The association between ophthalmic anomalies and headache still needs to be investigated largely. We aimed to look for it in the context of a rural community hospital of Nepal.
MethodsHundred patients with headache were investigated for ophthalmic anomalies after the probable systemic association was ruled out. All the patients were first examined by general physician, otorhinolaryngologist and psychiatrist. Ocular evaluation consisted of detailed refractive, binocularity assessment and anterior and posterior segment examination. Data were analyzed using t-test, chi-square test, multiple logistic regression, odds ratio as well as frequency and percentages.
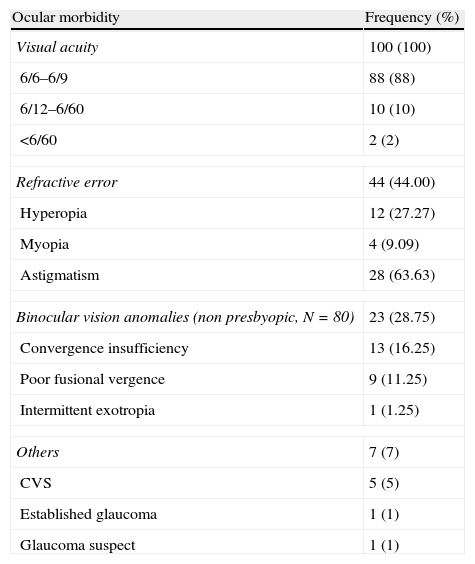
ResultsFemale above the age of 17 suffered more (p<0.05). Frontal headache was more common than occipital (p>0.05). In students and housewives frontal headache was more common (OR 3.467, 0.848–14.174; 95% CI and 1.167, 0.303–4.499; 95% CI). Refractive error was associated with frontal headache (OR, 1.429, 1.130–0.806, 95% CI). On presentation, 88% had visual acuity 6/9 or better. Forty-four percent had refractive error among whom astigmatism was more frequent (63.63%) followed by hyperopia (27.27%) and myopia (9.09%). Known eye problems were significantly associated with refractive error and binocular vision anomalies (p<0.001). Convergence insufficiency (16.25%) and fusional vergence (11.25%) deficiencies were common among unstable binocularity.
ConclusionOcular anomalies co-exist with headache complains very frequently. Refractive and binocular vision anomalies need to be largely investigated in all headache patients. It is important to get a good headache history so that patients can be referred to the appropriate specialist.
La asociación entre anomalías oftálmicas y cefalea todavía debe investigarse a fondo. Nuestro objetivo fue examinarlo en el contexto de un hospital de una comunidad rural de Nepal.
MétodosSe examinaron cien pacientes con cefalea en busca de anomalías oftálmicas una vez descartada una posible asociación sistémica. Todos los pacientes fueron explorados por un médico general, un otorrinolaringólogo y un psiquiatra. La evaluación ocular consistió en un examen detallado refractivo de la binocularidad y un examen del segmento anterior y posterior. Los datos se analizaron utilizando la prueba de la t, la prueba de la χ2 al cuadrado, regresión logística múltiple, razón de probabilidades, así como frecuencia y porcentajes.
ResultadosLas mujeres mayores de 17 años sufrieron más (p<0,05). La cefalea frontal fue más frecuente que la occipital (p>0,05). En estudiantes y amas de casa fue más frecuente la cefalea frontal (OR 3,467, 0,848 - 14,174; IC del 95% y 1,167, 0,303 - 4,499; IC del 95%). El error de refracción se asoció con cefalea frontal (OR, 1,429, 1,130-0,806, IC del 95%). En la presentación, el 88% tenían una agudeza visual de 6/9 o mejor. Un 40% presentaron errores de refracción, entre los cuales el más frecuente fue astigmatismo (63,63%), hipermetropía (27,27%) y miopía (9,09%). Los problemas oculares conocidos se asociaron de manera significativa con error de refracción y anomalías de visión binocular (p<0,001). La insuficiencia de convergencia (16,25%) y los déficits de vergencia fusional (11,25%) fueron frecuentes en la visión binocular inestable.
ConclusiónLas anomalías oculares coexisten muy frecuentemente con casos de cefalea. Las anomalías de refracción y de visión binocular deben investigarse a fondo en todos los pacientes con cefalea. Es importante obtener buenos antecedentes de cefalea para poder remitir a los pacientes al especialista adecuado.
Headache has been defined as the pain located above orbitomeatal line.1 It is one of the frequent reasons to seek a consultation with health care practitioners.2 It is a difficult condition to establish the actual cause. Diagnosis and treatment is often an impossible task without the correct views of etiology.3
Primary headache (headache without underlying disorders) prevalence varies with age, 9–11% in school children.4 The preponderance of headache is higher in female. In more than 80% patients, headache starts before age 40 with a lower prevalence rate at an advanced age (>50 years).5 Similarly, highly conflicting prevalence has been observed in different countries as 21.2% in the US,6 96% in Denmark,7 and past-year prevalence ranges from 13.4% in the US,6 to 87.3% in Canada.8
The evidence in the literature for a strong association between oculo-visual problems and headache is weak.2 Still patients who believe that appropriate ocular examination and treatment help to lessen their headache visit optometrists’ and ophthalmologists’ very frequently.8,9 Headache being one of the most common neurological symptoms has often been associated with Parkinson's disease, multiple sclerosis and myasthenia gravis. Nishimoto et al. revealed that in headache associated with myasthenia gravis, mild ocular symptoms are associated which range from slight degree of diplopia or ptosis which fluctuates dynamically and might lead to the worsening of headache.10 Harle and Evans report that in migraine headache often binocular vision anomalies in the form of decompensated heterophoria and reduced stereopsis might be present in subtle form.2
Ophthalmological studies on headache have reported the role of different ocular diseases like acute glaucoma, uveitis, optic neuritis11 and visual anomalies like refractive errors and accommodative and vergence deficiencies.12 The uncorrected refractive errors are often believed to be associated with frontal and/or occipital headache.13 Eye strain as a direct cause of headache has long been debated.14,15 Very frequently a careful eye examination and a possible correction of the defect has been observed to reduce headache symptoms.1 Thomas et al. noted that 21% of people with headache consult an eye care practitioner which is almost similar to those (27%) who seek a consultation with a general medical practitioner.9 Whittington reported that among more than 1400 consecutive patients attending for refraction, 45% complained of headache.16
Patients who fail Sheard's criterion (Prism Fusional Vergence less than twice the near phoria) are expected to suffer from headache symptoms.17 In 1966, Gordon et al.18 claimed that minor refractive error (RE) often caused more headache and symptoms of eyestrain than major RE. Ciliary muscle strain has also been suggested as possible source of headache.19 To the authors’ knowledge, there has not been any reports on exploring the ophthalmic share of headache symptoms among the Nepalese people who present to a general hospital.
The aim of this study was to investigate whether reported headache complaints of patients attending the general ophthalmic clinic are associated with ophthalmic anomalies.
MethodsPatientsThis study has a descriptive cross-sectional design. It was conducted in the Ophthalmology Department of Dhulikhel Hospital over a period of three months from March 2010. The hospital covers the rural population of approximately 1.9 million people from Kavrepalanchowk, Sindhu-palchowk, Dolakha, Sindhuli, Ramechhap, Bhaktapur and other surrounding districts. Hospital targets mainly the people with low socio-economic status who do not have access to the well facilitated health care services. It has provided services to 50 out of 75 districts of the country so far.20
We included only the patients with headache who were referred from the medical, otorhinolaringology (ENT) or psychiatry Out Patient Department (OPD). The diagnosis of primary headache was based on International Classification of Headache Disorders: 2nd edition (ICHD-II), based on physical and neurological examinations and head CT and/or MRI. Criteria for eye consultation were set as follows: all the patients needed to undergo thorough systemic evaluation with appropriate tests carried out. The appropriate investigation was ordered by the respective departments. The patients without definite diagnosis were then referred for eye examination. Only the patients with headache of more than three months duration were included in the study.
Each alternate patient complaining of headache (irrespective of nature/location/intensity) was included in the study with unrestricted random sampling method regardless of age, sex and referral. Alternate patients were chosen because it gave a plenty of time for the examination to be carried out in each patient in detail. Blood pressure was measured in each patient to look for undiagnosed hypertension. None of the patients had undiagnosed hypertension. Patients with other diagnosed systemic diseases such as migraine, sinusitis, and dental caries or women with menstrual migraine and/or women taking oral contraceptive pills were excluded from the study. Age groups of the patients were categorized as school children (<17 years), non-presbyopic adults (<40 years) and presbyopic adults (>40 years). This research was approved by the institutional research committee of Dhulikhel Hospital. The tenets of the Helsinki declaration were followed. Full informed consent was obtained and participants were able to abstain or withdraw from the research at any time without having to give a reason. No participants withdrew after they had arrived at the clinic. It was ensured that the clinician was masked about the identity of the patients with headache participating in the study and those excluded from the study, so that all the tests would be performed with equal emphasis to every patient.
AssessmentsHeadache questionnairesThe first part of the evaluation consisted of a structured interview conducted by one of the medical interns and utilizing a headache questionnaire. The questionnaires were based on an article “How to take a history of head or facial pain” by Blau.21 The questionnaires surveyed demographic data (e.g. sex, age, and occupation), headache occurrence and characteristics, headache onset and timetable (categorized into morning, afternoon, evening, during the night, or none) and pain topography (categorized into back, front, left sided, right sided or diffuse). The presence or absence of accompanying symptoms (nausea, vomiting, photophobia, phonophobia) and visual aura were assayed, as were treatment patterns (non-pharmacological measures or medications or spectacles), the presence or absence of aggravating factors (including physical or visual effort), family history, history of trauma, dental caries, sinusitis, menstrual disturbances and oral contraceptive pills intake in females.
Patients were asked to estimate the average number of hours spent daily in visually straining tasks (e.g., reading, watching television, and working with a computer) and whether headaches accompanied those tasks.
Visual acuity assessmentPresenting visual acuity was measured for each eye and for both eyes together at distance (6m) with internally illuminated Snellen's Chart. Near vision was recorded at a distance of 33cm with good illumination with reduced Snellen's Chart.
Refractive assessmentRetinoscopy was done with a retinoscope at the working distance of 50cm estimating refractive status of patients objectively, which was followed by subjective refraction in which the patient's response to the corrective lenses was assessed. Patients with dissimilar objective and subjective findings, fluctuating refractive status, below 15 years of age, and patients with binocular vision anomalies (BVA) underwent cycloplegic retinoscopy (1% cyclopentolate). In these patients subjective refraction was done after three days, when the cycloplegia effect dissapeared completely. Spherical and astigmatic deviations were measured to the nearest 0.50 D. Astigmatic axes were measured to the nearest five degrees, negative cylinders being used for all measurements. The degree of ametropia was stated as follows: patients with Spherical Equivalent Refractive Error (SERE) of −0.25 and +0.25 Dioptres (D) were considered as emmetropic, SERE>+0.50 D was considered as hyperopia and SERE>−0.50 D was considered as myopia. Astigmatism was defined as the cylindrical component of the refractive error more than 0.50 D. All examinations were carried out by the single observer (optometrist), who did not know the results of the headache questionnaire.
Binocular Vision Assessment (BVA)Cover test was performed at a distance of 6m and 40cm with an opaque occluder. A small non-accommodative target was used to control accommodation. The type and direction of heterophoria or heterotropia were recorded. Ocular motor functions were evaluated in six cardinal gazes. The Near Point of Convergence (NPC, which is the nearest distance from the eyes to which eyes can converge without experiencing diplopia or subjective discomfort) was assessed with a Royal Air Force (RAF) rule (an instrument used to measure NPC and accommodative amplitude). Amplitude of Accommodation (AA, it is the difference in the focus power of the eye while fixating from near to far) was measured in each eye separately and binocularly later with push up method. The first sustained blur was then noted (the carrier of the RAF rule which contains N series letter target is moved toward the patient resting the rule pad on cheeks. The patient is asked to state when letters become blurred; the first sustained blur is noted as the dioptric distance from the eye.).
Binocular Vision Assessment (BVA) except cover test was not carried out on presbyopes because they are assumed to demonstrate vergence dysfunction due to loss of accommodative convergence. Fusional reserves were measured with a vertical bar prism using an accommodative target. Distance divergent (base-in) followed by convergent (base-out) reserves were recorded as three values, the blur point, the break point, and the recovery point. Near base-in and base-out fusional reserves were recorded in the same way. Heterophoria was measured first, followed by divergence amplitudes and then convergence amplitudes so that each test did not have effect on other.
Other examinationsSlit lamp bimicroscopy and detailed fundus examination were carried out to rule out ocular pathology. Intraocular pressure was measured with Goldmann tonometer on all the patients. Patients whose diagnosis remained inconclusive on eye examination were referred to other departments such as medical, ENT or psychiatry as required and elicited by headache history for further investigation.1
Data analysisFor data analysis we included only the right eye in every patient when there were two readings for two eyes because findings in both the eyes of same individual are generally likely to be similar.22 Statistical analysis was done by calculating t-test to compare the means of two groups, chi-square test for non parametric data, multiple logistic regression to explore relationship between headache and occupation, odds ratio to explore risk of headache site with refractive and binocularity status as well as frequency and percentage to estimate the prevalence. Statistical software ‘Statistical Package for Social Sciences, version-11.5’ was used to analyze data. Statistical significance was set at p<0.05.
ResultsStudy populationA total of 100 patients with headache complaints participated in the study. Non-participation was due to severe headache while presenting to the OPD. Few patients were excluded because of the systemic diseases under investigation and which required simultaneous ocular consultation (like Hypertension, raised intracranial pressure, pregnancy induced migraine, suspected sinusitis, menstrual disturbances). Female gender predominated in the study (63%).
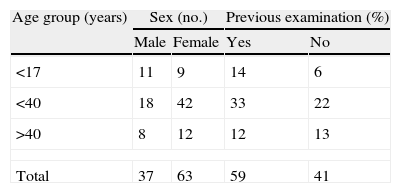
Age distribution and previous eye examinationMost of the headache complaints were in non presbyopic adults with females’ outnumbering males in each age category, except for school children (Table 1). Fifty-nine percent of the patients had previous eye examination among which 41% had ocular morbidities. Twenty-four patients (24%) had previous eye examination within six months. The female preponderance is not significant for the age below 17 years (χ22=5.538, p=0.063) but it is highly significant for age above 17 years (p=0.026).
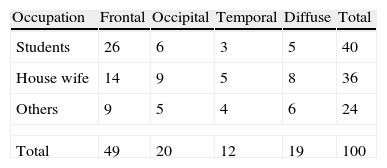
Profile of headacheIn 35% people headache lasted for one year. Some complained of long standing headache of more than one year even lasting up to nine years (one patient). The pattern of headache site with the occupation is presented in Table 2.
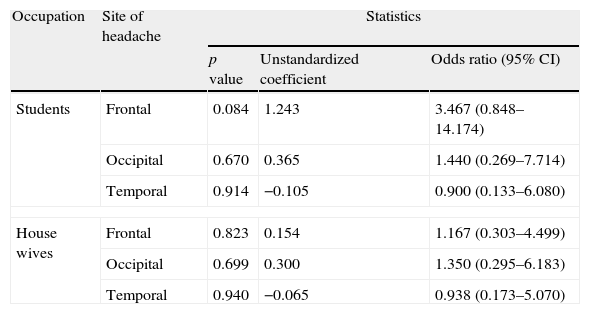
In multiple logistic regressions, we observed that the frontal and occipital headache is relatively determinant for both students and housewives (Table 3). It is seen that the unstructured odds ratio was significant with the occupations and site of headache but the p value is more than 0.05.
Relation between occupation and site of headache (for most frequently observed values).
| Occupation | Site of headache | Statistics | ||
| p value | Unstandardized coefficient | Odds ratio (95% CI) | ||
| Students | Frontal | 0.084 | 1.243 | 3.467 (0.848–14.174) |
| Occipital | 0.670 | 0.365 | 1.440 (0.269–7.714) | |
| Temporal | 0.914 | −0.105 | 0.900 (0.133–6.080) | |
| House wives | Frontal | 0.823 | 0.154 | 1.167 (0.303–4.499) |
| Occipital | 0.699 | 0.300 | 1.350 (0.295–6.183) | |
| Temporal | 0.940 | −0.065 | 0.938 (0.173–5.070) | |
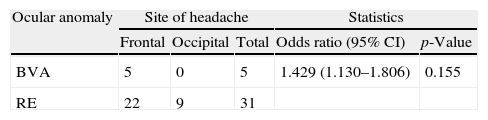
Previous eye examination was observed to be a risk factor both for refractive error; OR 1.213 (0.924–1.593, 95% CI) and binocular vision anomalies; OR 3.97 (0.111–1.417 in 95% CI). Six and seven patients each with RE complained of temporal and diffuse headache respectively. In four patients with BVA diffuse headache was present. Uncorrected RE was observed to be a risk factor for frontal headache (Table 4). None of the patients had BVA leading to occipital and temporal headache.
Statistical relation between oculo-visual anomaly and reported site of headache. The statistics includes Pearson χ2 tests and odds ratio with 95% confidence interval (CI).
| Ocular anomaly | Site of headache | Statistics | |||
| Frontal | Occipital | Total | Odds ratio (95% CI) | p-Value | |
| BVA | 5 | 0 | 5 | 1.429 (1.130–1.806) | 0.155 |
| RE | 22 | 9 | 31 | ||
BVA, binocular vision anomalies; RE, refractive error.
Most of the patients had normal to subnormal visual acuity (Table 5). Forty-four percent of the patients had refractive error. All of them were corrected with appropriate prescription which was evident through retinoscopy. Known eye problem was significantly associated with refractive error and BSV anomalies (χ12=11.225, p=0.001). Eight early presbyopes were prescribed the near vision glasses.
Summary table.
| Ocular morbidity | Frequency (%) |
| Visual acuity | 100 (100) |
| 6/6–6/9 | 88 (88) |
| 6/12–6/60 | 10 (10) |
| <6/60 | 2 (2) |
| Refractive error | 44 (44.00) |
| Hyperopia | 12 (27.27) |
| Myopia | 4 (9.09) |
| Astigmatism | 28 (63.63) |
| Binocular vision anomalies (non presbyopic, N=80) | 23 (28.75) |
| Convergence insufficiency | 13 (16.25) |
| Poor fusional vergence | 9 (11.25) |
| Intermittent exotropia | 1 (1.25) |
| Others | 7 (7) |
| CVS | 5 (5) |
| Established glaucoma | 1 (1) |
| Glaucoma suspect | 1 (1) |
Orthoptic examination was carried out on 80 non-presbyopic patients (Table 5). Seventy-one patients had orthophoria; eight had exophoria with good recovery. Fusional vergence satisfying Sheard's criteria was measured in 71(89%).
DiscussionThe prevalence of refractive errors (44%) in this group of this community was higher than that reported by different authors of other parts of the world. Cameron23 estimated a low prevalence of refractive error related headache in a sample of 50 patients referred for ocular examination and Jain et al.24 in an observational study conducted in India reported only 1.48% (of 202 patients) prevalence of refractive errors in headache patients. These discrepancies are from the patient enrolment. They have included every patient of headache without speciality consultation. We observed 28.75% patients with headache to have poor binocularity of which 16.25% (out of 80 non-presbyopic patients) had receded Near Point of Convergence. This prevalence of convergence insufficiency is less than that of Gupta et al.25 in India (49%), Romania26 (60.4%) and Patwardhan and Sharma27 (71.4%) in India. These discrepancies might be because of the different working environments of the patients. Gordon15 also cites poor binocular status as a potential source of headache. The literature also provides anecdotal support for the hypothesis that certain optometric anomalies, especially decompensated exophoria, may be prevalent in headache.28 A large number of patients with BSV anomalies in our study might be correlated to these observations. Although these data imply that Nepalese people from rural areas have more ocular problems leading to headache, the differing prevalence of these morbidities in different countries must be accounted for economical and psychological well being because these people might be exaggerating their headache symptoms. Moreover, these discrepancies could be because of the patient enrolment being very selective in our study where all the non ocular causes of headache were excluded. The higher proportion of people with previous eye examination in this study suggests that these people think that their eyes are culprit behind their headache. Our observations for the prevalence of headache in uncorrected refractive errors are in accordance with that of Gil-Gouveia and Martins.14
This study provides further evidence that headache is more common in female (p>0.001) similar to observation noted by Hendricks et al.29 We observed that every six patients out of ten have headache in the non-presbyopic adult group with females having more than two fold (2.33 fold) prevalence over male. Headache prevalence in this particular age group might be because of the psychological stress caused by educational pressures for career development, emotional factors and family conflicts. Female preponderance could be because of the culturally set factors and the effects of male dominated society which may lead to psychological stress.30 Prevalence rate of headache has been observed to increase at the age of 13, particularly among girls because of puberty.4 In our study, patients in the school age comprised of 20%. Headache in this age group could be because of home and school environment which puts pressure for better performance in the studies.
Some authors believe that spectacles for the correction of low degree of refractive errors is just a placebo15 while others claim it to be an effective method to ameliorate headache symptoms.29 Our results also suggest the claim that low degrees of refractive errors are associated with headache because 88% of these patients had been presenting visual acuity of 6/6 and 6/9. One hypothesis states that even the minor degree of astigmatic errors of refraction causes changes to visual perception that alter the hyper-excitability in the visual cortex of the brain of headache sufferers.30 Astigmatic blur may exacerbate the perception of striped patterns which are thought to be important in the visual triggers of different types of headaches.31 Another hypothesis could be the neurotic personality traits which mean that the patients with headache demand low degrees of refractive error correction.32,33 It is possible that refractive error could have an association with headache having no impact on the severity but the uncorrected refractive error exacerbates the headache symptoms.2 We have observed that the prevalence of astigmatism is higher than that of hyperopia and myopia (63.63%, 27.27% and 9.09%). Our study is in an agreement with that of Patwardhan and Sharma who claim the same trend in refractive error prevalence in headache patients.27
The prevalence of computer vision syndrome observed in our study (13%) is similar (9–12%) to that of the United States.28 The patho-physiology of headache associated with prolonged VDU use resides within the ocular surface abnormalities, accommodative spasms, dry eyes and/or extra-ocular etiologies.34
The first limitation of our study is that our patients were recruited from a hospital outpatient clinic population with a small sample size, so these results may not be representative of the general population as a whole. Second, we did not perform visual field testing as all the patients were first examined by different category of medical specialists which examine headache patients and all the possible non ocular causes were ruled out. Visual field testing has a core role in the differentiation of ocular and non ocular headache which needs to be included among the wide range of ophthalmic tests. Third, the inadequate patient masking is the probable reason to reveal high prevalence of ocular morbidity. Our strong point is the very selective patient enrolment. We have excluded every headache with known etiology.
In conclusion, this study provides the evidence that ocular morbidities and headache symptoms are linked very frequently. Thorough refractive evaluation and binocularity evaluation are important in headache. It is important to get a good headache history so that patient can be referred to the appropriate specialist for the management of headache and hence live a better quality of life.
Conflicts of interestsNone.
We would like to acknowledge Asst. Prof Dr Pankaj Pant; MD (General Medicine), Dr Bikash Shrestha; MD (ENT) and Dr Ajay Risal; MD (Psychiatry) for helping us in co-managing the patients. We would like to acknowledge Mr Roshan Kumar Mahato; Bachelor in Public Health, for helping us with statistical analysis.