To evaluate the potential influence and treatment-related changes of the corneal biomechanical properties (BMP) measured with the Ocular Response Analyzer (ORA, Reichert, Depew, NY) 15-days and 1-month after the initiation and cessation of corneal refractive therapy (CRT).
MethodsTwenty-four young healthy subjects (24.04±3.19 years) participated in two different experiments. In the first one (#1), twelve right eyes from 12 subjects who were fitted with CRT lenses were evaluated after 15 days and 1 month of lens wear. In the second trial (#2) 12 subjects who had been wearing CRT lenses for a period of 1 year were evaluated at 15 days and 1 month after treatment interruption.
ResultsThere was no statistically significant correlation between baseline BMP and absolute values of structural corneal parameters at 15 and 30 days treatment, and also when these variables were normalized according to the targeted refraction. In experiment #1, Corneal hysteresis (CH) reduction was observed over the time of treatment (p=0.019), but no significant differences were observed in the Corneal Resistance Factor (CRF) values. In addition, CRF reduction significantly correlated with spherical equivalent refraction (r=0.597; p=0.044), but no correlation was observed between CH or CRF reduction and the spherical component of the refraction. In experiment #2, no significant changes in CH or CRF were found initially after lens wear interruption, but a trend to increase was observed thereafter.
ConclusionCH decreases during onset of the CRT after 30 days of lens wear. Such changes seem to be reversible after cessation of contact lens wear following 1 year of treatment. Corneal biomechanics, however, do not predict the outcomes of CRT in clinical setting although with the data obtained some correlative tendencies were observed that may merit further investigation.
Evaluar la influencia potencial y los cambios relacionados con el tratamiento de las propiedades biomecánicas corneales, medidas con el Analizador de Respuesta Ocular (ORA, Reichert, Depew, NY), durante los 15 días y 1 mes posteriores al comienzo e interrupción de la terapia refractiva corneal.
MétodosVeinticuatro pacientes jóvenes y sanos (24,04±3,19 años) formaron parte de dos experimentos diferentes. En el primero (#1), se evaluaron doce ojos derechos pertenecientes a 12 pacientes, a los que se habían adaptado lentes CRT, durante los 15 días y 1 mes posteriores a la adaptación de dichas lentes. En el segundo ensayo (#2), se evaluó a 12 pacientes que habían utilizado lentes CRT durante 1 periodo de 1 año, durante los 15 días y 1 mes posteriores a la interrupción del tratamiento.
ResultadosNo se produjo una correlación significativa entre las propiedades biomecánicas corneales iniciales y los valores absolutos de los parámetros corneales estructurales durante los 15 y 30 días posteriores al tratamiento, ni tampoco cuando se normalizaron dichas variables, de acuerdo con la refracción objetivo. En el experimento #1, la reducción de la histéresis corneal (CH) fue estadisticamente significativa durante el tratamiento (p=0,019), aunque no se observó una reducción similar en el factor de resistencia corneal (CRF) y la CRT para dicho periodo de tiempo. Además, la reducción de los valores de CRF guardó una correlación significativa con el equivalente esférico de la refracción (r=0,597; p=0,044), aunque no se observó correlación alguna entre la reducción de CH o CRF y el componente esférico de la refracción. En el experimento #2, no se hallaron cambios significativos iniciales relativos a histéresis corneal (CH) o CRF tras la interrupción del tratamiento, aunque posteriormente se observó una tendencia al incremento.
ConclusiónLa histéresis corneal disminuye al inicio de la adaptación de las lentes CRT, durante los 30 días posteriores al tratamiento. Dichos cambios parecen reversibles al suprimir las lentes, tras 1 año de tratamiento. Sin embargo, la biomecánica corneal no predice los resultados de la CRT en el escenario clínico, aunque con los datos obtenidos se han observado ciertas tendencias correlativas que pueden merecer una investigación posterior.
Corneal refractive therapy (CRT), also known as orthokeratology, ortho-k or corneal reshaping has evolved in the last decade from a treatment marginally applied by few optometrists into a well accepted approach to provide a almost total independency from optical aids to myopic patients.1 The key for success relies in the predictability and simplicity of fitting systems2 as well as the repeatability, efficacy and safety of the results.3,4 Furthermore, CRT has gained increasing interest due the promising results obtained in the slowing of myopia progression in children when compared with spectacle wearers5 or contact lens wearers.6 Therefore there is a growing interest to understand the factors that influence the corneal response to CRT.
One of the factors that can potentially be involved in the corneal response to CRT is corneal rigidity. In the past, the lack of clinical instrumentation to measure the biomechanical properties (BMP) of the cornea, made it difficult to obtain conclusive results on this respect. With the development of the Ocular Response Analyzer (ORA), an instrument that provides the measurement of BMP,7 it has been possible to establish a link between values pertaining to corneal rigidity and responses to CRT.8 Different results have been found recently by Chen et al. after 15, 30 and 60min under closed-eye conditions and overnight trial,9 suggesting that different conditions and times of wear can be relevant for the potential involvement of the BMP of the cornea in the response to CRT. These authors also found a slight but statistically significant reduction in CRF measurements after the overnight trial.11 However, the same reduction was not observed in CH parameters. Authors concluded, however, that CH response would most likely change after a longer time of treatment.
The role of the BMP of the cornea on the response to CRT is a quite recent study field and relatively unknown, with many questions remaining unanswered. The objectives in this study are to try to address some of these questions: (1) the correlation of CH/CRF with changes in structural corneal parameters (absolute and normalized to refractive error) after initial CRT and after cessation following 1 year of treatment; (2) BMP of the cornea at initiation and cessation of CRT; (3) CH and CRF as predictors of CRT outcomes; and (4) reversibility of BMP after cessation of CRT. This is the first study addressing the changes and potential role of BMP during CRT treatment in a clinical setting.
MethodsWe designed a longitudinal, single-center study of one month duration. The study was approved by the Ethics Committee of the Hospital Carlos III and the study protocol adhered to the tenets of the Declaration of Helsinki. The participants were students of the Complutense University of Madrid; informed consent was obtained from the subjects after explanation of the nature and possible consequences of the study. Subjects were selected according to a set of inclusion criteria as well as an interest in trying the treatment under study. The inclusion criteria were: men or women aged 18–30 years, ocular refraction of −0.50 to −4.5 days of myopia with astigmatism no greater than 1.00. Subjects were excluded if they used or had in the past used gas permeable contact lenses. Hydrophilic lens wearers were instructed to stop wearing their contact lenses 4 weeks prior to the start of the study. Subjects were excluded if they: were pregnant, had any systemic or eye disease, a history of eye surgery, pupils larger than 5.5mm in photopic conditions, or were participating in another clinical trial.
Paragon CRT lenses were fitted to 12 patients in each experiment. Fitting approach has been previously described.2 Base curve radius (BCR), return zone depth (RZD) and landing zone angle (LZA) for the first diagnostic lens were derived from nomograms in the form of sliding tables produced by the manufacturer. Fitting evaluation was based on fluorescein assessment, lens centration and movement followed by over-refraction. The parameters of RZD and LZA were manipulated until a satisfactory fluoresce in fitting pattern was achieved with excellent centration, light apical bearing over a central 4-mm zone, a paracentral tear reservoir free of air bubbles, tangent peripheral zone and adequate axial edge clearance with an over-refraction between plano and +0.50 diopters.
The changes in CH and CRF as well as intraocular pressure equivalent to Goldman and compensated (IOPg and IOPcc, respectivelly) were obtained using the ORA (Reichert Inc, Depew, NY, USA). The principle and acquisition process have been fully described in the literature.7–10 Data were the result of three repeated measures taken at each visit along the follow-up periods. All measurements were performed in the same office and at the same time of day within a 2-h margin. In each follow-up session, the same clinical procedures were conducted in the same order by one optometrist.
The investigation consisted of two different experiments. In the first one (Experiment #1) twelve right eyes from twelve subjects undergoing CRT for the first time were observed at baseline and at 15 and 30 days after the beginning of the wearing period. In the second one (Experiment #2), twelve right eyes from twelve different subjects undergoing CRT treatment for 12 months were asked to interrupt their treatment for 1 month and BMP as well as other clinical measures were obtained before interruption, and after 15 and 30 days. Central corneal thickness (CCT) was measured with Oculus Pentacam (Oculus Optikgeräte GmbH, Wetzlar, Germany) and corneal topography was measured with Wavelight Allegro Topolyzer (WaveLight Laser Technologies AG, Erlangen, Germany). The repeatability of these instruments has been described previously.11,12
Statistical analysis was conducted using the statistical package SPSS version 14.0 (SPSS Inc, Chicago, IL). Baseline values of BMP of the cornea (independent variables) were correlated with the changes in the corneal curvature, eccentricity and thickness changes (dependent variables) at each follow-up time (ti) 15 and 30 days of wear or after cessation of lens wear in experiment #1 and experiment #2, respectively. Two different approaches were followed to calculate the dependent variables; the first one correlated the changes in each variable at a time ti=15 or 30 days in this study, according to equation 1 (ΔVariableabs), and the second one considered a normalized value (ΔVariablenorm) according to the targeted refractive error to be corrected according to Eq. (2).
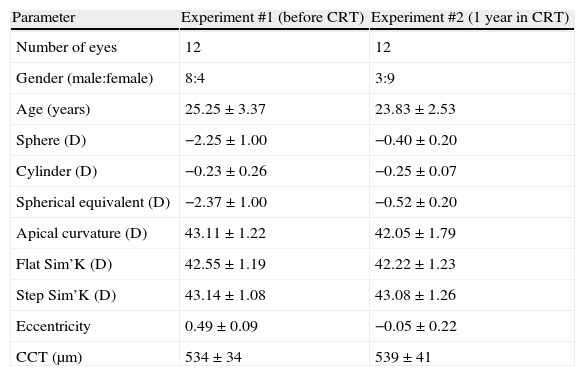
The time course of changes in CH, CRF as well as IOPg and IOPcc was plotted against time after lens fitting or after lens wear cessation to explore their changes using 1-factor repeated measures analysis of variance (RMANOVA) and p values adjusted for multiple comparisons. Kruskal–Wallis test was used when the data were not normally distributed. Paired t-tests were conducted when no significant differences were detected in above test. Normal distribution of variables was assessed by a Kolmogorov–Smirnov normality test. The level of statistical significance was set at p=0.05.ResultsTable 1 shows the demographic data of patients at baseline in experiment #1 and after 1 year of CRT treatment in experiment #2. Table 2 presents corneal biomechanical values obtained over time.
Demographic data of patients at baseline in experiment #1 and after 1 year of CRT treatment in experiment #2 except for refractive data which reflects baseline values.
| Parameter | Experiment #1 (before CRT) | Experiment #2 (1 year in CRT) |
| Number of eyes | 12 | 12 |
| Gender (male:female) | 8:4 | 3:9 |
| Age (years) | 25.25±3.37 | 23.83±2.53 |
| Sphere (D) | −2.25±1.00 | −0.40±0.20 |
| Cylinder (D) | −0.23±0.26 | −0.25±0.07 |
| Spherical equivalent (D) | −2.37±1.00 | −0.52±0.20 |
| Apical curvature (D) | 43.11±1.22 | 42.05±1.79 |
| Flat Sim’K (D) | 42.55±1.19 | 42.22±1.23 |
| Step Sim’K (D) | 43.14±1.08 | 43.08±1.26 |
| Eccentricity | 0.49±0.09 | −0.05±0.22 |
| CCT (μm) | 534±34 | 539±41 |
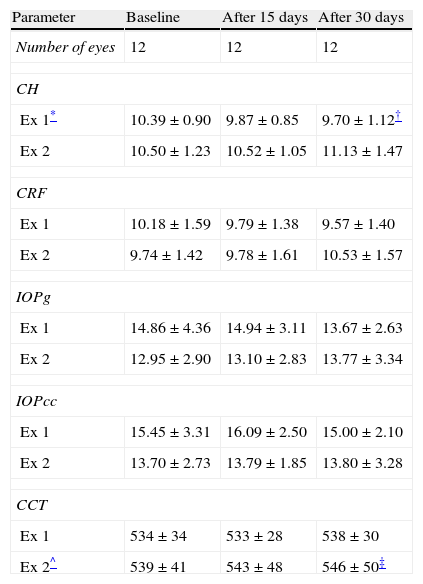
Corneal biomechanical properties and central corneal thickness at each follow up time.
| Parameter | Baseline | After 15 days | After 30 days |
| Number of eyes | 12 | 12 | 12 |
| CH | |||
| Ex 1* | 10.39±0.90 | 9.87±0.85 | 9.70±1.12† |
| Ex 2 | 10.50±1.23 | 10.52±1.05 | 11.13±1.47 |
| CRF | |||
| Ex 1 | 10.18±1.59 | 9.79±1.38 | 9.57±1.40 |
| Ex 2 | 9.74±1.42 | 9.78±1.61 | 10.53±1.57 |
| IOPg | |||
| Ex 1 | 14.86±4.36 | 14.94±3.11 | 13.67±2.63 |
| Ex 2 | 12.95±2.90 | 13.10±2.83 | 13.77±3.34 |
| IOPcc | |||
| Ex 1 | 15.45±3.31 | 16.09±2.50 | 15.00±2.10 |
| Ex 2 | 13.70±2.73 | 13.79±1.85 | 13.80±3.28 |
| CCT | |||
| Ex 1 | 534±34 | 533±28 | 538±30 |
| Ex 2^ | 539±41 | 543±48 | 546±50‡ |
Ex, experiment.
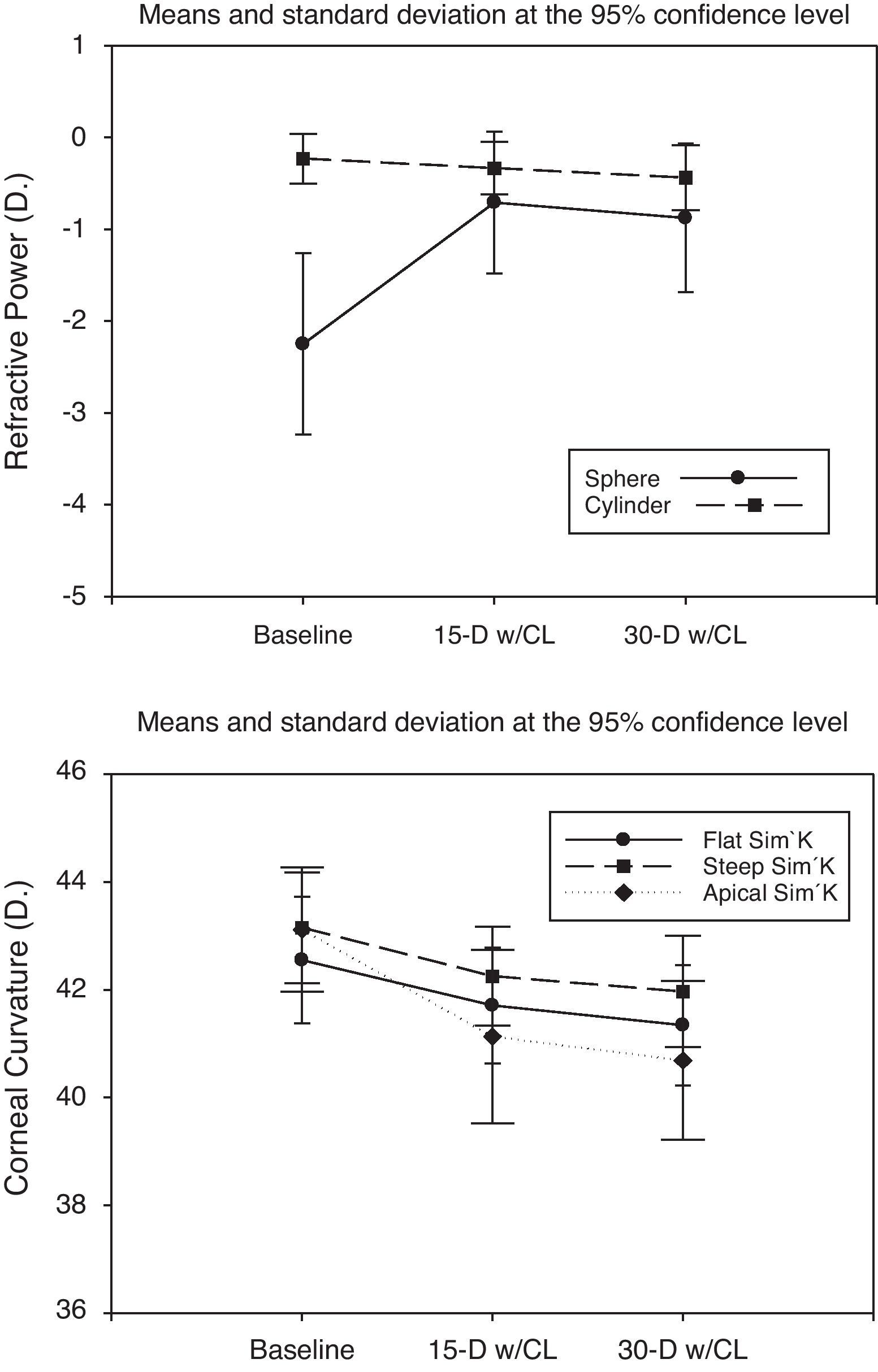
There was a statistically significant change in sphere, spherical equivalent refraction, flat and steep sim-k, apical curvature and eccentricity (p<0.05) during the first month of CRT treatment. Fig. 1 displays the changes in sphere, cylinder and corneal curvature parameters.
Temporal changes of refractive data (top) as sphere and cylinder and corneal parameters (bottom) as apical curvature, flat simulated keratometry (Flat Sim’K) and steep simulated keratometry (Steep Sim’K). Legend: 15 and 30 days after lens fitting (15Dw/CL and 30Dw/CL, respectively).
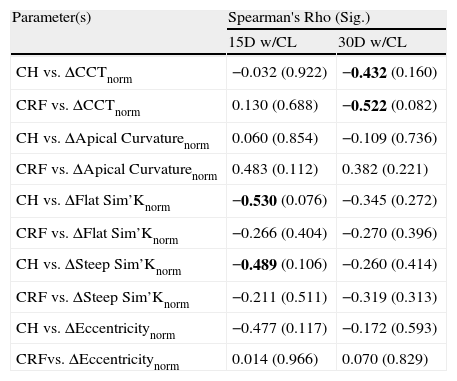
Correlation analysis did not show any significant relationship between the changes in corneal curvature, topography or thickness after 15 days or 30 days of treatment and the BMP of the cornea at baseline (Spearman's Rho<0.400, p>0.05) when absolute change values (ΔVariableabs) were considered. When changes in each of the test variables were normalized according to the target refraction (ΔVariablenorm), the correlations increased, several of them showing Spearman's Rho>0.400), but continued to be non-statistically significant (p>0.05). Table 3 shows the results of the correlation analysis between corneal BMP and corneal response in normalized terms (ΔVariablenorm) to CRT at 15 and 30 days.
Correlation analysis for experiment #1 between BMP and corneal parameters considering the values of changes normalized according to the target refractive error (Variablenorm) after 15 days with contact lenses (15Dw/CL) and 30 days with contact lenses (30Dw/CL).
| Parameter(s) | Spearman's Rho (Sig.) | |
| 15Dw/CL | 30Dw/CL | |
| CH vs. ΔCCTnorm | −0.032 (0.922) | −0.432 (0.160) |
| CRF vs. ΔCCTnorm | 0.130 (0.688) | −0.522 (0.082) |
| CH vs. ΔApical Curvaturenorm | 0.060 (0.854) | −0.109 (0.736) |
| CRF vs. ΔApical Curvaturenorm | 0.483 (0.112) | 0.382 (0.221) |
| CH vs. ΔFlat Sim’Knorm | −0.530 (0.076) | −0.345 (0.272) |
| CRF vs. ΔFlat Sim’Knorm | −0.266 (0.404) | −0.270 (0.396) |
| CH vs. ΔSteep Sim’Knorm | −0.489 (0.106) | −0.260 (0.414) |
| CRF vs. ΔSteep Sim’Knorm | −0.211 (0.511) | −0.319 (0.313) |
| CH vs. ΔEccentricitynorm | −0.477 (0.117) | −0.172 (0.593) |
| CRFvs. ΔEccentricitynorm | 0.014 (0.966) | 0.070 (0.829) |
n=12; correlation coefficients above 0.400 highlighted in bold; p-value in parentheses.
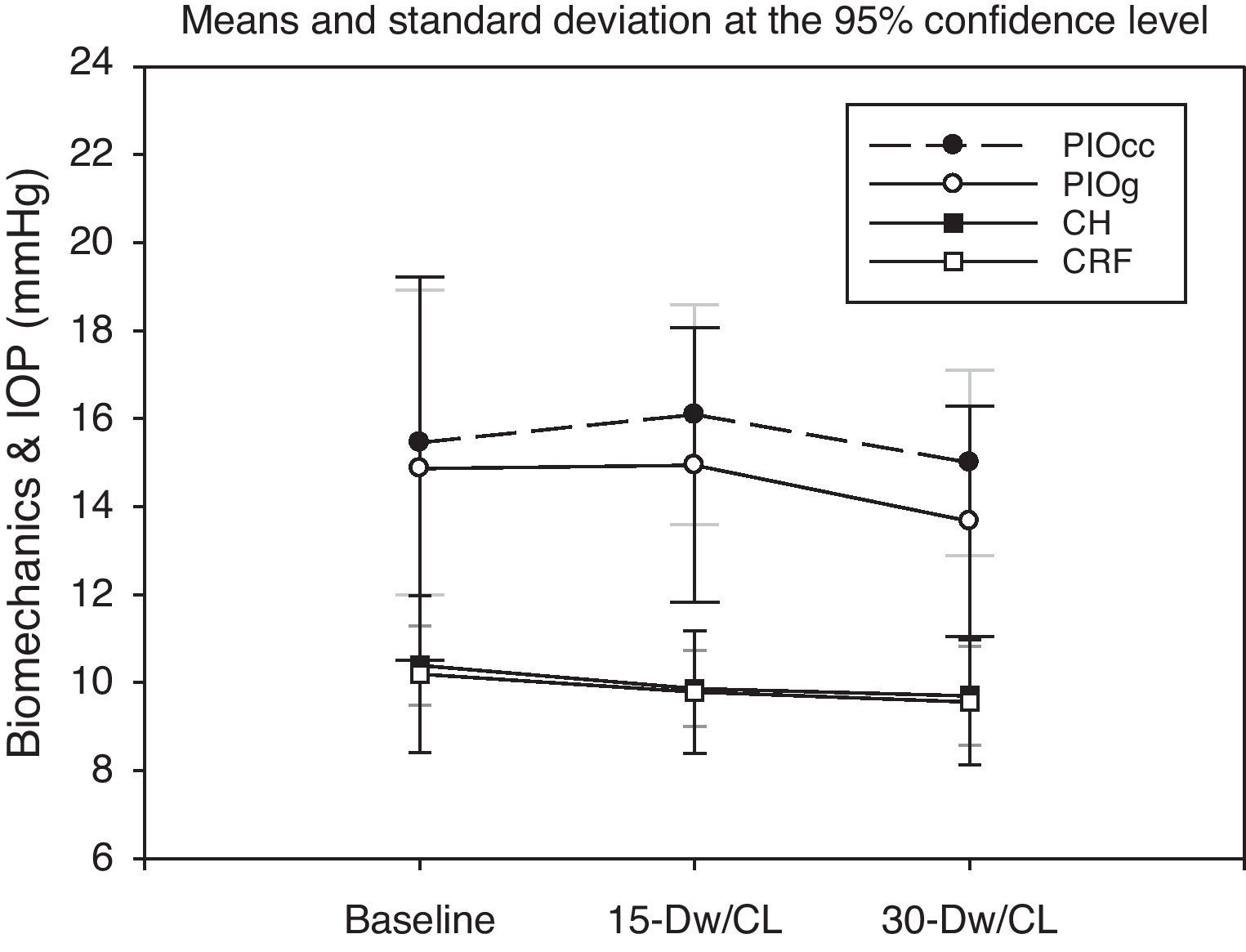
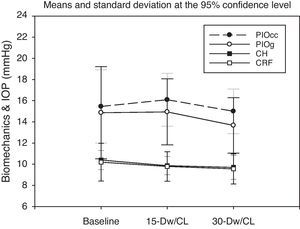
RMANOVA showed a significant decrease in CH (p=0.019) when analyzed for the whole study period. Post hoc Bonferroni test revealed a significant reduction in CH after 30 days (p=0.015, Table 2). However, there were not statistically significant in the CRF (p=0.08) or intraocular pressure (p>0.05). But CRF showed a trend to decrease as did CH. Fig. 2 shows the temporal changes in biomechanical corneal properties and IOP values.
Changes in corneal hysteresis (CH), corneal resistance factor (CRF), intraocular pressure equivalent to Goldmann (IOPg) and intraocular pressure compensated for corneal BMP (IOPcc) during the onset of the CRT treatment in Experiment #1. Legend: 15 and 30 days after lens fitting, respectively.
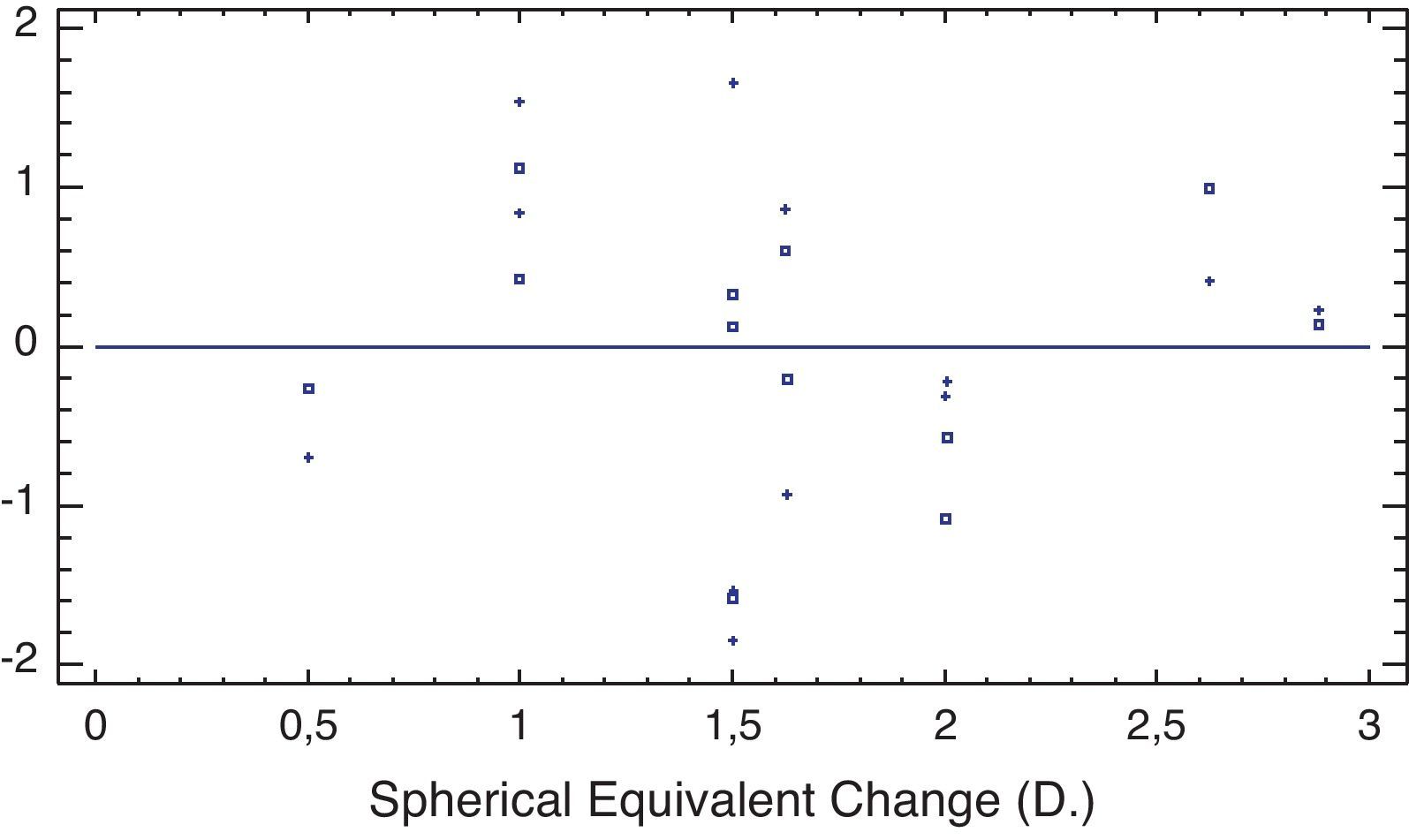
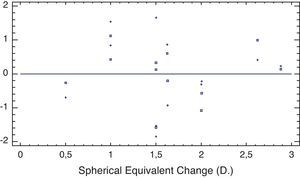
There was also a statistically significant correlation between the reduction in CRF after 30 days of treatment and the spherical equivalent refraction of the patient (Spearman's Rho=0.597, p=0.044), while the correlation with the spherical refraction was not significant (Spearman's Rho=0.566, p=0.055), nor was the correlation between the reduction in CH value after 30 days of treatment and the spherical equivalent (Spearman's Rho=0.285, p=0.783) or the spherical component of the refraction (Spearman's Rho 0.47, p=0.111). The relation between changes of both variables can be seen in Fig. 4. No correlations were present with the reduction in either biomechanical parameter after 15 days of treatment.
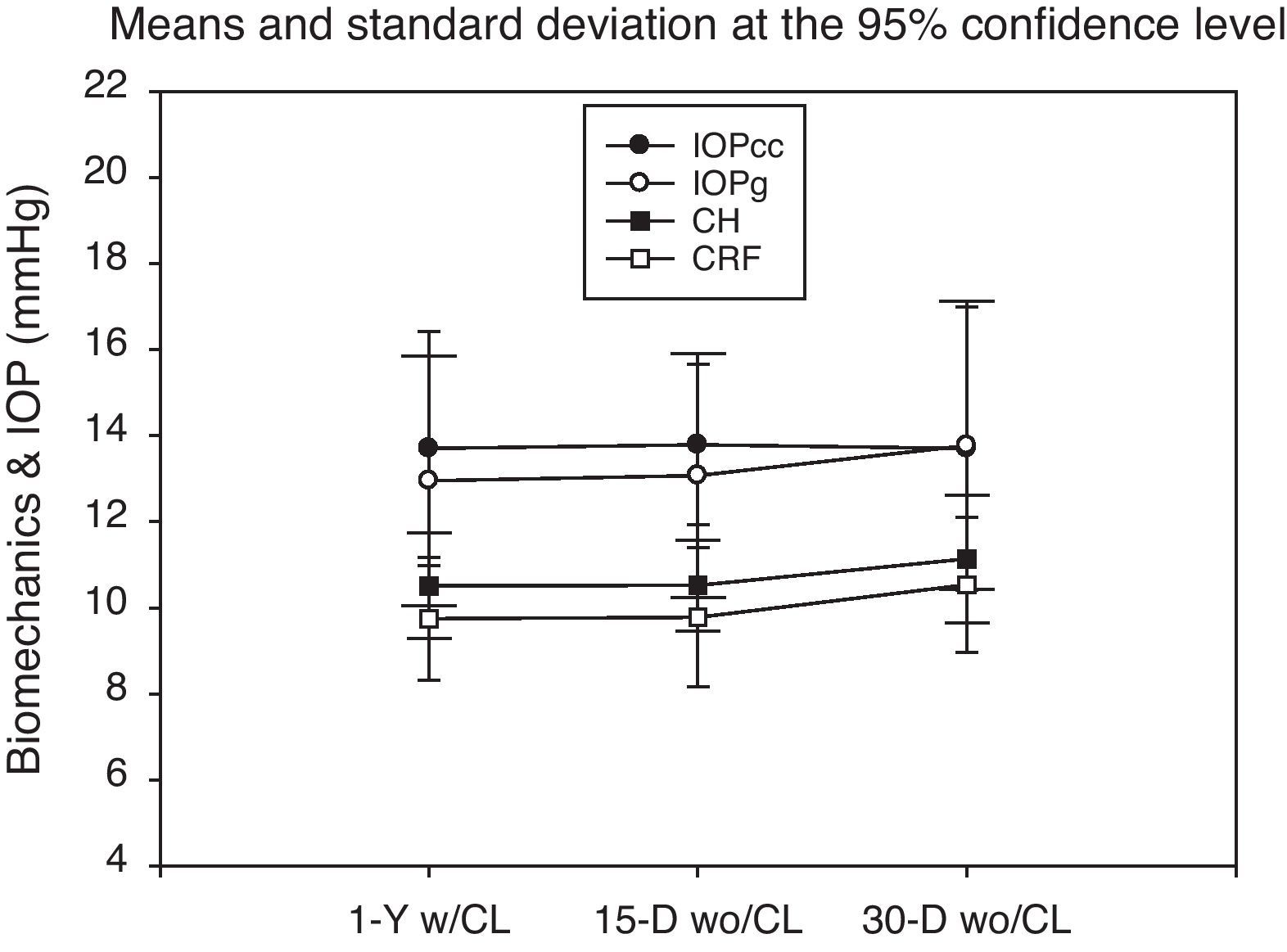
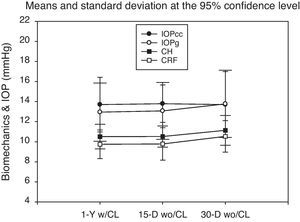
Experiment #2In experiment #2 there was no statistically significant change in the BMP of the cornea after lens wear cessation. Despite this, there was a slight trend for CH and CRF to increase as shown in Table 2 and Fig. 3.
Changes in corneal hysteresis (CH), corneal resistance factor (CRF), intraocular pressure equivalent to Goldmann (IOPg) and intraocular pressure compensated for corneal BMP (IOPcc) after cessation of CRT treatment in Experiment #2. Legend: 1-Yw/CL (1 year of treatment), 15D and 30D (days) after lens wear cessation, respectively.
Biomechanical properties changes as a function of spherical equivalent (SE) change 30 days after the onset of the CRT treatment in Experiment #1. Legend: Corneal Hysteresis (□, mmHg) and Corneal Resistance Factor (+, mmHg). ΔCH vs. ΔSE: Spearman's Rho=0.526, p=0.08. ΔCRF vs. ΔSE: Spearman's Rho=0.065, p=0.834.
Correlation analysis showed that there was no statistically significant relationship between CH or CRF with the absolute changes in corneal parameters at 15 or 30 days after lens wear cessation (Spearman's Rho<0.300; p>0.05). When normalized values of changes in corneal parameters were used, only recovery of CCT at 15 days showed a noteworthy correlation although it was not significant (Spearman's Rho=0.453; p=0.139).
Contrary to experiment #1, no statistically significant correlations were present between changes in CH or CRF after lens wear cessation and the target spherical or spherical equivalent refraction.
DiscussionThis study is the first one to document changes in BMP of the cornea measured with ORA after commencement and cessation of CRT. The results obtained demonstrated a statistically significant decrease in CH parameter during onset of the CRT after 30 days of lens wear. Nonetheless, when attempted to correlate the changes in corneal physical parameters according to the targeted treatment no statistical significance was found.
One possible limitation of the study is the limited sample size in both experiments. This could be the reason why changes in BMP in subjects after cessation of CRT were not statistically significant. Nonetheless, reduction in CH reduction was statistically significant. Moreover, results of the study warrant further investigations on this field in order to fully understand the course of changes in corneal properties during CRT.
From an anatomical perspective, corneal BMP changes observed in the study apparently do not compromise the integrity of the cornea or increase the risk of keratectassia. Comparative study show that BMP changes in CRT are not as relevant as BMP changes observed after refractive surgery.6–10,13 Other studies on LASIK demonstrate a significant decrease in CH and CRF post-operatively.14,15 Furthermore, from this preliminary data it may be assumed that changes in the BMP of the cornea produced by CRT treatment most likely revert after the cessation of treatment even after 1 full year of treatment.
The reasons behind the changes observed here are somewhat unclear. They are in agreement with previous reports by Chen et al.9 who showed that the CRF changes were related to the changes of corneal curvature. However, the reduction of CRF did not follow the degree of flattening of simulated keratometry. One possible explanation is the changes in the front surface corneal curvature because ORA uses this surface to measure the two aplannation points from which BMP and IOP values are derived. Most likely this may be the factor since a recent study that evaluated the correlation of CH and CRF values with corneal curvature demonstrated that flatter corneas related more to CH and CRF readings.15 However, data from this study were collected in Chinese children and it is known that BMP change with age.16 Conversely, Franco and Lira17 did not find correlation between the parameters measured with the ORA and central corneal radius. They found that CRF had a stronger correlation with the CCT than the CH, which may indicate that the CCT plays a more important role in the corneal elastic properties as suggested by Touboul et al.18 In view of this, the most plausible explanation for the trend in reduction of BMP values is the collective change of both parameters.
A tendency for BMP values to increase after lens wear cessation is also observed in the study. The opposite mechanisms of corneal curvature recovery (steepening) and CCT recovery after lens wear interruption could justify such result at least in part. These results are in agreement with a previous study19 that found a significant increase in CRF of 0.6mmHg after lens removal. Despite this, we cannot discard that other tissue-related mechanisms could be involved in the changes observed such as keratocyte density changes,20 epithelial alterations21 and the thinning of the Bowman layer and subbasal nerve plexus found on CRT wear described in previous CRT studies.21,22
The BMP variability found between individuals in our sample are in agreement with study of Radhakrishnan et al.23 who found that refractive error and CRF presented a weak correlation with spherical equivalent, but not CH as it happened in this study. In this sense, it seems to be of significance that there is a reduction in BMP. Particularly in CH because this biomechanical factor is responsible of the corneal elasticity and therefore of the flattening on the corneal surface in response to the CRT wear in those cases where the treatment is successful.
In summary, from the preliminary results reported here, it seems that subtle changes in BMP can be detected as shown in previous reports, and that these changes seem to be reversible as the treatment is discontinued. Remarkable questions still remain, particularly regarding the (1) long-term recovery and stability of corneal BMPs after longer periods of wear and (2) other potentially involved biological factors such as changes in corneal histology or metabolic function beyond corneal curvature changes as the etiological factors.
Conflict of interestThe authors have no conflicts of interest to declare.