We evaluated the effectiveness of office-based vergence/accommodative therapy with home reinforcement for intermittent exotropia in a private practice environment.
MethodsThis was a retrospective chart review study. Patients who received office-based vision therapy for intermittent exotropia in a private optometric clinic were reviewed. Patients with intermittent exotropia treated with and without strabismus surgery were both included. The pre-therapy baseline data were compared to the re-evaluation data obtained at the last therapy session. All patients received office-based vergence/accommodative therapy administered by a trained therapist during a 60 min office visit every one to two weeks, combined with home reinforcement for a minimum of 15 min, five times per week. The primary outcome measure in this study was the change in the Office Control Score from the pre-therapy visit to the post-therapy visit. The hypothesis was that office-based vergence/accommodative therapy would significantly improve the Office Control Score.
ResultsForty patients aged from 5 to 22 years old fulfilled the inclusion criteria. Eight of them were postoperative patients. After treatment, there was a change of −1.1 ± 1.6 (p < 0.001, z = 3.73, effect size: 0.42) and −1.1 ± 1.4 (p < 0.001, z = 4.26, effect size: 0.48) in distance and near Office Control Score, respectively. In the subgroup analysis, significant improvements in the Office Control Score were observed in both the operated and unoperated intermittent exotropes at distance and near.
ConclusionThis study showed that office-based vergence/accommodative therapy with home reinforcement significantly improved the distance and near control of exodeviation in both operated and unoperated intermittent exotropia patients in a private practice environment.
Intermittent exotropia is the most common form of exotropia and it is estimated that approximately 3% of Chinese teenagers suffer from this condition.1 The treatment of intermittent exotropia includes watchful observation,2,3 patching,2,3 prism,4,5 overminus lens,6 vision therapy7–13 and surgery.14,15 Currently, there is no consensus regarding which treatment modality is the best approach for this condition.16 There is a number of randomized clinical trials of occlusion2,3 and overminus lens6 that support the use of these approaches. Surgery is a common treatment modality for patients with intermittent exotropia but the evidence supporting its effectiveness is limited. There is a lack of randomized clinical trial data on the comparison between the effect of surgical treatment and observation alone.17,18 Furthermore, it is often reported that after receiving the surgery, there is still a strong tendency for the condition to recur,19,20 and a significant portion of patients require reoperation.14,21–23
Unlike surgery, which aims to reduce the size of the deviation, vision therapy is a treatment that mainly focuses on improving the control of exodeviation. Through vision therapy, visual skills that may contribute to the control of exodeviation are trained. These visual skills include but are not limited to sensory fusion, motor fusion (e.g., improving fusional vergence), proprioceptive awareness, accommodation and saccades according to different schools of thought.24–27 There is a number of studies supporting the effectiveness of vision therapy for intermittent exotropia, but none of them used validated methods to assess the control of exodeviation.7–13 Most studies classified patients into different groups after treatment. For example, participants were classified into functional cure, cosmetic cure, total cure and failure groups,28 or into good, fair and poor outcome groups,7 or into other similar groupings8–10,12,13,29 according to multiple criteria, making it impossible to isolate and analyze the ability of participants to control exodeviation. In recent years, an intermittent exotropia control scoring method developed by Mohney et al.30 has been validated in detail31,32 and adopted in a number of randomized clinical trials.2,3,6 The main objective of the current study is to evaluate the effectiveness of office-based vergence/accommodative therapy on intermittent exotropia as assessed by the validated Office Control Score in a private practice environment.
MethodsParticipantsThis was a retrospective chart review study. All patients who received office-based vision therapy for intermittent exotropia in a private optometric clinic from 2017/01 to 2018/12 were reviewed. Patients who received vision therapy were re-evaluated after every 5 therapy sessions, and only those who received at least 5 sessions of vision therapy were analyzed. In all patients, visual acuity was needed to be correctable to 20/25 or better in each eye. Patients with intermittent exotropia treated with and without strabismus surgery were both included. Intermittent exotropia was defined as having a ≥ Grade 1 control score for either the distance or near Office Control Score. Constant exotropia patients (i.e., those with Grade 5 control score for both distance and near with poor random dot stereopsis) were not included. Patients with a history of nystagmus, restrictive strabismus, paretic strabismus or significant ocular or neurologic disorders (e.g., cerebral palsy) other than strabismus were excluded.
ExaminationAll patients were assessed before the commencement of vision therapy. Examinations were performed by authors MMM, CC, and CS. The examination for each individual patient was performed by the same examiner before and after therapy. The pre-therapy examination included visual acuity, lensometry, subjective refraction, prism alternating cover test and Office Control Score. Sensory and motor fusion tests included but were not limited to the Worth 4 dots test, extraocular movement, near stereopsis, fusional vergence, vergence facility, near point of convergence, accommodative amplitude and facility tests, and developmental eye movement test was administered to the patient when indicated. However, these tests results are not reported as these data were not available for all patients.
A post-therapy evaluation visit was conducted after every 5 therapy sessions. For patients who received evaluations more than once (i.e., patients who attended 10 or 15 therapy visits), only the test data from the last therapy visit were used for analysis.
The Office Control Score was measured at 5 m and 33 cm. The score ranged from 0 (phoria, best control) to 5 (constant tropia, worst control). Based on the proportion of time that manifest exotropia was present during a 30-second observation period before any dissociation, a control score of 3–5 was assigned. When no manifest exotropia was present during this observation period, a control score of 0–2 was assigned based on the time to regain motor fusion after dissociation.30
TreatmentAll patients received office-based vergence/accommodative therapy administered by a trained therapist during a 60 min office visit every one to two weeks, combined with procedures to practice at home for a minimum of 15 min, five times per week. Office therapy was performed by authors MMM, CC, and CS and was on a one to one therapist/patient ratio. The treatment sequence used in this study was modified from the treatment protocol previously used in the Convergence Insufficiency Treatment Trial randomized clinical trial.33 In addition to the accommodative and near vergence techniques from the original protocol, distance vergence, oculomotor and anti-suppression were incorporated.34 The therapy procedures used are described in detail elsewhere34,35 and are listed in Table 1. Anti-suppression was not performed at the discretion of the first author if it was deemed likely to worsen a patient’s symptoms. For example, if debilitating diplopia was present at the baseline visit, anti-suppression was not performed. The length of vision therapy was determined based on the experience of the first author, patient’s time and financial factors, and patient’s binocular vision test result (e.g., office control score, positive fusional reserve and suppression test). It is noteworthy that some patients received only 5 sessions of vision therapy, which is less than the recommended amount.36 The major reasons for a short therapy duration included financial reasons, a lack of time by patients or their parents or a lack of any apparent improvement judged by examiner and/or parents.
Office-based vergence/accommodative therapy procedures.
| Phase one | Anti-suppression at near | Cheiroscopic drawing with single oblique stereoscope |
| Anti-suppression at distance | Red/Green glasses and penlight | |
| Gross convergence | Voluntary convergence | |
| Brock string | ||
| Barrel card | ||
| Near vergence | Vectograms (Quoits) | |
| Accommodation | Letter chart accommodative facility | |
| Loose lens accommodative facility | ||
| Saccades | Monocular hand held prism jump | |
| Hart chart saccades | ||
| Phase two | Vertical prism dissociation and hart chart | |
| Vis-à-vis | ||
| Anti-suppression at distance | Red/Green anti-suppression chart | |
| Near Vergence | Vectograms (Clowns) | |
| Distant Vergence | Free space fusion with eccentric circles | |
| Accommodation | Letter chart accommodative facility | |
| Loose lens accommodative facility | ||
| Saccades | Hart chart saccades | |
| Phase three | Near vergence | Vectograms jump vergence |
| Aperture Rule | ||
| Free space fusion with eccentric circles | ||
| Distant vergence | Free space fusion with eccentric circles | |
| Phase four | Near vergence | Aperture rule with prism flipper |
| Eccentric circles jump vergence | ||
| Sports fixation card (rotation and version) | ||
| Cover and uncover with prism | ||
| Distant vergence | Free space fusion with first degree fusion target and prism flipper | |
| Cover and uncover with prism | ||
| Accommodation | Polaroid bar reader with accommodative flippers | |
| Aperture rule with accommodative flippers |
No deliberate overminus lens or therapeutic occlusion was provided as these two approaches are not common treatment modalities for intermittent exotropia in China. However, hyperopic patients were prescribed an under-plus lens to stimulate the accommodative convergence. All patients worn the same optical correction throughout the entire therapy program. No patient received strabismus surgery during the therapy.
Primary and secondary outcome measuresThe primary outcome measure in this study was the change in the Office Control Score from the pre-therapy visit to the post-therapy visit. The secondary outcome measure was the change in the size of deviation. The hypothesis was that office-based vergence/accommodative therapy would significantly improve the Office Control Score.
Statistical analysisNormality of data was tested by the Shapiro–Wilk test. For parametric data, two-tailed paired t-tests were used to evaluate the outcome measures. Cohen’s D score effect sizes were presented when there was a significant finding. For non-parametric data, Wilcoxon signed-rank tests were used. Effect sizes (calculated by dividing the z value by the square root of number of observation) are presented when there was a significant finding. The significance level was 5% for all tests.
ResultsA total of 40 patients aged from 5 to 22 years old satisfied the inclusion criteria of this study. Their characteristics are shown in Table 2. Patients in this study received 8.6 ± 2.4 therapy sessions on average. Eight patients received strabismic surgery before the initiation of vision therapy, and they all underwent only one surgery. All patients treated with surgery had intermittent exotropia before surgery. The average time between the surgery and the start of vision therapy was 2.9 ± 1.3 years. Data on office control score were non-parametric while prism and alternate cover test data were parametric.
The study population demographics and clinical measures at the first and last follow-up visits.
| Characteristic | All patients (n = 40) | Unoperated (n = 32) | Operated (n = 8) | |||
|---|---|---|---|---|---|---|
| Pre-therapy | Post-therapy | Pre-therapy | Post-therapy | Pre-therapy | Post-therapy | |
| Male, n (%) | 24 (60%) | Not applicable | 18 (56%) | Not applicable | 6 (75%) | Not applicable |
| Age at the first therapy session, years, mean ± SD | 8.8 ± 3.7 | Not applicable | 9.0 ± 3.4 | Not applicable | 7.8 ± 4.5 | Not applicable |
| Cycloplegic objective refraction, right eye spherical equivalent, diopter, mean ± SD | −0.14 ± 2.44 | Not applicable | −0.27 ± 2.56 | Not applicable | 0.36 ± 1.79 | Not applicable |
| Cycloplegic objective refraction, left eye spherical equivalent, diopter, mean ± SD | 0.03 ± 2.41 | Not applicable | −0.09 ± 2.59 | Not applicable | 0.50 ± 1.37 | Not applicable |
| Number of patients who received strabismus surgery before vision therapy | 8 (20%) | Not applicable | 0 (0%) | Not applicable | 8 (100%) | Not applicable |
| Distance prism and alternate cover test exodeviation, prism diopter, mean ± SD | 15.1 ± 8.1 | 14.8 ± 8.4 | 15.2 ± 8.5 | 14.6 ± 9.1 | 14.8 ± 5.9 | 15.9 ± 4.6 |
| Near prism and alternate cover test exodeviation, prism diopter, mean ± SD | 18.0 ± 8.8 | 14.3 ± 8.2 | 17.7 ± 8.6 | 13.3 ± 8.1 | 19.1 ± 9.3 | 18.3 ± 7.0 |
| Office Control Score at distance, mean ± SD | 2.9 ± 1.9 | 1.7 ± 2.1 | 2.8 ± 1.9 | 1.7 ± 2.1 | 3.0 ± 1.8 | 1.7 ± 1.9 |
| Office Control Score at near, mean ± SD | 1.7 ± 1.6 | 0.6 ± 1.2 | 1.9 ± 1.7 | 0.6 ± 1.3 | 0.8 ± 0.7 | 0.3 ± 0.4 |
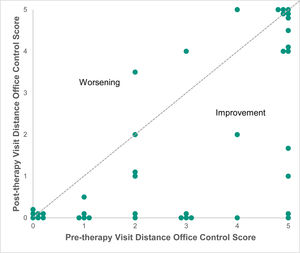
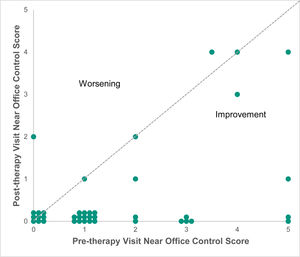
After treatment, there was a change of −1.1 ± 1.6 (p < 0.001, z = 3.73, effect size: 0.42) and −1.1 ± 1.4 (p < 0.001, z = 4.26, effect size: 0.48) in distance (Fig. 1) and near (Fig. 2) Office Control Score, respectively.
Although there was no significant change in the angle of distance exodeviation (p = 0.63) after treatment, a significant change was observed in the near angle (−3.7 ± 5.6 prism diopters, p < 0.001, effect size: 0.44).
In the subgroup analysis of unoperated patients, there was a change of −1.1 ± 1.6 (p < 0.001, z = 3.41, effect size: 0.43) and −1.3 ± 1.5 (p < 0.001, z = 4.75, effect size: 0.59) in distance and near Office Control Score, respectively. A change of −4.4 ± 5.5 prism diopters (p < 0.001, effect size: 0.53) was observed in near angle, while the distant angle remained unchanged (p = 0.30).
A similar trend was also observed in operated patients. There was a change of −1.3 ± 1.4 (p = 0.001, z = 3.29, effect size: 0.82) and −0.5 ± 0.5 (p = 0.001, z = 3.29, effect size: 0.82) in distance and near Office Control Score, respectively. Both the near (p = 0.71) and distant angles (p = 0.42) remained unchanged.
DiscussionThe results of this study indicate that office-based vergence/accommodative therapy was effective for improving the control of intermittent exotropia in both operated and unoperated patients in a private practice environment. This study also demonstrated that the Office Control Score can be implemented in a private practice environment.
There are numerous reports suggesting that vision therapy is effective in treating intermittent exotropia.7–13 However, previous studies usually used multiple criteria to judge the effectiveness of vision therapy. These criteria often varied across studies, making meaningful comparisons difficult. It is noteworthy that there is only one study of vision therapy11 in the literature that employs a standalone outcome measure for control ability. That study classified the control ability as good, moderate or poor control based on the frequency with which exodeviation was decompensated. They showed that their treatment group, in which fusion exercises were provided, demonstrated improvement in distance stereopsis, fusional vergence and the control of distant deviation. However, it should be pointed out that their assessment and grouping method for control ability was not validated. Mohney et al. developed the Office Control Score in 2006.30 Due to the fact that this scale is validated,31,32 has clear scoring criteria, and was used in previous randomized clinical trials,2,3,6 it was used as the primary outcome measure in the current study. Previously, it was shown that the Office Control Score improved by 1.2 and 0.3 with over-minus lens and part-time patching, respectively.2,6 According to our data, the effect of vision therapy (i.e., an improvement of 1.1 in control score at distance and near) was at least comparable to that of over-minus lens method. These significant improvements were found in both operated and unoperated intermittent exotropes both at far and near.
Some may argue that if the effect of overminus lens is similar to that of vision therapy, there is no rationale for practitioners to prescribe the latter approach, which usually requires more time, money and effort. First of all, over-minus lens is usually believed to be a temporary compensatory approach to improve the control of exodeviation through additional accommodative convergence. It was reported that 83.3% of the patients who achieved good control with an over-mins lens still required over-minus lens or base-in prism after 5 years of over-minus lens use.37 On the other hand, there is report indicated that the effects of vision therapy are long lasting. 38 Secondly, there are cosmetic issues related to spectacle wear. Thirdly, researchers and many parents in China are very concerned that the use of over-minus lens will cause myopia development or progression. Whether this is the case remains unknown in the Chinese population, although there is an indication that this does not happen in the Caucasian population.37
Regarding the improvement of the near angle size, its averaged reduction was only 3.7 prism diopters, therefore it is arguable whether it is clinically significant or not. Based on test-retest data, previous researchers have suggested that only a change of ≥10 prism diopters should be regarded as clinically significant.39 However, it should be noted that clinically it is not uncommon to observe a substantial reduction in the near angle size after vision therapy. For example, in this study population, the maximum reduction in the near angle was 20 prism diopters, and seven patients showed a ≥10 prism diopter reduction in the near angle. This improvement could be due to tenacious proximal convergence40 or slow vergence.10,41 Notably, these follow-up data were obtained immediately after the therapy was completed and therefore we are unsure of the long term effects. We believe that after prolonged occlusion, this apparent improvement will probably disappear. However, given that the change was substantial in some patients, it would be worthwhile to study whether patients benefit from this apparent change (i.e., Will it be easier to fuse the images by fusional vergence as the size of deviation is reduced?).
There are limited reports suggesting that vision therapy before or after surgery is beneficial.42,43 Qiu42 reported that postoperative binocular vision training was helpful for the recovery of binocular vision as measured by a synoptophore. They also reported that the deterioration rate (i.e., the deviation angle increased by >10 prism diopters at the 12-month follow-up compared to that at the 1-week follow-up) in the training group (11.5%) was significantly lower than that in the control group (35%). Their training is consisted of home-based exercises provided by computer software, but the authors did not provide any detail on what type of exercise was included in this software. Unfortunately, the deviation angle and control ability before and after treatment were not reported in their article. These two parameters are important for evaluating intermittent exotropia, and researchers have suggested that these parameters should be reported in studies in this field.44 In addition, the lack of this information precludes us from knowing the baseline characteristics of those who will be benefited from postoperative vision therapy. In another retrospective analysis by Figueira43 that aimed to identify the best treatment option for intermittent exotropia, it was reported that surgery combined with preoperative orthoptic/occlusion therapy achieved the highest successful treatment rate at the 5 year follow-up (84.6%) when compared to surgery alone (25%). Success was defined as orthophoria or <10 prism diopters esotropia/exotropia at distant and near with good stereoacuity and cosmesis. These two studies indicate that vision therapy is beneficial when combined with surgical treatment. This hypothesis was also supported by our data. Our data directly demonstrated how vision therapy improved the control of exodeviation at distance (an improvement of 1.3 in the Office Control Score) and near (an improvement of 0.5 in the Office Control Score) in patients who previously underwent surgery. This improvement may help to explain the reduction in the deterioration rate observed in the two studies mentioned above.42,43
The main strength of this study was its use of validated scoring criteria to assess the control of intermittent exotropia. Potential weaknesses included the score being measured only once but not thrice.32 The study was retrospective in nature. It should also be noted that the patients included in this study were only those patients whose condition was severe enough to seek consultation from our clinic or be referred by their eye care practitioners. Patients with poor prognosis for vision therapy were not included in this study. These prognostic factors included but were not limited to large horizontal deviation (i.e., >35 prism diopters), poor compliance, and a young age (i.e., younger than 5 years old). There is a lack of control group (e.g. placebo therapy) and masking for both examiners and patients thus there is potential for bias. For example, the enthusiasm and compassion of a therapist during therapy may lead to a placebo effect. The sample size of the operated group was also small.
ConclusionIn conclusion, this study showed that office-based vergence/accommodative therapy with home reinforcement significantly improved the control of exodeviation in both operated and unoperated intermittent exotropia patients in a private practice environment. Eye care practitioners should consider vision therapy when treating intermittent exotropia. Our preliminary results warrant further investigation, such as randomized controlled clinical trials, into the effect of vision therapy on intermittent exotropia. The impact of postoperative vision therapy on the prognosis of intermittent exotropia (i.e., reducing the chance of recurrence and need for reoperation) should also be studied in greater detail.
Disclosure of funding sourcesNone.
Conflicts of interestMartin Ming-Leung Ma, Chao Chen, Cuiyun Su, Zhen Tian, Meihua Le are employees of the private optometric clinic, Bright Vision Clinic, mentioned in this report.
A preliminary version of this paper was presented at the conference of American Academy of Optometry 2019, Orlando, United States.