Asthenopic symptoms associated with convergence insufficiency (CI) may compromise a person's ability to work or study. We investigated the effectiveness of orthoptic exercises in relieving symptoms related to CI and long-time results in adults and children.
MethodsThe data were retrospectively gathered from the patient clinical files. A total of 135 patients met the inclusion criteria of suffering asthenopic symptoms and CI but had not received prior strabismus surgery or orthoptic exercises.
ResultsThe mean age was 26±17 years, 74% of them were female. The patients (N=135) suffered from CI and had at least one of the following symptoms: eyestrain, blurring of vision, problems in reading and while doing work-up at close distance or headache. In the two-year follow-up time, 4% of the patients needed to be retreated and 3% of the patients required strabismus surgery. There were no significant differences between adults and children in near point of convergence (NPC), number of visits needed or fusional vergence at the end of treatment nor did the outcome depend on the number of visits. 59.5% of children vs. 51.9% of adults were free of symptoms when completing the exercises.
ConclusionsIn conclusion orthoptic exercises are effective in relieving asthenopic symptoms in adults and children. The effects of orthoptic exercises on NPC and fusional vergence were equal in adults and in children and not dependent on the number of visits needed for successful outcome. With orthoptic exercises it is possible to achieve longstanding relief on the symptoms of CI.
los síntomas astenópicos asociados con la insuficiencia de convergencia (IC) pueden comprometer la capacidad de trabajo o estudio de la persona. Estudiamos la eficacia de los ejercicios ortópticos en los síntomas de alivio en relación con la IC y los resultados a largo plazo en adultos y niños.
Métodosse reunieron datos retrospectivos de los archivos clínicos de los pacientes. En total 135 pacientes cumplieron los criterios de inclusión de presentar síntomas astenópicos e IC, pero no se habían sometido previamente a cirugía de estrabismo o ejercicios ortópticos.
Resultadosla media de edad eran 26±17 años y el 74% eran mujeres. Los pacientes (N=135) presentaban IC y tenían como mínimo uno de los síntomas siguientes: fatiga ocular, visión borrosa, problemas para leer o realizar tareas a corta distancia o cefalea. En el periodo de seguimiento de dos años, el 4% de los pacientes tuvieron que volver a recibir tratamiento y el 3% tuvieron que someterse a cirugía de estrabismo. No hubo diferencias significativas entre adultos y niños en cuanto al punto próximo de convergencia (PPC), el número de visitas o la vergencia fusional al final del tratamiento, y el resultado no dependió del número de visitas. El 59,5% de los niños frente al 51,9% de los adultos no presentaron síntomas al completar estos ejercicios.
Conclusioneslos ejercicios ortópticos son eficaces para aliviar los síntomas astenópicos en adultos y niños. Los efectos de los ejercicios en el PPC y la vergencia funcional fueron iguales en adultos y niños y no dependieron del número de visitas necesarias para obtener resultados existosos. Con los ejercicios ortópticos se puede obtener el alivio duradero de los síntomas de la IC.
Convergence insufficiency is a common reason for asthenopic symptoms, which usually manifest as blurred vision, diplopia, difficulties in performing close-up work, headache, eye pain, redness, and eyestrain. Asthenopic symptoms are very common: 46% of adults have been reported to experience asthenopia during or after working on a computer1 and 23% of schoolchildren have been reported to have asthenopic symptoms.2 Eye-related symptoms are the most frequently occurring health problems encountered in computer users3 and are in part, related to difficulties with accommodation or binocular vision problems such as convergence insufficiency that do not cause any symptoms when performing less demanding visual tasks.4,5
Asthenopia can de divided into two main groups: refractive asthenopia and muscular asthenopia. Asthenopia due to refractive errors can be alleviated with eyeglasses, which may also improve accommodation and asthenopia.6 Muscular asthenopia, which is associated with accommodative anomalies and convergence insufficiency, may be relieved in addition to proper refractive and prismatic correction by accommodative and convergence training.7 Recently, a new era of orthoptic treatment has dawned, with the publication of several randomized controlled trials on the effect of orthoptic exercises during the last few years.
The group of Scheiman and colleagues have investigated the effectiveness of treatments for symptomatic convergence insufficiency. In a randomized, controlled trial they found that office-based vision therapy was successful in about 75% of children aged 9–18 and was more effective than placebo treatment, pencil-push ups or home-based computer vergence/accommodative therapy for children with symptomatic convergence insufficiency.8 In young adults aged 19–30 years, 42% of subjects achieved statistically significant relief of their asthenopic symptoms with office-based vision therapy/orthoptics, 31% in office-based placebo vision therapy/orthoptics, and 20% in home-based pencil push-ups meeting predefined criteria for elimination of symptoms.9,10 Furthermore, in the study of Birnbaum et al.11, vision therapy was successful in 62% of adult male patients aged over 40 years who received in-office plus home therapy, whereas only 11% of the control group gained relief of asthenopic symptoms.
In the present study we wanted to evaluate the effectiveness of orthoptic exercises in relieving asthenopic symptoms in adults and children and also to follow-up the treatment effect. During recent decades, the demand for near-work has increased and this has increased asthenopic symptoms. When proven effective, one can predict that the orthoptic exercises will become popular, since they are easy, non-invasive and effective way of treating convergence insufficiency.
Patients and methodsThis study was a retrospective analysis of case records. The study population consisted of patients referred to orthoptic exercises in the University Central Hospital of Oulu, Oulu, Finland during years 2005 and 2006. The patients were eligible for inclusion into the study if they had asthenopic symptoms, such as problems in reading and while doing close-up work, had blurred vision or headache and had no prior history of strabismus surgery or had previously performed prior orthoptic exercises. Only patients with convergence insufficiency (defined as near point of convergence with RAF rule12 more than 6cm and a fusional vergence insufficiency with positive fusional vergence amplitude less than 20 degrees estimated with major amblyoscope) were included.13 Refractive errors were corrected for at least two to three months before initiating the exercises. The total number of patients was 289 and 135 patients met the inclusion/exclusion criteria.
Though the retrospective design of the current study, we examined patients carefully and standardized assessment procedure was used. The following parameters were recorded at each visit: symptoms (improved, no change, worsened), cover/uncover test for distance and near, near point of accomodation with RAF rule and the near point of convergence with fingertip and ruler. The presence of heterophoria/tropia and fusional vergence amplitude (degrees) was also determined with a major amblyoscope. At the first visit, the visual acuity, binocularity with the Worth four dot test and stereo tests were also recorded.
The orthoptic exercises were conducted as office-based convergence and divergence therapy combined with home training. The convergence exercises were pencil push-ups at the beginning and the patient was asked to maintain a single image of the fixation object as close to the nose as possible. If the convergence was normal at the beginning of exercises, the patients were not instructed to perform push-up exercises. Thereafter, the patient practised the adoption of physiological diplopia and finally, convergence could be performed involuntarily without the help of a pencil. Fusional vergence exercises included stereograms and the patient was asked to create a fused central image of two dissimilar pictures in the cards, finally also by altering their vergence. At each visit, home-exercises were given in order to maintain and strengthen the achieved results.
We collected the following information from the patient records of 135 patients: patient gender, age, diagnosis, best corrected visual acuity and refraction, asthenopic symptoms. The data concerning orthoptic exercises collected were: number and dates of visits, total follow-up time, duration and type of exercises.
Statistical analysis was done using the SPSS program version 16.0 (SPSS Inc., Chicago, IL, USA). The tests used were Kolmogorov–Smirnov and Shapiro–Wilks as well as t-test (independent samples t-test or pairwise t-test).
ResultsThe total number of patients was 135 and they were aged from 6 to 79, with mean age 26 years (SD 17.3). Seventy-four percent of them were female (N=100) and 26% were male (N=35). Most of them were teenagers or young adults, i.e. 67% of them were under 30 years of age and 38% were aged 10–20 years. The mean age of the children (under 18 years, N=66) was 12.4 years (range 6.6–17.6) and with adults (N=69) it was 38.7 years (range 18.4–79.7). The patients had made 1–28 visits to conduct orthoptic exercises with a mean of 6.5 visits (SD 4.7, median 5) at a mean interval of 21 days (SD 13.8). The average duration of performing the exercises was 123 days (SD 112 days). Sixty-seven patients (50%) had a minor degree of exophoria at the beginning of exercises and sixty (44%) had orthophoria.
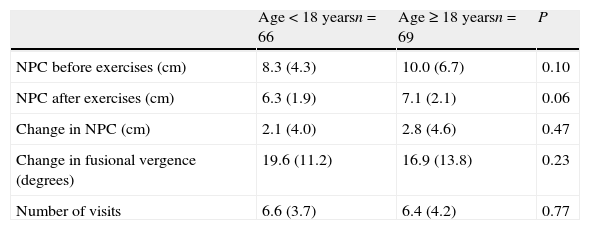
Asthenopia symptomsTable 1 shows the symptoms at the beginning of orthoptic exercises. Asthenopic symptoms, such as problems in reading and doing work at close-up, blurred vision or headache were inclusion criteria in this study.
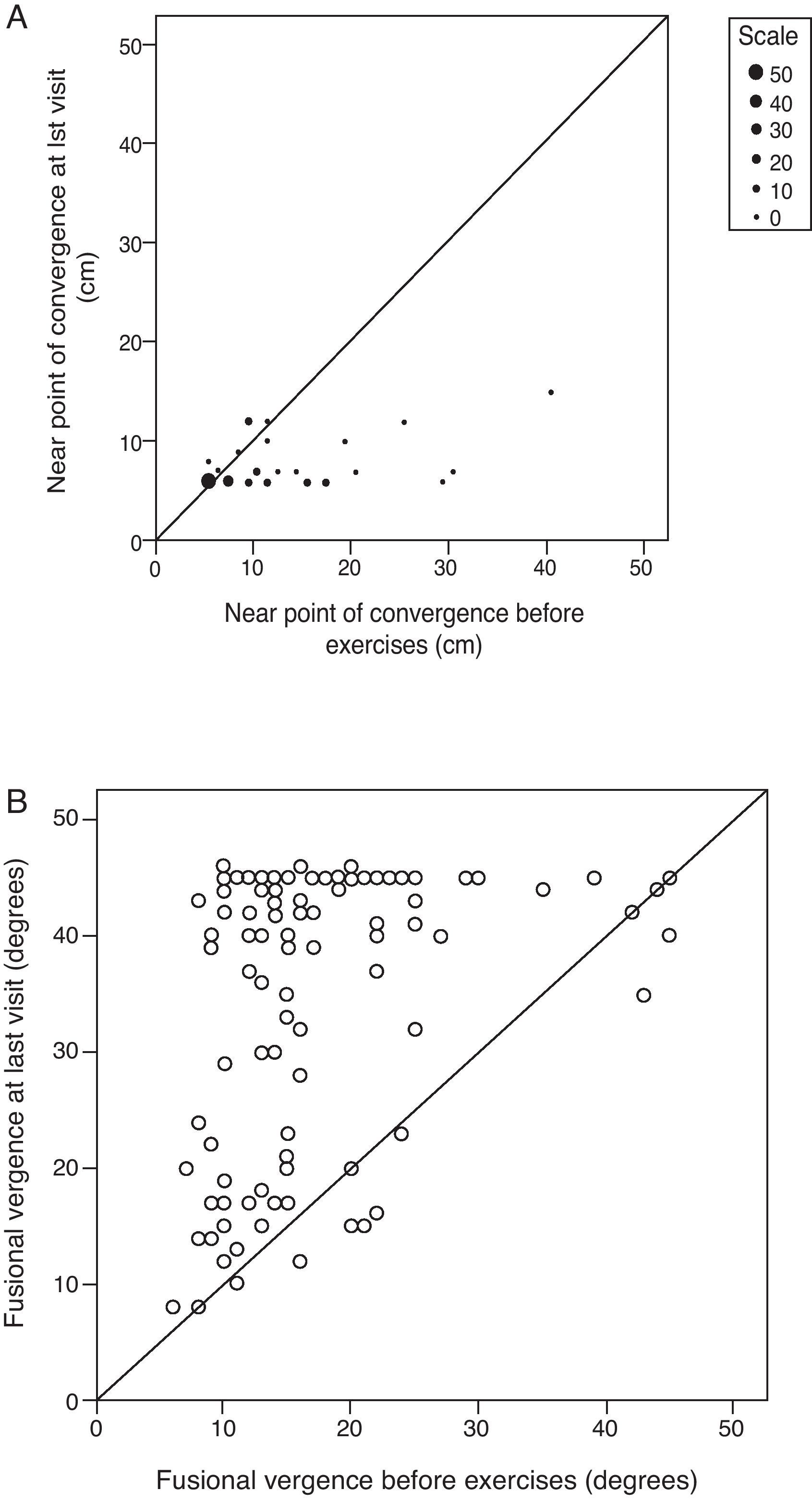
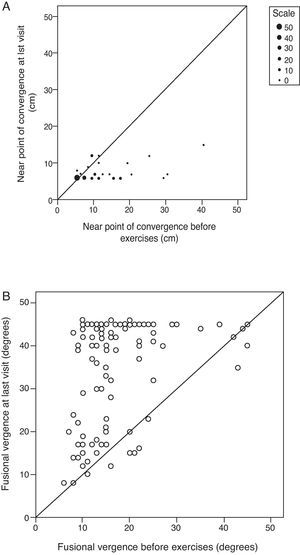
ConvergenceIn 60% of patients, the near point of convergence (NPC) was insufficient (range from 7 to 40cm) at the beginning of exercises. NPC improved in 37% of all patients (N=49) whereas in 38% (n=51) of patients NPC did not change. (Fig. 1A) However, majority of those patients whose convergence did not improve, had good convergence (6cm or less) already at the beginning of the exercises. In four percent of patients (N=5) NPC worsened during the exercises. The mean change in convergence was 2.6cm (SD 5.2cm). If the NPC was greater than 6cm before the exercises, the mean change in NPC was 5cm (SD 6.4cm) (N=56). The mean NPC improved significantly during the exercises (mean 10.2, SD 5.9 at the beginning vs. 6.7, SD 1.7 at the end of exercises, p<0.001).
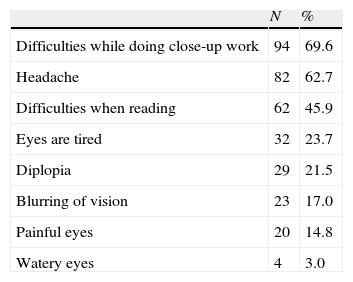
Fusional vergence amplitudeThe improvement of fusional vergence is shown in Fig. 1B. At the beginning of the exercises, the fusional vergence amplitude was poor (defined as 20 degrees or less) in 71.1% (n=96) of patients. The mean change in fusional vergence amplitude measured with the major amblyoscope was 18.6 (SD 12.2) degrees after the exercises.
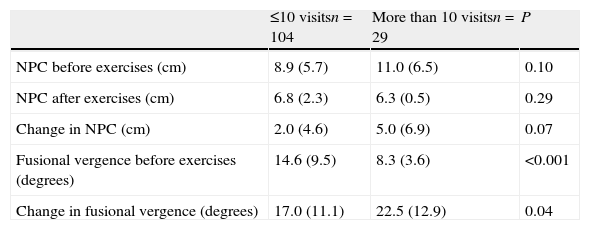
Measurements and number of visits in adults and in childrenThere were 66 children and adolescents aged under 18 and 29 adults (aged≥18) in the study. The adults and children responded to the exercises similarly, whether determined as change in near point of convergence (NPC), a change in fusional vergence and or in the number of visits in adults and in children (Table 2). There were no significant differences in these parameters between adults and children, however, there was a trend that children had better NPC at the end of exercises (p=0.06). 59.5% of children vs. 51.9% of adults were free of symptoms after they had completed the exercises. The number of visits needed for successive outcome varied considerably, but did not differ significantly between adults and children. The variation between patients having under or equal to 10 visits vs. patients having more than 10 visits is shown in Table 3. It seems that those individuals having more than 10 visits had marginally lower NPC and significantly worse positive fusion at the beginning of the exercises. However, at the end of exercises their NPC or fusional vergence did not differ significantly from the patients having maximum of 10 visits.
Near point of convergence (NPC), change in fusional vergence and number of visits in adults and in children. The data is shown as mean (SD).
| Age<18 yearsn=66 | Age≥18 yearsn=69 | P | |
| NPC before exercises (cm) | 8.3 (4.3) | 10.0 (6.7) | 0.10 |
| NPC after exercises (cm) | 6.3 (1.9) | 7.1 (2.1) | 0.06 |
| Change in NPC (cm) | 2.1 (4.0) | 2.8 (4.6) | 0.47 |
| Change in fusional vergence (degrees) | 19.6 (11.2) | 16.9 (13.8) | 0.23 |
| Number of visits | 6.6 (3.7) | 6.4 (4.2) | 0.77 |
Near point of convergence (NPC), change in fusional vergence and number of visits in patients having ≤ 10 visits or more than 10 visits. The data is shown as mean (SD).
| ≤10 visitsn=104 | More than 10 visitsn=29 | P | |
| NPC before exercises (cm) | 8.9 (5.7) | 11.0 (6.5) | 0.10 |
| NPC after exercises (cm) | 6.8 (2.3) | 6.3 (0.5) | 0.29 |
| Change in NPC (cm) | 2.0 (4.6) | 5.0 (6.9) | 0.07 |
| Fusional vergence before exercises (degrees) | 14.6 (9.5) | 8.3 (3.6) | <0.001 |
| Change in fusional vergence (degrees) | 17.0 (11.1) | 22.5 (12.9) | 0.04 |
The mean follow-up time was 2.3 years, and only 4% of them (N=5) needed to be treated again with orthoptic exercises and 3% (N=4) did undergo strabismus surgery during follow-up time. In addition, there were 2 patients who were both retreated with orthoptic exercises and finally, had undergone strabismus surgery.
DiscussionSeveral treatment modalities have been used in the treatment of convergence insufficiency, such as base-in prism glasses, reading glasses, pencil push-up therapy, home-based vision therapy/orthoptics, and office-based vision therapy/orthoptics.14 In the case of convergence insufficiency, in a study with 72 children aged 9–18 years base-in prism reading glasses were found to be no more effective in relieving symptoms than placebo reading glasses.15 Recently, the effect of office-based orthoptic exercises has been shown to be superior to placebo treatment, pencil-push ups or home-based computer vergence/accommodative therapy in the treatment of children with symptomatic convergence insufficiency.8 The current study aimed at evaluating the effect of orthoptic exercises in relieving asthenopic symptoms in adults and children and furthermore to investigate the long term treatment effect.
In present study we determined the success rate as absence of all symptoms and found that 59.5% of children vs. 51.9% of adults were free of symptoms after they had completed the exercises. This is in line with a study by Scheiman et al.9 having success rate of 42% and Scheiman et al.16 55.9% with office-based vision therapy/orthoptics. The success rates are also in concert with other previous studies such as study by Daum (1983) where the symptoms totally disappeared in 53% of patients and altogether 96% gained some relief of exercises17 and with a study Birnbaum et al.11 who observed a success rate of 61.9% in patients who gained in-office therapy with supplementary home therapy. Majority of the rest gain some relief on their symptoms. The orthoptic exercises are easy, non-surgical and cheap intervention on convergence insufficiency and this treatment has proved its efficacy. Nevertheless, there was considerable variability in number of visits needed for successive outcome in our present study and in patients with more than 10 visits this was mainly due to worse NPC and positive fusion vergence at the beginning of the exercises. However, at the end of exercises these patients did not differ significantly from those having less than or equal to 10 visits and they succeed as well as or even better than other subjects. It has been shown that by increasing the treatment time even beyond 12 weeks the proportion of patients being asymptomatic increases.16
Asthenopic symptoms are a common complaint not only in working-age people1 but also in schoolchildren6 and convergence insufficiency is a common reason for athenopic symptoms. One purpose of the current study was to determine whether all patients, children and adults, gain long-lasting relief of their asthenopic symptoms which are due to convergence insufficiency. During recent years, a growing body of evidence has accumulated that orthoptic exercises may be effective in certain, selected cases, such as convergence insufficiency and decompensating exophoria18 with several randomized controlled trials being published. The group of Scheiman and colleagues has evaluated the long-term effectiveness of treatments for symptomatic convergence insufficiency in children and in adults9,10 and reported that twelve weeks of office-based vergence/accomodative treatment resulted in a significantly greater improvement in symptoms and clinical measures compared to placebo treatment or home-based exercises.16 Furthermore, these children maintained their improvements for at least 1 year after discontinuing the treatment.8 In present study, those patients with successive outcome on symptoms, enjoyed a long-lasting effect. For most of the patients, the effect of exercises seemed to last for at least several years, since only 11 patients (8%) required surgery or needed to be treated again with orthoptic exercises or both during the follow-up time. This is a longer follow-up time than that in the study of Scheiman et al.8 However, there are no reports on the effect of symptoms of convergence insufficiency on quality of life or the cost-effectiveness of orthoptic exercises. If it is proven that the relief of symptoms impacts significantly on the quality of life the conclusion may be drawn that the orthoptic exercises are a highly effective form of treatment. However, this question will need to be resolved in a separate study since we did not collect such kind of data in our study.
Though there has been impressive research conducted on the effect of orthoptic exercises in children and adolescents,9,10 there are surprisingly few reports published on the impact of orthoptic exercises in adult patients.11 In previous studies of children undergoing treatment for convergence insufficiency, it has been noted that the rate of improvement is more rapid for clinical signs such as near point of convergence than for relief of symptoms.9 However, we did not find any differences between adults and children in NPC, fusional vergence or the number of visits needed to achieve the relief of symptoms. In our study, it seems that the effect of orthoptic exercises when determined as the rate of improvement does not seem to differ in adults from that what is known to occur in children/adolescents. Moreover, it has been also postulated that evidence of various non-surgical treatments such as orthoptic exercises are less effective among adults than children.13 However, we did not observe a difference between our adult patients and the children/adolescent patients and based on this evidence we propose that orthoptic exercises would be suitable for adults as well.
Two limitations of the present study are its retrospective design and the lack of controls. However, we applied strict selection criteria for the patients with respect to the exercises and the assessment procedure was standardized. The proportion of patients gaining relief for their symptoms in our study was similar to that reported in previous studies, such as that of Scheiman et al.9,15 The recently published randomized clinical trials provide excellent information on the effect of orthoptic exercises on children and adults. However, this study adds information since it compares the effect of orthoptic exercises in adults and children, concluding that there does not seem to be a difference on the effect of exercises on symptoms or NPC or in the number of visits needed for relief of symptoms.
In conclusion, it seems that orthoptic exercises are effective in relieving asthenopic symptoms in adults and children. The effects of orthoptic exercises on NPC and fusional vergence were equal in adults and in children and not depending on the number of visits needed for successive outcome. Furthermore, with othoptic exercises it is possible to achieve longstanding relief on the symptoms of convergence insufficiency.
Conflict of interestsThe authors have no commercial or financial interest involved in the development of their work.