To study the impact of the depth of focus on subjective refraction and distribution of myopic and hyperopic refractions.
MethodsA total of 450 eyes of 305 subjects in the age range of 23–34 years were recruited for the study. A distribution of refractions was examined using a traditional method of the subjective refractometry on the basis of point-like posterior focus notion. Correction of the results was made on the assumption that the emmetropic eye retains high visual acuity when applying convex lenses with values which are fewer or equal to the depth of focus values. The following values of the depth of focus were used: ±0.55D, ±0.35D and ±0.2D for visual acuity 1.0, 1.5 and 2.0, respectively.
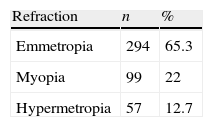
ResultsApplication of the traditional method of refractometry produced the following occurrence of refractions: hypermetropia 59.3%, myopia 22% and emmetropia 18.7%. After correction of the initial results of values of the depth of focus the distribution of refractions was as follows: hypermetropia 12.7%, myopia 22% and emmetropia 65.3%.
ConclusionThe traditional method of subjective refractometry with application of trial lenses was developed on the basis of data of large optical aberrations and significant depth of focus which values should be taken into account during interpretation of results of subjective refractometry. Our data regarding to prevalence of emmetropic refraction falls in line with basic science provisions in respect of the physiology of the eye.
Estudiar el efecto de la profundidad de foco en la refracción subjetiva y la distribución de los estados refractivos miópicos e hipermetrópicos.
MétodosPara el estudio se incluyeron 450 ojos de 305 sujetos con un intervalo de edad de 23 a 34 años. Se examinó la distribución de estados refractivos utilizando un método tradicional de refractometría subjetiva sobre la base de la noción de foco posterior en forma de puntos. La corrección de los resultados se realizó asumiendo que el ojo emétrope conserva una alta agudeza visual al aplicar lentes convexas con valores inferiores o equivalentes a los valores de profundidad de foco. Se utilizaron los valores de profundidad de foco siguientes: ±0,55 D, ±0,35 D y ±0,2 D para una agudeza visual de 1,0, 1,5 y 2,0 respectivamente.
ResultadosLa aplicación del método de refractometría tradicional produjo la incidencia de refracciones siguiente: hipermetropía 59,3%, miopía 22% y emetropía 18,7%. Tras la corrección de los primeros resultados de valores de profundidad de foco, la distribución de refracciones fue la siguiente: hipermetropía 12,7%, miopía 22% y emetropía 65,3%.
ConclusiónEl método tradicional de refractometría subjetiva con la aplicación de lentes de prueba se desarrolló basándose en datos de altas aberraciones ópticas y una profundidad de foco significativa, valores que deberían tenerse en cuenta a la hora de interpretar los resultados de refractometría subjetiva. Nuestros datos relativos a la prevalencia de refracción emétrope coinciden con las previsiones científicas básicas respecto a la fisiología del ojo.
A subjective method for verifying the type of refraction and degree of ametropia using trial lenses was initially formulated by C. Donders in the mid-nineteenth century. Presently, objective refraction has become increasingly automated; nevertheless, there is an even greater need for a high quality subjective examination. Subjective refraction remains a key element of an eye examination.1
Duke-Elder presented a thorough review of papers published from the late nineteenth to mid-twentieth centuries regarding the relative incidence of refraction.2 In subjective refractometry, hypermetropia occurred in over half of the population in the age range of 20–50 years.
The prevalence of hypermetropia gives the illusion that hypermetropia is the preferable refraction for visual performance; although the majority of authors think that emmetropia presents the optimal refraction.
It is important to note that the optical system of the schematic eye with a point-like posterior focus was the theoretical basis for developing the subjective method of refractometry.
A series of studies3–11 revealed conflicting data about depth of focus of the living human eye. The gained values of the depth-of-focus varied from ±0.02D4 to ±1.25D,5 however other authors obtained values of about ±0.3D for a pupil diameter of 3mm.3,6–9 According to our studies10,11 there is a relationship not only between the depth-of-focus and the pupil diameter, but also between the depth-of-focus and visual acuity. This relationship is basically conditioned by the influence of the optical aberrations on both the depth of focus and visual acuity. We have found the following values of the depth-of-focus ±0.55D, ±0.35D and ±0.2D for visual acuity 1.0, 1.5 and 2.0. The smaller the pupil size the larger are the depth of focus values. Under condition of the pupil diameter of 1.0mm the depth of focus is about 2.0D.6–8,10
The existence of the depth of focus motivates us to refine the traditional subjective method of refractometry.
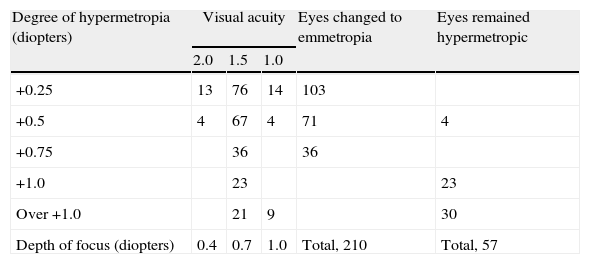
Depth of focus represents some distance along the optical axis and has at least three variant positions (Fig. 1): middle, posterior and anterior.
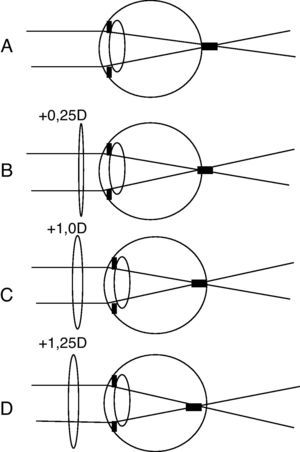
In the case of emmetropia and the posterior position of depth of focus, the addition of lens +0.25D shifts the focus forward; however, the quality of retinal image will remain the same (Fig. 2B). A stimulus for accommodative activity will not follow. It is important to note that the emmetropic eye attains normal vision without an accommodative response. Adding lenses with a higher power such as +0.5D, +0.75D or +1.0D, will not change the situation because the depth of focus for visual acuity 1.0 is 1.1D. Only the lens +1.25D impairs the retinal image and would trigger an accommodative reflex (Fig. 2C and D).
The described evidence leads to an important practical aspect related to the diagnostic distinction between emmetropia and hypermetropia. An emmetropic eye easily tolerates convex lenses with their optical power under a value of depth of focus without the help of accommodation. The degree of hypermetropia should be determined by the highest power convex lens (on assumption of subtraction of the depth of focus value) with which the eye attains optimal distant vision.
The purpose of this work was to study an impact of the depth of focus on subjective refraction and distribution of myopic and hyperopic refractive errors.
MethodsThe subjects for this study were selected from the serving military officers of armed forces, Kiev. The medical records of about 3000 military men were reviewed to find persons with visual acuity of at least 1.0 or higher. The visual acuity was examined in 940 subjects, and then 450 eyes of 305 persons in the age range of 23–34 years were enrolled in the study.
All participants were aware of the purpose of the investigation and gave verbal consent.
The inclusion criteria were normal levels of visual acuity, a natural pupil diameter between 3 and 5mm, no evidence of ocular diseases. The exclusion criteria were an astigmatism of ≥1.0D, irregular astigmatism, any opacity of the ocular media which could impact a visual performance.
All the investigations were performed in the same room with uniform artificial illumination of about 210lx. Visual acuity was tested at distance of 5m using Landolt's broken ring chart fixed in the standard box having the local luminance about 145cd/m2. The lower 3 lines of the chart relate to a visual acuity 1.0, 1.5 and 2.0. These lines content the Landolt's circles with a size of 7.3mm, 4.8mm and 3.6mm which at distance of 5m subtend 5min, 4.1min and 2.5min of arc, respectively.
A typical set of lenses was provided with spheres every quarter of a diopter to ±4.0D. Visual acuity scoring was performed if the subject correctly located Landolt's ring opening at least 5 times out of 7 attempts. The study was preceded by the preliminary screening examination of a significant group of young persons in order to find eyes achieving visual acuity 2.0.
The degree of ametropia was assessed in two ways.
- (1)
According to a traditional approach, the degree of hypermetropia was determined by the highest power convex lens and myopia by the lowest concave lens, which allowed the highest visual acuity to be reached: 1.0, 1.5 or 2.0. An eye was considered emmetropic if unaided visual acuity was at the highest level and adding a +0.25D lens impaired acuity.
- (2)
The data from hypermetropic eyes examined using the traditional method were corrected by a means of depth of focus. The degree of hypermetropia in an eye with visual acuity of 1.0, 1.5 or 2.0 was reduced at a depth of focus 1.0D, 0.7D and 0.4D, respectively. A difference between the degree of hypermetropia and depth of focus less than 0.1D was not taken into account.
According to the traditional method of subjective refractometry, the distribution of refractions obtained in this study is consistent with the results of previous studies (Table 1). Hypermetropia occurred in 59% of cases and emmetropia in much fewer cases (18.4%).
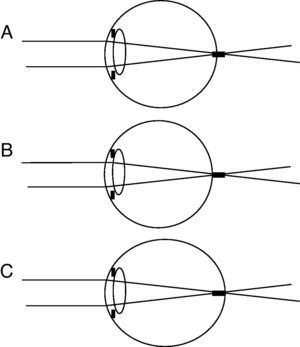
As noted above, according to our concept, the depth of focus does not impact the incidence of myopia. Results regarding the degrees of hypermetropia and visual acuity are presented in Table 2. The eyes with light degrees of hypermetropia, +0.25D or +0.5D, were prevalent in 105 and 75 cases, respectively.
Visual acuity and depth of focus of hyperopic eyes.
| Degree of hypermetropia (diopters) | Visual acuity | Eyes changed to emmetropia | Eyes remained hypermetropic | ||
| 2.0 | 1.5 | 1.0 | |||
| +0.25 | 13 | 76 | 14 | 103 | |
| +0.5 | 4 | 67 | 4 | 71 | 4 |
| +0.75 | 36 | 36 | |||
| +1.0 | 23 | 23 | |||
| Over +1.0 | 21 | 9 | 30 | ||
| Depth of focus (diopters) | 0.4 | 0.7 | 1.0 | Total, 210 | Total, 57 |
If we compare the hypermetropia +0.25D with the depth of focus values (4D, 0.7D and 1.0 for visual acuity 2.0, 1.5 and 1.0, respectively), then these values are higher than the degree of hypermetropia. This finding was sufficient reason to consider all of these eyes as emmetropic. In a group of hypermetropia +0.5D 4 eyes with visual acuity 2.0 had a depth of focus 0.4D that was less than degree of hyperopia. These 4 eyes (Table 2) retained their place in the hypermetropic group. The other 71 eyes were changed to the emmetropic group.
The depth of focus of eyes with hypermetropia +0.75D appeared to be equal to or greater than the degree of hypermetropia. Therefore, all 36 eyes were transferred to the emmetropic group. The depth of focus of eyes with hypermetropia +1.0D and greater was less than the degree of hypermetropia. All of these eyes were regarded as hypermetropic.
As a result, the distribution of refractions changed (Table 3). The incidence of emmetropia rose to 65.3%, and hypermetropia occurred in only 12.7% of cases. The number of myopic eyes remained stable at 22%.
DiscussionMethod of subjective refraction is associated with number of sources of uncertainty.12 The depth-of-field/depth-of-focus are considered as the most important among them. The goal of this study was to clarify a role of the depth-of-focus in the subjective refractometry. We do not pretend to establish a new definition for refractive error or to claim a new distribution of refractive error in the general population. Our study cohort presents the pre-selected subjects with good and very good visual acuity. We ignored such factors as accommodation fluctuations and infinity vergence.
The real optical system of the human eye posses a number of the optical errors including aspheric shape refractive surfaces of the cornea and lens, decentration of the refractive surfaces, lens tilt, refractive irregularity inside the lens structure. All mentioned factors act simultaneously and summarize in the joint optical defect which now is called the wavefront aberration and can be measured by the aberrometers.
Aberrometry examination demonstrated that distribution of refractions within the optical zone varies between 1.0D and 1.5D. Emmetropic eyes are characterized by the both myopic and hyperopic refractions. The picture of distribution of refractions allows distinguishing the two components: irregular and regular astigmatism. The first is large and the second is too small.
The study of a relationship between the degree of wavefront aberrations and visual performance revealed a moderate correlation.13–16
The wavefront aberrations render a substantial impact on depth-of-focus and visual acuity. The depth-of-focus ±0.35D relates to visual acuity 1.5 which is close to an average value of visual acuity. The visual acuity 2.0 is characterized by less ocular aberrations and shorter depth-of-focus ±0.2D. The eyes with the lowest limit of a normal vision 1.0 possess a significant amount of the aberrations and a depth of focus ±0.55D. The mentioned values were found for the pupil diameter 3mm.
The aberration patterns are altering during an accommodation tension. This phenomenon does not relate to our study because all our measurements were carried out under condition of relaxed accommodation.
It is fundamental point how to consider in terms of refraction the eyes presented in Fig. 1A–C. When the retina is positioned in the middle of the depth-of-focus (Fig. 1A) the aberrometry map demonstrates irregular distribution of both myopic and hyperopic refractions with amplitude of 1.0–1.5D.
In Fig. 1 anterior edge of the depth-of-focus touches the retina. Hyperopic refractions are dominant in the aberrometry map. At the same time the eye has normal visual acuity and optimal retinal image quality without help of accommodation. We believe that such eye should be considered as emmetropic.
When different degrees of myopia are prevalent in the aberrometry map (Fig. 1C), then however this eye is not myopic, but emmetropic because it possesses a normal unaided visual acuity.
The findings of our study have a more theoretical, rather than practical value.
Theoretically, emmetropia has always been considered the best for adapted refraction, and our data created a basis for verification of that point of view. Many papers regarding the prevalence of hypermetropia2 have presented questions without proper answers. If nature selects for hypermetropia, then the reasons for this phenomenon should be determined. The necessity of constant accommodative tension, not only during near vision but also for far, appears to be a disadvantage of hypermetropia when compared with emmetropia. Our data on the prevalence of emmetropia make our knowledge about the distribution of refractions more consistent, and this distribution falls in line with basic science provisions regarding the physiology of the eye.
We do not insist on the implementation of our approach in the everyday practice of optometrists because the method requires much more time, than conventional methods. Additionally, the depth of focus is a variable parameter that depends on pupil diameter, state of accommodation and pre-corneal tear film. It is impossible to know exactly the extent of the depth of focus, so approximations are inevitable.
However, there are practical implications that can be derived from this study. Namely, an estimation of preciseness of preoperative calculations of IOL optical power for the required target refraction requires postoperative refractometry. The refinement of the subjective method of refractometry does provide a guide for reconsidering the current methods. Light degrees of hypermetropia may not be regarded as an error. The majority of these eyes present emmetropia and predict the target refraction (Fig. 2).