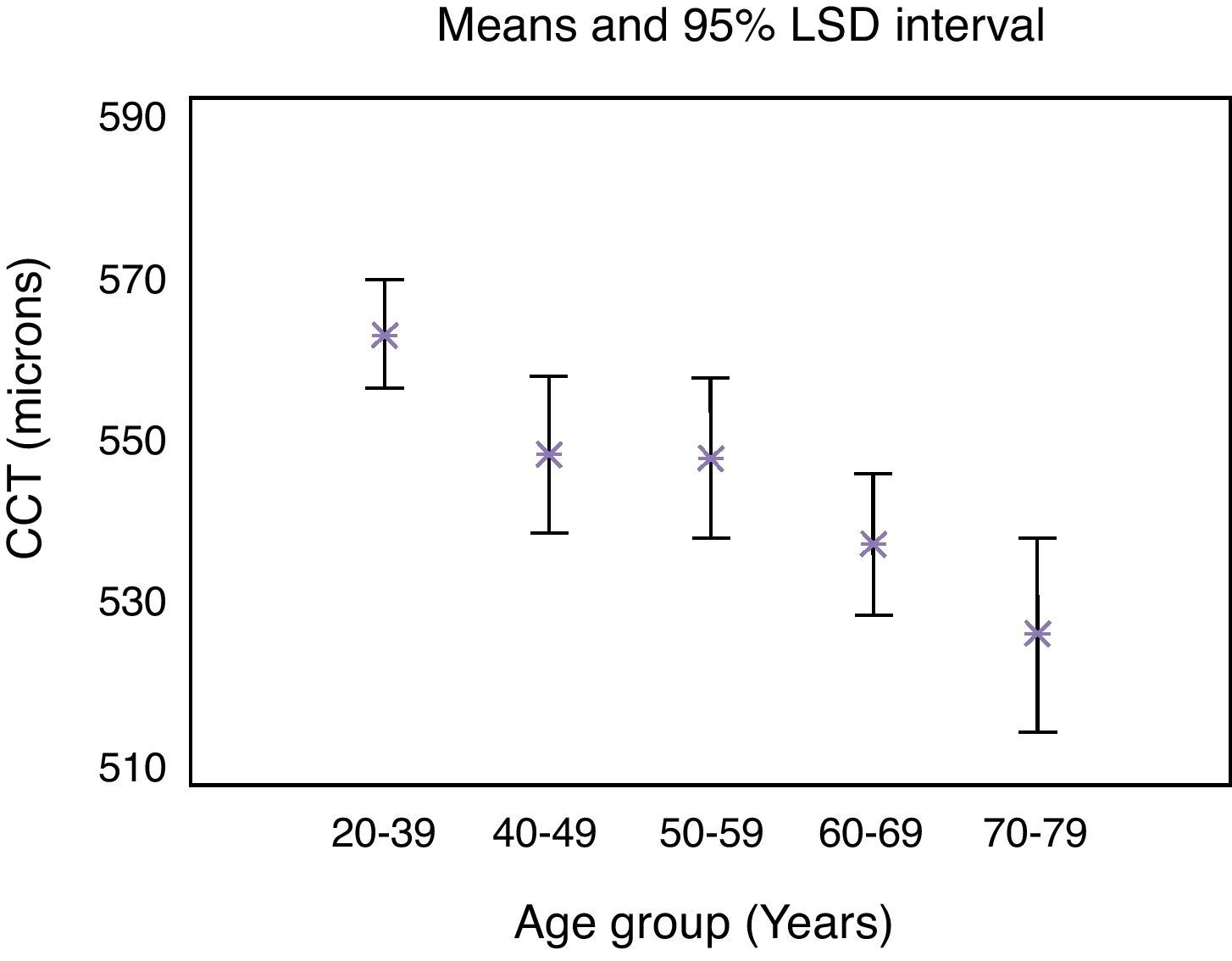
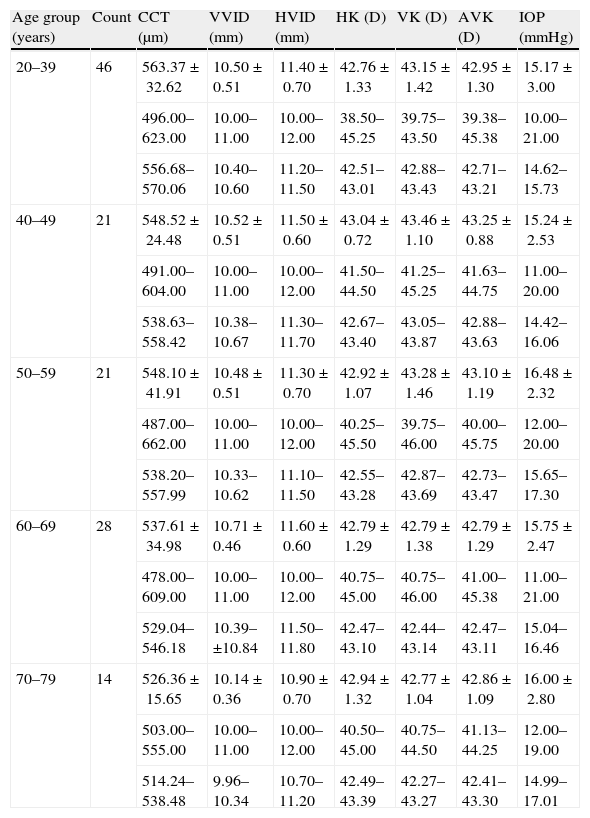
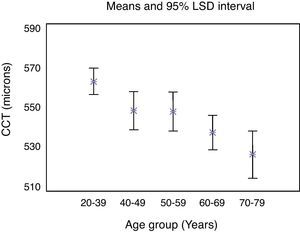
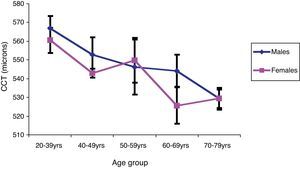
The difference in mean CCT across age groups (Table 4) was statistically significant (p<0.001). The mean CCT of the 20–39 years old was significantly thicker than that of the 60–69 years and 70–79 years age groups. Fig. 3 plots the mean value and the 95% CI for the mean at the various age groups. The general trend is the reduction of CCT in the older age groups.
The effect of age group on measured variables in the present study.
| Age group (years) | Count | CCT (μm) | VVID (mm) | HVID (mm) | HK (D) | VK (D) | AVK (D) | IOP (mmHg) |
| 20–39 | 46 | 563.37±32.62 | 10.50±0.51 | 11.40±0.70 | 42.76±1.33 | 43.15±1.42 | 42.95±1.30 | 15.17±3.00 |
| 496.00–623.00 | 10.00–11.00 | 10.00–12.00 | 38.50–45.25 | 39.75–43.50 | 39.38–45.38 | 10.00–21.00 | ||
| 556.68–570.06 | 10.40–10.60 | 11.20–11.50 | 42.51–43.01 | 42.88–43.43 | 42.71–43.21 | 14.62–15.73 | ||
| 40–49 | 21 | 548.52±24.48 | 10.52±0.51 | 11.50±0.60 | 43.04±0.72 | 43.46±1.10 | 43.25±0.88 | 15.24±2.53 |
| 491.00–604.00 | 10.00–11.00 | 10.00–12.00 | 41.50–44.50 | 41.25–45.25 | 41.63–44.75 | 11.00–20.00 | ||
| 538.63–558.42 | 10.38–10.67 | 11.30–11.70 | 42.67–43.40 | 43.05–43.87 | 42.88–43.63 | 14.42–16.06 | ||
| 50–59 | 21 | 548.10±41.91 | 10.48±0.51 | 11.30±0.70 | 42.92±1.07 | 43.28±1.46 | 43.10±1.19 | 16.48±2.32 |
| 487.00–662.00 | 10.00–11.00 | 10.00–12.00 | 40.25–45.50 | 39.75–46.00 | 40.00–45.75 | 12.00–20.00 | ||
| 538.20–557.99 | 10.33–10.62 | 11.10–11.50 | 42.55–43.28 | 42.87–43.69 | 42.73–43.47 | 15.65–17.30 | ||
| 60–69 | 28 | 537.61±34.98 | 10.71±0.46 | 11.60±0.60 | 42.79±1.29 | 42.79±1.38 | 42.79±1.29 | 15.75±2.47 |
| 478.00–609.00 | 10.00–11.00 | 10.00–12.00 | 40.75–45.00 | 40.75–46.00 | 41.00–45.38 | 11.00–21.00 | ||
| 529.04–546.18 | 10.39–±10.84 | 11.50–11.80 | 42.47–43.10 | 42.44–43.14 | 42.47–43.11 | 15.04–16.46 | ||
| 70–79 | 14 | 526.36±15.65 | 10.14±0.36 | 10.90±0.70 | 42.94±1.32 | 42.77±1.04 | 42.86±1.09 | 16.00±2.80 |
| 503.00–555.00 | 10.00–11.00 | 10.00–12.00 | 40.50–45.00 | 40.75–44.50 | 41.13–44.25 | 12.00–19.00 | ||
| 514.24–538.48 | 9.96–10.34 | 10.70–11.20 | 42.49–43.39 | 42.27–43.27 | 42.41–43.30 | 14.99–17.01 |
Mean and standard deviation (top row), range (middle row) and 95% confidence interval (bottom row). CCT=central corneal thickness, VVID=vertical visible iris diameter (vertical corneal diameter), HVID=horizontal visible iris diameter (horizontal corneal diameter), HK=horizontal corneal curvature, VK=vertical corneal curvature, AVK=average corneal curvature (HK+VK)/2)), IOP=intraocular pressure, μm=micron meter, mm=millimetre, mm Hg=millimetre of mercury, D=dioptre.
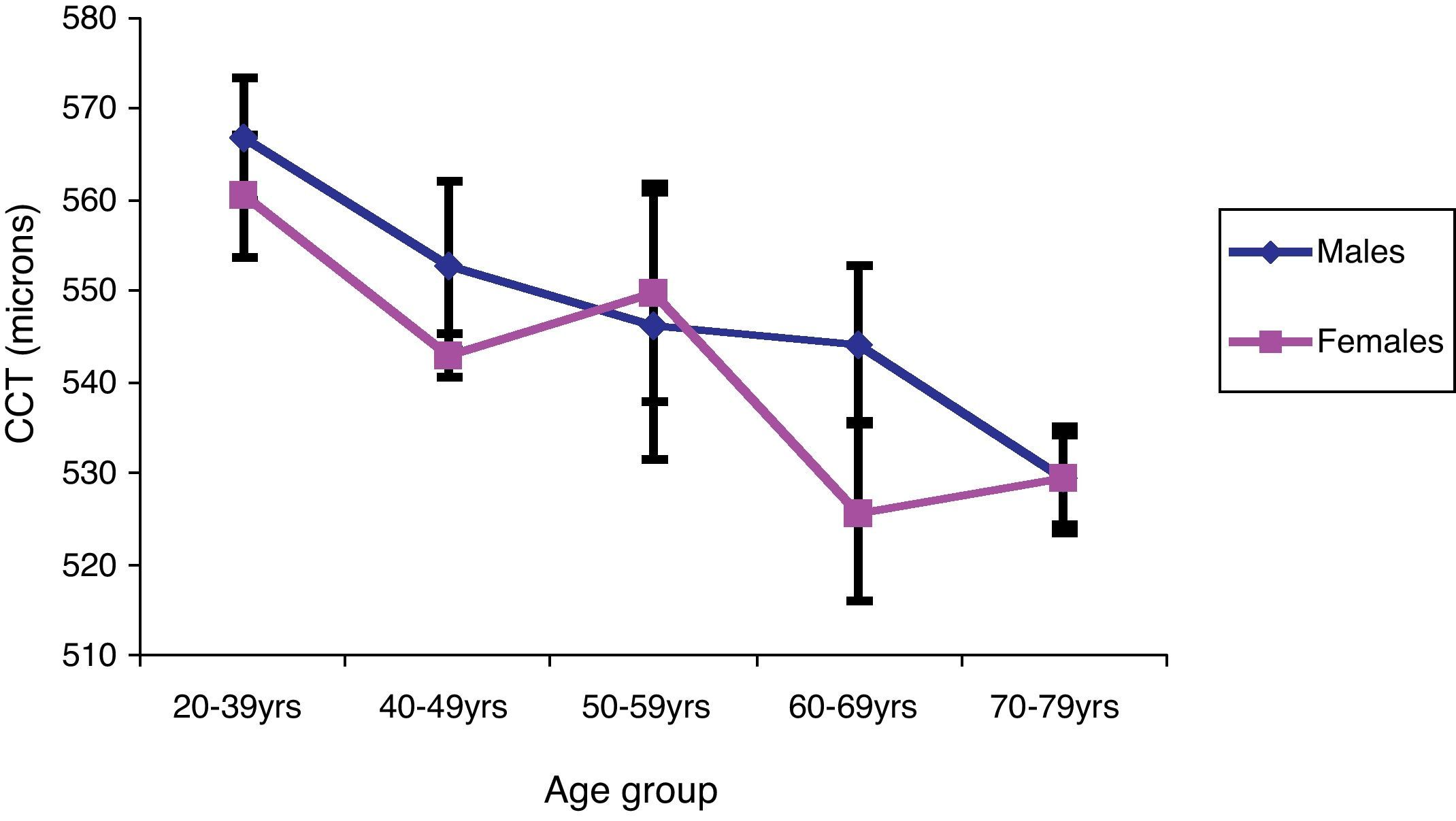
Fig. 4 displays the mean CCT±1 SD of male and female subjects at each age group. The decrease in CCT with increasing age is evident for both genders.
Table 5 shows the values of the measured variables according to gender.
The effect of gender on measured variables.
| Variable | Gender | Count | Mean±SD | Median | Range | 95% CI |
| CCT (μm) | M | 77 | 551.00±37.20 | 545.0 | 478.0–662.0 | 545.50–556.45 |
| F | 53 | 546.06±29.62 | 544.0 | 478.0–636.0 | 539.46–552.65 | |
| HK (D) | M | 77 | 42.74±1.18 | 42.75 | 38.50–45.30 | 42.55–42.93 |
| F | 53 | 43.02±1.18 | 43.00 | 39.50–45.50 | 42.79–43.25 | |
| VK (D) | M | 77 | 42.93±1.33 | 42.88 | 39.75–46.00 | 42.71–43.14 |
| F | 53 | 43.36±1.31 | 43.25 | 40.75–46.00 | 43.11–43.62 | |
| AVK (D) | M | 77 | 42.83±1.19 | 42.88 | 39.38–45.38 | 42.65–43.02 |
| F | 53 | 43.19±1.17 | 43.25 | 40.63–45.75 | 42.97–43.42 | |
| HVID (mm) | M | 77 | 11.49±0.60 | 12.00 | 10.00–12.00 | 11.39–11.60 |
| F | 53 | 11.23±0.80 | 11.00 | 10.00–12.00 | 11.10–11.36 | |
| VVID (mm) | M | 77 | 10.52±0.50 | 11.00 | 10.00–11.00 | 10.44–10.60 |
| F | 53 | 10.49±0.50 | 10.00 | 10.00–11.00 | 10.39–10.59 | |
| IOP (mmHg) | M | 77 | 15.23±2.63 | 15.00 | 10.00–21.00 | 14.81–15.66 |
| F | 53 | 16.15±2.73 | 17.00 | 10.00–21.00 | 15.64–16.66 |
CCT=central corneal thickness; HK=horizontal corneal curvature; VK=vertical corneal curvature; AVK=average corneal curvature; HVID=horizontal visible iris diameter (horizontal corneal diameter); VVID=vertical visible iris diameter (vertical corneal diameter); IOP=intraocular pressure, D=Dioptre, mm=millimeter, μm=micron meter, mmHg=millimeter of mercury, CI=confidence interval, SD=standard deviation, M=males, F=females.
A one-way ANOVA shows that gender did not significantly affect central corneal thickness (p=0.42). Also, there was no significant interaction effect of gender and age group on CCT (p=0.61).
The effect of age and gender on corneal diameterAge had no significant effect on vertical corneal diameter (VVID, p=0.09, Table 4). However, the effect of age group on VVID was significant (p=0.01). Post hoc test (Fisher's LSD) shows that the VVID of the 20–39 years and 40–49 years age groups was each significantly higher than the value for the 70–79 years age group (mean difference 0.4mm). Similarly, the 50–59 years and 60–69 years age groups had significantly deeper VVID than the 70–79 years age group (mean differences equal 0.3 and 0.6mm, respectively). In the same way, age had no significant effect on horizontal corneal diameter (HVID, p=0.11, Table 4). Nevertheless, HVID was significantly different between age groups (p=0.03).
Gender did not significantly affect VVID (p=0.75). Males had wider HVID than females (p=0.03). There was no significant interaction effect of gender and age group on VVID (p=0.41) and HVID (p=0.35).
The effect of age and gender on corneal curvatureFemales had slightly higher mean average corneal curvature (AVK) than males. However, age, age group and gender did not significantly affect horizontal, vertical or average corneal curvature.
The effect of corneal diameter (HVID and VVID) and corneal curvature on CCTThere was no significant association between CCT and VVID (p=0.63) or between CCT and HVID (p=0.80). Similarly there was no association between CCT and horizontal (p=0.80), vertical (p=0.80) or average corneal curvature (p=0.70).
The effect of age, gender, corneal diameter and CCT on IOPTable 4 shows the results of the measured intraocular pressure according to age group. Age, age group and gender did not affect IOP. Similarly, horizontal and vertical corneal diameter did not significantly correlate with IOP. The association between measured IOP and CCT in normotensive subjects was not significant (p=0.63).
DiscussionCCT is routinely measured in the clinic before corneal refractive procedures and also because of its potential to significantly affect the measured intraocular pressure and consequently the classification and treatment of glaucoma.3,6,13–16,20,25,41
The present study has demonstrated a mean CCT of 548.97±34.28μm (95% CI=543.02–554.92μm) for Nigerian adults with normal intra ocular pressure. CCT values in Nigeria adults outside of this range may be abnormal and could potentially affect measured IOP. Analysis showed that the CCT of our subjects was normally distributed. The normal distribution of CCT had been previously reported.12,17,23 Prior studies of CCT on Nigerian subjects (Table 2) returned values ranging from 535.0 to 551.6μm.14,24–26 The mean age of the subjects studied by Mercieca and colleagues14 was 63.1±11.2 years compared to 47.8±16.8 years for the current subjects. This difference in mean age probably explains why their mean CCT (535.0±38.0μm) was smaller than the current value (548.97±34.28μm). We have established that CCT decreases with age. The mean CCT (537.61±34.98μm) of our 60–69 years old subjects is similar to the average value (535.0±38.0μm) reported by Mercieca et al.14 Babalola et al.,26 investigated normotensive and glaucoma subjects (mean age=46 years; standard deviation=13.8 years, range=9–78 years). The average CCT of all subjects was 537.9±38.4μm (95% confidence interval 532.1–543.7μm). The difference between our value and that obtained by Babalola et al.,26 may be due to the category of subjects studied. The glaucoma subjects will be expected to have lower the average CCT although their average age is similar to that of our volunteers. The average values reported by Iyamu and Itua25 are similar to the present findings. The male subjects studied by Iyamu and Memeh24 had thicker CCT (561.8±44.9μm, 95% CI=529.7–593.9μm) than our male subjects (551.00±37.2μm). The reason for the difference in these values is not immediately clear. However, females in both studies had similar CCT. Our mean CCT for Nigerians may not be comparable to values reported for Sudanese19 because the average age of the subjects and their ethnicity (Africans versus Arabs) was not known. The mean CCT of male and female Cameroonians27 was slightly less than our value. The difference (19.68μm) is small and less than 1SD and may therefore not be clinically significant.
Reported CCT for African-Americans ranges from 521.0 to 555.0μm.3–6 Some of these values are outside the 95% confidence interval obtained in the present experiment (543.02–554.92μm). This observation implies that the average CCT of African-Americans may be different from values reported for Nigerians. This may be related to different experimental methods, environmental factors, category of subjects investigated, genetics and the inhomogeneity of reported racial background among African Americans.4
The mean values of the central corneal thickness as a function of age group are represented in Table 4. We established that age was significantly related to CCT. The relationship was best represented by the equation: CCT=583.16–0.72*AGE. According to the formula, a 10-year increase in age would lead to approximately a 7.0μm decrease in CCT. Previous investigators reported no significant association between CCT and age in normotensive Nigerians.24,25 This discrepancy may be due to the narrow age range and small sample size of subjects previously studied. Brandt et al.,5 reported a significant rate of decrease of CCT with age (6.3μm per decade). Foster et al.,42 observed a thinning of 10μm per decade. These rates are similar to the value obtained presently. Several investigators have reported a significant effect of age on CCT3,5,9,13,14,17 while others found that age did not affect CCT.6,19,21 Faragher et al.,43 commented that keratocytes are the major cellular components of the cornea stroma. They observed that the keratocytes density decreases with age and that the collagen fibres are broken down as part of the normal aging process. Hahn et al.13 argued that these changes are the most likely reasons for the observed reduction in CCT with age.
Gender had no significant effect on CCT among normotensive Nigerian adults contrary to the report of Mercieca et al.14 who found that Nigerian males have thicker CCT (541.0±47.0μm) than their female counterparts (522.0±22.0μm). However, it could not be ascertained if the reported that significant difference in CCT between men and women was age related since the average age of the male and female subjects was not provided. Our observation was consistent with the finding of Aghaian and colleagues,3 Durkin et al.,16 and Eysteinsson et al.21 However, others have reported that gender significantly affects CCT.6,13 Shimmyo et al.,6 combined subjects of different racial groups (Caucasians, Asians, Hispanics and African-Americans). This may have led to their finding that male subjects had thicker corneas than their female counterparts. Hahn et al.,13 also found that male Latinos had thicker corneas than females. The difference between the genders was only 4.6μm. They observed that this was less than the mean interocular difference in CCT (7.7μm) for their normal subjects. They concluded that the difference between men and women was statistically but not clinically significant.
The present results show that CCT did not significantly affect measured intraocular pressure in subjects with normal IOP. However, other authors21 reported a significant association between CCT and IOP among normotensive groups. Eysteinsson et al.,21 studied Northern Europeans (Icelanders). IOP was measured by non-contact tonometer while CCT was measured by Scheimpflug slit images of the anterior eye segment. The difference between our findings may therefore be related to differences in methodology and possibly genetics and/or environmental factors.
The effect of age groups on corneal diameter (VVID, HVID) was significant. The oldest age group (70–79 years) had significantly smaller corneal diameter than the younger age groups. This may be linked to the smaller average height for the oldest group. Fledelius and Stubgaard44 and Quant and Woo45 reported that certain facial measurements including inter outer orbital distance and the interpupillary distance decreases with age. This finding was explained by the smaller stature of the older generation. Also, there are reports of the decrease in axial length with age.46–49 Although males had significantly wider HVID, gender did not significantly affect VVID. This finding may be explained by the fact that men are generally taller and have correspondingly larger eyes than women.50–52 Henriques et al.,37 reported a significant positive association between corneal diameter and axial length (p<0.0001).
The tendency for females to have steeper corneas may be linked to the fact that females have shorter axial length than males.33,52–56 Smaller eyes are associated with steeper corneas.20,50,54 Several investigators20,21,28,29 have reported no association between CCT and central corneal radius of curvature (CR). In contrast to others6 have found that CCT was negatively correlated with corneal curvature. Thicker corneas are flatter and thinner corneas are steeper. The relationship between cornea curvature and CCT may be confounded by gender as the female cornea is on the average thinner than the male cornea.6
Kotecha57 reasoned that the low coefficient of determination between CCT and IOP suggests that corneal biomechanical properties may also have significant influences on IOP measures. Two of the corneal biomechanical properties that have been investigated include corneal hysteresis, CH (a measure of visco-elasticity) and corneal resistance factor, CRF (a measure of elasticity). Recent evidence suggests that there is a positive and significant correlation between CCT and CH, CCT and CRF and CCT and IOP in normal eyes.58,59 Consequently the age related changes in CCT observed in the current study imply that the corneal biomechanical properties may be affected consequently impacting on measured IOP.
The strength of this study is that we investigated more subjects than previous studies of CCT in adult Nigerians. We also studied for the first time among Nigerian subjects, the relationships between age, gender, corneal curvature, corneal diameter (horizontally and vertically), CCT and IOP. One potential weakness of our study is that we did not provide the refractive error of our subjects. Iyamu and Itua25 had demonstrated that spherical equivalent of refraction was not significantly correlated with CCT in Nigerian adults.
In conclusion, our results show that the average CCT of Nigerian adults with normal intra ocular pressure is 548.97±34.28μm (95% CI=543.02–554.92μm). Clinically this means that CCT values outside of this range in Nigeria adults may be abnormal and could potentially affect measured IOP. There was a significant decrease in the CCT with age. This relationship was represented by the equation, CCT (μm)=583.16–0.72*AGE. This will be useful to predict the CCT of normotensive Nigerian adults. Consequently extra caution should be exercised in interpreting IOP measurements in older Nigerian subjects because the natural thinning of the CCT is likely to lead to lower values of IOP measurements. This could potentially affect the diagnosis, classification and therapy of glaucoma. We are currently not aware of any data on the rate of corneal thinning with age in patients that have undergone photorefractive surgery. If the same rate of corneal thinning currently found is maintained (7μm per decade), then this could have clinical implications in the future for young patients undergoing photorefractive surgery. For example, a 20-year-old patient with a postoperative CCT of 400μm will have a CCT of 379μm in 30 years! Our findings imply that accurate measurement of CCT should be undertaken in all candidates to undergo corneal photorefractive refractive surgery as is currently the case. Also in cases where a patient displays the signs and symptoms of glaucoma but where the IOP is within the normal value, they should be questioned about any history of previous corneal ablation refractive surgery. Corneal curvature, corneal diameter and gender did not significantly affect CCT.
Conflict of interestsThe author has no conflict of interests to declare.