A clinical evaluation of the L80 videokeratographer (Visionix Luneau, Chartres, France) was performed to assess its validity and repeatability compared with a traditional Bausch and Lomb (B & L) keratometer.
Methods87 right eyes of 87 subjects, (mean age 23.72±3.62 years old, 70 women and 17 men), participated in this study. Corneal curvature was measured using the L80 instrument by one practitioner and the manual B & L keratometer by a different practitioner. Intratest and intertest repeatability were assessed.
ResultsCorneal curvature was found to be statistically different between the two instruments (p<0.001), with the L80 providing a slightly steeper bias of 0.05mm and 0.07mm for the horizontal and vertical meridians, respectively than the B & L keratometer. 78.2% and 86.2% of the L80 results were within ±0.1mm (±0.06D) and 95.4% and 97.7% within ±0.2mm (±0.11D) of the readings obtained with the B & L keratometer along the horizontal and the vertical meridians, respectively. The agreement between the L80 and B & L keratometers axes was 31.0% within ±5°, 54.0% within ±10°, 60.9% within ±15°, 71.3% within ±20° and 87.4% within ±40°. Intratest repeatability was the same for both instruments. Intertest repeatability was better for the L80 videokeratographer compared to the B & L keratometer and showed no significant difference between the two sessions.
ConclusionThe L80 videokeratographer is a reliable objective instrument comparable to other autokeratometers which, in addition, combines many other useful clinical features. It provides steeper radii of curvature measurements than the B & L keratometer. An offset incorporated into the instrument could mitigate the difference between the two instruments and make them interchangeable.
se llevó a cabo una evaluación clínica del videoqueratógrafo L80 (Visionix Luneau, Chartres, Francia) para valorar su validez y repetibilidad en comparación con el queratómetro tradicional Bausch and Lomb (B&L).
Métodosen este estudio se examinaron 87 ojos derechos de 87 sujetos (media de edad 23,72 ± 3,62 años, 70 mujeres y 17 hombres). La curvatura corneal se midió utilizando el instrumento L80 y el queratómetro manual B&L, cada uno manejado por un examinador diferente. Se evaluó la repetibilidad intratest e intertest para los dos instrumentos.
Resultadosse obtuvieron medidas de curvatura corneal estadísticamente diferentes con los dos instrumentos (p < 0,001): el L80 proporcionó medidas ligeramente más curvas que el queratómetro B&L, 0,05mm y 0,07mm para los meridianos horizontal y vertical, respectivamente. El 78,2% y el 86,2% de los resultados del L80 se encontraban dentro de ± 0,1mm (± 0,06 D) y el 95,4% y el 97,7% dentro de ± 0,2 mm (± 0,11 D) de las lecturas obtenidas con el queratómetro B&L a lo largo del meridiano horizontal y vertical respectivamente. Se obtuvo una concordancia en los ejes de las medidas queratométricas obtenidas con los instrumentos L80 y B&L del 31,0% entre ± 5°, del 54,0% entre ± 10°, del 60,9% entre ± 15°, del 71,3% entre ± 20° y del 87,4% entre ± 40°. La repetibilidad intratest fue la misma para ambos instrumentos. La repetibilidad intertest resultó mejor con el videoqueratógrafo L80 que con el queratómetro B&L aunque no hubo diferencias significativas entre las dos sesiones.
Conclusiónel videoqueratógrafo L80 es un instrumento objetivo fiable en comparación con otros queratómetros automáticos y, además, contiene muchas otras herramientas clínicas de gran utilidad. Proporciona unas medidas de de radio de curvatura algo más curvas que el queratómetro tradicional B&L. Mediante la incorporación de un factor de corrección en las medidas queratométricas proporcionadas por el sistema L80 se podría limitar la diferencia entre ambos instrumentos y hacerlos intercambiables.
Many optometrists in clinical practice measure corneal curvature prior to contact lens fitting. Most of them still use their manual and subjective keratometers, such as the Javal-Schiotz or Bausch and Lomb (Helmholtz) keratometer. Recently, automated keratometers have become popular because they provide an objective measurement very rapidly, easily and over a much larger corneal area than manual keratometers (usually 9mm or more vs. 3mm). These instruments are used not only in contact lens practice but also in refractive surgery,1 in calculations of intraocular lenses prior to cataract surgery2,3 and in detecting and evaluating the severity of keratoconus,4–8 although most clinicians nowadays have opted for corneal topography as a means of detecting keratoconus.9–11
There are several autokeratometers currently available such as the Grand Seiko W-5100K and Grand Seiko Auto Ref/Keratometer WAM-5500,12,13 the Canon RK2,14,15 the Topcon KR,16 the Zeiss IOL Master,17 the Zeiss Humphrey HARK and the new optical low coherence reflectometry device (LenStar).18 Most of these instruments combine keratometry and refractometry, except the IOL Master and the LenStar. The L80 (Visionix Luneau, Chartes, France) is a new instrument that combines refraction,19 topography and keratometry, but can also measure higher-order aberrations to the 7th order of the Zernike polynomial function series.20 The keratometric function of the L80 analyses the image of the concentric rings of a Placido disk that is reflected on the anterior cornea. The illumination consists of red light of wavelength 650nm. In the analysis, each ring is split into 256 radial spots which are fitted with an ellipse. The ellipse is compared with an image from a calibration eye to calculate the local radius. There are 24 rings in total thus giving 6144 analysis points for the entire cornea (9.5mm in diameter). The instrument is factory-tested for corneal curvatures in the range 6–9mm, corresponding to 37.5–56.25D. The screen display shows steps of 0.01mm for the radius and steps of 1° for cylinder axis. The keratometric radii, K1 and K2, which indicate the flat and steep curvatures, are given for 3mm, 5mm and 7mm corneal diameters separately in the corneal topography function; alternatively a Sim-K value that simulates the reading of a standard subjective keratometer is also given. The 3mm, 5mm and 7mm corneal diameter values are calculated from the corresponding rings that cover these corneal areas. The Sim-K value that is used for the keratometric function is calculated from rings that cover the area of 2–4mm, similar to a standard keratometer. The radii of curvature (in mm) is converted to powers automatically by the software using a refractive index of 1.3375. The aim of the present study was to evaluate the agreement and repeatability of the keratometric values of the measurements obtained with the L80 automatic videokeratographer and the manual Bausch and Lomb (B & L) keratometer.
MethodsThis study was approved by the ethics committee of Hadassah Academic College, Jerusalem and carried out according to the tenets of the Declaration of Helsinki. Participants were students of the Department of Optometry at Hadassah Academic College. Exclusion criteria included a history of contact lens wear or corneal or ocular surgery, trauma and ocular pathology. The nature of the research was explained to all subjects before signing an informed consent form. The right eye of each subject was used in all analyses.21
Keratometry was performed on the right eye of all participants by two practitioners (MZ and MW) who were masked to each other's results and both very experienced in using these particular instruments. B & L keratometry was carried out by MZ, and L80 autokeratometry in almost all instances by MW. Participants were asked to perform a complete blink before each measurement. The calibrations of both instruments were checked at the beginning and at the end of the study according to the manufacturers’ instructions. The eyepiece of the B & L was adjusted before each reading to avoid introducing accommodative errors and the instrument was realigned before each measurement. The L80 has auto-focusing and auto-centring and automatically moves to the other eye to complete the measurement cycle. Three measurements were recorded for the right eye and an average was calculated with each instrument. Although the L80 automatically records the data for both eyes we used only the results of the right eye for the analysis, since the two eyes of the same subject are not independent and are highly correlated.21 The Sim-K value for keratometry obtained with the L80 system was used for the comparative analysis. Approximately half of the subjects were randomly measured firstly with the B & L keratometer and the other half with the autokeratometer and the procedure was then reversed. Agreement between the two instruments was analyzed for each principal meridian and calculated as suggested for repeated measurements by Bland and Altman.22,23
Intratest repeatability of each instrument was determined in all subjects (n=87) and estimated in terms of standard deviations of the difference as well as two way analysis of variance (ANOVA) to determine whether there were significant differences between the three measurements for each subject, for both the horizontal and vertical meridians.21 We also calculated the coefficient of repeatability using the formula 1.963× within-subject standard deviation,21 which is a measure of the interval within which 95% of the measurement differences lie. Intertest repeatability was estimated by calculating the p value between the first and the second set of measurements obtained 1–60 days after the initial data on 24 of the original subjects who were willing to participate in this part of the experiment. This is not an uncommon occurrence. In Buckhurst el al.18 only 31 patients out of the initial 112 participated in a similar part of their experiment and the figure was n=22 and n=23 in other reports on intertest repeatability of corneal curvature measurements.24,25 Obviously this gives a low power, which we have estimated to be 68% using Altman's nomogram.26 All data samples were normally distributed (Anderson-Darling test). Therefore, we used the Student's t-test for paired data to assess the difference between variables and calculated the confidence intervals (CI). p values of 0.05 or lower were considered statistically significant.
Results87 students (87 eyes) from the Department of Optometry at Hadassah College participated in the study. The mean age of the cohort was ±SD: 23.7±3.6 years old; range 18–37 years. Mean (±SD) astigmatism was −0.53D (±0.65) and the maximum value was −3.31D. For the intertest repeatability study, 24 students participated (24 eyes; mean age 25.75±2.81 years old).
Mean keratometric values measured with the L80 and B & L keratometers for the two principal meridians are given in Table 1. The radius of curvature was flatter along the vertical meridian with both instruments. The data showed that the L80 yielded steeper radii of curvatures than the manual B & L keratometer.
Mean (±SD) readings (in mm) obtained with the L80 and B & L keratometers and 95% confidence intervals (CI) of the mean of the differences (N=87 right eyes of 87 subjects).
| L80 | B & L | p value | Mean difference (95% CI) | |
| Horizontal K | 7.70±0.03 | 7.76±0.02 | p<0.001 | −0.05 (−0.026 to −0.074) |
| Vertical K | 7.57±0.03 | 7.65±0.01 | p<0.001 | −0.07 (−0.053 to −0.087) |
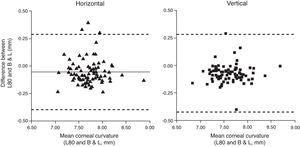
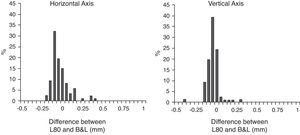
The validity of an instrument or procedure is generally expressed in terms of agreement with another or with a standard reference12,17,22,27 and this is represented by plotting the difference between the methods for each subject against their mean. The mean differences (bias) of the present data are given in Fig. 1(a and b) and are equal to −0.05mm (95% CI −0.026 to −0.074) and −0.07mm (95% CI −0.053 to −0.087) for horizontal and vertical meridians, respectively (Table 1). The limits of agreement (LoA) between the two methods were −0.40 to 0.29 (or ±0.35mm) for the horizontal and between −0.42 and 0.28 (or ±0.35mm) for the vertical meridian (Fig. 1). About 78.2% of the L80 results were within ±0.1mm (±0.06D) and 95.4% within ±0.2mm (±0.11D) of the readings obtained with the B & L keratometer along the horizontal meridian and 86.2% within ±0.1mm (±0.06D) and 97.7% within ±0.2mm (±0.11D) along the vertical meridian (Fig. 2).
Difference in (A) horizontal axis and (B) vertical axis between the L80 autokeratometer and B & L keratometer, plotted against the mean corneal curvature. Mean bias is indicated by the solid lines and the 95% limits of agreement by the dashed lines (n=87 eyes). Each data point represents the mean of three measurements.
The agreement between the L80 and B & L keratometers axes was 31.0% within ±5°, 54.0% within ±10°, 60.9% within ±15°, 71.3% within ±20° and 87.4% within ±40°. Better agreement between the two instruments was found with increasing corneal astigmatism. For corneal toricity ≥0.20mm (with the B & L), the mean difference in axes between the two instruments was 3.04±2.94° (n=15) and for toricity below this magnitude, the mean difference was 21.68±23.19° (n=72).
The mean and standard deviation of the three repeated measurements of the curvature of the horizontal and vertical meridians obtained in each subject in one session with each instrument are shown in Table 2. The table also gives the within-subject variance and coefficient of repeatability23 for each instrument. The coefficient of variation (standard deviation/ mean x100%) for each instrument were calculated and found to vary between 0.13 for the B & L and 0.39 for the L80. Two-way ANOVA showed no significant differences between the repeated measurements for both instruments and along both meridians (p=0.09–0.99).
Intratest (n=87) and intertest (n=24) variability of the curvature results obtained with the L80 and B & L keratometers.
| L80 | B & L | |||
| Horizontal | Vertical | Horizontal | Vertical | |
| Intratest | ||||
| Mean of 1st session (mm) | 7.70 | 7.57 | 7.76 | 7.65 |
| Within-subject variance | 0.18 | 0.18 | 0.12 | 0.12 |
| Coefficient of repeatability | 0.61 | 0.61 | 0.41 | 0.41 |
| Intertest | ||||
| Mean difference (mm) | 0.010 | 0.004 | −0.016 | −0.034 |
| SD of difference (mm) | 0.055 | 0.059 | 0.058 | 0.093 |
| p value (between 1st and 2nd session) | 0.397 | 0.767 | 0.197 | 0.085 |
The intertest repeatability was much better for the L80 autokeratometer than for the manual B & L keratometer and the curvatures measured in the second session with the B & L were steeper than in the initial session. This was not statistically significant for both the horizontal meridian (p=0.197) and the vertical meridian (p=0.085). The data are shown in Table 2. The small, but not significant, increase in steepening observed in the second session only with the manual B & L could be explained by differences in external factors, such as realignment, tear instability28 or measurements made at different times of day.
DiscussionThe results of this study showed that the mean curvature in the horizontal and vertical meridians differed significantly when measured by either the L80 autokeratometer or the manual B & L keratometer (mean difference: −0.053mm (0.28D) p<0.0001; −0.072mm (0.37D) p<0.0001; respectively), with the L80 providing a slightly steeper mean radius of curvature than the B & L instrument (Table 1). One possible reason for the significant difference between the results of the L80 and B & L instruments may stem from variations in keratometric measurement procedure of the two instruments: the autofocus function of the L80 reduces the number of potential focusing errors compared with the slower manual measurement procedure of the B & L keratometer. Moreover, the fact that two different practitioners, albeit experienced, performed the measurements could, to some extent, account for the discrepancy and furthermore changes in tear film properties are known to vary continuously throughout the day. The mean difference between the two instruments is clinically significant (>0.25D) and the two instruments cannot be used as interchangeable. Shirayama et al.29 also found a statistically significant difference between the IOLMaster and the Bausch & Lomb devices. Since the L80 gave steeper radii of curvature than the B & L keratometer it would seem to be beneficial for the L80, a new instrument, to incorporate in its software a mathematical offset to the keratometric value of 0.05mm. This would eliminate the mean difference in the horizontal meridian and reduce the difference to 0.02mm in the vertical meridian, which is not clinically significant. The findings from both instruments indicated a steeper curvature along the vertical than the horizontal meridian, which is to be expected in a group of young subjects in whom astigmatism is usually “with the rule”.30–32
The steeper radius of curvature provided by the L80 is consistent with the results of Sheppard and Davies12 who found that the Grand Seiko Autokeratometer WAM-5500 gave a mean value steeper by 0.05mm in the horizontal and 0.06 in the vertical meridian than a Javal-Schiotz keratometer. This is in agreement with other studies which reported a mean astigmatism steeper with the Zeiss IOL Master than with a Javal-Schiotz instrument17,33 or a B & L keratometer.29
The standard deviations for the horizontal and vertical meridians were almost the same (Table 1) with both instruments, which indicated a consistent variance along both meridians, whereas other investigators have reported greater variations in the vertical meridian, albeit to a different extent and measured with other instruments.12,13,32 In our study the limits of agreement (LoAs) between the two instruments were found to be ±0.35mm (Fig. 1). Davies et al.13 reported LoAs of ±0.17mm and ±0.27mm for the horizontal and vertical meridians, respectively and Sheppard and Davies12 found LoAs of ±0.15mm and ±0.16mm for the horizontal and vertical meridians, respectively. Shiriyama et al.29 found a mean difference (bias) between the Zeiss IOL Master and B & L keratometer (0.16D) and a narrower LoA than in our study. The discrepancy with our results may be due in part to the participation in their investigation of a sample of older subjects (mean 36±12.5 years) with some presbyopic eyes. Miranda et al.25 found no significant changes in anterior corneal curvature with a slightly younger sample (19–40 years; mean age 26.74±5.30 years) and no presbyopes. Alternatively the discrepancy could be inherent to the difference in instruments (IOL Master and L80), or to some other external factors,28 or to the fact that we used the analysis suggested by Bland and Altman in their 1999 paper, whereas comparative studies used the formula from their 1986 paper, which underestimates the LoA.
Repeatability in measuring corneal curvature with both instruments at the same session (intratest) showed standard deviations of 0.02–0.03mm and within-subject variance of 0.12–0.18mm (Table 2). The analysis of variance (ANOVA) of the three measurements for the two meridians and the two instruments were not significant indicating a good degree of reliability. The coefficients of repeatability also showed a smaller range of variability of measurements for the B & L than for the L80 instrument (Table 2). Results obtained by Koch et al.31 using a B & L keratometer were similar to our findings with the same instrument and slightly better than those obtained with the EyeSys Corneal Analysis System, although Hough and Edwards34 found intratest SD of 0.08mm with the EyeSys instrument. Buckhurst et al.18 obtained a similar intratest repeatability to ours with an SD of 0.14D (0.028mm). Other studies showed smaller SD using the Zeiss IOL Master: Vogel et al.35 obtained intratest SD of 0.013mm with five subjects much older (mean age: 37 years, range 26–72 years) than in our sample and similar outcomes were obtained by Shirayama et al.29 in a sample of subjects of mean age 36 years (range 23–62 years). The difference between our results and those obtained with the IOL Master may be due to the different instrumentation. It is also likely that the discrepancy was due to the fact that our sample of subjects was much younger (mean age 25.75±2.81 years) than in the other studies, in which presbyopic patients were included. This may have led to wider standard deviations since fluctuations in accommodation have been shown to induce changes in corneal curvature.36,37
Intertest repeatability in which measurements are made at different sessions is of greater importance than intratest repeatability. It was found to be higher with the L80 autokeratometer than with the B & L keratometer. The mean difference in readings measured on different days did not exceed 0.01mm (±0.055) for horizontal meridian and 0.004 (±0.059) for vertical meridian with the L80 whereas it was between 0.016mm and 0.034mm with the B & L instrument for the horizontal and vertical meridians, respectively. The results obtained with the L80 are similar to those of other studies,12,13,17 some of them reporting smaller mean differences but wider SDs.13,17 The worst repeatability was demonstrated with the Orbscan II24 (Table 3).
Common autorekeratometers and their repeatability.
| Instruments | Manufacturer | Type | Mean repeatability | 95% confidence interval | |
| Santodomingo-Rubido et al.17 | IOLMaster | Zeiss Instruments | Reflection from six points of light arranged hexagonally | 0.00mm | −0.04 to 0.04 |
| Cho et al.24 | Humphrey Atlas 991 | Zeiss Humphrey | Reflection of concentric rings | 0.001mma | −0.07 to 0.08 |
| Cho et al.24 | Orbscan II | Bausch & Lomb Inc. | Slit-scanning | −0.3mma | −0.47 to 0.41 |
| Cho et al.24 | Medmont E300 | Medmont International | Reflection of concentric rings | 0.005mma | −0.05 to 0.06 |
| Davies et al.13 | Shin-Nippon NVision-K5001 | Shin-Nippon Commerce | Reflection of three arcs | 0.00±0.12mm | |
| Huynh et al.32 | RK-F1 Auto-Ref-Keratometer | Canon Inc. | Reflection of a circular mire | −0.005mma | −0.01 to 0.004 |
| Miranda et al.25 | Pentacam | Oculus Inc. | Slit-scanning with a rotating Scheimpflug camera | 0.01mm | −0.09 to 0.10 |
| Sheppard and Davies12 | Grand Seiko AutoRef/K WAM-5500 | Grand Seiko Co. | Reflection of a ring | 0.00±0.06mm | −0.009 to 0.009 |
| Current study | L80 | Visionix Luneau | Reflection of concentric rings | 0.01±0.05mm | −0.01 to 0.03 |
Corneal curvature data showed reasonably good agreement between the two instruments with regard to axes, with slightly more than half of all objectively determined axes within 10° of those measured with the B & L keratometer, although that figure varied with the degree of astigmatism, being more accurate the greater the astigmatism was. However, Sheppard and Davies12 found closer agreement between the Grand Seiko Autokeratometer WAM-5500 and Javal-Schiotz keratometer, which may in part be accounted for their slightly older sample of subjects including some presbyopes (range 18–69 years) in whom there may be less variation in corneal curvature with accommodation36,37 than in the young group of subjects in our study, notwithstanding the fact that the Grand Seiko is an open-field instrument thus mitigating the effect of accommodation. Nevertheless, it must be noted that measurements with the B & L keratometer may be liable to errors because it has a shorter working distance than the Javal-Schiotz keratometer used in Sheppard and Davies's study.12
In summary, the results of this study showed that the L80 videokeratographer is a reliable instrument for measuring corneal curvature comparable to other autokeratometers currently available.12,13,29 However, to render this instrument interchangeable with the standard B & L keratometer it would need a software adjustment. In addition, the L80 provides an objective measurement much more rapidly than traditional keratometry and it has other useful features for the determination of refraction,19 higher-order aberrations and corneal topography.
We would like to thank Dr. Ian Melnick for help with analysis and for critical reading of the manuscript, Dr. Gary Roth for clinical support and Dr. Eric Karasanty for advice with statistics. Dr. Einat Shneor received a grant from the Israel Society of Psychobiology.