To assess the agreement between the Eye Refract, an instrument to perform subjective automated refraction, and the traditional subjective refraction, as the gold standard, in young hyperopes under noncycloplegic and cycloplegic conditions.
MethodsA cross-section and randomized study was carried out, involving 42 participants (18.2 ± 7.7 years, range 6 to 31 years). Only one eye was chosen for the analysis, randomly. An optometrist conducted the refraction with the Eye Refract, while another different optometrist conducted the traditional subjective refraction. Spherical equivalent (M), cylindrical components (J0 and J45), and corrected distance visual acuity (CDVA) were compared between both refraction methods under noncycloplegic and cycloplegic conditions. A Bland-Altman analysis was performed to assess the agreement (accuracy and precision) between both refraction methods.
ResultsWithout cycloplegia, the Eye Refract showed significantly lower values of hyperopia than the traditional subjective refraction (p < 0.009), the mean difference (accuracy) and its 95% limits of agreement (precision) being -0.31 (+0.85, -1.47) D. Conversely, there were no statistical differences between both refraction methods under cycloplegic conditions (p ≥ 0.05). Regarding J0 and J45, both refraction methods manifested no significant differences between them under noncycloplegic and cycloplegic conditions (p ≥ 0.05). Finally, the Eye Refract significantly improved CDVA (0.04 ± 0.01 logMAR) compared with the traditional subjective refraction without cycloplegia (p = 0.01).
ConclusionsThe Eye Refract is presented as a useful instrument to determine the refractive error in young hyperopes, the use of cycloplegia being necessary to obtain accurate and precise spherical refraction.
Subjective refraction represents the most important procedure in optometric practice and is considered the gold standard for evaluating refractive errors because it considers the optical and neural aspects of visual processing.1 Instead, objective refraction by retinoscopy or autorefraction represents a starting point to facilitate subjective refraction. However, autorefractors present some limitations, hindering to obtain accurate and precise refraction, mainly overestimating myopia or underestimating hyperopia.2-7
In the last few years, progress in automation processes allowed the dissemination in the market of new instruments to perform automated subjective refraction.8-14 The optical systems to conduct this automated refraction incorporate both an autorefractor for objective refraction and a phoropter for subjective adjustment into a single device. This allows for the automation of all the steps of refraction, which are guided by an automated algorithm and controlled by a hardware and software system, saving exam time.12-14
The Eye Refract (Luneau Technology; Chartres, France), which incorporates a binocular open-field aberrometer and a phoropter, was one of the first instruments to conduct automated subjective refraction. This system has been previously validated to determine refractive errors in a healthy general population and keratoconus patients.12,14,15 Nevertheless, the clinical implications of the Eye Refract in hyperopes, whose accommodative function could influence the result, especially when hyperopia is uncorrected or undercorrected,16 are still unclear.
It is known that hyperopes present an increased accommodative demand in both distance and near vision, increasing accommodative convergence, which could accompany a convergent eye misalignment, especially in high hyperopia.17 In addition, this accommodative effort could lead to a spasm of the ciliary muscle, resulting in latent hyperopia and the underestimation of this refractive error.18 Spasms and fluctuations in accommodation are factors inducing error in the refraction procedures, the reason why cycloplegia is used to paralyze the ciliary muscle, allowing to estimate more accurately and precisely the refractive error in these cases.19
Since instruments of automated subjective refraction have not been evaluated yet in a population whose accommodative response could be altered, the purpose of this study was to assess the agreement (accuracy and precision) between the Eye Refract (automated refraction) and the traditional subjective refraction (subjective refraction) in young hyperopes under noncycloplegic and cycloplegic conditions. The results of the Eye Refract were compared with the traditional subjective refraction as the gold standard to assess refraction.
MethodsThis study presents similar methods to those previously evaluating the accuracy and precision of the Eye Refract system in a healthy general population12 and keratoconus patients.14
Design of the studyA cross-sectional and randomized study was carried out following the good clinical practice guidelines, the institutional review board regulation, and the Declaration of Helsinki. The study protocol was approved by the research ethics committee of Hospital Clínico San Carlos (code 18/459-R_P; Madrid, Spain). All the procedures were performed at the University Clinic of Optometry of the Complutense University of Madrid. All participants were voluntarily included in the study after signing a written informed consent form where all the study procedures were detailed.
The measurements of each participant were taken in two different days: one day under physiological conditions (without cycloplegia) and another day under cycloplegia, randomly assigned during the same week. Each day, an optometrist conducted the automated subjective refraction with the Eye Refract system (automated refraction) and another different optometrist conducted the traditional subjective refraction (subjective refraction) in random order. Cycloplegia was induced by topical instillation of two drops, with an interval of 15 min, of a commercial 1% cyclopentolate hydrochloride (Alcon Cusí; Barcelona, Spain), and both refractions were conducted 15 min after the last instillation. In addition, neither optometrist had data about the refractions obtained by the other to avoid bias.
ParticipantsForty-two participants (18.2 ± 7.7 years, range 6 to 31 years; 32 female and 10 male) of a total of 50 evaluated were included in the study, choosing one eye per participant randomly (flipping a coin) for the statistical analysis.
Inclusion criteria were age between 6 and 35 years, a spherical equivalent between +0.50 D and +6.00 D with cycloplegia, and understanding and signing the informed consent (by the legal tutors in case of participants under 18 years). Exclusion criteria were clinical history of amblyopia, strabismus, or other visual dysfunction affecting binocular refraction, the presence of any ocular disease, surgery, or trauma, and the use of systemic or ocular drugs that could alter accommodation. Participants belonged to the University Clinic of Optometry database, and different optometrists of the clinic previously evaluated their accommodative and vergence functions before the visit to participate in the study.
Eye refract systemThe Eye Refract system is a binocular open-field aberrometer combined with a phoropter to conduct a fully automated refraction. All the procedures during the refraction were controlled by a digital tablet connected to the Eye Refract. Firstly, following the manufacturer's instructions, the participants were instructed to put their chin and forehead on the supports and to look ahead through the system at the fixation image projected on the digital screen at a 4 m distance. Then, the Eye Refract performed dynamic aberrometry in both eyes at the same time under physiologic pupil conditions. The two Hartmann-Shack sensors of the system incorporate an infrared light of 800 nm and chromatic aberration is compensated after this measurement. The pitch of the microarray lenses is 0.1 mm. The wavefront metric used for determining the objective refraction is based on the principle of equivalent quadratic, using the method of paraxial curvature matching proposed by Thibos et al.20 This metric considers the Zernike coefficients C02 and C04 for spherical equivalent (M) determination, C22 and C24 for vertical cylindrical component (J0), and C − 22 and C − 24 for oblique cylindrical components (J45).
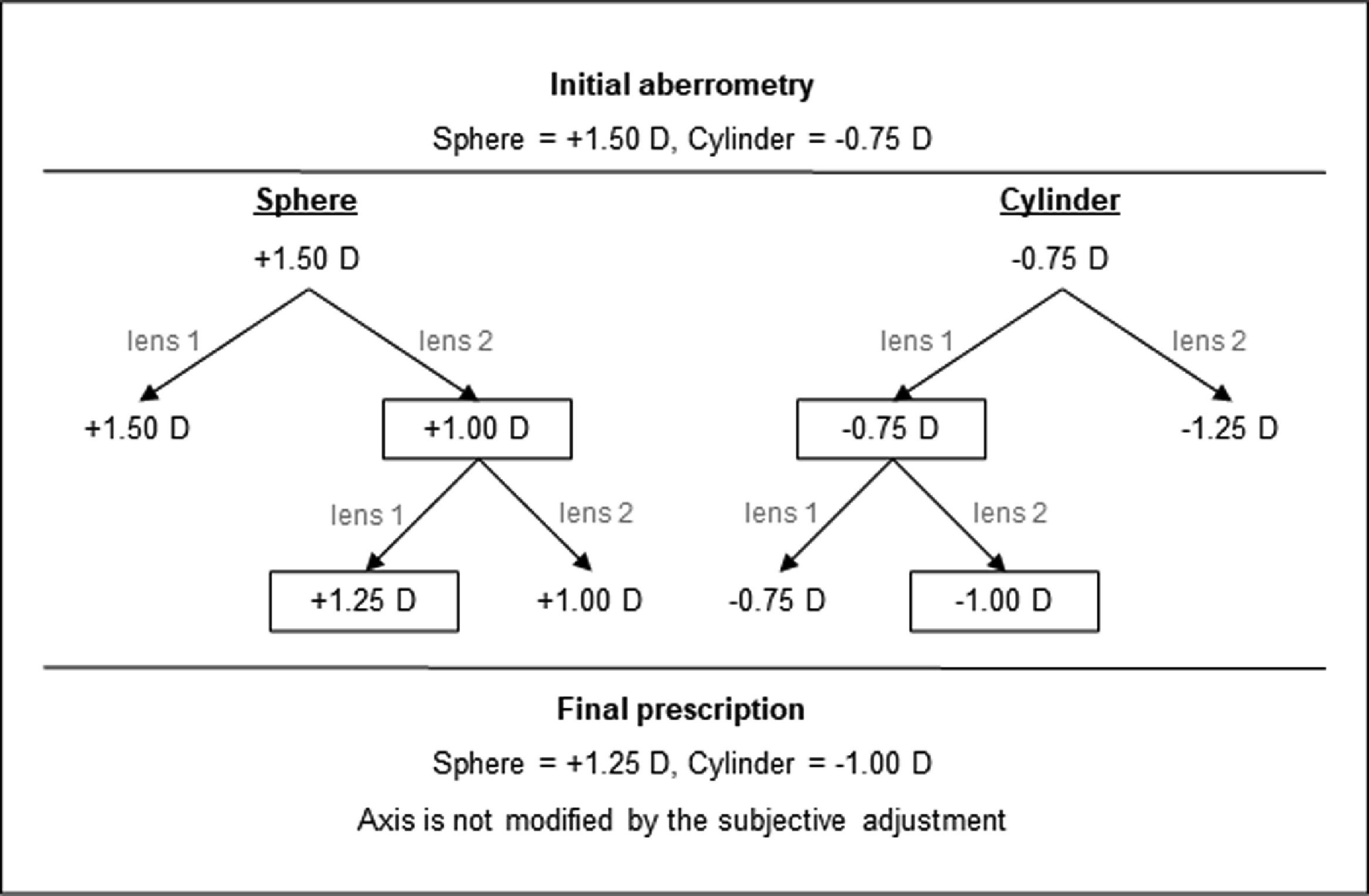
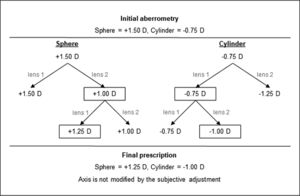
Considering the objective refraction as a starting point to perform the subjective adjustment, the Eye Refract adjusted the final refraction after a series of questions to the participants asked by the optometrist. These questions consisted of comparing a series of two spherical lenses, firstly, and two cylindrical lenses, secondly: “Are the letters clearer with lens 1, lens 2, or are they the same?”. The refraction was adjusted based on the answers of the participants and the automated algorithm of the Eye Refract, as the example in Fig. 1 shows.
Representative scheme with an example of how the automated algorithm of the Eye Refract modifies the initial aberrometry to obtain the final prescription based on the subject's answers. The algorithm of the Eye Refract only considers the two comparisons shown to measure the sphere, firstly, and the cylinder, secondly.
The traditional subjective refraction was performed with a trial frame by a different optometrist in the same laboratory and using the same digital screen as for automated refraction by the Eye Refract. The optometrist began all the refractions with retinoscopy. After that, starting from the raw value of the retinoscopy, the maximum positive (or minimum negative) sphere to reach maximum visual acuity was obtained by the fogging technique. Then, the cylinder was adjusted by the astigmatism chart numbered from 1 to 12 (clockwise, in steps of 30°), followed by the ±0.50 D Jackson cross-cylinder to obtain the final axis and cylinder. Finally, the maximum positive sphere was adjusted again. This refraction procedure was the same for all the participants, evaluating first the right eye and the left eye later.
Analysis of refractive variablesOnce the sphere and cylinder were determined with the different refraction methods, the refractive variables were analyzed in terms of M, J0, and J45 according to the method proposed by Thibos et al.21:
where enantiomorphism associated with J45 was corrected changing the sign of the left eye.Measurement of visual acuity and time spentCorrected distance visual acuity (CDVA) was monocularly measured with the high-contrast (100%) Early Treatment Diabetic Retinopathy Study test of the digital screen of the Eye Refract placed at 4 m, once each refraction was finished. CDVA was measured through the oculars of the Eye Refract, in the case of automated refraction with this system, and with a trial frame, in the case of traditional subjective refraction.
The time spent performing each refraction was measured with a timer. With the Eye Refract, the time was measured from the dynamic aberrometry to the final visual acuity measurement. With traditional subjective refraction, the time was measured from the initial visual acuity measurement to the final visual acuity measurement.
Statistical analysisStatistical analysis was performed with the software SPSS Statistics 23 (IBM; Chicago, Illinois, USA). The normality of the distributions for each variable was assessed using the Shapiro-Wilk test. Once normality was confirmed, the one-way analysis of variance (ANOVA) for related samples with Bonferroni correction was applied for the pairwise comparison between the different refraction methods (noncycloplegic subjective, cycloplegic subjective, noncycloplegic automated, and cycloplegic automated). Furthermore, the Bland-Altman analyses were performed to assess the agreement (accuracy and precision) between the different refraction methods. The 95% limits of agreement (precision) were mathematically defined as “1.96 x the standard deviation of the mean difference between two refraction methods (accuracy)”.22 A statistical significance of 95% (p < 0.05) was established. Additionally, the Pearson correlation coefficient between the age of participants and the mean difference between two refraction methods was calculated. A statistical significance of 95% (p < 0.05) was established for all the tests.
The studied variables were M, J0, J45, CDVA, and time spent performing refraction. The values are expressed as mean ± 1 standard deviation.
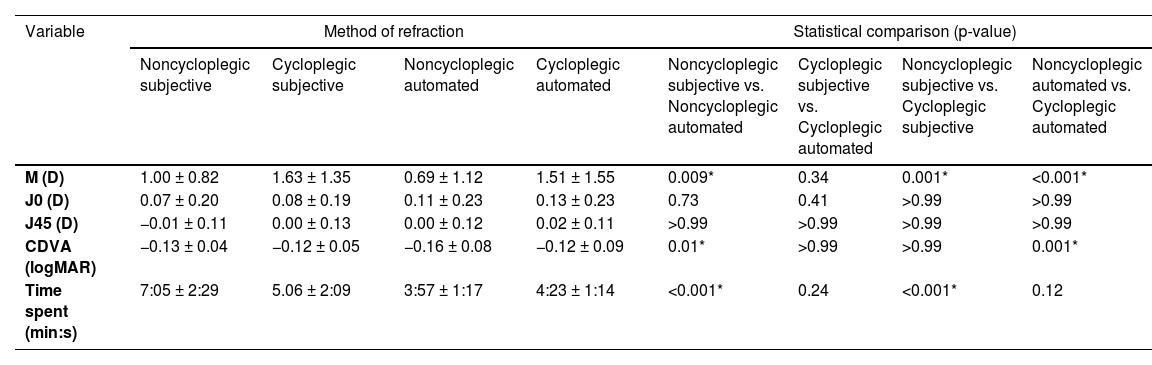
ResultsTable 1 summarizes the values of all the studied variables with the different refraction methods and the pairwise statistical comparison between them.
Values of spherical equivalent (M), cylindrical components (J0 and J45), corrected distance visual acuity (CDVA), and time spent obtained with the different refraction methods: noncycloplegic subjective, cycloplegic subjective, noncycloplegic automated, and cycloplegic automated.
The statistical comparison between the different refraction methods was done with the one-way ANOVA for related samples (pairwise comparison with Bonferroni correction). *p < 0.05.
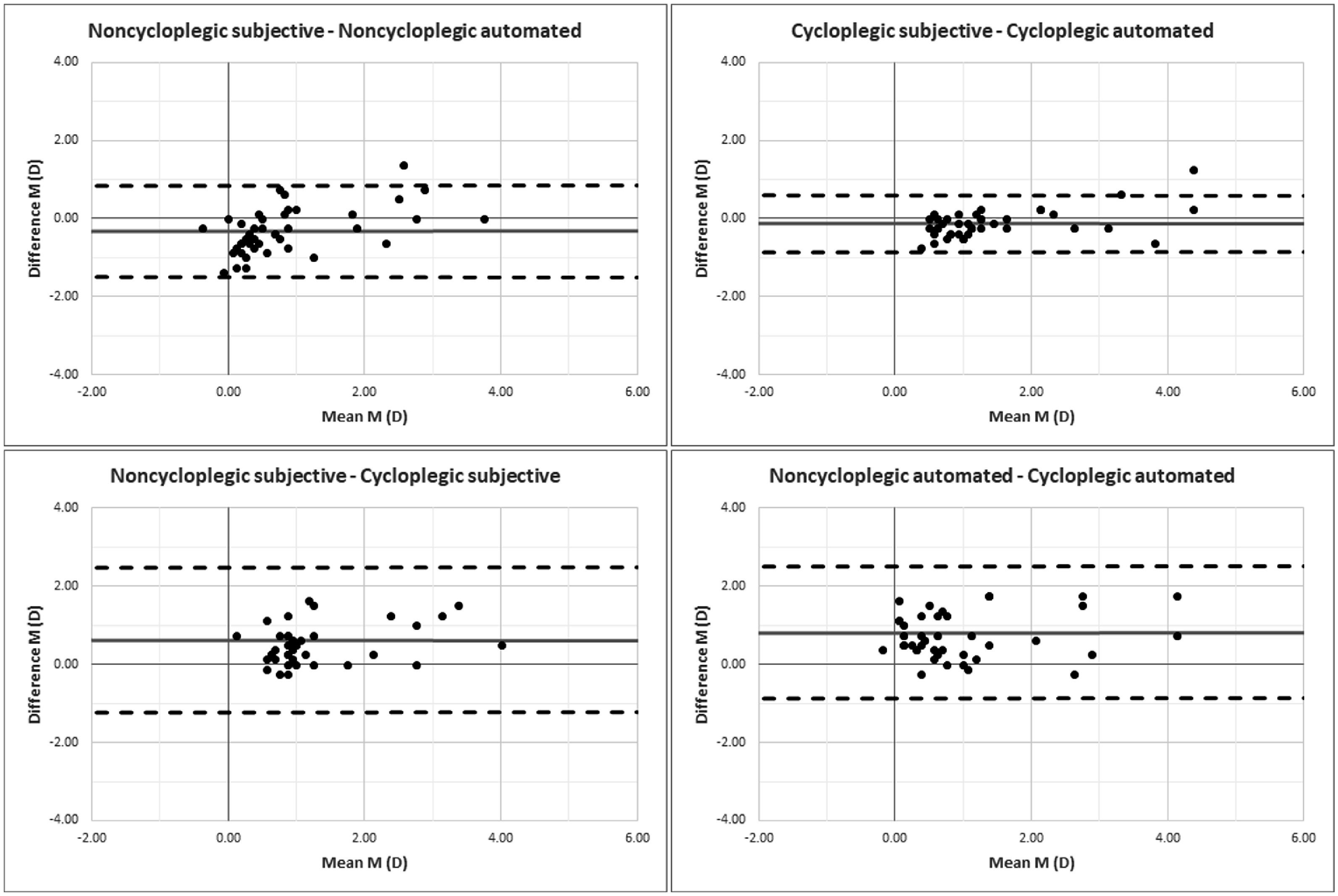
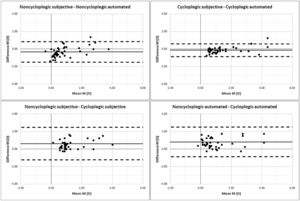
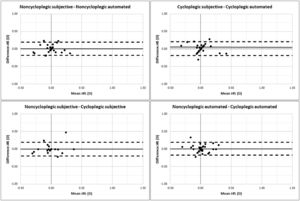
Concerning M, the Bland-Altman plots are shown in Fig. 2. Without cycloplegia, the automated refraction showed significant lower values of hyperopia than the subjective refraction (p = 0.009), the mean difference and its 95% limits of agreement (upper, lower) being −0.31 (+0.85, −1.47) D. Conversely, there were no statistically significant differences between both refraction methods under cycloplegic conditions (p ≥ 0.05). On the other hand, both refraction methods also presented higher levels of hyperopia with cycloplegia than without cycloplegia (p < 0.001), the mean difference and 95% limits of agreement being +0.63 (+2.48, −1.22) D for the subjective refraction and +0.82 (+2.52, −0.87) D for the automated refraction.
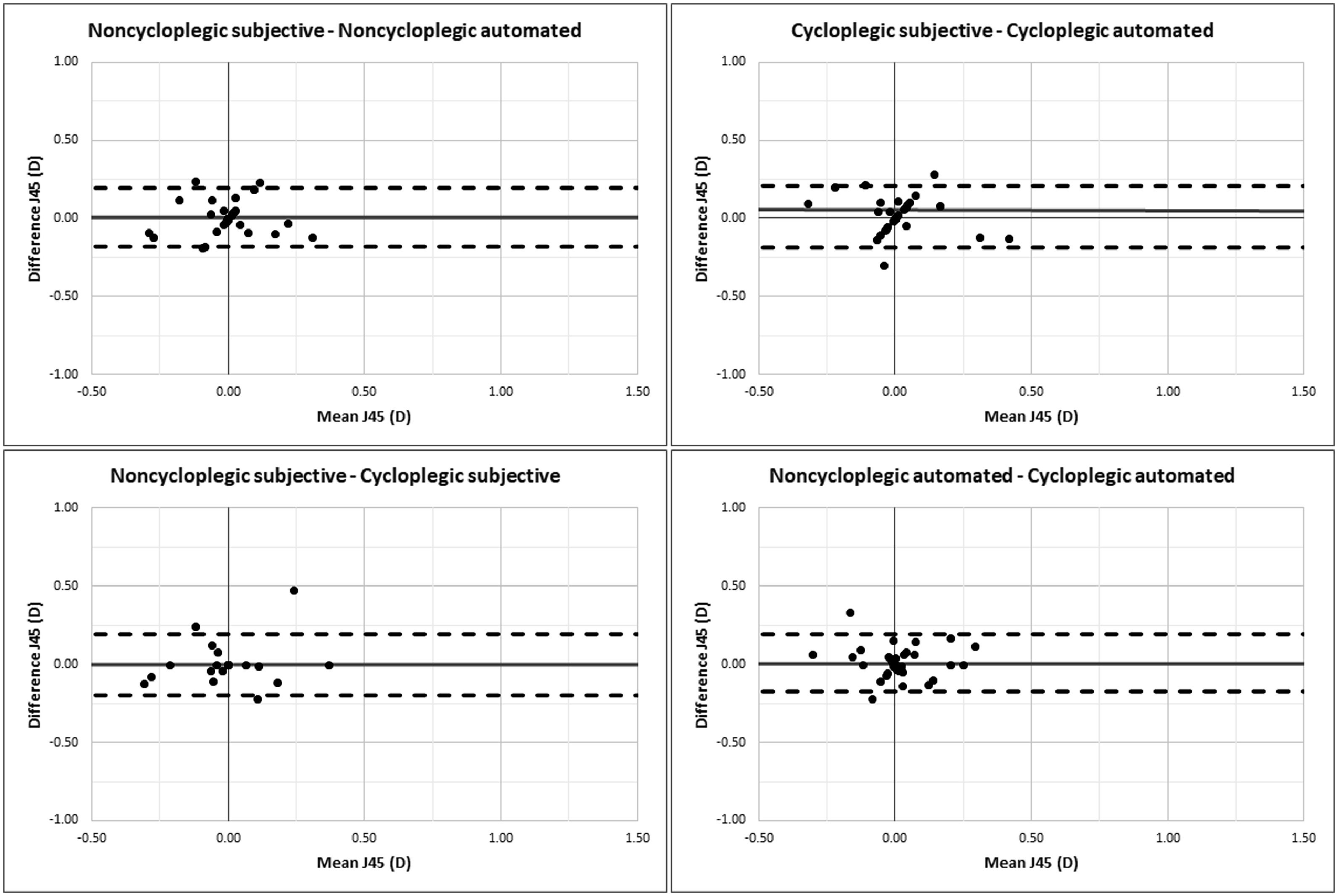
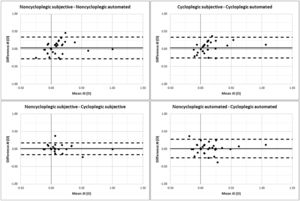
The Bland-Altman plots for J0 and J45 are shown in Figs. 3 and 4, respectively. The subjective and automated refractions did not manifest statistically significant differences between them under noncycloplegic and cycloplegic conditions (p ≥ 0.05). Furthermore, with both refraction methods, the procedure without cycloplegia also presented similar results to the refraction with cycloplegia (p ≥ 0.05).
Regarding CDVA, the automated refraction showed a significant improvement of 0.04 ± 0.01 logMAR compared with the subjective refraction under noncycloplegic conditions (p = 0.01). Besides, in the case of the automated refraction, the procedure without cycloplegia provided a visual acuity of 0.05 ± 0.01 logMAR better than with cycloplegia (p = 0.001).
The time spent performing the automated refraction was 3:08 ± 0.22 min:s faster than the subjective refraction under noncycloplegic conditions (p < 0.001). Also, in the case of the subjective refraction, the procedure with cycloplegia was 2:00 ± 0.21 min:s faster than without cycloplegia (p < 0.001).
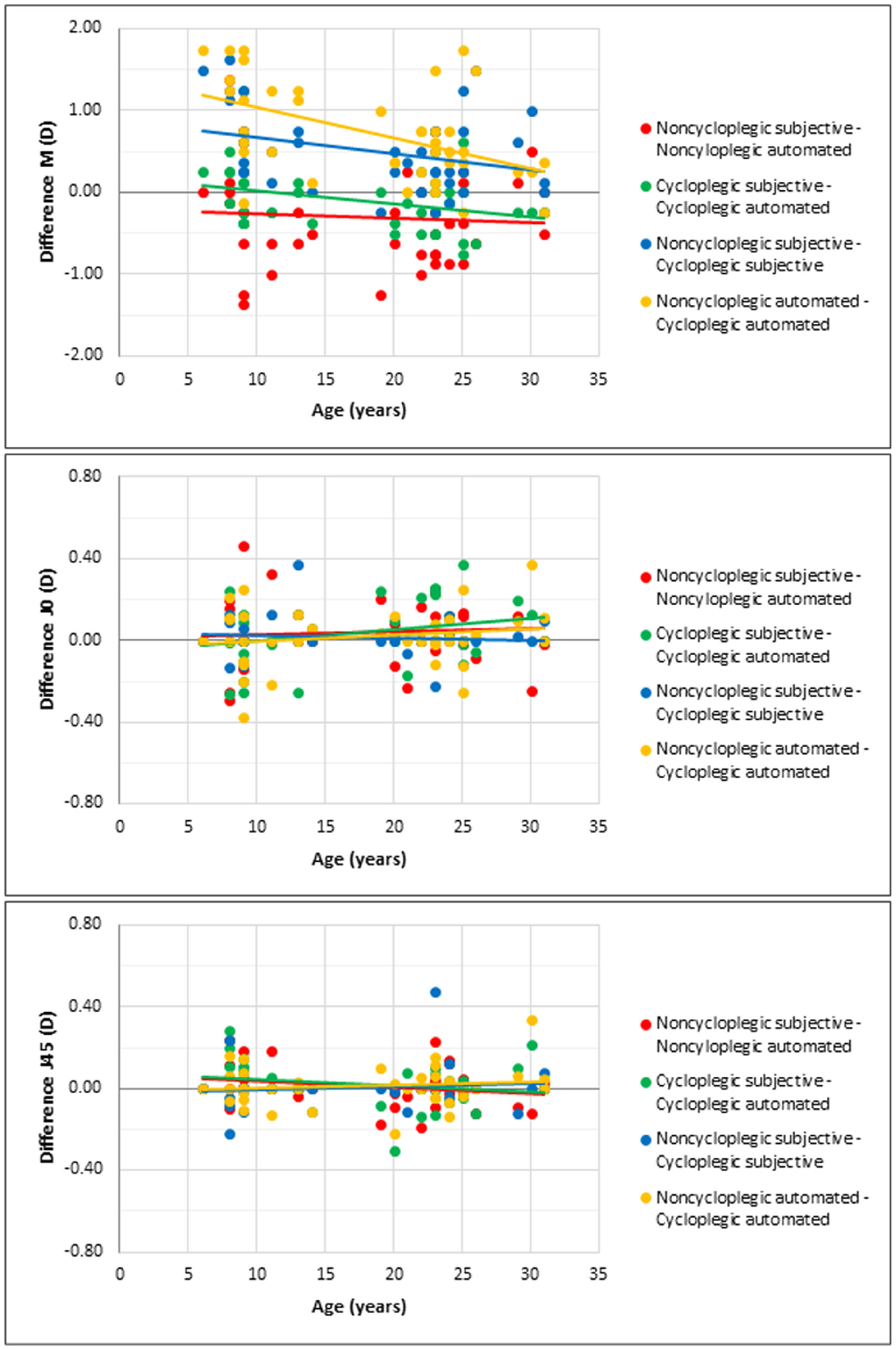
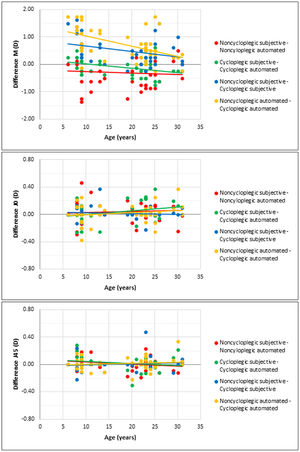
Finally, Fig. 5 shows the scatter plots and linear correlations between the age of participants and the mean difference between the refraction methods. M was the only variable that manifested statistically significant correlations (p < 0.05). With cycloplegia, the automated refraction weakly tended to overestimate hyperopia with age (r = −0.35, p = 0.024; red line) but did not under noncycloplegic conditions (r = −0.07, p = 0.670; green line). On the other hand, both refraction methods tended to reduce the difference between noncycloplegic and cycloplegic hyperopia with age, weakly with the subjective refraction (r = −0.32, p = 0.044; blue line), and moderately in the case of automated refraction (r = −0.49, p = 0.001; yellow line).
DiscussionTo our knowledge, this was the first study that assessed the efficacy in terms of accuracy and precision of an instrument to conduct automated subjective refraction, the Eye Refract, in a young hyperopic population. The interest in evaluating the impact of hyperopia on the refraction procedures lies in the possible presence of spasms and fluctuations in accommodation that could underestimate this refractive error.19 In this study, the underestimation of hyperopia occurred with both refraction methods under noncycloplegic conditions but affected the Eye Refract more, which could be associated with different factors discussed below.
Under noncycloplegic conditions, the automated refraction performed by the Eye Refract underestimated the spherical equivalent compared with the traditional subjective refraction. This underestimation was considered clinically relevant since was higher than 0.25 D, which is the minimum value that a clinician could change in the clinical practice. The fact that the Eye Refract tended to over-minus the spherical refraction could be associated with relative myopia induced by an instrument acting as an accommodative stimulus. In agreement with this hypothesis, Ohlendorf et al.23 found that both manual and digital phoropters induced more negative spherical error than the trial frame when conducting subjective refraction. However, unlike the current study, they did not perform retinoscopy as a starting point to facilitate subjective refraction, the reason why their findings should not be directly extrapolated to ours. Another reason for the difference between both refraction methods without cycloplegia could be their inter-session and inter-evaluator variability,15,24,25 considering that only one refraction by a different optometrist was conducted with each method. On the other hand, it should be highlighted that both refraction methods underestimated hyperopia without cycloplegia, but there were no differences between them under cycloplegic conditions. This would manifest the importance of paralyzing the ciliary muscle to obtain accurate and precise refraction in young hyperopes and children not only with the Eye Refract but also with the traditional subjective or objective procedures, as scientific evidence supports.18 Concerning the influence of age in the measurement of spherical refraction, it should be highlighted that the Eye Refract weakly tended to overestimate hyperopia with age, but only under cycloplegia. Besides, both refraction methods (Eye Refract and traditional subjective refraction) tended to be more accurate with age, which is logical considering that accommodative function is reduced over time.
In terms of spherical equivalent, a refraction method would be considered accurate if presents no statistical differences from the gold standard (the traditional subjective refraction) and precise if its 95% limits of agreement are between ±0.50 D.26 In this regard, the Eye Refract accurately estimated hyperopia under cycloplegic conditions only, while its 95% limits of agreement were more than twice the ideal range without cycloplegia (±1.16 D) but improved to ±0.72 D with cycloplegia. In two previous studies of our research group under noncycloplegic conditions,12,14 the 95% limits of agreement of the Eye Refract for a healthy general population were lower (±0.90 D) than in the current study, worsening in keratoconus patients to ±1.70 D without intracorneal ring segments and to ±4.50 D with these segments. However, in both studies, the Eye Refract showed no statistical differences compared with the traditional subjective refraction. The protocol for subjective refraction of these two studies was similar to the current study, except that, in keratoconus patients, retinoscopy was not performed due to their refractive irregularity.
For a direct comparison of the spherical equivalent with other systems of automated subjective refraction, it should be noted that all the studies found in the scientific literature were carried out in a general myopic and hyperopic population under noncycloplegic conditions. With the first instrument of the market to conduct subjective automated refraction, the BV-1000 (Topcon; Tokyo, Japan), Dave and Fukuma8 reported no differences in the spherical equivalent compared with the traditional subjective refraction, while Sheedy et al.9 found an overestimation of myopia of around 0.25 D, which agrees with the current study. Other recent instruments to perform subjective automated refraction neither manifested statistical differences from the traditional subjective refraction.10,11,13 Furthermore, all the previously referenced studies that evaluated the precision of these systems reached 95% limits of agreement between ±0.57 D and ±0.80 D, values slightly better than those obtained by the Eye Refract in a healthy general population12 and the young hyperopes of this study.
An accurate, precise, and repeatable objective refraction with the Eye Refract is crucial to obtain an accurate subjective adjustment since the automatic algorithm only includes a few limited questions to determine both sphere and cylinder (see Fig. 1). The binocular open-field aberrometer incorporated in the Eye Refract demonstrated better accuracy, precision, and repeatability than a monocular closed-field aberrometer.7 However, the binocular open-field design would not be enough to avoid the instrument-induced accommodation that underestimated hyperopia in this young population, the use of cycloplegia being necessary. In this regard, an open question is whether the Eye Refract would have the same efficacy with other cycloplegic drugs such as tropicamide or under a different posology.19,27
Concerning astigmatism, the Eye Refract presented good accuracy to determine J0 and J45 since did not show significant differences from the traditional subjective refraction under noncycloplegic and cycloplegic conditions. This manifests that paralyzing the accommodation would not be necessary to determine astigmatism in these young hyperopes. Furthermore, the Eye Refract was equally precise to determine astigmatism with or without cycloplegia, showing 95% limits of agreement under ±0.50 D for J0 and ±0.25 D for J45, similar to those obtained by our research group in a healthy general population.12 In agreement with these findings, other authors found no differences in terms of J0 and J45 between other instruments to conduct automated subjective refraction and the traditional subjective refraction as the gold standard, also presenting similar 95% limits of agreement.8,13 A recent study by Lara-Lacárcel et al.28 described how instrumental accommodation could induce changes in astigmatism power and its axis. They reported mean changes in J0 by about −0.02 D per dioptre of accommodation and minimal changes in J45. In the current study, there were no significant differences in terms of J0 and J45 between the subjective refraction and the Eye Refract under noncycloplegic conditions. Thus, the mean 0.31 D of accommodation induced by the Eye Refract compared with the traditional subjective refraction would not be enough to manifest significant changes in astigmatism.
In relation to CDVA, the statistical improvement found with the Eye Refract under noncycloplegic conditions was not clinically relevant, considering a visual acuity equal to or higher than 0.10 logMAR (one line) to be relevant. In this regard, only seven participants presented a CDVA with the Eye Refract equal to or higher than 0.10 logMAR compared with the traditional subjective refraction. This could be associated with the inter-evaluator variability between the two different optometrists who measured this variable, one with the Eye Refract and another with the traditional procedure. In a healthy general population, only the previous study of our research group evaluated CDVA by automated subjective refraction, reporting no differences between the Eye Refract and the traditional subjective refraction.12
The main advantage of automated subjective refraction is saving time in clinical practice due to autorefraction and subjective adjustment being incorporated into a single instrument, allowing the automation of all refraction steps.12-14 On the other hand, the Eye Refract presents some limitations such as considering a single sphere adjustment, but not a second one immediately after the cylinder. In addition, the final axis is determined by the initial aberrometry and cannot be modified during the refraction procedure guided by the algorithm. However, at the end of the refractive procedure, the evaluator can manually modify the final refraction following its clinical criteria.
One of the main limitations of this study was that only cyclopentolate was used to paralyze the ciliary muscle, the reason why the results should be extrapolated with caution to other cycloplegic drugs or posology. Furthermore, the traditional subjective refraction was performed by a single optometrist, not considering the inter-evaluator variability that these young hyperopes could show. It should be also considered that the traditional subjective refraction was conducted with a trial frame. Thus, the impact that subjective refraction through phoropter could have on this sample remains unknown, considering also the lack of scientific evidence about this question.
In conclusion, the Eye Refract underestimated hyperopia compared with the traditional subjective refraction without cycloplegia but showed similar results under cycloplegic conditions. Therefore, the Eye Refract is presented as a useful instrument to determine the refractive error in young hyperopes, the use of cycloplegia being necessary to obtain accurate and precise spherical refraction.
The authors want to thank Luneau Technology for providing the Eye Refract during the conduct of the study.