To compare the effect of full-correction versus under-correction on myopia progression.
MethodsA literature search was performed in PubMed, Scopus, Science Direct, Ovid, Web of Science and Cochrane library. Methodological quality assessment of the literature was evaluated according to the Critical Appraisal Skills Program. Statistical analysis was performed using Comprehensive Meta-Analysis (version 2, Biostat Inc., USA).
ResultsThe present meta-analysis included six studies (two randomized controlled trials [RCTs] and four non-RCTs) with 695 subjects (full-correction group, n=371; under-correction group, n=324) aged 6 to 33 years. Using cycloplegic refraction, the pooled difference in mean of myopia progression was – 0.179 D [lower and higher limits: −0.383, 0.025], which was higher but not in full correction group as compared to under correction group (p=0.085). Regarding studies using non-cycloplegic subjective refraction according to maximum plus for maximum visual acuity, the pooled difference in myopia progression was 0.128 D [lower and higher limits: −0.057, 0.312] higher in under-correction group compared with full-correction group (p=0.175). Although, difference in myopia progression did not reach significant level in either cycloplegic or non-cycloplegic refraction.
ConclusionsOur findings suggest that, myopic eyes which are fully corrected with non-cycloplegic refraction with maximum plus sphere, are less prone to myopia progression, in comparison to those which were under corrected. However, regarding cycloplegic refraction, further studies are needed to better understand these trends.
Myopia has already become the more prevalent refractive error worldwide, and its incidence is increasing particularly in young adults and school-aged children.1,2 For decades, researchers had typically focused on the genetic basis of the myopia. While, genetic factor alone cannot explain this dramatic increase. Increasing evidence suggests a role of environmental factors in etiology of the myopia or even myopia progression, such as outdoor activities, physical activities,3 socioeconomic factors and near work activities such as studying, reading, watching television, and using computer.4
There are some available options for myopia correction including spectacle, contact lens and refractive surgery. Spectacles are the most acceptable method in comparison with contact lens and refractive surgery, which is less invasive approach for correction.5 It has been approved that while myopia occurs early in life, it has a tendency toward progression due to related possible factors.6 Different approaches have been used in order to slow or reduce the progression of myopia, such as cycloplegic drugs (Atropine),7–9 specially designed contact lenses such as orthokeratology contact lenses,8–10 multifocal contact lenses,11,12 specially designed spectacles such as bifocal or multifocals13,14 and under-correction of the refractive error.6,9
While there is no evidence for FDA (United State Food and Drug Association) approved pharmaceutical agents which slow the myopia progression, there are some studies concern the possible effect of some drugs on controlling myopia progression such as atropine.15,16 Contributed studies show that atropine is an effective method in slowing the myopia progression.17–19 However, in a study which considered the different concentrations of atropine, side effects were cautioned with 1% concentrate of atropine and also with long term usage.19 Chia et al. also compared three different concentrations of atropine and reported that 0.01% concentration has less side effects compared with 0.50 and 0.1%.20 Although it has been shown that, lower dosages of atropine were found to have less rebound myopic progression.21
Special design of contact lenses such as orthokeratology, rigid contact lenses, and soft multifocal contact lenses,11,12 are alternative methods to control the progression of myopia.22 Orthokeratology contact lenses control myopia through reshaping and flattening the cornea during sleep, these lenses provide the clear vision in all day. It has been proved that, providing the successful fit, it will slower the progression of the myopia, particularly in low-to-moderate myopic patients.23–26 It has been shown that multifocal soft contact lenses reduce myopia progression through providing less peripheral refractive error.27 Similar to contact lenses, bifocal or mulifocal spectacles also control myopia progression through reducing accommodative effort at near vision.13
Under-correction is one of the interventions to reduce or slow myopia progression. One hypothesis about under-correction is that it may decrease the accommodative effort and also the lag of accommodation and subsequently slow or reduce the myopia progression.6,28,29 Some studies have already compared under-correction versus full correction in myopic population.6,30–33 Whereas, there is contradiction in study's findings with regards to the under-correction or full correction of myopia, it seems valuble to have a definite conclusion and provide clinically an appropriate and effective method of correction. Therefore, we aimed to conduct a meta-analysis to investigate whether the under-correction is the method of choice for myopic patients or the full correction is the better way.
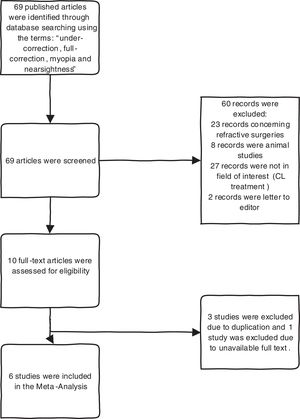
Materials and methodsCurrent meta-analysis was performed based on PRISMA statement, the Preferred Reporting Items for Systematic Reviews and Meta-Analysis. The PRISMA Statement consists of a 27-item checklist and a four-phase flow diagram. The aim of the PRISMA Statement is to help authors improve the reporting of systematic reviews and meta-analyses. PRISMA is used as a basis for reporting systematic reviews, particularly evaluations of interventions.34
Search strategyComplete literature searches of the PubMed, Science direct, Ovid, Web of Science, Scopus and Cochrane library databases was done to find relevant published articles on comparing under-correction with full-correction of myopia. We used a search algorithm that was based on a combination of the terms: “Under-correction, Full-correction, Myopia and Nearsightedness”. The Boolean operators “AND” and “OR” were used in order to specify the search. No beginning date limit or language restriction was used; the search was updated until July 2019. To expand our search, references of the retrieved articles were also screened by two independent authors (NY and SH) for more related studies.
Study selectionStudies concerning the difference between under-correction and full-correction of myopia were considered for inclusion. The exclusion criteria were shown in Flow chart. (Fig. 1) Two researchers (NY and SH) independently reviewed the titles and abstracts of the retrieved articles, applying mentioned inclusion and exclusion criteria and also reviewed the full-text version of the remaining articles to verify their suitability for inclusion.
Data extractionFor each study, information was gathered regarding basic study data (authors, journals, year of publication, country of origin, and study design), patient characteristics (mean age, gender, number of patients) and technical aspects (amount of under-correction, type of refraction and applied device). (Table 1).
Characteristics of included studies.
| Author | Title | Sample size | Age | Refraction | Device | Amount of U | Result |
|---|---|---|---|---|---|---|---|
| Daniel Adler (2006)6 | The possible effect of under-correction on myopic progression in children. | 48 (F:23, U:25) | 6–15y | Non-cycloplegic | Retinoscopy | −0.50D | Under-correction produced a slight but not statistically significant increase in myopic progression compared to full correction. |
| Kahmeng Chung (2002)30 | Under-correction of myopia enhances rather than inhibits myopia progression. | 94 (F:47, U:47) | 9–14y | Non-cycloplegic | Retinoscopy | −0.75D | Under-correction produced more rapid myopia progression. |
| Si yuan Li (2015)31 | Effect of under-correction on myopia progression in 12 year old children. | 253 (F:133,U:120) | 12y | Cycloplegic | Autorefractometer | −0.50≤D | Under-correction or full-correction of myopia by wearing spectacles did not show any differences in myopia progression or axial elongation. |
| Balamurali Vasudevan (2014)33 | Under-correction of human myopia- is it myopigenic? | 79 (F:35, U:12) | 11–33y | Non-cycloplegic | Autorefractometer | −0.50D | Under-correction of myopia produced a small but progressively greater degree of myopic progression than did full correction. |
| Yun-Yun Sun (2017)37 | Effect of under-correction versus full-correction on myopia progression in 12 year-old children. | 121 (F:56, U:65) | 12.7y | Cycloplegic | Autorefractometer | −0.50D | Myopia progression decreased with under-correction. |
| Yao-Hua Chen (2014)38 | Clinical observation of the development of juvenile myopia wearing glasses with full-correction and under-correction. | 132 (F:77, U:55) | 12–18y | Non-cycloplegic | Retinoscopy | −0.50D | The progression of myopia is slow if patients wear glasses with full correction. |
F: Full correction, U: Under-correction. UK: United Kingdom, USA: United State of America, NA: Not available, Y: Years.
Critical Appraisal Skills Program (CASP), was used to assess the methodological quality of included studies based on study design. This tool presents a number of questions that deal very broadly with some of the principles or assumptions that characterize the qualitative aspect of a research. Three broad issues are considered when appraising a qualitative study: 1. Are the results of the study valid? 2. What are the results? 3. Will the results help locally? You are asked to record a “yes”, “no” or “can’t tell” to most of the questions. (CASP; http://www.casp-uk.net/) CASP cross-sectional tool assess quality in five aspects: selection bias which assess whether is the sample representative of a defined population or is everybody included who should have been included, measurement bias which asses if measurements truly reflect what you want, data collection clarifies how data were collected, sample size to assess whether study have enough participants to minimize role of chance and results presentation which assess the main result and if it could be applied to local population. CASP randomized control trials tool assess quality in six aspects: sample allocation which assess whether participants were appropriately allocated to intervention and control group, blinding which assess whether participants, staff and study personnel were blind to participants, informed about the study which assess whether all of the participants who entered the trial were accounted for at its conclusion, similarity in method which assess if all participants were examined in the same way, sample size which clarify whether enough participants were enrolled to minimize role of chance and results presentation assess how the results were presented and what is main result. CASP cohort tool assess quality in four aspects: selection bias, which assess whether cohort recruited in acceptable way and if appropriate sample were included, measurement bias which assess whether exposure was accurately measured to minimize bias, considering confounding factors which assess whether authors identified all confounding factors and acceptable follow up which assess whether follow up was complete enough. (Table 2).
Quality assessment of included studies. (CASP).
| Cross-sectional studies | |||||
|---|---|---|---|---|---|
| Study | Selection Bias | Measurement Bias | Data collection | Sample size | Results presentation |
| Daniel Adler (2006)6 | Yes | Yes | Yes | Cannot tell | Yes |
| Balamurali Vasudevan (2014)33 | Yes | Yes | Yes | Cannot tell | Yes |
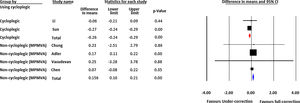
For each study, the mean difference in myopia progression recorded in diopter notation was determined for the full-correction and under-correction groups. To pool the effect sizes across studies, a random effects model was used. The random effects model is a statistical method in which between study variability is accounted for. This method is used especially in pooling data across studies which are different in terms of design, included patients etc. In the forest plot, left column shows the identity (type of applied refraction whether it is cycloplegic or non-cycloplegic) of each included study, and is followed by name of the first author. Next, to the right, we meet some statistic data for each study which includes difference in means of myopia progression in diopter between two approaches of under or full correction, lower and upper limits of confidence interval and p-value. The right-hand column visually displays each study results. The horizontal lines through the boxes illustrate the length of the confidence interval. The longer the lines, the wider the confidential interval, the less reliable the study results. The width of the diamond serves the same purpose. The vertical line is the line of no effect. The boxes show the effect estimates from the single studies, while the diamond shows the pooled result. The larger the box, the bigger the sample size and the narrower the confidence interval (CI), the higher the percentage weight and more the influence the study has on the pooled result. If the diamond shape does not touch the line of no effect, the difference found between the two groups was statistically significant. In that case, the p-value is usually <0.05.
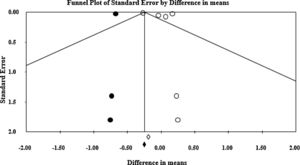
Heterogeneity was evaluated by the Cochrane Q test (the significance level was considered to be 0.05.), and I2 index.35I2 index is the inconsistency index and represents how much of the heterogeneity among the included studies is real and cannot be attributed to sampling error. Publication bias was evaluated graphically by funnel plots and statistically by Egger's regression intercept method.36 The Funnel plot is the plot of the standard errors of the included studies on the y-axis and the effect size on the x-axis. Each dot represents a single study. The y-axis is usually the standard error of the effect estimate. Larger studies with higher power are placed toward the top. Lower powered studies are placed toward the bottom. Asymmetry of this plot may be due to publication bias. Egger's regression intercept is the mathematical counterpart of this visual assessment. Statistically significant results of this test indicate a large asymmetry in the funnel plot. All statistical analyses were performed using Comprehensive Meta-Analysis (version 2, Biostat Inc., USA).
ResultsPRISMA flow chart (PRISMA 2009 flow diagram) of the study has been presented in Fig. 1. Overall six studies were included in this meta-analysis. Two studies with Randomized Controlled Trial (RCT) design, two studies with Cross-sectional and two Cohort studies. (Table 1). Among included studies, 2 studies, used cycloplegic auto refraction (group1) and 4 studies, used non-cycloplegic refraction with retinoscopy and auto refractometer, which were followed by refined subjective refraction based on maximum plus sphere as the end point for best corrected distance visual acuity (group2).
The pooled difference in mean of myopia progression using cycloplegic refraction was −0.179 D [lower and higher limits: −0.383, 0.025], which was higher in the full- correction group as compared to the under-correction group (p=0.085). In group 2, the pooled difference in myopia progression was 0.128 D [lower and higher limits: −0.057, 0.312] higher in under-correction group compared with full-correction group (p=0.175). Fig. 2 shows the forest plot of the myopia progression. The Cochrane Q value was 6.99 (p=0.008) and I2=85.69 for cycloplegic studies and Q value was 1.48 (p=0.686) and I2=0.000 for non-cycloplegic studies. Fig. 3 shows the funnel plot of the included studies. Estimated Eggers regression intercept was 3.70, p=0.33, which indicates a symmetrical funnel plot.
Forest-plot of subgroup analysis based on refraction. Left column shows the identity of each included study and name of the first author. Statistics for each study part presents difference in means of myopia progression, confidence interval and p-value. In left hand column, boxes show the effect estimates from the single studies, while the diamond shows the pooled result. MPMVA=Maximum Plus to Maximum Visual Acuity.
The subgroup analysis of the results of the studies in group 1 and 2 demonstrated pooled progression rates of −0.26 diopter (95% CI −0.24 to −0.29) in group 1, in comparison with 0.15 diopter (95% CI 0.10 to 0.21) in group 2. In the first group of studies, myopia progression was significantly higher in full-corrected subjects in relation to under-corrected cases. (p<0.001) While, in the group 2, myopia progression decreased significantly with full-correction (p<0.001). Although, difference in means of progression was statistically significant in both types of refraction, but the difference was not clinically significant.
DiscussionToday myopia is the main global cause of visual impairment, especially in Asia.39,40 Rapid increase of myopia prevalence has become a considerable global concern for both visual science researchers and practitioners 41 and assessment of approaches to slow down the myopia progression are the main topics of recent studies. Different approaches, such as single-focus spectacles, contact lenses and atropine eye drops, have been employed in an attempt to reduce myopia progression.42–46 Spectacles are still the most common and easiest option. The corrected amount of myopia (full-correction or under-correction) has been the topics of several studies and discussed in several literatures.6,30,31,33,37,38 Under-correction has been believed that can reduce the accommodative stimulus and demand at near,47 and subsequently reduce the blur drive for accommodation, which may be a myopigenic factor.48 Moreover, animal studies have also revealed that myopic defocus resulting from under correction or lack of correction could slow myopia.49–51 A controversial hypothesis regarding under-correction is that defocused retinal image might cause myopia progression due to form deprivation myopia.52 On the other hand, it has been hypothesized that full-correction of myopia optically position the far point of the eye close to the infinity and thus reducing any retinal defocus-induced, blur signals at distance.53 Several studies have compared the effect of under-correction and full-correction of myopia on its progression, but there are discrepancies in findings. Some studies showed that under- correction slows down the myopia progression,31,37 however, other studies reveled that full-correction could be effective in reducing myopia progression.6,30,33,38
This systematic review and meta-analysis showed that the rate of myopia progression significantly differs between under-correction and full-correction approaches. The difference was statistically significant but clinically did not reach the significance level. According to the findings in this meta-analysis, in non-cycloplegic sub-group (retinoscopy followed by maximum plus to the best visual acuity), under-correction caused significantly greater degree of myopia progression as compared to full-correction. The possible rational belief behind it, is that full-correction could prevent any induced defocus of retinal image53 and form deprivation,54 which is believed to be an effective factor in myopia progression or incidence. The present findings are in consistence with Adler,6 Chung,30 Chen38 and Vasuadevan33 studies, which reported that full-correction could significantly reduce the myopia progression compared with under-correction group. Besides, eyes with under-correction are continuously stimulated by blurred image which could causes greater rate of progression.30 Regarding studies with cycloplegic refraction, under-correction could significantly reduce myopia progression compared with full-correction. The possible reason is that under-correction reduce the accommodative stimulus and demand at near,48 and thus reduce the blur drive for accommodation, which is thought to be a myopigenic factor.
The reason that inference on the basis of between sub-groups differences is that there may be another factor, aside from types of refractions, which could be possible reason that could explain the difference between cycloplegic and non-cycloplegic sub-groups. Amount of under-correction may be more than what is really applied in cycloplegic group, as it has been reported myopia progression significantly decreased with increasing amount of under-correction.31 Besides, it has been approved as if under-correction continues, then myopia progression shows higher degree of reduction.55
Moreover, our findings show that, the results of two studies with cycloplegic refraction31,37 could not be comparable with other four non-cycloplegic studies.6,30,33,38 The reason may be that Li31 and Sun,37 in their studies, have applied different amount of under-correction, and just in one study31 the exact rate of progression was reported based on each amount of under-correction, which was a limitation in Sun study. Sun et al.37 have just reported the myopia progression for no correction group and compared it with full-correction. Another reason concerns the definition of under-correction could be the cause of error. In Li31 study, under-correction of myopia was defined as improved presenting visual acuity for at least 2 lines with subjective refraction. Using this criterion of under-correction of myopia may not have detected all under-corrected children because myopes may possess reduced blur sensitivity. Lastly, further randomized control trials investigations are needed using cycloplegic refraction, which in essence serve as the gold standard for precise refraction, to understand better the relation between amount of correction and myopia progression.
This study has also some limitations. Possible heterogeneity has already been reported in all meta-analysis, especially those which evaluate the pooled estimate. Our results showed the high heterogeneity which is likely to arise through differences in inclusion criteria, amount of under-correction and types of refraction. Also, the studies quality might affect the heterogeneity of the results. Therefore, any conclusion was limited by the characteristics of the studies. Otherwise, heterogeneity can be considered as an important drawback in meta-analysis to find the variables associated with variation across the primary studies can help future research on a topic. Publication bias is a major concern in all systematic reviews. The only method in order to avoid publication bias is searching a broad number of databases to locate all possible studies. We did our best to increase the sensitivity of our search strategy. However, publication bias is a major concern in all systematic reviews and cannot be avoided altogether. Citation bias is always a concern in systematic reviews. However, we only used citation analysis as an adjunct to the main search strategy.
ConclusionThe myopic eyes which are fully corrected with non-cycloplegic refraction with maximum plus sphere, are less prone to myopia progression, in comparison with those which were under corrected. Although, our results show statistically significant difference in myopia progression comparing under-correction and full-correction, in either cyclo or non-cyclo groups, this difference might not be clinically considerable. Further studies are warranted to provide reliable evidences in this regard, particularly with cycloplegic refraction.