This research investigated the reported optometric prescribing criteria of Israeli optometrists.
MethodsAn online questionnaire based on previous studies was distributed via email and social networking sites to optometrists in Israel. The questionnaire surveyed the level of refractive error at which respondents would prescribe for different types of refractive error at various ages with and without symptoms.
Results124 responses were obtained, yielding a response rate of approximately 12–22%, 92% of whom had trained in Israel. For all refractive errors, the presence of symptoms strongly influenced prescribing criteria. For example, for 10–20 year old patients the degree of hyperopia for which 50% of practitioners would prescribe is +0.75D in the presence of symptoms but twice this value (+1.50D) in the absence of symptoms. As might be expected, optometrists prescribed at lower degrees of hyperopia for older compared with younger patients. There was a trend for more experienced practitioners to be less likely to prescribe for lower degrees of myopia and presbyopia. Practitioner gender, country of training, the type of practice environment, and financial incentives were not strongly related to prescribing criteria.
ConclusionsThe prescribing criteria found in this study are broadly comparable with those in previous studies and with published prescribing guidelines. Subtle indications suggest that optometrists may become more conservative in their prescribing criteria with experience.
Este estudio investigó los criterios de prescripción optométrica reportados por los optometristas israelíes.
MétodosSe distribuyó un cuestionario online basado en estudios previos, utilizando el correo electrónico y las redes sociales, a los optometristas de Israel. Dicho cuestionario sondeaba el nivel de error refractivo para el cual los encuestados realizarían prescripciones, para los diferentes tipos de error refractivo, a diversas edades y con variedad de síntomas.
ResultadosRespondieron 124 personas, obteniéndose un índice de respuesta de aproximadamente el 12–22%. El 92% de los participantes se había formado en Israel. En hipermetropía, la presencia de síntomas influyó considerablemente en los criterios de prescripción. Por ejemplo, para pacientes de 10-20 años de edad, el grado de hipermetropía para el cual el 50% de los facultativos realizaría una prescripción sería de +0,75D en presencia de síntomas, pero se duplicaría este valor (+1,50D) en ausencia de ellos. Como cabría esperar, los optometristas prescribirían a personas mayores grados más bajos de hipermetropía, en comparación a las personas jóvenes. Los facultativos más experimentados reflejaron una tendencia de menor probabilidad de prescripción cuanto menor fuera el grado de miopía y presbicia. El sexo del facultativo, el país de formación, el tipo de entorno de práctica, y los incentivos financieros no guardaron una relación sólida con los criterios de prescripción. Los criterios de prescripción hallados en este estudio son ampliamente comparables a los de los estudios previos y a los de las guías publicadas.
ConclusionesLos criterios de prescripción optométrica en Israel pueden compararse a las recomendaciones de las guías publicadas por país de formación de los facultativos, profesional, género, o entorno laboral. Existen débiles indicadores que sugieren que los optometristas pueden volverse más conservadores, en cuanto a criterios de prescripción, con la experiencia.
One of the most frequent decisions that optometrists make is whether to prescribe a correction for refractive errors, whether it be with spectacles or contact lenses. This decision is generally straightforward if a large uncorrected anomaly is present, but becomes much more difficult in borderline cases. Considering the fact that most optometrists make this decision several times every day, it is surprising that little research has been undertaken to help determine at what point optometrists typically intervene.
There are several guidelines that have been published to help optometrists and ophthalmologists when prescribing for refractive errors with either specific or general guidelines. The American Optometric Association provides guidelines for correction of hyperopia, myopia and presbyopia based on consensus among expert optometrists.1–3 The American Academy of Ophthalmology has general guidelines for adults with refractive errors4 and specific guidelines for children age three and younger.5 The Royal College of Ophthalmologists has specific guidelines for strabismus, but not for healthy adults or children with refractive errors. The American Association for Pediatric Ophthalmology and Strabismus warns about and defines high refractive errors in children that might lead to amblyopia, but does not have specific prescribing guidelines.6 Leat7 provides guidelines for prescribing in childhood for various refractive conditions and the topic was reviewed by O’Leary and Evans.8
In Israel, following the 1991 Optometry Law9 two academic programs in optometry were established in 1995, with the first intake graduating in 1999. Most of the optometrists in Israel are graduates of those two schools, which provide a four-year undergraduate degree in optometry based on the European Diploma Syllabus. The schools, Hadassah Academic College10 and Bar Ilan University, share several clinical faculty. In Israel, prescribing is carried out primarily by optometrists and not by ophthalmologists; therefore we limited this survey to optometrists.
This study aimed to assess prescribing decisions for borderline refractive prescriptions by Israeli optometrists and whether prescribing is influenced by working environment, gender and years of experience.
MethodsAn online questionnaire based on one used by O’Leary and Evans8 was distributed to Israeli optometrists via email and social media: emails were sent to approximately 500 graduates of the two Israeli optometry schools. In addition, the questionnaire was posted on three Israeli optometry Facebook pages (with a total of 1600 members). It should be noted that there is considerable overlap between the email list and the members of the Facebook page, and that some members of the Facebook page are not optometrists (opticians, suppliers, distributers, etc.). The questionnaire invited optometrists only and required all questions to be answered to submit the questionnaire (see Appendix 1). Google Docs was used to design the questionnaire and responses were automatically exported to Excel 2010 hence avoiding transcribing errors.
Questionnaire designThe questionnaire included demographic questions pertaining to the practitioner's age and gender, alongside professional questions, which included years of experience, work environment, scope of practice and financial incentives (Appendix 1).
There were 12 questions regarding prescribing philosophies for different refractive errors (simple myopia, simple hyperopia, astigmatism without a spherical component and presbyopia with cylinder less than 0.75D) in the presence and absence of symptoms and for varying age group ranges. Symptoms were not defined and the clinicians were left to interpret this as they thought best. It was anticipated at the outset that it would be challenging to persuade busy practitioners to complete the questionnaire. Therefore, brevity was an import design consideration. It was felt that a questionnaire that sampled all prescribing decisions for every age group would be too lengthy, so the decision was made to target the age groups that would be most instructive for each type of refractive error. In Israel children under the age of 6 years rarely consult community optometrists. Furthermore, myopia and astigmatism are infrequently corrected in this age-group.11 Thus, for myopia and astigmatism the questionnaire started at age 6 years. The few children who are seen under the age of 6 years are mostly aged 4–6 years and hyperopic11; therefore, this category was included for hyperopia. Once patients reach the age of 40 years, prescribing decisions are likely to be confounded by presbyopia and the possibility of multifocal lenses. Therefore, over the age of 40 years the questionnaire concentrated on presbyopia.
The exact questions can be seen in Appendix 1. The participant was forced to select from a scale of refractive errors in 0.25D increments (bins).
Statistical analysisAnalyses were performed with SPSS, version 22 (SPSS, Inc., Chicago, IL) and with Microsoft Excel 2010. Normality was tested using the Anderson–Darling test and statistical significance was assessed with the Mann–Whitney test. Armstrong12 criticized the blanket use of Bonferroni corrections for multiple corrections as being so conservative that it would lead many “real” effects to go undetected. However, he recommended a Bonferroni correction should be considered to be appropriate in some circumstances. In the present work, we have included a Bonferroni correction where one hypothesis is tested several times in similar datasets (e.g., in testing whether the prescribing behavior of men differs from that of women using the same statistical tests on data for myopia, hyperopia, astigmatism, and presbyopia). Non-parametric correlations (Spearman test) were calculated in order to evaluate correlations between years of experience and the answer for each question.
For each question, the average, standard deviation and range were calculated. The 50th percentile and 75th percentile were calculated using the Excel Percentile function, which calculates the kth percentile of a supplied range of values for a given value of k. The frequency of each bin was counted for every question and the cumulative percentage was calculated.
In addition, Igor pro (Wavemetrics, Lake Oswego, OR) was used to fit a univariate distributions using least squares estimates of the cumulative distribution functions with the equation: y=y0+A*e(invTau*x). The constant y0 was set to 100%, since a cumulative percentile distribution will plateau at that value.
ResultsRespondentsMost of the optometrists in Israel are graduates of Hadassah Academic College and Bar Ilan University. At the time of the study, there were approximately 900 graduates of both Institutions. Personal emails were sent to 500 graduates for whom current information was available and Facebook was used in an attempt to reach other optometrists. A total of 112 Israeli graduates participated in the survey with an average (±SD) of 5.42±4.3 years of work experience (range 0.4–17 years). The response rate varies from 12 to 22% depending on the audience reached. If only the graduates contacted via email are considered, then the response rate is (112/900) ∼22%. On the other hand, if all 900 graduates are members of the Facebook page and actually saw the post, then the response rate is 12% of optometrists trained in Israel (112/900).
An additional 12 participants responded who studied optometry abroad. An initial analysis demonstrated that the results for the Israeli educated cohort (N=112) were not significantly different from the total cohort, therefore, all the data were pooled.
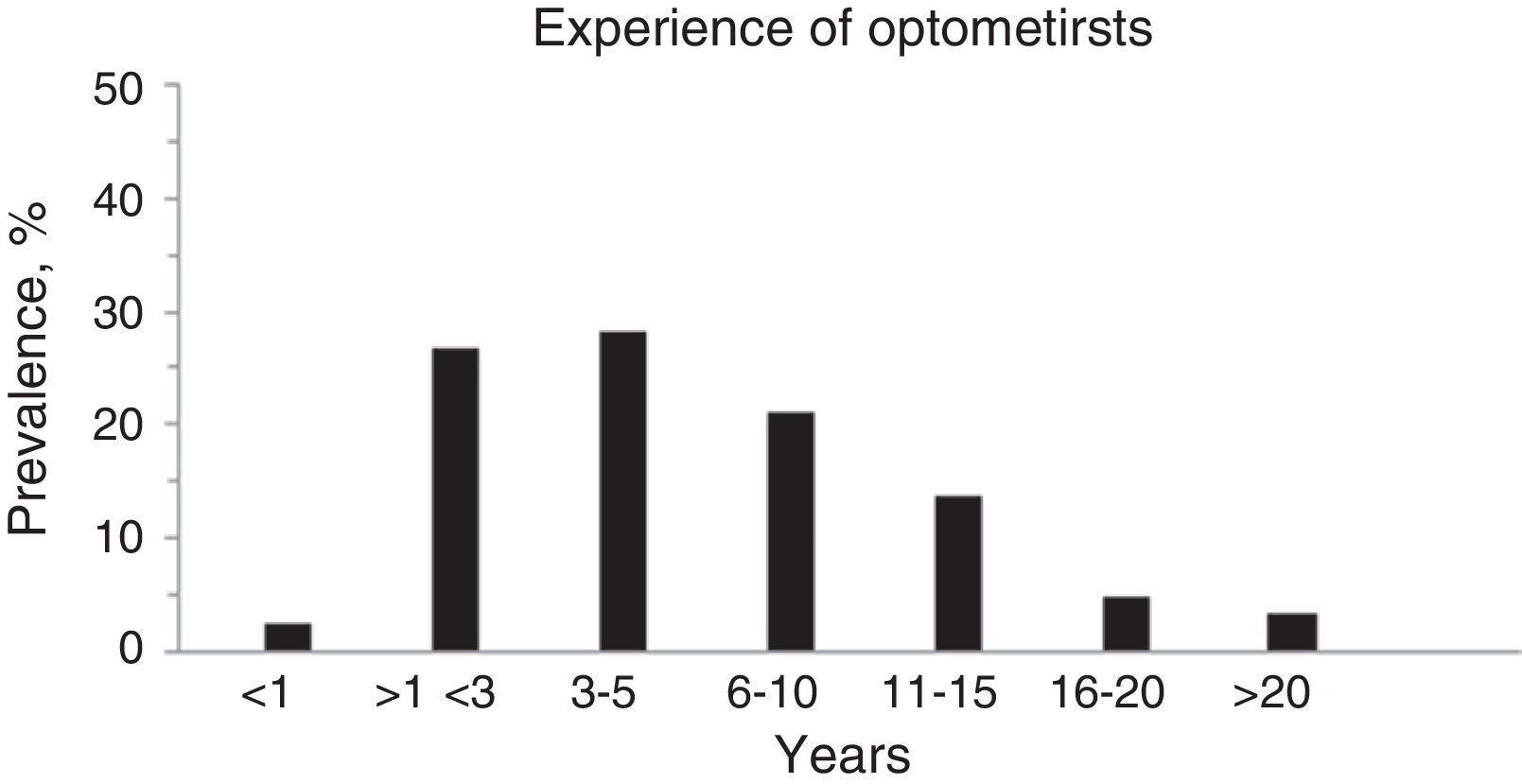
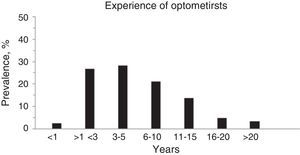
In total, 124 subjects participated in the survey with an average of 7.18±8.0 years of work experience (range 0.4–48 years, see Fig. 1).
Years of work experience was not normally distributed (Anderson–Darling, p<0.0005) with the majority of respondents having five or fewer years of work experience (see Fig. 1). 66.1% of the respondents were women.
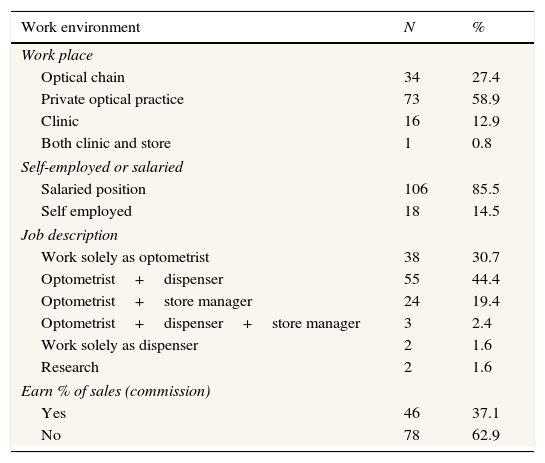
Table 1 describes the working environment of the cohort. Most respondents work in a private optical store (58.9%), are in salaried positions (85.5%), and work as optometrists and sell products (44.4%) without sales incentives (62.9%). Thirty-two subjects (25.8%) reported that they work in an optical chain with at least 10 branches. Two subjects manually commented that they work in a chain of four branches, and were included in the category of “optical chain.”
Work environment of the cohort.
| Work environment | N | % |
|---|---|---|
| Work place | ||
| Optical chain | 34 | 27.4 |
| Private optical practice | 73 | 58.9 |
| Clinic | 16 | 12.9 |
| Both clinic and store | 1 | 0.8 |
| Self-employed or salaried | ||
| Salaried position | 106 | 85.5 |
| Self employed | 18 | 14.5 |
| Job description | ||
| Work solely as optometrist | 38 | 30.7 |
| Optometrist+dispenser | 55 | 44.4 |
| Optometrist+store manager | 24 | 19.4 |
| Optometrist+dispenser+store manager | 3 | 2.4 |
| Work solely as dispenser | 2 | 1.6 |
| Research | 2 | 1.6 |
| Earn % of sales (commission) | ||
| Yes | 46 | 37.1 |
| No | 78 | 62.9 |
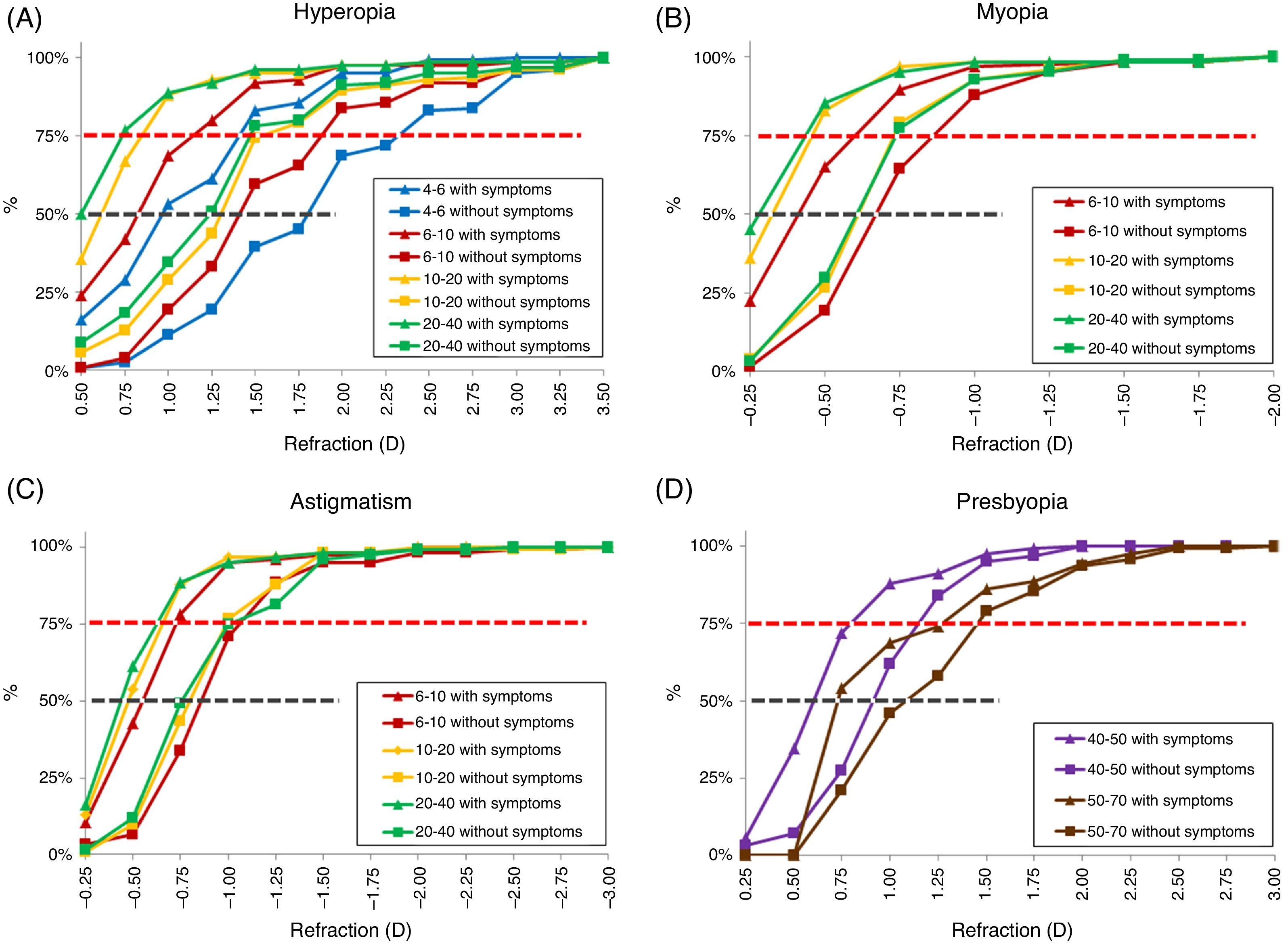
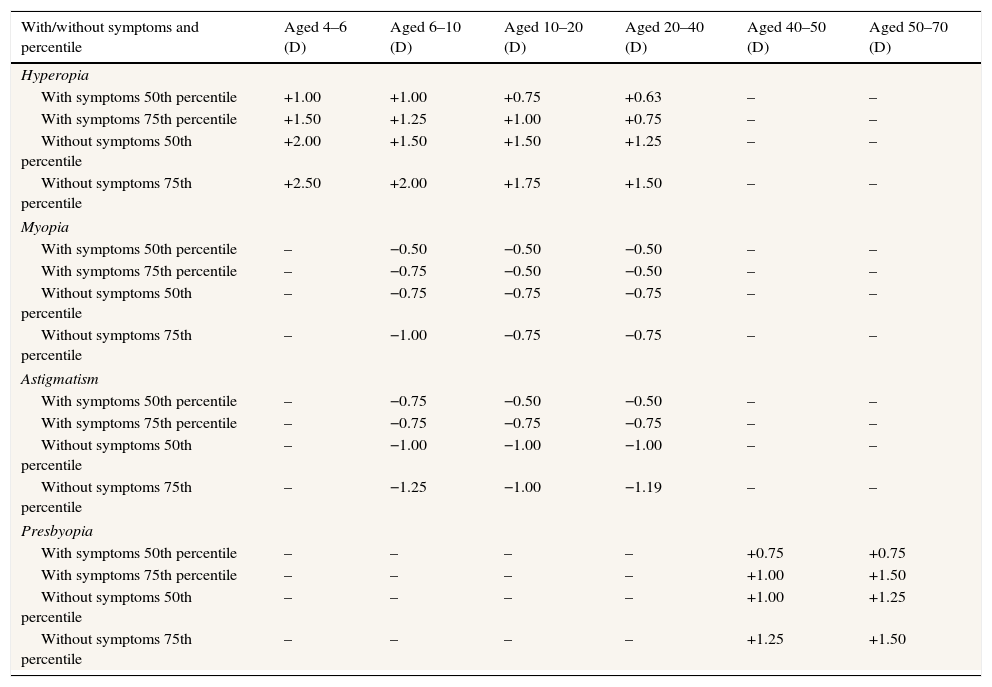
Fig. 2 shows the cumulative frequency plotted as a function of refractive error bin for each question. Fig. 2A–D summarizes data from all the questions regarding hyperopia, myopia, astigmatism and presbyopia, respectively. Each age group is represented by a single color, and shown for asymptomatic (square) and symptomatic (triangle) questions. For all types of refractive errors, in the presence of symptoms, optometrists prescribe at lower refractive errors than in the absence of symptoms (p<0.0001 in all cases, Mann–Whitney, Table 2). Even when using the Bonferroni correction, these results remain highly significant (p<0.0025). The age of the patients determines prescribing philosophy in many cases (Table 3), but not all, as will be described below.
Cumulative frequency plotted as a function of refractive error bin for each question [(A) hyperopia, (B) myopia, (C) astigmatism and (D) presbyopia]. Age groups represented by a single color (ages 4–6 years: blue, ages 6–10 years: red, ages 10–20 years: yellow, ages 20–40 years: green, ages 50–70 years: brown). Both asymptomatic (square) and symptomatic (triangle) questions are shown. Dash red and black lines represent the 75th and 50th percentile respectively. The lines connecting the data points are not fitted curves and are for illustrative purposes only. They cannot be used to extrapolate. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
Columns 2–7 give the refractive error at which the proportion of respondents indicated in column 1 would prescribe for the scenario outlined in column 1.
| With/without symptoms and percentile | Aged 4–6 (D) | Aged 6–10 (D) | Aged 10–20 (D) | Aged 20–40 (D) | Aged 40–50 (D) | Aged 50–70 (D) |
|---|---|---|---|---|---|---|
| Hyperopia | ||||||
| With symptoms 50th percentile | +1.00 | +1.00 | +0.75 | +0.63 | – | – |
| With symptoms 75th percentile | +1.50 | +1.25 | +1.00 | +0.75 | – | – |
| Without symptoms 50th percentile | +2.00 | +1.50 | +1.50 | +1.25 | – | – |
| Without symptoms 75th percentile | +2.50 | +2.00 | +1.75 | +1.50 | – | – |
| Myopia | ||||||
| With symptoms 50th percentile | – | −0.50 | −0.50 | −0.50 | – | – |
| With symptoms 75th percentile | – | −0.75 | −0.50 | −0.50 | – | – |
| Without symptoms 50th percentile | – | −0.75 | −0.75 | −0.75 | – | – |
| Without symptoms 75th percentile | – | −1.00 | −0.75 | −0.75 | – | – |
| Astigmatism | ||||||
| With symptoms 50th percentile | – | −0.75 | −0.50 | −0.50 | – | – |
| With symptoms 75th percentile | – | −0.75 | −0.75 | −0.75 | – | – |
| Without symptoms 50th percentile | – | −1.00 | −1.00 | −1.00 | – | – |
| Without symptoms 75th percentile | – | −1.25 | −1.00 | −1.19 | – | – |
| Presbyopia | ||||||
| With symptoms 50th percentile | – | – | – | – | +0.75 | +0.75 |
| With symptoms 75th percentile | – | – | – | – | +1.00 | +1.50 |
| Without symptoms 50th percentile | – | – | – | – | +1.00 | +1.25 |
| Without symptoms 75th percentile | – | – | – | – | +1.25 | +1.50 |
All Mann–Whitney tests between with symptoms vs. without symptoms were significant (at least p<0.0001).
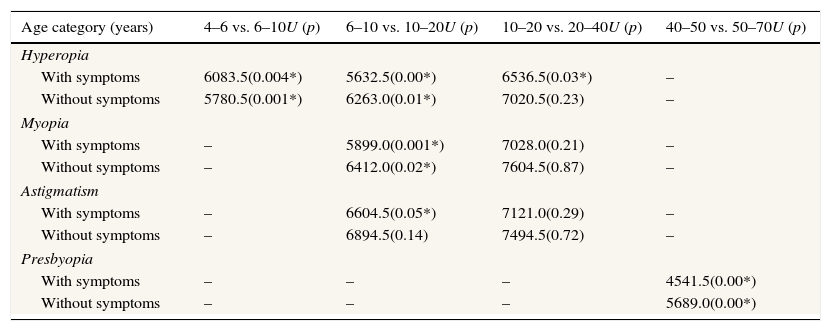
Prescribing behavior as a function of patient age group. Mann–Whitney U statistic and p values between the adjacent age groups are given in the table. (p values are in brackets, * demonstrates significant value.).
| Age category (years) | 4–6 vs. 6–10U (p) | 6–10 vs. 10–20U (p) | 10–20 vs. 20–40U (p) | 40–50 vs. 50–70U (p) |
|---|---|---|---|---|
| Hyperopia | ||||
| With symptoms | 6083.5(0.004*) | 5632.5(0.00*) | 6536.5(0.03*) | – |
| Without symptoms | 5780.5(0.001*) | 6263.0(0.01*) | 7020.5(0.23) | – |
| Myopia | ||||
| With symptoms | – | 5899.0(0.001*) | 7028.0(0.21) | – |
| Without symptoms | – | 6412.0(0.02*) | 7604.5(0.87) | – |
| Astigmatism | ||||
| With symptoms | – | 6604.5(0.05*) | 7121.0(0.29) | – |
| Without symptoms | – | 6894.5(0.14) | 7494.5(0.72) | – |
| Presbyopia | ||||
| With symptoms | – | – | – | 4541.5(0.00*) |
| Without symptoms | – | – | – | 5689.0(0.00*) |
We reasoned that the 50th percentile represents the cut-off criteria at which a prescription is no longer considered borderline. The 75th percentile is interpreted as indicative of commonplace prescribing practice. These data are shown in Table 2 and will be addressed in the next section for different refractive conditions. The Excel Percentile function was used the function to calculate these variables, which uses interpolation where required. For example, the 50th percentile for prescribing for a hyperope with symptoms aged 20–40 is +0.625, indicating that fewer than 50% of the respondents would prescribe for refractive errors of 0.625D or less.
In addition, the exact 50th and 75th percentiles were calculated from the data plotted in Fig. 2. Curves were fit with a univariate cumulative distribution function with similar results to that shown in Table 2, with no statistically significant difference (paired t-test, p=0.91).
HyperopiaThe data in Table 2 highlight the importance of symptoms in prescribing for hyperopia. For example, for 10–20 year old patients the degree of hyperopia for which 50% of practitioners would prescribe is +0.75D in the presence of symptoms but twice this value (+1.50D) in the absence of symptoms. As can be seen in Table 3, there is a shift to prescribing at lower powers from younger to older age groups (aged 4–6 to 6–10, 6–10 to 10–20 with and without symptoms and 10–20 to 20–40 with symptoms only; p value Mann–Whitney <0.05). The exception is that there is no difference, in the absence of symptoms, between prescribing criteria for hyperopia in 10–20 and 20–40 year olds.
MyopiaTable 2 demonstrate that the degree of myopia for which 50% of practitioners would prescribe is the same for all age groups: −0.50 in the presence of symptoms and −0.75 in the absence of symptoms. However, there is a shift to prescribing lower powers in older patients when contrasting the 6–10 year and 10–20 year age groups (Tables 2 and 3). These trends most likely reflect the similar visual needs of high school students and young adults.
AstigmatismThere is a shift to prescribing lower powers from younger to older age groups at ages 6–10 to 10–20 with symptoms only (p value Mann–Whitney <0.05, see Fig. 2C and Table 3).
PresbyopiaThere is a shift to prescribing lower powers from younger to older age groups at age 40–50 to 50–70 with and without symptoms (p value and Mann–Whitney U statistic <0.05, Fig. 2D and Table 3), which reflects loss of accommodation with age.
Work environment and prescribing philosophiesThe optometrist's work environment may influence prescribing philosophy. For example, if an optometrist earns a commission (a percentage of spectacle sales) it might provide an impetus (if so, hopefully only subconsciously) to prescribe at lower powers. Based on the assumption that the prescribing philosophy may be influenced by the work environment, the cohort was divided into two groups: those who receive commission and those who do not. In the former group we included both salaried employees who receive a bonus based on sales and optometrists who own the optical business at which they work. The Mann–Whitney test was used to compare these groups, as the data were not normally distributed (Anderson–Darling). A statistically significant difference was observed only in two areas (from a total of 24 comparisons): for myopic patients ages 6–10 and 10–20 with symptoms, the optometrists who earn commission were more likely to prescribe at lower powers (Mann–Whitney, p<0.04 and p<0.02, respectively). However, when applying the Bonferroni correction, this lost statistical significance.
Similarly, it could be hypothesized that optometrists who work for chains would be more likely to prescribe at lower powers. We defined a chain as at least 4 stores. In this case a statistically significant difference was observed in only three comparisons (from a total of 24): symptomatic hyperopic patients ages 4–6 and 6–10 and symptomatic myopic patients ages 10–20. In these cases, optometrists who worked at chains were more likely to prescribe at lower powers (Mann–Whitney, p<0.05 in all cases). Again, when applying the Bonferroni correction, these values no longer reached statistical significance.
GenderThe gender of the optometrist did not emerge as a factor affecting prescribing behavior in almost all cases. There was only a statistically significant difference between men (1.21±0.6D) and women (1.03±0.4D) in prescribing for 50–70 year old patients without symptoms, but this did not reach statistical significance when using the Bonferroni correction.
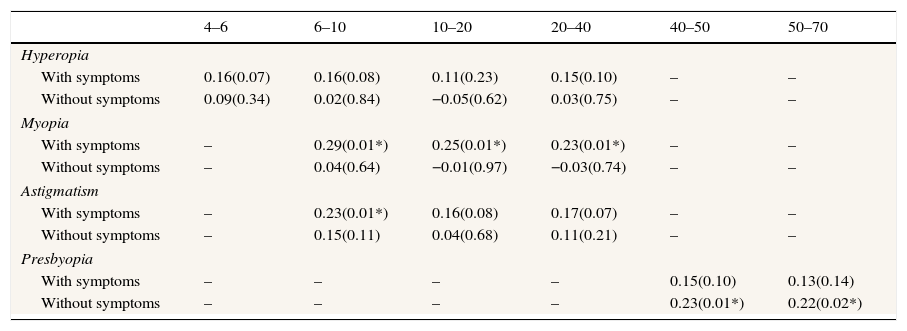
Experience and prescribing behaviorTo test whether years of work experience in optometry influenced prescribing behavior, a Spearman correlation was calculated between years of experience and the prescription at which the optometrist would prescribe spectacles, for every question (Table 4). Two interesting trends emerged, although only with a weak correlation. For myopic patients of all ages with symptoms and for all presbyopic patients in the absence of symptoms, there was a positive correlation between years of experience and the level of refractive power at which practitioners prescribed. In other words, more experienced practitioners were less likely to prescribe for low degrees of myopia and presbyopia. In addition, for young (6–10 year old) astigmatic patients there is also a positive correlation between experience and refractive power.
Spearman correlation between years of experience and prescribing behavior in each age group. (p values are in brackets, * demonstrates significant value.).
| 4–6 | 6–10 | 10–20 | 20–40 | 40–50 | 50–70 | |
|---|---|---|---|---|---|---|
| Hyperopia | ||||||
| With symptoms | 0.16(0.07) | 0.16(0.08) | 0.11(0.23) | 0.15(0.10) | – | – |
| Without symptoms | 0.09(0.34) | 0.02(0.84) | −0.05(0.62) | 0.03(0.75) | – | – |
| Myopia | ||||||
| With symptoms | – | 0.29(0.01*) | 0.25(0.01*) | 0.23(0.01*) | – | – |
| Without symptoms | – | 0.04(0.64) | −0.01(0.97) | −0.03(0.74) | – | – |
| Astigmatism | ||||||
| With symptoms | – | 0.23(0.01*) | 0.16(0.08) | 0.17(0.07) | – | – |
| Without symptoms | – | 0.15(0.11) | 0.04(0.68) | 0.11(0.21) | – | – |
| Presbyopia | ||||||
| With symptoms | – | – | – | – | 0.15(0.10) | 0.13(0.14) |
| Without symptoms | – | – | – | – | 0.23(0.01*) | 0.22(0.02*) |
As expected from previous research,8 this study shows that symptoms are an important factor that influences prescribing criteria. It is reassuring that in this cohort, the prescribing behavior between different modes of optometric practice was insignificant using Bonferroni correction, i.e. we did not find financial incentive to be an influential factor in prescribing decisions. Patients’ age was a significant factor when comparing prescribing criteria for young children to older children and teenagers, for both hyperopia and myopia. In most cases patients’ age was not a factor for prescribing in astigmatism but was a factor for prescribing in presbyopia, which increases with age.13
A weak correlation emerged between the optometrists’ years of experience and prescribing criteria in the following scenarios: all myopic patients in the presence of symptoms, young astigmatic patients in the presence of symptoms and all presbyopic patients in the absence of symptoms. This may suggest that the more years of experience the optometrist has, the less likely they are to prescribe glasses at borderline refractive errors. However, since the correlation was weak, this conclusion should be regarded with caution.
This is the first survey of prescribing philosophy carried out in Israel. Since optometry in Israel is a young profession with only 15 years of local graduates, it is important to evaluate the optometrists’ prescribing behavior and compare to that of more established counties. In our study, most participants have graduated recently thus having a few years of experience, and this may influence results.
Various prescribing guidelines exist for pediatric patients based on evidence and expert opinion. For example, the American Academy of Ophthalmology,14 American Association for Pediatric Ophthalmology and Strabismus (AAPOS),15 The Royal College of Ophthalmologists16 and the American Optometric Association17 all have prescribing guidelines. Leat7 reviewed these guidelines, updated them and provided more detail. Therefore, the results of the present study were compared with Leat's recommendations, where our questions related to similar age groups to those covered by Leat.
In general, the 50th percentile for prescribing for this cohort is very similar to the recommendations of Leat7 for all refractive errors assessed except for pre-school age hyperopic children. For this age group, Leat recommends prescribing only above +2.50D in the absence of signs or symptoms. This is based on studies of visual function and functional vision18–20 and the upper 95th percentile of the range for refractive error in this age group, which was +2.60at 3 years and +2.90at 4 years.21 In the current study, Israeli optometrists prescribed at +2.00D in the absence of symptoms and +1.00D in the presence of symptoms. The findings in the absence of symptoms are similar to Leat's recommendations. We think that the symptom most likely to be reported in pre-school hyperopes is a parental report of strabismus and Leat indicates that in this scenario prescribing is required. We therefore speculate that our finding of a lower threshold for prescribing in the presence of symptoms is consistent with Leat's recommendations.
For school age hyperopic children, Leat's recommendations were identical to the 50th percentile in this study: >1.50 and >1.00D in the absence and presence of symptoms, respectively.
The results of this study for myopia and astigmatism are similar to the recommendations of Leat.7 Concerning prescribing recommendations for myopia, Leat recommends full correction although does not specify from what refractive error one should do so. The cohort in this study would prescribe for >−0.75 and >−0.50 in the absence and presence of symptoms, respectively. Since −0.25D is in the range of error of emmetropia, our cohort is effectively prescribing in the presence of any refractive error. For astigmatic school age children, Leat recommends correction of >0.75D, which is within 0.25D of that recommended in all cases in this study.
Prescribing guidelines do not necessarily reflect prescribing behavior in clinical practice. Surveys of prescribing behavior attempt to describe what actually happens in clinical practice (see “Limitations” section below). We will attempt to compare the results of this study to previous ones, although many did not specify the presence of symptoms or age group. In general, the results of this study were similar to other surveys of optometrists. However, when there are differences, the trend is that Israeli optometrists prescribe at lower refractive errors. Further research will be required to validate this finding and, if replicated, explore the reason(s).
HyperopiaPrescribing for hyperopia in young children was surveyed in several studies showing a wide range for behavior. Surveys of American optometrists22 and German ophthalmologists (OMD)23 found that 67% and 84%, respectively, of practitioners would prescribe spectacles for four-year-old children with +3.00D of hyperopia. While this is similar to the 50th percentile in the current study (+2.00D), it is hard to compare since the choices in those surveys were either +1.00D or +3.00D as opposed to the 0.25D bins in this study. Farbrother24 surveyed 93 hospital based optometrists and found the 50th percentile for non-symptomatic children to be slightly higher than the results in the present study (+2.50D). Leat et al.25, in an audit of pediatric patient cases (including both those with and without symptoms) found the 50th percentile to be +2.70D. Two studies of OMDs, found that these practitioners prescribed only for higher refractive errors. Lyons22 found that OMDs prescribed only above +5.00D (54%) in the absence of symptoms for patients aged 4–6 years, while in a survey of 334 AAOPS members15 the 50th percentile was +4.00D.
The only publication that we have found addressing prescribing behavior for older hyperopic children and teenagers is Leat et al.25 The differences between their results and this study were between 0.15 and 0.58D, which may be due to the fact that their age groups were slightly different.
Only one study surveyed prescribing behavior for hyperopic adults.8 That study found that for patients under age 40, in the presence of symptoms, the 50th percentile for prescribing is +0.75D. However, in the absence of symptoms optometrists would not prescribe at any of the powers in the questionnaire (+1.75D) more than 50% of the time that they are encountered. For the current study, in the presence of symptoms, the 50th percentile for 20–40 year olds is +1.25D, which is within 0.50D of the cited study.8 However, in the absence of symptoms, the 50th percentile for the Israeli cohort was +0.625D, which is much lower than the previous (UK) study.
Myopia and astigmatismA survey of the AAOPS members (N=334),15 assessed prescribing for myopic and astigmatic children age 4–7 years. For myopic children, the 50th percentile was higher (−1.50D) than that found in this study, −0.75 and −0.50 in the absence and presence of symptoms, respectively. This may reflect the difference in prescribing philosophy between optometrists and ophthalmologists.
The results for astigmatic children were within 0.50D of that found in the current study (−1.00D). To the best of our knowledge, there are no previous surveys of prescribing for myopia for other age groups and only one study of prescribing behavior for astigmatism. The survey of O’Leary and Evans8 referred to astigmatic patients “of any age” and their results are similar to the current study in the presence of symptoms (−0.75). However, in the absence of symptoms the 50th percentile for prescribing was higher than the current study (−1.50D vs. −1.0D), again reflecting the trend of Israeli optometrist to prescribe at lower refractive errors.
PresbyopiaThe results for prescribing in presbyopia were similar to a previous study in the presence of symptoms (0.75),8 however, in the absence of symptoms, Israeli optometrists would prescribe at lower additions (1.00D as opposed to 1.50D).
LimitationsSurveys of prescribing behavior attempt to describe what actually happens in clinical practice. However, it is important to note that people may tend to optimize their responses toward what they think they should do, rather than what they actually do.
One of the limitations of this study is the low response rate (12–22%). However, the results are within what can be expected from other electronic surveys.26 While electronic surveys are increasingly used because of their accessibility, rapidity, reduced cost, less need for human resources and elimination of human errors, paper-based surveys still possess higher response rates.27
Shah et al.28 reviewed methods of measuring clinical practice and noted that the gold standard methodology is “standardized patients” who present unannounced to clinics. However, such research (e.g., Shah et al.29) is expensive and can only sample a relatively small proportion of a profession. Another approach would be record abstraction,30 but this is also time-consuming and practitioners might be less willing to consent to having their records examined than to answering a survey. The advantage of surveys, such as that used in the present research, is that a larger proportion of the profession can be sampled, but it has to be acknowledged that such approaches are likely to over-estimate clinical competence.31 Although the sample size in the present research of 124 is more than could have been investigated with standardized patient methodology, this is only 7% of the Israeli optometric population and this is another limitation of the present research. It is reassuring that we sampled practitioners working in a range of practice environments and we are not aware of any systematic biases in those who responded to this survey.
Another limitation of the study is the wide age bracket used in the older presbyope question (aged 50–70). Also, for the myopia and hyperopia questions the optometrists were not instructed as to whether they should respond, for astigmatic cases, considering the spherical equivalent, lower or higher powered meridian.
In addition, in this study most participants have graduated recently thus having a few years of experience, which may influence results.
Future researchThis study and the comparison with other research have highlighted a broad spectrum of prescribing philosophies. There are only a few studies that have investigated the effect of optometric interventions on visual performance in real patients32,33 rather than the artificial situation of simulating refractive errors, typically in university students. More research, preferably randomized controlled trials, would be valuable to investigate the benefit from borderline optometric prescriptions.
Conflicts of interestAuthors report no conflicts of interest and have no proprietary interest in any of the materials mentioned in this article.
The authors would like to thank Dr. Mark Guggenheim, Director of Bar Ilan Optometry Clinic for sharing information about the department and Prof. Sharona Gordon for help with statistical analyses. The authors would like to thank Ms. Dinah Paritzky for critical reading of the manuscript.
The following are the supplementary data to this article:


![Cumulative frequency plotted as a function of refractive error bin for each question [(A) hyperopia, (B) myopia, (C) astigmatism and (D) presbyopia]. Age groups represented by a single color (ages 4–6 years: blue, ages 6–10 years: red, ages 10–20 years: yellow, ages 20–40 years: green, ages 50–70 years: brown). Both asymptomatic (square) and symptomatic (triangle) questions are shown. Dash red and black lines represent the 75th and 50th percentile respectively. The lines connecting the data points are not fitted curves and are for illustrative purposes only. They cannot be used to extrapolate. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.) Cumulative frequency plotted as a function of refractive error bin for each question [(A) hyperopia, (B) myopia, (C) astigmatism and (D) presbyopia]. Age groups represented by a single color (ages 4–6 years: blue, ages 6–10 years: red, ages 10–20 years: yellow, ages 20–40 years: green, ages 50–70 years: brown). Both asymptomatic (square) and symptomatic (triangle) questions are shown. Dash red and black lines represent the 75th and 50th percentile respectively. The lines connecting the data points are not fitted curves and are for illustrative purposes only. They cannot be used to extrapolate. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)](https://static.elsevier.es/multimedia/18884296/0000000900000001/v2_201601130107/S1888429615000795/v2_201601130107/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w90elkTtpMHXMkN9jatH7+0Y=)





