Detection of anisocoria in those with dark irides is difficult, and failure to detect anisocoria can have dire consequences. Whether infrared pupillometry and gross measurement would yield different prevalence rates for anisocoria in those with dark irides is unknown. We compared the frequency of anisocoria in healthy adults with dark irides assessed with mm ruler versus infrared pupillometry.
MethodsPupil diameters in light (L) and dark (D) conditions were obtained to identify anisocoria in 59 human subjects with dark irides using two techniques. To avoid bias, gross measurements (S) with ruler were taken first. Pupils were imaged under infrared illumination mounted in a spectacle frame with mm tape attached. Adobe Photoshop was used to measure pupil sizes on the digital images (O).
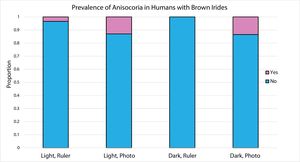
ResultsProportions of anisocoria by group were SL .034, OL .130, SD 0.00, OD .135. Fisher's exact test showed that anisocoria in dim light was more frequent with the infrared photo technique. Exact binomial probability testing showed that the anisocoria in SL and SD conditions was not different from an expected proportion of 5%; whereas anisocoria in OL condition was not different from an expected proportion of 20%, and anisocoria in OD condition was not different from expected proportions of 10, 15, and 20%.
ConclusionsIn people with dark irides, ruler measurements of pupil size underestimate the frequency of anisoria in dim lighting conditions compared to the use of infrared pupillometry. Whether detection rates of pathologic anisocoria differ with measurement technique remain to be explored.
La detección de anisocoria en los sujetos con iris oscuros es difícil, y la falta de detección puede tener consecuencias nefastas. Se desconoce si la pupilometría de infrarrojos y la medición en bruto arrojarían diferentes tasas de prevalencia de anisocoria en los sujetos con iris oscuros. Comparamos la frecuencia de anisocoria en adultos sanos con iris oscuros, valorados con regla en mm versus pupilometría de infrarrojos.
MétodosSe obtuvieron los diámetros de la pupila en los iris claros (L) y oscuros (D) para identificar la anisocoria en 59 sujetos con iris oscuros, utilizando dos técnicas. Para evitar sesgos, se realizaron en primer lugar las medidas brutas (S) con la regla. Las pupilas se fotografiaron mediante un sistema de iluminación de infrarrojos montado en gafas con cinta en mm anexa. Se utilizó Adobe Photoshop para medir los tamaños de las pupilas en las imágenes digitales (O).
ResultadosLas proporciones de anisocoria por grupo fueron SL 0,034, OL 0,130, SD 0, OD 0,135. La prueba exacta de Fisher reflejó que la anisocoria con luz tenue era más frecuente con la técnica de fotografías de infrarrojos. La prueba de probabilidad binómica exacta reflejó que la anisocoria en las situaciones de SL y SD no era diferente a la proporción prevista del 5%, mientras que la anisocoria en la situación OL no era diferente a la proporción prevista del 20%, y la anisocoria en la situación OD no era diferente a las proporciones previstas del 10, 15, y 20%.
ConclusionesEn las personas con iris oscuros, las mediciones del tamaño de la pupila realizadas con regla subestimaron la frecuencia de anisocoria con luz tenue, en comparación con el uso de pupilometría de infrarrojos. Queda por explorar si las tasas de detección de anisocoria patológica difieren con la técnica de medición.
Recognition of anisocoria and observation of its variation under normal vs. dim room illumination can help differentiate between benign essential anisocoria (congenital) and acquired anisocoria related to a potentially serious health condition.1 Identification of benign essential anisocoria (i.e., “physiological anisocoria”, reportedly present in 5–20% of the population2–8) is necessary to avoid confusion and to mitigate an unnecessary and potentially expensive diagnostic work-up in the context of new visual symptoms.
Gross assessment of pupil size and shape with a ruler in both normal and dim room illumination continues to be the primary method taught to clinical students and performed in general practice; however, gross assessment may be an insensitive technique for assessing pupils, especially in dim illumination and in patients with brown irides. Images captured with infrared pupillometers have greater contrast between the iris and pupil, enabling better detection of pupil size and shape in those with dark irides, but these instruments cost considerably more than a mm ruler and are not yet widely used in routine clinical practice. Whether infrared pupillometry and gross measurement would yield different prevalence rates for anisocoria in those with dark irides is unknown.
The purpose of this study is to determine whether the frequency of anisocoria in normal, healthy adult subjects with brown irides, assessed in both bright and dim illumination, differs across two measurement techniques: (1) photography with binocular infrared illumination,9 versus (2) gross measurement with mm ruler and additional dim illumination below the chin (as needed).
MethodsThe experimental protocol complied with the tenets of the Declaration of Helsinki and received approval by the Institutional Review Board of the Southern College of Optometry. Informed consent was obtained from all subjects prior to their participation.
SubjectsParticipating subjects included 59 healthy adults, aged 18–39 years, all having brown irides. (We did not differentiate between shades of brown eyes, but the brown color had to be definite; i.e., not “hazel” or “yellow-brown”.) Exclusion criteria included history of blunt trauma to the eye, history of anterior uveitis, presence of any iris abnormality, history of any type of glaucoma other than primary open angle, history of ocular surgery, and medications known to affect pupil size or reactivity. Subjects also excluded if any corneal opacities were visible on gross inspection on either eye that could inhibit visualization of any part of the iris/pupil border.
ProceduresThe magnitude of anisocoria was determined from the difference in the pupil diameters between the two eyes. Pupil diameters in the horizontal and vertical directions were obtained for each subject by a single examiner using two techniques, which are described below. Because the increment scale for measuring pupil size differed for the two methods (0.5mm for the gross measurement vs. 0.25mm for the photograph), anisocoria for this study was defined as a pupil size difference ≥0.5mm.
Gross measurementThe examiner qualitatively determined by observation, with no supplemental magnification devices, whether anisocoria could be detected in normal room illumination. Subsequently, the examiner took pupil measurements of both eyes in normal room illumination (680lux, measured with Digital Light Meter LX1330B, Dr. Meter, range 0–200,000lux) using the “half moons” on a standard optometric millimeter ruler (Fig. 1). The room lights were turned off and, after about 10s, the examiner again observed and measured the pupil diameters. Additional indirect illumination with a transilluminator or the stand light was used in both room light conditions if needed, with care taken to evenly illuminate the two eyes. The magnitude of anisocoria was determined separately for each of two sets of measurements, and the mean of the two anisocoria measurements was used in the statistical analysis. This method of determining the magnitude of anisocoria from two separate sets of measurements (rather than using the means of the left and right pupil diameters to determine the magnitude of the anisocoria) was done so that the technique would be more comparable to the photographic technique, in which the magnitude of the anisocoria could be observed and recorded from each photograph.
Ruler used for gross assessment of pupil size. The numbers adjacent to the black “half moons” indicate the pupil diameter in millimeters. Pupils of size determined to be between two of the “half moons” were assigned a size half way between the two. For example, if the pupil size was between that of number 4 and number 5, the size was assigned a value of 4.5mm.
An inexpensive illumination device was constructed using six infrared emitting diodes (850nm, 1100mW/sr) attached to a spectacle frame and connected to a 9-volt battery as described by Shazly et al.9 Adhesive metric ruler tape was attached along the top and lateral sides of the frame so that a measuring device was included in each photograph (Fig. 2). Using a digital camera sensitive to infrared light (Sony Cybershot) and instructing the subject to look across the room past the camera, each subject's pupils were photographed from a distance of 40–50cm in normal room illumination (680lux) and after approximately 10s in dim illumination (0lux). At least two photographs were taken; additional photographs were taken if the subject blinked or the quality of the photographs was otherwise poor. The red filter and the line drawing tool of the digital photo-editing software (Adobe Photoshop CS5 version 12.1) were used to enhance the contrast at the pupil border and delineate the diameter of the pupil, which was then matched to the millimeter scale on the ruler in the photograph. From each photograph the magnitude of the anisocoria was assessed, and the mean anisocoria across two photographs was used for data analysis.
Custom-build infrared light source used for digital pupillometry (Shazly et al.9). The top photo was taken in normal room light with the infrared LEDs turned off. The bottom photo was taken with room lights off and the infrared LEDs turned on.
To minimize bias that could have been introduced by seeing the photographs first, all subjects underwent gross measurement of their pupils with the millimeter ruler before photographs were taken. Additionally, although the gross measurements with the millimeter ruler were recorded at the time of collection, the pupil diameters from the photographs were not recorded at the time the photographs were taken. Instead, the measurements from the photographs of an individual subject were taken hours to days after the subject's data collection session, as time to work with the software became available. The gross pupil measurements were not referenced when the photographs were evaluated.
ResultsDescriptive and comparative statistics were calculated using R, version 3.5.1.
The mean age of the subjects was 24.1±2.7 years. Gender frequency was unequal within the sample, with 17 males and 42 females. The distributions of anisocoria magnitude were not normal for either the horizontal or vertical direction for either light condition or measurement method used (Shapiro–Wilk, p>.05 for all light conditions and measurement methods). Additionally, since the increment scale for measuring pupil size differed for the two methods used in our study (0.5mm for the gross measurement vs. 0.25mm for the photograph), a comparison of mean magnitude of anisocoria across the two methods was not done.
To determine whether the proportion of subjects with anisocoria ≥0.5mm differed based on the method of assessment, McNemar's test of within-subjects proportions was used to compare the gross measurement technique with the infrared photograph technique. For horizontal anisocoria assessed under photopic conditions, the unsigned difference in proportions was 0.4425 (two-tailed p<.000001, odds ratio=8.14, 95% CI of odds ratio 3.7–17.9). For vertical anisocoria assessed under photopic conditions, the unsigned difference in proportions was 0.469 (two-tailed p<.000001, odds ratio=14.25, 95% CI of odds ratio 5.2–39.3). For horizontal anisocoria assessed under scotopic conditions, the unsigned difference in proportions was 0.4602 (two-tailed p<.000001, odds ratio=8.43, 95% CI of odds ratio 3.9–18.5). For vertical anisocoria assessed under scotopic conditions, the unsigned difference in proportions was .5045 (two-tailed p<.000001, odds ratio=19.7, 95% CI of odds ratio 6.2–62.7).
The frequency of anisocoria ≥0.5mm for each test condition is shown in Fig. 3. For statistical comparison, the frequency data were cross-categorized and Fisher's exact probability test was used to determine whether anisocoria was more likely to occur in one of the two conditions compared. Table 1 shows the results of this analysis. Odds ratios could not be calculated for the comparison conditions that included the ruler measurement in dim illumination because zero cases of anisocoria were identified in that condition. Of the four comparisons listed in Table 1, Fisher's exact probability test indicates that anisocoria in dim illumination was more likely to be identified by the photograph assessment than by the ruler measurement. For the other three comparisons, anisocoria was equally likely to be detected in the two conditions compared.
Analysis of cross-categorized frequencies of anisocoria.
| Conditions compared | Odds ratio | 0.95 confidence interval for odds ratio | Fisher's exact probability test, 2-tailed p value |
|---|---|---|---|
| Photo light vs. Ruler light | .2356 | .0467, 1.1884 | .084 |
| Photo dark vs. Ruler dark | NA | NA | .005 |
| Ruler light vs. Ruler dark | NA | NA | .496 |
| Photo light vs. Photo dark | 1 | .3253, 3.074 | 1.0 |
To compare the observed proportions of anisocoria ≥0.5mm with the previously reported prevalence rates of between 5 and 20%, we calculated the cumulative binomial probability of finding the exact number or fewer observed cases of anisocoria ≥0.5 when the expected proportions were either 5, 10, 15, or 20%. The results for horizontal anisocoria are shown in Table 2. When measured with a ruler in the light, the observed frequency of anisocoria ≥0.5mm (3.4%) was consistent with prevalence rates of 5 and 10%. When measured with a photograph taken in the light, the observed frequency of anisocoria ≥0.5mm (13.0%) was consistent with a prevalence of 10%, 15%, and 20%. When measured with a ruler in the dark, the observed frequency of anisocoria ≥0.5mm (0%) was consistent with a prevalence of 5%. When measured with a photograph taken in the dark, the observed frequency of anisocoria ≥0.5mm (13.4%) was consistent with a prevalence of 10%, 15%, and 20%. Thus, when measured with a ruler, the observed frequency of anisocoria in these subjects with brown irides was consistent with a prevalence of 5–10%, whereas when measured from a photograph, the observed frequency of anisocoria was consistent with a prevalence of 10–20%. The results for vertical anisocoria were similar (data not shown).
Comparison of observed frequencies of anisocoria with previously reported rates.
| Test condition | Expected proportiona | Observed proportion | Cumulative probability of finding the same or fewer number of observed cases |
|---|---|---|---|
| Ruler, Light | 0.05 | 0.034 | 0.429 |
| 0.10 | 0.057 | ||
| 0.15 | 0.004 | ||
| 0.20 | 0.0002 | ||
| Photo, Light | 0.05 | 0.130 | 0.99 |
| 0.10 | 0.707 | ||
| 0.15 | 0.427 | ||
| 0.20 | 0.13 | ||
| Ruler, Dark | 0.05 | 0 | 0.052 |
| 0.10 | 0.002 | ||
| 0.15 | <0.0001 | ||
| 0.20 | <0.0001 | ||
| Photo, Dark | 0.05 | 0.135 | 0.986 |
| 0.10 | 0.856 | ||
| 0.15 | 0.472 | ||
| 0.20 | 0.157 | ||
Examination of the data from individual subjects showed that no subject who demonstrated ≥0.5mm aniscoria in the light also demonstrated ≥0.5mm anisocoria in the dark. This observation held for measurements taken with each technique. We found this observation of particular interest, since (by photograph method) the frequency of aniscoria ≥0.5mm in normal room illumination was similar to the frequency of anisocoria ≥0.5mm in dim illumination (13.0 vs. 13.4%).
DiscussionThe main finding of this study was that the frequency of anisocoria ≥0.5mm measured in those with brown irides was significantly different when assessed with gross measurement and a ruler compared to measurement from photographs captured with infrared light. This difference was observed for pupil assessment both in normal room illumination and in the dark. The fact that the examiner in this study was unable to detect anisocoria ≥0.5mm in any of the subjects by gross assessment with a ruler in the dark illustrates the lack of sensitivity of this technique when used with brown eyes in dim illumination.
The frequency of physiological anisocoria depends on how anisocoria is defined. Lam et al., found in their study of 128 subjects that anisocoria of greater than or equal to 0.4mm was present in 19% of their subjects at any given time. They noted that the prevalence of anisocoria changes dramatically with changes in the value used as the cut-off point for its definition, dropping to 9% prevalence in their subjects at any given time if the cut-off value is changed to 0.5mm or greater. We chose 0.5mm as the cut-off value for defining anisocoria for this study because of the type of ruler used for the measurement (the half-moons were in 1mm increments; a pupil whose diameter measured between two of the half-moons was assigned the diameter of the smaller half-moon plus 0.5mm), and because common clinical practice is to document pupil size in 0.5mm increments. Lam et al. also stated that iris color was not a significant factor in the prevalence of anisocoria; however, no data on iris color were presented in their paper.
For a given definition of anisocoria, the frequency of physiological anisocoria also varies with test conditions. In their study on variations in anisocoria across different levels of illumination and accommodative demand, Ettinger et al. found that the average magnitude and variability of anisocoria tended to be greater in dark conditions.4 Ettinger et al. also noted that, “conditions that produce even modest changes in variability can cause dramatic changes in the probability of observing anisocoria.”4 Their study did not assess the relationship between iris color and frequency of anisocoria. The present study only assessed anisocoria in two illumination conditions, which were well-controlled by using the same examination area for each subject. While some variability may have been introduced in the gross measurements with the ruler when extra light was needed to visualize the pupils, the fact that no subjects were identified as having anisocoria in dim light by this technique indicates that the extra light source did not contribute variability to the measurement. The extra light may have contributed to the identification of 2 subjects with anisocoria ≥0.5mm as measured with the ruler in normal room illumination. Had these two cases of anisocoria not been identified, the difference in the frequency of anisocoria across techniques would have been greater than reported. With respect to the infrared photograph technique, the present study found the frequency of anisocoria in normal room light and in dim light to be very similar (13.0 vs. 13.4%). We did not evaluate intrasubject variability of anisocoria nor the variability of either measurement technique.
Steck et al. used a commercially-available monocular infrared pupilometer to evaluate anisocoria in 126 healthy subjects, 51 of whom underwent measurements under several lighting conditions.10 Using the criterion of diameter difference ≥0.4mm to define anisocoria, 23% of their subjects demonstrated anisocoria under photopic conditions and 43.1% demonstrated anisocoria under scotopic conditions. When the cutoff for anisocoria was changed to a diameter difference ≥0.6mm for both lighting conditions, the prevalence of anisocoria approached 0%. When anisocoria was defined as a difference of at least 0.6mm under all conditions tested, only 1.9% of their subjects demonstrated anisocoria. This prevalence of anisocoria under all conditions tested is comparable to the rate of 3% of subjects who demonstrated anisocoria each time tested in the Lam et al. study. In our study, no subject who had anisocoria of 0.5mm or greater in the photopic condition demonstrated anisocoria also in the scotopic condition, regardless of the technique used to assess the anisocoria. The photographs for six of our subjects were not of sufficient quality to assess anisocoria, which may have affected the results. Still, our data support the previous work demonstrating that physiologic anisocoria varies with lighting conditions.
Rickmann et al. used a binocular infrared digital pupilometer to assess pupil size in a large number of subjects with normal pupils.8 By their definition of anisocoria (any difference in pupil size that was within the measuring limits of the instrument), their data show increasing anisocoria with age, but a greater increase for scotopic and mesopic light levels, which supports the findings of Ettinger et al. The mean magnitude of anisocoria in their oldest subjects, however, did not exceed 0.4mm, which likely would have been undetectable, at least in dim illumination, using the gross measurement with ruler technique used in clinics. The age range and number of subjects in our study did not permit evaluation of the effects of age on anisocoria. Rickmann et al., did not determine the prevalence of anisocoria across all 5 light levels used in their study, nor did they examine the prevalence of anisocoria over time.
The data in the present study show a difference in the frequency of anisocoria ≥0.5mm based on measurement technique. Since all subjects had brown irides, whether similar differences in anisocoria frequency based on measurement technique would occur in those with lighter irides is unknown. Additionally, since all subjects in this study were healthy, whether detection rates of pathologic anisocoria differ for the two measurement techniques remains to be investigated.
A limitation of the present study is that the quantitative chromatic characterization of iris color was not used to select the subjects that were included. Had our purpose been to determine the chromatic characteristics of the iris that caused a change in the proportion of anisocoria found by each technique, a quantitative assessment of iris color would have been necessary. Given that our aim was to compare the techniques’ abilities to identify anisocoria in subjects similar to those for whom pupil size is often difficult to assess during patient care, our recruitment efforts specified that subjects must have “dark brown eyes”. This recruitment statement did not result in any subjects presenting for participation with an iris color that was deemed too light for inclusion. Additionally, the result that the infrared photograph technique, but not the gross measurement technique, was able to identify a few cases of anisocoria in the dark suggests that the criterion of recruiting subjects with difficult-to-measure pupil sizes due to iris color was met.
Another limitation of this study is the use of the half-moon millimeter ruler for the gross measurements, since the pupil size cannot be measured in increments finer than 0.5mm. The measuring tape attached to the infrared glasses was marked with 1mm increments; however, magnification of the image with the software could enable the examiner to discriminate pupil size in 0.25mm reasonably well. The half-moon mm ruler was chosen for this study because the ruler is commonly used in clinical practice for pupil size assessment. The infrared photograph technique was chosen for this study because of its low cost relative to manufactured instruments that can measure pupil size in smaller increments. Given the limitations of the equipment used, we set the definition of anisocoria for this study based on the larger 0.5mm increment scale of measurement available with the half-moon ruler and did not attempt to compare the magnitude of anisocoria identified by the two techniques.
The prevalence of physiologic anisocoria ≥0.5mm in subjects with brown irides was greater for assessments made from photographs taken with an inexpensive, custom-built binocular infrared illumination source versus assessments made with a ruler, in both normal and dim room illumination conditions. Thus, in the context of potential neuro-pathology, detection of anisocoria in those with brown irides may be enhanced with the use of photographs of the eyes obtained under infrared illumination, compared to the current standard clinical measurement with a ruler. Given the variability of anisocoria with lighting conditions reported here and in previous work, lighting conditions should be standardized for pupillometry, and care should be taken when comparing an observed anisocoria with past reports or photographs of anisocoria taken in uncertain lighting conditions. Since anisocoria that differs in bright versus dim illumination may yet be physiologic when all other clinical findings are normal, employment of techniques that measure dynamic pupil parameters, such as constriction latency, constriction velocity, and redilation velocity, are recommended for differentiating normal from pathology.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interestThe authors have no conflicts of interest to declare.
Clay Jones (mounting infrared LEDs to spectacle frame).