The use of ophthalmic instruments requires increased effort on the accommodation and vergence system. This study aimed to understand the prevalence of binocular vision anomalies among ophthalmology trainees attending a surgical training program at a tertiary eye care center.
MethodsThis prospective cohort study was carried out between April and November 2017 at a tertiary eye care center in South India. All the ophthalmology trainees inducted for the training programs at the institution underwent a comprehensive ophthalmic and binocular vision assessment. Subjects with previous diagnosis of binocular vision dysfunction and vision therapy were excluded.
ResultsThe mean (SD) age of the subjects was 29 (3) among which 48 were females. Out of the total 75 subjects, 66 had prior surgical experience [range: 1 to 17 years]. Thirty-eight subjects were asymptomatic and 37 were symptomatic. The most common asthenopic symptom was the presence of headache. Forty-one (55%) out of the 75 had a diagnosis of a non-strabismic binocular vision dysfunction. The range of phoria at distance was orthophoria to 14 Prism Diopter (PD) exophoria (mean +/− SD: −1 +/− 3), and at near 4PD esophoria to 25PD exophoria (mean +/− SD: −4 +/− 5). Based on standard diagnostic criteria, 15 subjects (20%) had convergence insufficiency, 14 (19%) had accommodative infacility, 9 (12%) had intermittent divergent squint (IDS), while 3 subjects (4%) had convergence excess.
ConclusionsThis study shows the high frequency of binocular vision dysfunctions among ophthalmology trainees joining a tertiary eye care center.
El uso de instrumentos oftálmicos requiere un esfuerzo incrementado de los sistemas de acomodación y vergencia. El objetivo de este estudio fue comprender la prevalencia de anomalías de visión binocular entre los alumnos de oftalmología que asistían a un programa de formación quirúrgica en un centro terciario de cuidados oculares.
MétodosEste estudio de cohorte prospectivo fue realizado entre abril y noviembre de 2017 en un centro terciario de cuidados oculares en el sur de India. Todos los estudiantes de oftalmología inscritos en los programas de formación en el centro fueron sometidos a un amplio examen oftálmico y binocular. Se excluyó a los sujetos con diagnóstico previo de disfunción de visión binocular y terapia ocular.
ResultadosLa edad media (DE) de los sujetos fue de 29 años (3), de los cuales 48 eran mujeres. Del total de 75 sujetos, 66 tenían experiencia quirúrgica previa [rango: de 1 a 17 años]. Treinta y ocho sujetos eran asintomáticos y 37 sintomáticos. El síntoma de astenopía más común fue la presencia de cefalea. Cuarenta y uno (55%) de los 75 sujetos fueron diagnosticados de disfunción visual binocular no estrábica. El rango de foria de lejos fue de ortoforia a 14 dioptrías prismáticas (DP) a exoforia (media +/− DE: −1 +/− 3) y, de cerca, de esoforia a 4DP a esoforia a 25DP (media +/− DE: −4 +/− 5). Basándonos en criterios diagnósticos estándar, 15 sujetos (20%) tenían insuficiencia de convergencia, 14 (19%) falta de facilidad acomodativa, 9 (12%) tenían estrabismo divergente intermitente (EDI), y 3 sujetos (4%) tenían exceso de convergencia.
ConclusionesEste estudio muestra la alta frecuencia de disfunciones de visión binocular entre los estudiantes de oftalmología que acudieron a un centro terciario de cuidados oculares.
Ophthalmic training programs play a vital role in upgrading the knowledge of the medical professional to a super-speciality. Microsurgery training becomes one of the essential surgery skills of focus. Ophthalmic instrumentation used during micro-surgery heavily relies on microscope examination with the use of magnification. The use of magnification extends to the use of day-to-day instruments in outpatient department such as slit-lamp, fundus examination using +90 Diopter lens and indirect ophthalmoscope. These instruments require additional accommodation and convergence to maintain the clarity and singularity of the images.1
Recent studies report a high prevalence of binocular dysfunction among university students, ranging between 32.3–42%.2 It can be hypothesized that a similar or an increased prevalence is expected in professions where the visual demand is high as in specialties like ophthalmology.
It has been reported by Porcar et al. that, some trainees experience blurred images while using indirect ophthalmoscope, but it is unclear if the blur is due to an actual binocular vision dysfunction or inappropriate technique and learning curve. Some trainees tend to place +2.00 Diopter lens in oculars to decrease the blur, and have also reported a reduction in symptoms though it does not solve the underlying cause.3 Other than these few studies, there are no studies that investigated the prevalence of binocular vision anomalies among eye care professionals.
It is possible that non-strabismic binocular vision issues could give rise to symptoms under the high demands of operating and viewing microscope and during fine motor tasks such as suture handling. In the presence of refractive errors corrected by spectacles, the imposed vergence demand due to change in vertex distance, and any potential centration issues in spectacles can also add to the focusing difficulty through operating microscopes. As a first step to explore these hypothesis, the present study aimed to document the frequency of non-strabismic binocular vision anomalies among ophthalmology trainees joining a tertiary center.
Material and methodsThis prospective cohort study was carried out between April and November 2017, at a tertiary eye care center in Southern India. The ophthalmology trainees who were inducted into the institution during the study period were enrolled into the study. The trainees signed a written informed consent prior to enrollment into the study.
The study was approved by the institutional review board of Vision Research Foundation (VRF) and it adhered to the Tenets of Declaration of Helsinki. All the ophthalmology trainees inducted during the study period underwent a comprehensive ophthalmic and binocular vision assessment including documentation of visual symptoms. All the subjects were administered a visual fatigue checklist and a task specific questionnaire (Appendix A and B). The questionnaire and checklist were designed based on expert interaction with 5 senior ophthalmology surgeons with more than 10 years of professional experience.
Inclusion criteria- •
All ophthalmology trainees who attended the training program in the tertiary eye care center.
- •
No age criteria.
- •
Subjects with known history of binocular vision dysfunction and vision therapy.
Binocular vision parameters assessed in this study included:
- 1
Stereopis using Titmus stereo test.
- 2
Worth four dot test for distance and near.
- 3
Magnitude of distance and near phoria was assessed using prism bar cover test and Modified Thorington test done at 6 m and 40 cm.
- 4
Inter-pupillary distance (IPD) for near using an IPD ruler.
- 5
Accommodation convergence/Accommodation (AC/A) ratio by heterophoria method.
- 6
Near point of convergence (NPC) with accommodative target (linear vertical target of reduced Snellen 6/9, subjective and objective) and penlight with red-green filter. Both break and recovery were documented and average of three measurements was documented.
- 7
Near point of accommodation (NPA) by the push-up method. The first sustained blur was documented, monocularly and binocularly.
- 8
Dynamic retinoscopy - Monocular estimate method (MEM) at 40 cm was used to assess the accommodative response for the right and left eyes.
- 9
Negative and positive relative accommodation (NRA and PRA) were measured using N6 target at 40 cm.
- 10
Step vergence amplitudes were assessed for distance and near using prism bar done at 6 m and 40 cm.
- 11
Vergence facility was measured using 12 base out/3 base in vergence flippers at 40 cm.
- 12
Accommodative facility was measured with ±2.00 Diopter lens accommodative flippers at 40 cm, for subjects below 40 years of age.
The criteria for diagnosis of non-strabismic binocular vision anomalies (NSBVA) was adopted from Scheiman and Wick.4
ResultsThe total sample size of the study was 75, with 48 females. The mean (SD) age of the subjects was 29 (3) years (range: 24 to 48). Out of the 75 subjects, 66 had prior surgical experience, ranging between 1 and 17 years, and 9 did not have prior surgical experience. Twenty-four subjects were emmetropic (32%), followed by astigmatism in 8 (11%) subjects, myopia in 18 (24%) subjects and myopic astigmatism in 22 (29%) subjects, hyperopia in 2 (3%) subjects, and hyperopic astigmatism in 1 (1%) subject.
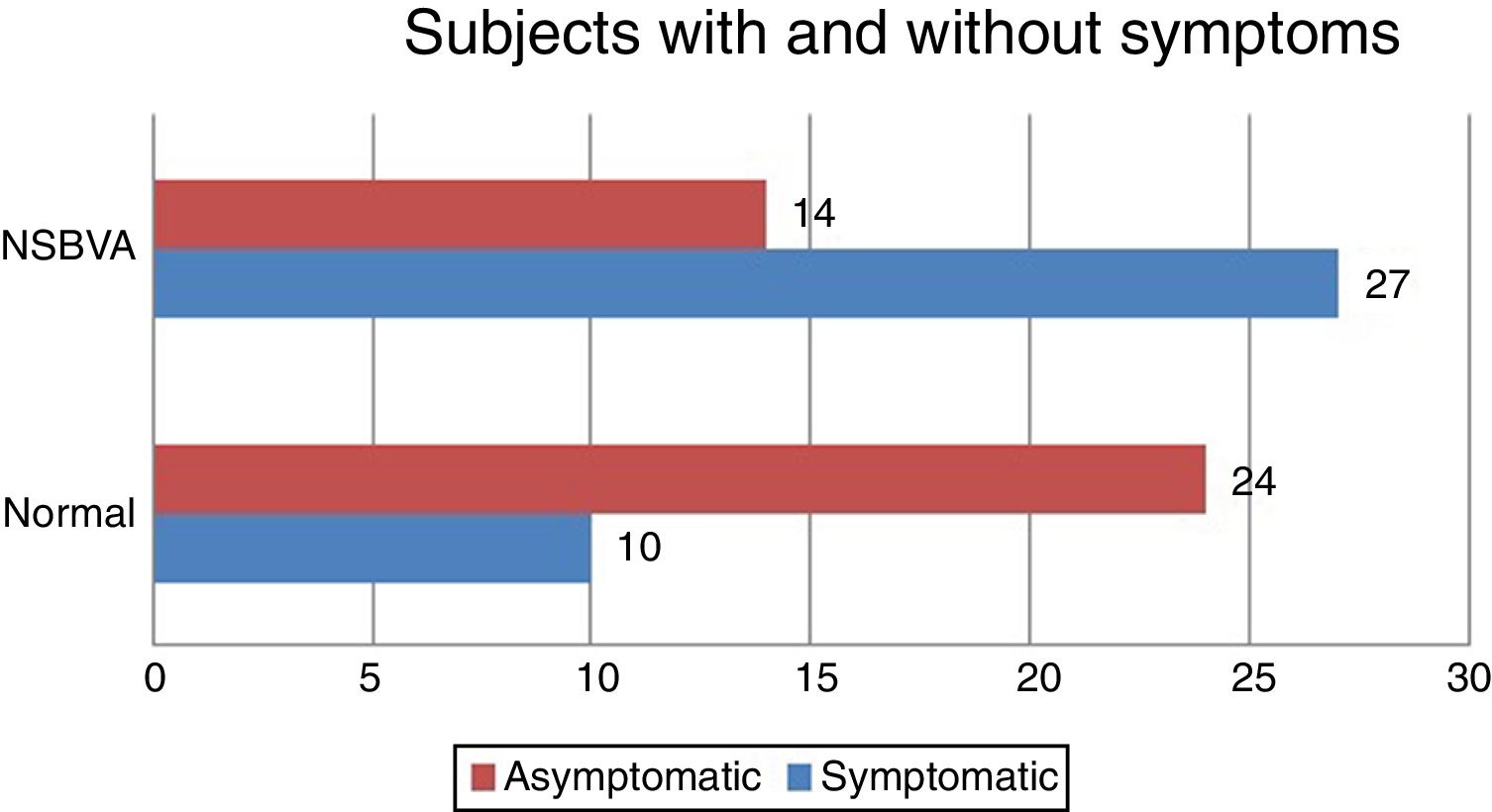
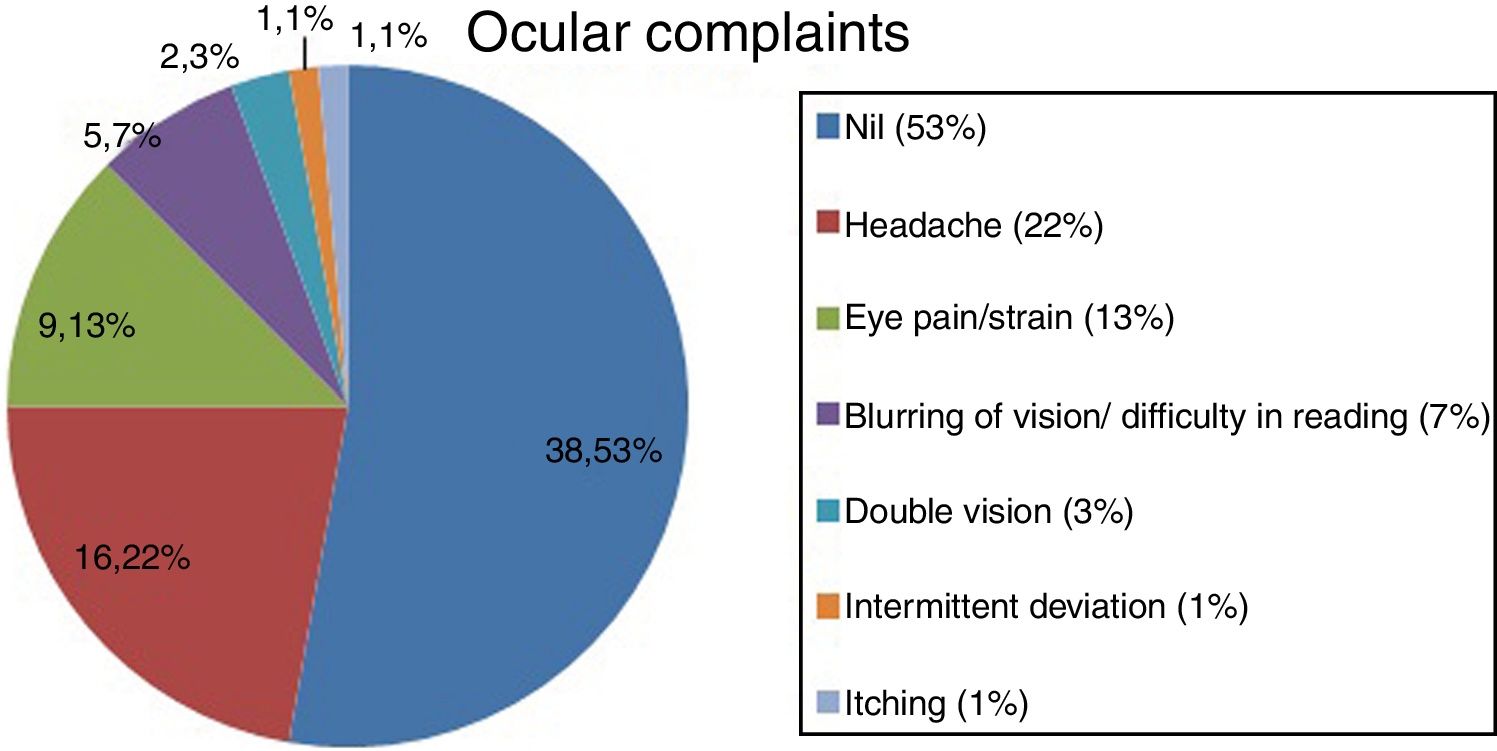
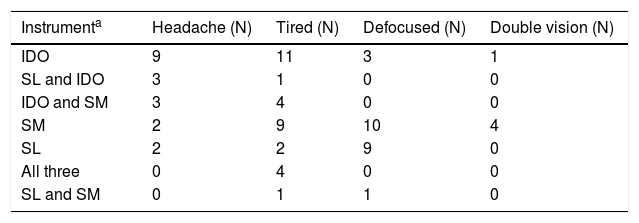
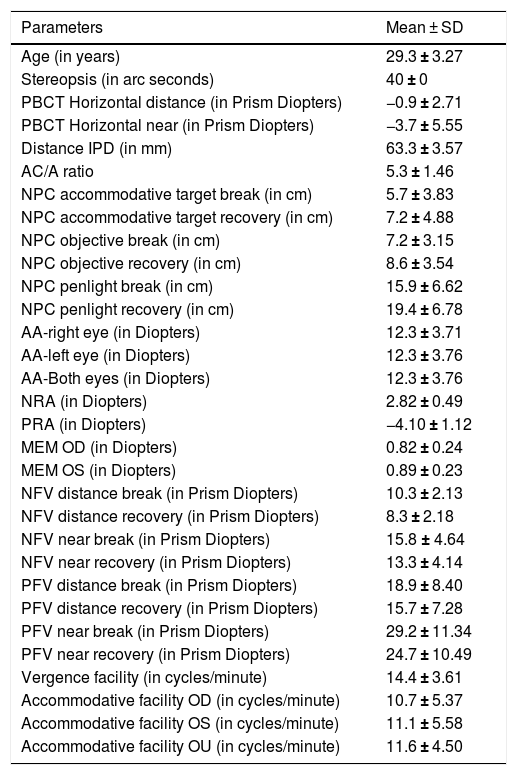
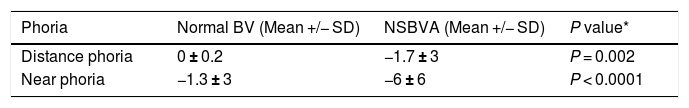
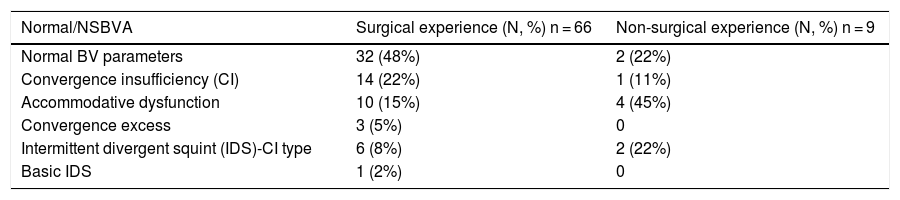
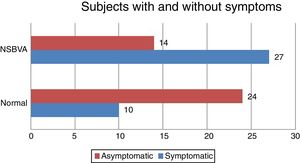
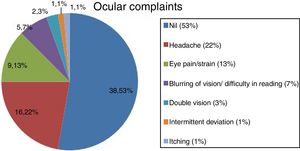
Among the 75 subjects, 41 subjects had a diagnosis of NSBVA and 34 had normal binocular vision. Among the NSBVA group, 27 were symptomatic and 14 were asymptomatic (Fig. 1). The most common asthenopic symptom was headache (23%) followed by eye pain and eyestrain (12%) (Fig. 2). The details of task specific questionnaire are specified in (Table 1). The descriptive statistics for all binocular vision parameters in the overall sample is depicted in (Table 2). The range of phoria at distance and near was orthophoria to 14PD exophoria (mean +/− SD: −1 +/− 3) and 4PD esophoria to 25PD exophoria (mean +/− SD: −4 +/− 5) respectively (Table 3). Compared to subjects with normal binocular vision, the differences in phoria parameters were found to be statistically significant for distance (independent T-test, P = 0.002), and near (independent T-test, P < 0.0001). In the prior surgical experience group, 32 subjects had normal BV (48%) and 34 subjects (52%) were diagnosed with a NSBVA. Convergence insufficiency was the most common NSBVA found in 14 subjects (22%), followed by accommodative dysfunction in 10 subjects (15%). In the non-surgical group, 2 subjects had normal binocular vision and 4 subjects had an accommodative dysfunction. The overall distribution of NSBVA in this sample is depicted in Table 4. There was no statistically significant difference in the proportion of NSBVA between ametropia and emmetropia in this sample (Z-test, P > 0.05).
Task specific questionnaire details.
| Instrumenta | Headache (N) | Tired (N) | Defocused (N) | Double vision (N) |
|---|---|---|---|---|
| IDO | 9 | 11 | 3 | 1 |
| SL and IDO | 3 | 1 | 0 | 0 |
| IDO and SM | 3 | 4 | 0 | 0 |
| SM | 2 | 9 | 10 | 4 |
| SL | 2 | 2 | 9 | 0 |
| All three | 0 | 4 | 0 | 0 |
| SL and SM | 0 | 1 | 1 | 0 |
Mean and standard deviation of the Binocular vision parameters in the overall sample.
| Parameters | Mean ± SD |
|---|---|
| Age (in years) | 29.3 ± 3.27 |
| Stereopsis (in arc seconds) | 40 ± 0 |
| PBCT Horizontal distance (in Prism Diopters) | −0.9 ± 2.71 |
| PBCT Horizontal near (in Prism Diopters) | −3.7 ± 5.55 |
| Distance IPD (in mm) | 63.3 ± 3.57 |
| AC/A ratio | 5.3 ± 1.46 |
| NPC accommodative target break (in cm) | 5.7 ± 3.83 |
| NPC accommodative target recovery (in cm) | 7.2 ± 4.88 |
| NPC objective break (in cm) | 7.2 ± 3.15 |
| NPC objective recovery (in cm) | 8.6 ± 3.54 |
| NPC penlight break (in cm) | 15.9 ± 6.62 |
| NPC penlight recovery (in cm) | 19.4 ± 6.78 |
| AA-right eye (in Diopters) | 12.3 ± 3.71 |
| AA-left eye (in Diopters) | 12.3 ± 3.76 |
| AA-Both eyes (in Diopters) | 12.3 ± 3.76 |
| NRA (in Diopters) | 2.82 ± 0.49 |
| PRA (in Diopters) | −4.10 ± 1.12 |
| MEM OD (in Diopters) | 0.82 ± 0.24 |
| MEM OS (in Diopters) | 0.89 ± 0.23 |
| NFV distance break (in Prism Diopters) | 10.3 ± 2.13 |
| NFV distance recovery (in Prism Diopters) | 8.3 ± 2.18 |
| NFV near break (in Prism Diopters) | 15.8 ± 4.64 |
| NFV near recovery (in Prism Diopters) | 13.3 ± 4.14 |
| PFV distance break (in Prism Diopters) | 18.9 ± 8.40 |
| PFV distance recovery (in Prism Diopters) | 15.7 ± 7.28 |
| PFV near break (in Prism Diopters) | 29.2 ± 11.34 |
| PFV near recovery (in Prism Diopters) | 24.7 ± 10.49 |
| Vergence facility (in cycles/minute) | 14.4 ± 3.61 |
| Accommodative facility OD (in cycles/minute) | 10.7 ± 5.37 |
| Accommodative facility OS (in cycles/minute) | 11.1 ± 5.58 |
| Accommodative facility OU (in cycles/minute) | 11.6 ± 4.50 |
PBCT- Prism bar cover test, IPD – Interpupillary distance, NPC – near point of convergence; AA – Amplitude of accommodation; AC/A – accommodation convergence to accommodation; NFV – Negative fusional vergence; PFV – Positive fusional vergence; MEM – Monocular estimate method; NRA – Negative relative accommodation; PRA – Positive relative accommodation.
Mean and standard deviation of phoria among subjects with normal binocular vision (BV) and non-strabismic binocular vision anomalies (NSBVA).
| Phoria | Normal BV (Mean +/− SD) | NSBVA (Mean +/− SD) | P value* |
|---|---|---|---|
| Distance phoria | 0 ± 0.2 | −1.7 ± 3 | P = 0.002 |
| Near phoria | −1.3 ± 3 | −6 ± 6 | P < 0.0001 |
Frequency of non-strabismic binocular vision anomalies (NSBVA) in surgical and non-surgical experience group.
| Normal/NSBVA | Surgical experience (N, %) n = 66 | Non-surgical experience (N, %) n = 9 |
|---|---|---|
| Normal BV parameters | 32 (48%) | 2 (22%) |
| Convergence insufficiency (CI) | 14 (22%) | 1 (11%) |
| Accommodative dysfunction | 10 (15%) | 4 (45%) |
| Convergence excess | 3 (5%) | 0 |
| Intermittent divergent squint (IDS)-CI type | 6 (8%) | 2 (22%) |
| Basic IDS | 1 (2%) | 0 |
The purpose of this study was to report the frequency of undetected binocular vision anomalies among ophthalmology trainees. Of the total 75 subjects, 41 subjects (55%) were diagnosed to have NSBVA. It is well established that NSBVAs are highly prevalent among the general population,2,3 and thus it is expected to be high among this study sample as well. Nonetheless the intention of the study is to understand the awareness of this among eye care professionals who diagnose these disorders, and to assess the symptomatology of these issues impacting their focusing and training with binocular microscopes.
The most common disorders among this sample include convergence insufficiency and accommodative excess. Accommodative excess presented either solitarily or combined with vergence anomalies. These results were similar to the study done by Porcar and Martinez-Palomera3 in a population of university students (1997). However, the results cannot be directly compared due to the age and methodology differences between the studies. Frantz et al. reported 23 subjects with the presence of binocular vision syndrome among 30 optometry students.5 In another study of 212 first year university students, about 12.7% of subjects were diagnosed with vergence anomalies, and convergence insufficiency was the commonest binocular vision anomaly6 whereas, in this study both vergence and accommodative anomalies were present. The symptomatology reported among the university students included intermittent diplopia, headache and transient blurred vision, that was similar to the symptoms reported by the Ophthalmology trainees in this study who reported headache and eye strain as the commonest symptoms.
A case reported by Smith et al.1 discussed about a 36-year-old plastic surgeon who had binocular diplopia while looking through the operating microscope at the end of residency training program. He was then diagnosed to have intermittent exotropia at near with convergence insufficiency, and with vision therapy for the same reported improvement in signs and symptoms. This case report highlights the difficulties in microsurgical performance with impaired binocular vision. Similarly, a study on microscope operators at an electronic plant reported significant phoria in almost 30% of subjects and intermittent exotropia in one case.7
In this study, except for one subject, rest with refractive errors used spectacles as the preferred mode of refractive correction. It could be hypothesized that the vergence demands could differ between an emmetrope and subject with refractive error while viewing through the microscope due to the vertex distance, and distance from the eye to the microscope. * Nonetheless we did not find any difference in the frequency of NSBVA between emmetropia and ametropia in general in this sample.
*A separate paper computing the vergence demands from this sample is under review.
In a study2 done among 3rd and 4th year optometry students, the authors tried to understand ocular accommodation while viewing through Binocular indirect ophthalmoscope (BIO) with +2.00 Diopter (plus group) and without +2.00 Diopter (plano group). In this study, an increased number of subjects in BIO plus group had no accommodative or binocular syndromes compared to BIO plano group. BIO plus group also showed primarily convergence excess due to the increased convergence demand with +2.00 Diopter lenses. The current study also showed that a higher percentage of subjects reported asthenopic symptoms while using BIO compared to other instruments. Also there was an increased predilection for exophoric tendency and convergence insufficiency among ophthalmology trainees. It is also important to note that, almost 18.6% of the sample remained asymptomatic despite the clinical diagnosis of a non-strabismic binocular vision. It is also not clear if the asymptomatic group will develop symptoms over a period of time, especially with increased visual demands.
It is also important that the awareness related to potential visual symptoms, and ergonomic considerations to be taught or discussed during the early stages of training for eye care professionals.
ConclusionThis study emphasizes the need for early detection of non-strabismic binocular vision anomalies among ophthalmology trainees and highlights the high frequency of convergence insufficiency and accommodative dysfunctions in this sample. Future studies are intended to understand the visual demands pertinent to accommodation and vergence in this population and also to test the efficacy of vision therapy in remediating and improving the binocular vision parameters.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestThe authors have no conflicts of interest to declare.
Statement of publicationThis article has not been submitted/published elsewhere.
Dr. Krishna Kumar R, Principal, Elite School of Optometry and Dr. P.P. Santanam, Professor of Occupational Optometry, Elite school of Optometry for inputs with the manuscript. This study was presented in part as a oral presentation at 17th Dr. E. Vaithilingam memorial scientific session, Sankara Nethralaya, Chennai and The World Congress of Ophthalmology, Barcelona.
- 1
Have you already done ophthalmic microsurgery – yes/no
- 2
Have you already used slit lamp and IDO – yes/no
- 3
For how many years have you been using the microscopes which include IDO, slit lamp, operating microscope
- 4
Approximate number of slit lamp examinations already done <50/50–100/>100/>500
- 5
Approximate number of ophthalmic microsurgery already done <50/50–100/>100/>500
- 6
Approximate number of indirect ophthalmoscopy (IDO) already done <50/50–100/>100/>500
- 7
Do you have symptoms of headache after use of microscopes – yes/no
- 8
Do you feel your eyes are tired after use of microscopes – yes/no
- 9
Do you have a problem adjusting the focus of the microscope while operating – yes/no
- 10
Does the operating field keep getting defocussed as your time of surgery increases – yes/no
- 11
Do you have problems assessing the depth while operating – yes/no
For each item, circle the most appropriate response on five‐point scale (low to high):
(a) Eyes feel tired
(b) Eyes feel dry, irritated or burning
(c) Eyes tearing
(d) Eye pain
(e) Blurred vision
(f) Double vision
(g) Blinking more frequently
(h) Headache