To evaluates the role of measuring intraocular pressure (IOP) outside office-hour in primary adult onset glaucoma.
MethodsThis retrospective study included 100 cases of primary adult onset glaucoma. IOP readings obtained with Goldmann applanation tonometry between 7 am and 10 pm were compared to office-hour readings.
ResultsOne hundred patients were enrolled (mean age: 58.64±10.98 years) in the study. Overall, mean diurnal IOP was significantly higher than mean office IOP (p<0.05). Two-thirds of the patients had peak IOP measurements outside office-hour. Mean diurnal IOP fluctuation (7.03±2.69mm Hg) was significantly higher than mean office IOP fluctuation (4.31±2.6mm Hg) (p<0.003). There was a significant correlation between baseline IOP and fluctuation in IOP (r=0.61, p<0.001).
ConclusionThe mean diurnal IOP and IOP fluctuations were higher than office-hour readings in patients with primary adult onset glaucoma. Diurnal monitoring may be particularly useful in patients with high baseline IOP.
Evaluar la función de la medición de la presión intraocular (PIO) fuera del horario de consulta en el glaucoma de reciente aparición en edad adulta.
MétodosEste estudio retrospectivo incluyó 100 casos de glaucoma primario en adultos. Se compararon las mediciones de la PIO obtenidas mediante tonometría de aplanación de Goldmann entre las 7:00 y las 22:00, con los valores en horario de consulta.
ResultadosSe incluyó a cien pacientes (edad media: 58,64±10,98 años). Globalmente, la PIO media diurna fue significativamente superior que la PIO media en horario de consulta (p<0,05). Dos tercios de los pacientes reflejaron unos valores elevados de la PIO fuera del horario de consulta. La fluctuación de la PIO media diurna (7,03±2,69mm Hg) fue considerablemente superior que la fluctuación de la PIO media en horario de consulta (4,31±2,6mm Hg) (p<0,003). Se produjo una correlación significativa entre la PIO basal y la fluctuación de PIO (r= 0,61, p <0,001).
ConclusiónLas fluctuaciones de la PIO media diurna y la PIO fueron superiores a los valores medidos en horario de consulta en pacientes con glaucoma primario de aparición en la edad adulta. La supervisión diurna puede resultar particularmente útil en pacientes con una elevada PIO basal.
Intraocular pressure (IOP) is the only treatable risk factor in patients with glaucomatous optic neuropathy.1–4 Although IOP measurement at one time point is important in a glaucoma patient, significant diurnal and nocturnal IOP variations have been reported.5–7 While some studies show a morning IOP peak,8–11 there are others which report that the nocturnal supine IOP may be higher for many individuals.12–16
Diurnal IOP behavior in glaucoma patients has implications for both disease pathogenesis and management. Peak IOP and IOP fluctuations are known to be independent risk factors for the progression of glaucoma.17,18 Since the management of glaucoma subjects is commonly based on isolated IOP readings obtained during the office-hours visits, there is a chance that the peak IOP and IOP fluctuations may be missed. For these reasons, monitoring IOP during the daytime or over a 24h period offers obvious theoretical benefits. While some ophthalmologists schedule patient visits at different times of the day or obtain IOP measurements throughout the day, obtaining IOP measurements outside of normal office hours is uncommon considering the cost and inconvenience caused to both the patient and the treating physician or optometrist.
This study was conducted to evaluate the IOP behavior across diurnal and office hours; and factors associated with IOP fluctuation in patients with both primary open angle glaucoma (POAG) and primary angle closure glaucoma (PACG).
MethodsThis retrospective study involved a review of the records of all patients visiting the outpatient services at our glaucoma facility between October 1, 2009, and October 1, 2010. One hundred patients on chronic topical antiglaucoma medications (50 cases of primary open angle glaucoma and 50 cases of primary angle closure glaucoma post-laser iridotomy) were randomly selected for the study. The study conformed to the tenets of 1995 Declaration of Helsinki.
Inclusion criteria included an elevated IOP (>21mm Hg) on at least two repeated measurements, ophthalmoscopic evidence of glaucomatous optic disc damage (cup-disc diameter>0.6, asymmetry ≥0.2 between the two eyes, localized thinning of neuroretinal rim, or disc hemorrhage) and glaucomatous visual field defects identified on visual field testing with Humphrey 30-2 SITA Standard (a cluster of three points with probabilities of 5% on the pattern deviation map in at least one hemifield, including at least one point with a probability of 1%; and a glaucoma hemifield test (GHT) result outside 99% of age-specific normal limits, and a pattern standard deviation (PSD) outside 95% of normal limits). The subjects were classified into POAG and PACG depending on the gonioscopy findings. In subjects with PACG, posterior trabecular meshwork was not visible in more than two quadrants on indentation gonioscopy with a Sussman gonioscope. All PACG patients had a peripheral iridotomy completed at least six weeks prior to inclusion in the study. Exclusion criteria were patients with IOP>30mm Hg, pseudoexfoliation/pigmentary glaucoma, any other anterior segment or posterior segment pathology, and corneal disease interfering with the applanation tonometry. If both eyes were found eligible, one eye was randomly selected for the study.
The review of records of the patients included making a note of the corrected distance visual acuity, baseline IOP, number of antiglaucoma medications, and ultrasound central corneal thickness measured with Pacscan (300AP, Sonomed, USA).
The diurnal IOP measurements, routinely run at our center, are taken at three hour intervals between 7 am and 10 pm by a trained resident ophthalmologist. The measurements are recorded with the Goldmann applanation tonometer with the patient in the sitting position on the same day for each patient. The Goldmann tonometer is calibrated at the start of each day. At each time point, the eyes are anaesthetized with 0.5% proparacaine eye drops (Paracain, Sunways, Mumbai, India) and the tear film is stained with fluorescein strips. The readings are taken at 7am, 10am, 1pm, 4pm, 7pm and 10pm.
Characterization of IOP measurements: The IOP measurements were characterized as follows:
- 1.
Mean office IOP (IOPo): Average of IOP values obtained between 9am and 5pm (10am, 1pm, 4pm).
- 2.
Mean diurnal IOP (IOPd): Average of IOP values obtained between 7am and 10pm (7am, 10am, 1pm, 4pm, 7pm, 10pm).
- 3.
Office IOP fluctuation (IOPof): Difference between the highest and the lowest IOP readings obtained between 10am and 4pm (10am, 1pm, 4pm).
- 4.
Diurnal IOP fluctuation (IOPdf): Difference between the highest and the lowest IOP readings obtained between 7am and 10pm (7am, 10am, 1pm, 4pm, 7pm, 10pm).
Statistical Analysis was completed using the SPSS software (version 11.5, SPSS, Inc., Chicago, Illinois). The mean IOP and IOP fluctuations during the office hours were compared with those recorded during the entire period (diurnal) using the paired, 2-tailed t test. Correlation between the IOP fluctuation and various measured variables (age of the patient, baseline IOP, central corneal thickness, and number of antiglaucoma medications used) was assessed using the Pearson correlation coefficient.
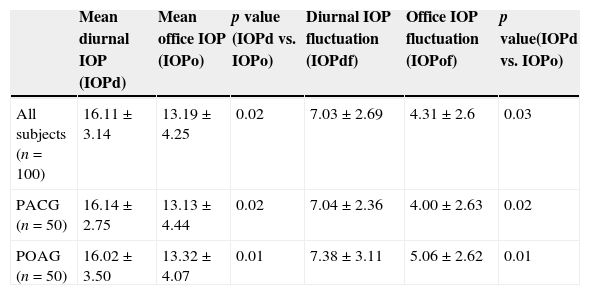
ResultsThe study included 100 eyes (50 POAG and 50 PACG, 42 females and 58 males). The mean age of the patients was 58.64±10.98 years (POAG: 56.99±8.1 years, PACG: 59.23±9.6 years, p=0.67). Table 1 shows the details of the IOP measurements of the patients enrolled. The mean office IOP and office fluctuations in IOP were statistically lower than the mean diurnal IOP and diurnal fluctuations in IOP respectively. The mean central corneal thickness was 524.47±26.94μm. The mean number of antiglaucoma medications used by all the patients was 1.56±0.77.
Intraocular pressure (IOP) characteristics across the study population.
| Mean diurnal IOP (IOPd) | Mean office IOP (IOPo) | p value (IOPd vs. IOPo) | Diurnal IOP fluctuation (IOPdf) | Office IOP fluctuation (IOPof) | p value(IOPd vs. IOPo) | |
|---|---|---|---|---|---|---|
| All subjects (n=100) | 16.11±3.14 | 13.19±4.25 | 0.02 | 7.03±2.69 | 4.31±2.6 | 0.03 |
| PACG (n=50) | 16.14±2.75 | 13.13±4.44 | 0.02 | 7.04±2.36 | 4.00±2.63 | 0.02 |
| POAG (n=50) | 16.02±3.50 | 13.32±4.07 | 0.01 | 7.38±3.11 | 5.06±2.62 | 0.01 |
IOP: Intraocular pressure; POAG: Primary open angle glaucoma; PACG: Primary angle closure glaucoma.
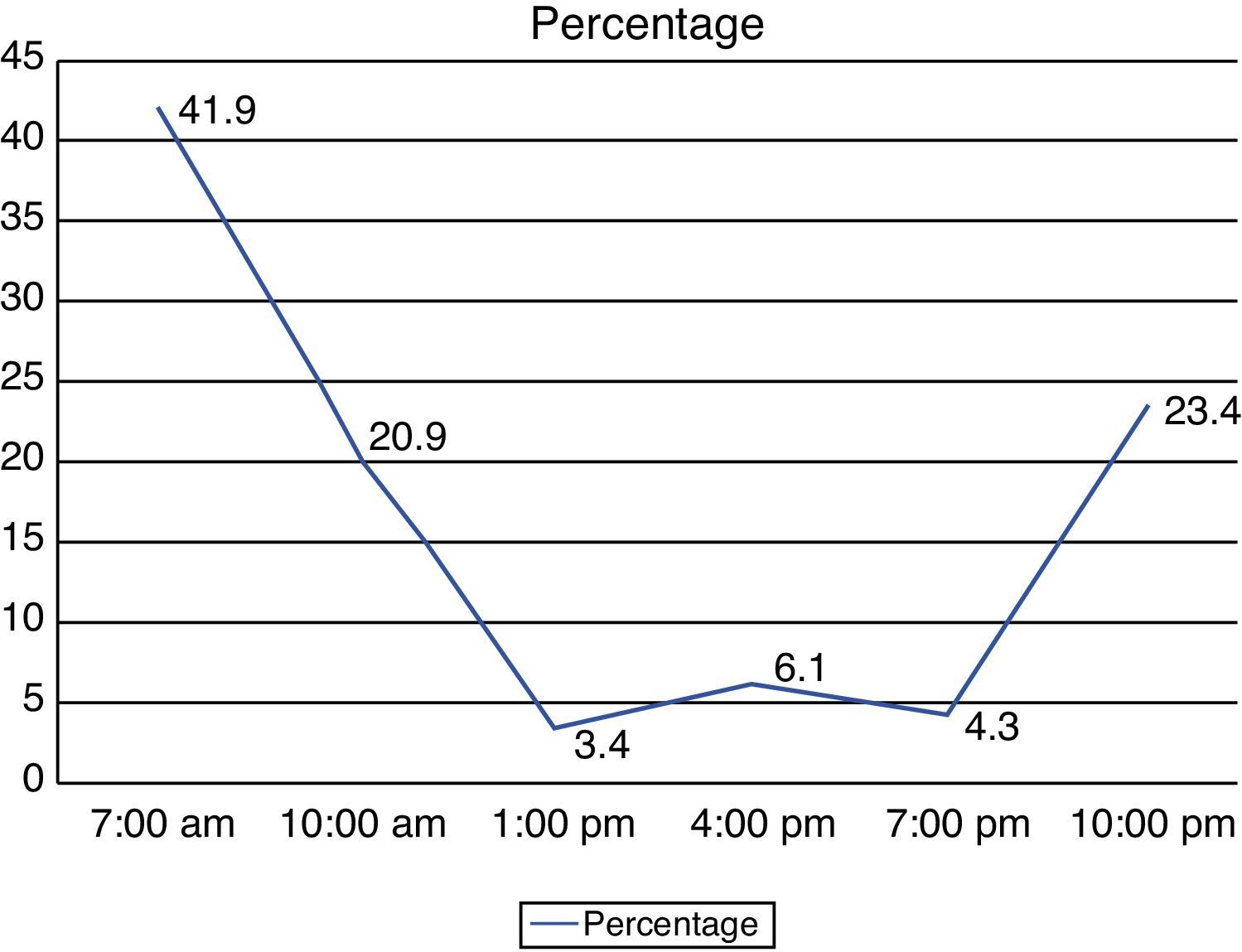
Peak IOP was reached most often at 7am (42/100; 42%) followed by 10pm (23/100; 23%). The percentage of patients having their IOP peak at 10am, 1pm, 4pm, and 7pm were 20.9%, 3.4%, 6.1%, and 4.3% respectively. Thus, two-third of the patients had their IOP peak outside the office hours (Fig. 1).
On comparing the PACG and the POAG subjects, there was no significant difference between the two groups with respect to mean diurnal IOP (p=0.31), mean office IOP (p=0.24), mean diurnal fluctuation (p=0.45) and mean office fluctuation (p=0.63).
The overall mean baseline IOP (pretreatment) was 24.20±4.61mm Hg (PACG: 25.00±4.69mm Hg; POAG: 23.40±4.41mm Hg, p=0.46). The patients were grouped into those with diurnal fluctuation greater or less than 4mm Hg. The mean baseline IOP was 25.01± 4.21mm Hg in the former group and was 20.17±2.32mm Hg in the latter (p=0.001). Statistically significant correlation was noted between the baseline IOP and IOP fluctuation (r=0.61, p<0.001). The IOP fluctuation did not show significant correlations with CCT (r=0.02, p=0.183), the number of topical antiglaucoma medications used by the patient (r=0.01, p=0.988) and age (r=0.01, p=0.461).
DiscussionDiurnal IOP testing holds great importance in the treatment of glaucoma. It can help explain the presence and progression of glaucoma in subjects whose randomly sampled IOP seems to be consistently normal or well controlled. If significant peaks are noted, IOP fluctuations may be responsible for the pathological changes associated with glaucoma.13.14 This study was conducted to evaluate the office and diurnal IOP fluctuations in our glaucoma population. The inclusion of PACG patients and evaluation of various correlations of several clinical parameters with diurnal fluctuation in IOP are the novel points in our study.
IOP measurements obtained during the office hours form the basis of management of glaucoma patients in routine clinical settings. In the present study, we noted that two-thirds of the glaucoma patients had their IOP peak outside office hours. Diurnal IOP estimation is not routinely performed in developing countries due to various issues including cost, inconvenience and time involved both for the patient and for the treating physician. Additionally the working hours for most government institutions are from 9am to 5 pm, adding to the difficulty of obtaining measurements before or after this time.
Several studies have been conducted in relation to the diurnal curve. Magacho et al. studied IOP fluctuations in 25 eyes with POAG and reported that IOP measurements on different days, at different time points, strongly correlate to diurnal curve.19 However, the repeatability of the diurnal IOP curves has been questioned by recent studies. Realini et al. recently studied diurnal IOP pattern in 40 healthy individuals. They suggested that diurnal IOP measurements are not repeatable in the short term.20 It has also been reported previously that a subject might have a “falling curve” one day and a “rising curve” the next day.21 Nonetheless, in our experience, we suggest that the significance of diurnal IOP measurements cannot be overestimated.
Usually, IOP measurements obtained during the office hours form the basis of management of glaucoma patients. In our study, two-thirds of the subjects had their peak IOP outside office hours. This is similar to the results published by Hughes et al. reporting that half of their patients had their IOP peak outside office hours.22 They also noted that the peak IOP during 24-h monitoring was on average 4.9mm Hg higher than the peak clinic IOP. The 24h IOP monitoring resulted in a change of clinical management in 79% of their patients. However, the study enrolled a small number of patients.22 Jonas et al. also studied 547 Caucasian glaucoma patients and reported that any single intraocular pressure measurement taken between 7am and 9pm has a higher than 75% chance to miss the highest point of a diurnal curve.23 Another study by Barkana et al. including 22 patients with glaucoma showed that peak IOP was recorded outside of office hours in at least 69% of their patients.24 It was also noted that 24-h IOP monitoring revealed a significantly higher IOP fluctuation than that during office hours. However, the authors in this study compared the diurnal readings with the IOP measurements obtained during the previous office visits. Recently, studies have shown that peak IOP and IOP fluctuations can be extrapolated from the office hour IOP readings taken in the supine position, reducing the need for obtaining 24h curves.16,25
It is difficult to compare the results of diurnal variation between various studies. Differences in clinical settings including medication, position, time points and the use of different tonometers may contribute significantly to the differences. In cases with corneal edema, IOP measurements taken too soon after waking up could be artificially low. The fact is that in case of glaucoma subjects, the use and timing of antiglaucoma medications may alter the timing of diurnal fluctuations and explain differences between studies. This may be critical for closed angle cases as without treatment their fluctuation could be dominated by an episode of closure. When compared to the study by Barkana et al. where 24h measurements were obtained,24 our mean diurnal IOP and fluctuations are comparable (16.11±3.14mm Hg vs. 16.8±3.2mmHg; 6.9±2.9mmHg vs. 7.03±2.69mmHg), whereas the office hour values are slightly lower as compared to their study population (13.19±4.25mmHg vs. 14.7+3.2mmHg; 3.8±2.3mm Hg vs. 4.31±2.6mm Hg). Similarly, the mean values are comparatively higher in the study by Fogagnolo and colleagues where again the 24h values were measured (mean IOP: 21.3±4.5mm Hg; fluctuation 9.3±3.2mm Hg).25
Whereas most studies have elaborated on the diurnal patterns in patients with POAG, few studies have characterized the diurnal variation of IOP in PACG. Visual field loss in PACG is associated with IOP fluctuations.26 A diurnal fluctuation of 4–5mm Hg has been reported in eyes with PACG, which is comparable to that in our set of patients where the same was 4.00±2.63mm Hg.26 Sihota et al. reported a diurnal variation of more than 6mm Hg in 85% chronic PACG and 90.7% of POAG eyes.27 Similar to the results from the present study, the diurnal IOP values found by Sihota and her colleagues were comparable between the POAG and PACG eyes. Also both the POAG and PACG groups seem to have no significant difference with respect to the fluctuation in IOP, as seen in these studies.
We attempted to identify the factors associated with the IOP fluctuations. A significant correlation was observed between baseline IOP and the IOP fluctuation. This finding implies that in patients with higher baseline IOPs, the diurnal IOP measurement requires greater consideration given that the findings may ultimately affect management of these patients. In accordance with Shah et al., no significant correlation was noted between IOP fluctuations and CCT.28 Similarly, Fogagnolo et al. have shown that 24h IOP fluctuation is independent of CCT variations regardless of the body positions in which they are measured.29 Additionally, neither age nor the number of topical antiglaucoma medications was found to contribute to IOP fluctuations.
The strengths of our study include a large number of subjects. Considering the reports of low repeatability of diurnal patterns of IOP, we used the same day measurements to compare the diurnal and office-hour fluctuations. The limitations of our study are the retrospective design and that we did not perform 24h IOP measurements for our patients. We also realize that although all the IOP measurements were obtained by a trained resident, there could have been some inter-observer bias in our results. Moodie et al. have reported that 24h phasing offers little advantage over daytime phasing in the identification of IOP fluctuations in patients with glaucoma.30 Our study did not aim to compare the daytime phasing and the 24h IOP measurements. Although the early morning peak, as reported by Zeimer et al., 31 may have been missed in our study, we believe that inclusion of the 24-h IOP monitoring would not have altered our conclusions. Ambulatory 24h continuous IOP monitoring can now be performed using a contact lens sensor (CLS; SENSIMED Triggerfish®, Sensimed AG, Lausanne, Switzerland). The device records circumferential shifts in the area of the corneoscleral junction; and these changes in corneal curvature and circumference are assumed to correspond to fluctuations in IOP. Initial studies have shown good safety and reproducibility of this device.32
Thus, we conclude that IOP measurements obtained during office hours may not be representative of the diurnal IOP measurements for patients with primary glaucoma. In glaucoma patients progressing despite “normal” IOP readings obtained during routine visits and particularly those with high baseline IOP, diurnal IOP measurements may reveal higher peaks or wider fluctuations.
Conflicts of interestThe authors have no conflicts of interest to declare.