Vitamin D is good for bones and teeth. It may also have a role in preventing and treating diabetes, certain cancers, atherosclerosis, multiple sclerosis, hip fractures and ocular conditions such as age-related macular degeneration.
La Vitamina D es buena para los huesos y dientes. También puede jugar un papel importante en la prevención y tratamiento de la diabetes, ciertos cánceres, ateroesclerosis, esclerosis múltiple, fracturas de cadera y situaciones oculares tales como la degeneración macular asociada a la edad.
Activated vitamin D (calciferol) is a fat-soluble hormone-like essential vitamin that was discovered by Professor Edward Mellanby in 1922. The kidney makes calcitriol to help regulate the calcium and phosphorous economies (endocrine function), thus preventing skeletal diseases. The German organic chemist Adolf Windaus won the Nobel Prize by isolating this vitamin in 1926. We now know that vitamin D also regulates cells, systems and organs throughout the body. It is the only vitamin formed with the help of sunlight.
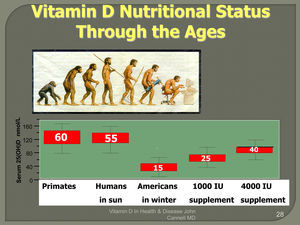
Vitamin D synthesis begins when 7 dehydrocholestrol in the skin is converted to pre-vitamin cholcalciferol by UV B radiation (290–320nm). This precursor molecule is then converted to the diagnostically important non-active storage form called 25-hydroxycholcalciferol (also called 25 (OH) D, or 25-hydroxyvitamin D), via hydroxylation in the liver. An average person maintains a 60-day supply of 25 (OH) D. Biologically active calciferol, less important to ascertain from the clinical diagnostic standpoint, results from the second hydroxylation at the kidneys (1,25 dihydoxyvitamin D). Calciferol is activated at peripheral tissues, such as the brain, directly by the enzyme 1 alpha hydroxylase. That is, tissues all over your body activate calcitriol for local use. The amount of calcitriol available for these paracrine and autocrine functions depends on your 25 (OH) D level. This sunlight driven process is how 90% of pre-industrial people obtained their supply of vitamin D.1
The two dietary biologically inactive vitamin D precursors include vitamin D2 (ergocalciferol) from plants and vitamin D3 (cholcalciferol) from marine life (Table 1). Vitamin D3, along with crucial essential fatty acids, is especially abundant in cold-water fish (i.e. red wild sockeye salmon and sardines. The less potent vitamin D2 is used to fortify milk. For example, the 2010 USDA Dietary Food Intake Guidelines recommends the equivalent of 3 glasses or 24 ounces/day, supplying a meager 300IU of this less potent plant-based and synthetic vitamin D2.2,3 There is growing consensus that milk sources are simply not enough to maintain overall health for Caucasians, let alone African Americans and populations living further from the equator.2,3
1000IU vitamin D daily is safe for most patients. Potential benefit outweighs potential harm.
| 3 ways to get vitamin D: Food, sun, and supplements9 | Source | Amount |
| Food | 1 cup of fortified milk | 100IU vitamin D3 |
| One serving (3.5 oz) of oily fish (salmon, tuna, sardines, mackerel or herring) | 200–300IU vitamin D | |
| Sun (ultraviolet B radiation) | Expose face, arms, hands, or back for 10–15min (without sunscreen) at least twice a week during summer months or in warm climates | 3000IU vitamin D3 per exposure |
| Supplements | Vitamin D3 | 1000IU/day |
| Vitamin D2 | 50,000IU every 2–4 weeks |
The Food and Nutrition Board (FNB) at the Institute of Medicine of the National Academies established a Recommended Dietary Allowance (RDA) in 2010, modestly increasing their equivalent vitamin D dose recommendations.3 An RDA represents the average daily level of intake believed to be sufficient to meet the nutrient requirements of 97–98% of healthy people and are listed in both International Units (IU) and micrograms (mcg). The new 2010 RDA for vitamin D is based on age, but unfortunately still makes no allowance for race, gender, season or geographic location:
1–70 years 600IU (15mcg)
70 years 800IU (20mcg)
One full-body summer sun exposure (one MED) delivers 20,000IU to the systemic circulation of Caucasians at southern latitudes. It takes 200 glasses of milk or 50 typical multivitamin tablets (400IU) to do the same. The season, latitude, time of day, cloud cover, smog, and sunscreens all affect UV B exposure. For example, a sunscreen protection factor of 8 or higher blocks vitamin D synthesis. Special populations vulnerable to lack of sunlight include those living in northern climates, people of color, indoor workers, infants and the housebound elderly, as well as patients advised by their doctors to avoid sunlight. Can the degree of UV B sunlight exposure based on one's latitude, working environment (office worker vs. forester) or even race determine one's health status? Can living in a northern country such as Canada be a health hazard? Can taking a winter sun-drenched vacation be as healthy as visiting a doctor? Can over-zealous application of sunscreen worsen one's overall health? This all appears to be true according to the www.vitaminDcouncil.org and leading scientists.4
Vitamin D is actually a pre-hormone – like vitamin that regulates cells, tissues, organs and systems. In fact, it is the most potent steroid hormone in the human body. Deficiency, thus far, has been linked to 17 types of cancer, cardiovascular disease, diabetes, multiple sclerosis, schizophrenia and even influenza (the flu).2,4,5 The degree of autism has been found in one study to vary with distance from the equator. Ricketts in African Americans has returned to inner city Chicago area hospitals. This is conjectured to be related to a combination of factors, including the 24/7 indoor – service economy, omega-3 deficient fast food, and relinquishing the ethnic tradition of providing children with cod liver oil. This review will bring you up to date (Fig. 1).
(Image courtesy, Bill Sardi, Knowledge of Health, San Dimas, CA).
Vitamin D synthesis in skin occurs only when the UV index is 3 or higher, roughly the period around noon from March to October in southern parts of the country. A rule of thumb is that if your shadow is longer than you are, the sunlight is not intense enough.
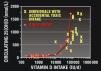
The 25 (OH) D blood test, a biomarker for Vitamin D reserves, is an inexpensive and widely available blood test. Liver stores are affected by environmental factors such as latitude, season, diet, medications and personal sunning behavior. While a loin-clothed equatorial man would be expected to have a 25 (OH) D of 20ng/ml, the typical normative laboratory reference range is 30–100ng/ml with optimal values occurring mid-range at 40–60ng/ml. Any 25 (OH) D liver- reserve value below 20ng/ml is considered deficient (Fig. 2).
The EvidenceCancer and vitamin D – i.e. breast, prostate, colon and other cancersVitamin D is now recognized as an effective regulator of cell growth and differentiation in a number of different cell types, including cancer cells. Vitamin D interacts directly with 2.5% of the human genome or some 1000 genes, working like a master on-off switch.1 Researchers believe a deficiency of this vitamin leads to a deficit of proteins manufactured under the direction of these genes, which then undermines a cell's key defenses. Recently, vitamin D supplementation has been linked to an astonishing 60–77% decrease in all cancer risk in females, according to a 4-year “gold standard” study of cancer mortality in 1180 Nebraska women over the age of 55.5 The estimated relative risk reduction was dramatic (0.23) and the 95% confidence interval was 0.09–0.60, meaning that the true relative risk reduction has a 95% probability of being in the range of 40–91%. The P value of <.005 suggests that the probability of this finding occurring by chance alone is less than 1 in 200.6 Lappe et al. predict a 35% reduced breast cancer risk for every 10ng/mL increase in serum 25(OH) D.5 Equally dramatic are values associated with prognosis of prostate cancer. Serum levels of 25(OH)D in n=160 men were classified as deficient (<20ng/ml), insufficient (20–32ng/ml) or adequate (>32ng/ml). Insufficient 25(OH) D (OR 0.33; 95% CI 0.14–0.77), or adequate (OR 0.16; 95% CI 0.05–0.43) serum levels were dramatically related to better prognosis compared with the lowest level.
Vitamin D is also related to overall cancer risk in males. In the Health Professionals Follow-up Study, cancer mortality was followed in a cohort of 47,800 men, from 1986 until 2000. Low levels of Vitamin D were associated with an increased incidence of both cancer and mortality.7 Another study found people with the highest levels of Vitamin D reserves had four times less colon cancer than people with the lowest levels The same study estimated the dose to cut colon-cancer risk in half as only 1000IU D3 daily.8–10 The amount of Vitamin D estimated to cut breast-cancer risk in half is 4000IU daily.11 In summary, Vitamin D is known to have cancer protective effects at the cellular level and prior population based studies support this association.5 “The Canadian Cancer Society has recently suggested citizens supplementing with at least 1000 units of Vitamin D. The American Cancer Society? “Mum's the word,” according to Bill Sardi, a consumer health advocate and journalist.12
Cardiovascular disease and vitamin DMechanistically, Vitamin D works against arteriolosclerosis in six distinct ways: (1) inhibition of vascular smooth muscle proliferation; (2) suppression of vascular calcification and depression of parathyroid hormone; (3) down regulation of pro-inflammatory cytokines such as C reactive protein; (4) up regulation of anti-inflammatory cytokines; (5) negative endocrine regulation of the renin-angiotensin system and (6) lowering insulin resistance.13
In the Framingham Study (1996–2001), both hypertension and low Vitamin D were found to worsen cardiovascular risks.14 The current paradigm is that heart disease is caused by a combination of genetics, hypertension, diabetes, high cholesterol, smoking, obesity, physical inactivity, and diet. A paradox is a fact that contradicts the paradigm, and the current “cholesterol hypothesis” appears to be waning. For example, when the current paradigm is applied to British men for ten years, the researchers found 84% of the heart disease occurred in the men classified as low risk! Furthermore, 75% of the men classified as high risk were still free of heart disease ten years later. It seems the “cholesterol hypothesis” is missing a few variables. Vitamin D deficiency, in fact, doubles the risk of myocardial infarct (MI), cerebrovascular accident (CVA) and heart failure over a mean of 5.4 years in patients with hypertension. Optimal Vitamin D status attenuates age-associated increases in systolic blood pressure (SBP). Sufficient concentrations of 25(OH) D>32ng/ml decreased the age-related increase in systolic blood pressure by 20% compared with participants having deficient 25(OH) D concentrations <20ng/ml (P<0.001). Furthermore, only 8% of blacks had sufficient 25(OH) D concentrations >32ng/ml.15,16
A Vitamin D deficiency is far more predictive of a future heart attack than cholesterol status, says a report of 18,255 American men published in the Archives of Internal Medicine on June 9, 2008. High cholesterol combined with a Vitamin D deficiency increased the risk of a heart attack by about 2.4 times, but a Vitamin D deficiency alone accounted for 2.0 times that risk, or 83% of the entire increased risk.17
Type 1 and type 2 diabetes mellitusAmong children under 14, Canadians are believed to have the 3rd highest rate of diabetes type 1 in the world. A youngster growing up in Finland is about 400 times more likely to develop the lifelong ailment involving insulin deficiency than one growing up in Venezuela.18 Researchers from the University of California, San Diego, found that the incidence of diabetes tends to be low at or near the equator, where the rate often approaches zero, and then rises steadily at progressively higher latitudes, reaching peaks in places like Canada, Finland and southern Argentina's Tierra del Fuego. This “would revolutionize”, I think, pediatric preventive medicine practice by allowing the doctors to ensure adequate Vitamin D status and prevent a terrible, lifelong disease,” said Dr. Garland, one of the study's authors.18,19
Vitamin D deficiency has also been associated with insulin deficiency and insulin resistance.20,21 The higher the vitamin D level, the lower the blood glucose.21,22 Furthermore, obesity, diabetes and the Syndrome X or “Metabolic Syndrome” all appears influenced by Vitamin D deficiency.22,23 Vitamin D reduces the secretion of leptin, a hormone produced by fat cells, which is thought to signal the brain when the fat cells are “full”.24,25 Obesity by itself probably worsens Vitamin D deficiency due to decreased bioavailability from the skin and diet. This is because Vitamin D is held in body fat.25–27 Weaker pancreatic function and inflammatory pancreatitis are also related to Vitamin D's action as an immunosuppressant.21,23
Skeletal disease, muscle tone and enhanced athletic performanceVitamin D's classic role is aiding the absorption of calcium and phosphorous, which along with vitamin K2, magnesium, zinc, boron and essential fatty acids helps form and maintain bone mineralization. Without Vitamin D, bones become thin, weak, brittle, soft, or misshapen (i.e. rickets in children or osteomalacia in adults). Fortification of milk products (400IU D2 per quart of milk) in the 1930s largely eliminated rickets as a major public health concern in the United States. Nonetheless, in the past 10 years, physicians have been seeing an increase in the number of infants diagnosed with Vitamin D deficiency rickets, a disease once considered virtually nonexistent. The Canadian Pediatric Society recommends that pregnant and nursing women take a 2000IU Vitamin D supplement during the winter to protect themselves and their infants from rickets.28
As many as 25 million adults in the United States, the majority women, are at risk of developing osteopenia and full blown osteoporosis or fragile bones. Increased risk of bone fractures (i.e. hip fracture, also related to decreased visual contrast sensitivity) is also related to higher mortality rates. Keep in mind that it may take 30 years or longer for these latter skeletal diseases to manifest in a long latency condition such as Vitamin D deficiency. A group from Minnesota found that 100% of elderly patients admitted for fragility fractures were Vitamin D deficient despite the fact that half of them were taking Vitamin D supplements. The authors found that women taking supplemental Vitamin D had deficient average levels of only 16.4ng/ml while women not taking supplements had levels even lower at 11.9ng/ml, both dangerously low. None of the 82 women received adequate sun or sufficient dietary Vitamin D to obtain a desirable level of 40ng/ml. These were fragility fractures, not fractures caused by unusual trauma – their bones just fell apart.29 Clinical studies now justify increased emphasis on Vitamin D supplementation beyond the RDA, as well as calcium/magnesium 2:1 recommendations for at-risk individuals. A meta-analysis of 68 studies concluded, “oral Vitamin D supplementation between 700 and 800IU/d appears to reduce the risk of hip and non-vertebral fractures in ambulatory or institutionalized elderly persons. “An oral Vitamin D dose of 400IU/d (found in a pabulum multivitamin) is simply not sufficient for fracture prevention in Caucasians.”30
Researchers at the Institute of Physical Medicine, University Hospital Zurich, Zurich, Switzerland, cite that Vitamin D has other geriatric health benefits including reduced risk for falls, reduced admission to nursing homes, cancer prevention, lowering high blood pressure and even fewer dental cavities. The most advantageous serum levels were at least 30ng/ml, with a higher optimal range for cancer prevention of 36–48ng/ml.31 This translates to more than the suggested 3000IU/day in the Archives of Internal Medicine June 2008 study. Vitamin D appears to boost athletic performance as well. “There's just clear evidence, especially in the German literature, of quicker reaction time, balance, muscle strength, endurance – all improve with Vitamin D and this may explain why senior citizens on Vitamin D are less likely to fall and hurt themselves” according to John Cannell, MD.12
Multiple sclerosisThere exists a well-known association between multiple sclerosis (MS) prevalence and latitude. An unknown viral vector has been hypothesized to explain this enigma. In the US, MS rates are four times higher in northern states than in the southern parts of the country. Higher circulating levels of 25-hydroxyvitamin D have been associated with a lower risk of MS among Caucasians.32 Similarly, Australian research shows the incidence of MS increases the farther people live from the equator. The highest MS incidence rates in the world are found in Northern Europe and Canada. One explanation is that Vitamin D mediates a shift to a more anti-inflammatory immune response, in particular to enhanced regulatory T cell functionality.33
Obstetrics, autism and the vitamin D autism hypothesisDuring the two decades of sun-avoidance advice, Vitamin D recommendations did not change for pregnant women or their children. There was no effort made to compensate for the Vitamin D deficiency such advice would predictably induce. IOM recommendations stayed the same, that is, 200IU per day for infants, children, and pregnant women. Gestational Vitamin D deficiency is associated with a significantly increased risk of neonatal pneumonia,34 a doubled risk for preeclampsia,35 a tripled risk for gestational diabetes,36 and a quadrupled risk for primary cesarean section.37
The “Vitamin D deficiency – Autism Hypothesis” has appeared recently in scientific journals. That Vitamin D is both a steroid as well as a neuro-steroid, suggests it modulates both the maternal immune system status during pregnancy as well as fetal brain development.38 The robustness of this parsimonious hypothesis is that it explains and encompasses all existing facts and competing autism hypotheses. These include (1) high monozygotic twin concordance rates with epigenetic environmentally determined variations in neuropeptide levels during pregnancy/infancy creating varying autism spectrum phenotypes; (2) vaccine challenge to a weakened immune system unable to detoxify heavy metals due to Vitamin D deficiency induced down-regulation of neural glutathione, at the time toddlers would be off formula and expected to become Vitamin D deficient; (3) increased prevalence of the disease in the African American community and among newly arrived Ethiopian immigrants living in Minnesota (4) Increased prevalence at northern latitudes (Alabama least, New Jersey most); (5) The coincident increase in Vitamin D deficiency during the last 20 years, as a result of over-zealous sun-protection, sequestering children indoors, and a shift to indoor video/computer screen activities, especially for boys; (6) The discrepant effects of sex steroids on calcitriol neuropeptide metabolism, explaining the 4:1 male autistic gender enigma; (7) William's syndrome, a chromosome 7 disease, often results in Vitamin D excess. These children display the opposite phenotype of those with autism –empathetic, socially engaged with superior eye contact skills.39,40 If this hypothesis is true, it might be possible to protect pregnant females with sunlight/supplements while providing 1000IU Vitamin D drops to their infants. All optometrists and non-optometric clinicians should be aware of this important hypothesis.
The flu, winter mortality, auto-immune disease, schizophrenia & chronic fatigueFlu and even the death rates from heart attack rise in the winter and at higher latitudes.41,42 Rheumatoid arthritis and autoimmune diseases such as fibromyalgia and Chrohn's have now been linked to vitamin D deficiency. Chronic low-level sunlight exposure normalizes immune function and enhances immune cell production, reducing abnormal inflammatory responses found in these disorders, and reduces occurrences of infectious disease.43–45,23. Progression of degenerative arthritis of the knee and hip is faster in people with lower Vitamin D 25 (OH) liver reserves.46,47 There is some evidence that the side effects of steroids might even be modulated with judicious Vitamin D supplementation.
The incidence of schizophrenia has been found to be related to prenatal sunshine as Vitamin D is a known brain growth and development modulator.48 Activated adrenal gland Vitamin D regulates tyrosine hydroxylase, the rate-limiting enzyme necessary for the production of dopamine, epinephrine and norepinephrine. Low Vitamin D also contributes to chronic fatigue and depression.49 Seasonal affective disorder has been treated successfully with Vitamin D. In a 30-day study comparing Vitamin D vs. 2h daily use of ‘light boxes’, depression completely resolved in the Vitamin D group, but not the light box group.50
Researchers from Ireland were the first to demonstrate that Vitamin D acts as an anti-inflammatory agent and turns old rat brains into young brains – at least as far as inflammatory cytokines are concerned, suggesting Vitamin D may prevent, or even treat, age-related cognitive decline in humans.51,52
Surviving the intensive care unitVitamin D has immunomodulating and antimicrobial properties through antimicrobial peptides such as cathelicidin.1 A retrospective study was under taken to evaluate if Vitamin D deficiency was associated with less than optimal ICU outcomes in veterans. The study included 136 veterans with 25(OH) D levels drawn within a month of admission to ICU to the Mountain Homes Veterans Affairs Medical Center. The average 25(OH) D level were insufficient at 24.6ng/ml with 38% of patients falling in the Vitamin D—deficient category. ICU survivors had a significantly lower rate of Vitamin D deficiency compared with non-survivors (28% versus 53%). Twenty-nine percent of Vitamin D replete patients were in ICU 3 days or more, whereas 58% of patients with Vitamin D deficiency stayed in ICU 3 days or longer. This difference was highly significant translating to twofold increased risk (OR=2.0) for 3-day or longer stay in ICU for patients with Vitamin D deficiency. Moreover, the risk of death was significantly higher in ICU patients with Vitamin D deficiency (OR=1.81). Obtaining adequate 25 OH Vitamin D levels in patients with critical illness enhances post ICU survival.53
The eye and secondary manifestations of system disease, ocular infectious disease and age related macular degeneration (AMD)Most Vitamin D associated conditions (i.e. cardiovascular disease, diabetes, multiple sclerosis, inflammatory and neoplastic disease) have secondary ocular manifestations and thus potential for sight threatening complications. There is also at least a theoretical postulation between impaired immunity and diseases of the cornea such as herpes simplex and varicella zoster reactivation as well as acanthamoeba keratitis.54
There are several epidemiological studies suggesting an association between Vitamin D deficiency and AMD. A 2007 study suggested Vitamin D may protect against age-related macular degeneration (AMD). The odds ratio (OR) and 95% confidence interval (CI) for early AMD among 7752 participants, 11% of who had AMD, in the highest vs. lowest quintile of serum Vitamin D was 0.64 (95% CI, 0.5–0.8; P trend <.001). Levels of serum Vitamin D were inversely associated with early AMD but not advanced AMD. The researchers speculated that beneficial effects of Vitamin D might be via an anti-inflammatory effect.55 As well, a more recent study of Vitamin D status and early AMD in 1313 postmenopausal women with complete ocular and risk factor data suggested among women younger than 75 years, intake of Vitamin D from foods and supplements was related to decreased odds of early AMD in multivariate models. No relationship, however was observed with self-reported time in direct sunlight.56 Seddon et al. evaluated monozygotic twin pairs with discordant AMD phenotypes to assess differences in behavioral and nutritional factors. The twin with the earlier stage of AMD, smaller drusen size and area, and less pigment had higher dietary Vitamin D, betaine, or methionine intake. These results suggest that behavioral and nutritional factors associated with epigenetic mechanisms are involved in the etiology of AMD, in addition to genetic susceptibility.57
In a cross-sectional study of 517 patients, Vitamin D deficiency was associated with an increased prevalence of retinopathy in young people with type 1 diabetes. The inflammatory and angiogenic effects of Vitamin D deficiency may contribute to early retinal vascular damage; however, further investigations are warranted.58 The results of a clinic-based, cross-sectional study on 221 subjects suggests that patients with type 2 diabetes, especially those with PDR, have lower 25(OH)D levels than those without diabetes. Patients with type 1 diabetes and those taking >1000IU of Vitamin D daily were excluded from the analyses.59 Whether Vitamin D supplementation in diabetic patients can prevent or improve the prognosis for retinopathy remains to be investigated.
Mutti found that myopes had lower levels of blood Vitamin D by an average of 3.4ng/ml compared with non-myopes when adjusted for age and dietary intakes (P=0.005 for refractive error group, model R=0.76). Adjusted for differences in the intake of dietary variables, myopes appear to have lower average blood levels of Vitamin D than non-myopes. Replication in a larger sample is needed to establish a stronger association.60
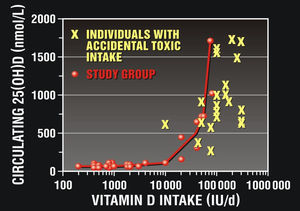
Vitamin D toxicityThe IOM (Institute of Medicine) pegs toxicity level @150ng/ml with a Tolerable Upper Intake level of 4000IU/day for adults and children older than 1 year. This is considered by many as overly conservative, dangerous and too low by a factor of five. Scientists have demonstrated that only intake levels at of 20,000–40,000IU (0.5–1mg) and above over several months is risky.61,62 see Fig. 3. Though rare, those with diseases that increase serum levels (such as mild to moderate renal failure) and those with chronic granulomatous diseases (such as sarcoidosis) are considered to be at higher risk of developing Vitamin D toxicity at lower doses. More common and notable is the risk of Vitamin D deficiency from the environmental and racial factors discussed as well as iatrogenic poly pharmacy. There are a plethora of different classes of medications, most notably the chronically used OTC and Rx acid blockers that significantly inhibit Vitamin D absorption, as well as the carotenoids, vitamin E and B vitamins all of which are crucial for properly functioning eyes.63 Malabsorption syndromes and mild or moderate hepatic failure would also decrease rather than increase serum levels.
Safety of excessive sun exposure and sunscreen recommendationsIs there a dark side of Vitamin D in terms of skin cancer risk, particularly for Caucasians? The American Academy of Dermatology Web site finds it “appalling” that “anyone in good conscience could make the claim that intentional sun exposure - for any length of time - is beneficial.” The latest recommendation “For day, wear sunscreen and consider using products containing antioxidants because they also have sun-protection properties”.64 Prior sunburns are associated with melanoma risk and reoccurrence with a mortal US risk of 8000 persons per year.65 However, there is now scientific evidence for an increased risk of melanoma beyond 40-degree latitude in users of sunscreen, entirely inconsistent with the UV dermal damage hypothesis.66
Clinicians certainly should not abandon their recommendations to avoid extended periods of unprotected harsh mid-day sunshine. This also places a patient at higher risk for cataracts and AMD. Few would disagree with the judicious use of sunscreen, wide brimmed hats and wrap around sunglasses, particularly in the young. However, the recommendations to completely avoid sunlight and zealously and immediately apply UV B sunscreen appear particularly misplaced in an age of 24/7 urban indoor work, darkening US racial patterns, poly pharmacy, and low D3 intake afforded by the current 2010 RDA. Indeed, while some 11,590 people per year die from skin cancer, a far greater number of persons die from systemic cancer (1500 people per day).66 Vitamin D and analogs have also been hypothesized to protect against skin cancer in 2 publications.67,68 Tanning Beds typically emit UV A that can destroy dermal 7 dehydroxycholesterol Vitamin D within the skin. However, the novel use of UVB tanning beds that emits vitamin D – producing ultraviolet radiation is associated with higher 25(OH) D concentrations and thus may have a benefit for the skeleton, according to a study from the Boston University School of Medicine. However, even with conventional tanning beds, one study showed that subjects who used regular tanning bed had serum 25(OH)D concentrations 90% higher than those of control subjects (P<0.001), had parathyroid hormone concentrations 18% lower than those of control subjects (P=0.01), and had significantly higher bone mineral density than non-tanners.69
Studies published have suggested a possibility that regular use of sunscreen to prevent skin cancer may put the population, particularly elderly people, at risk of Vitamin D deficiency. A 1992 study however suggests that during the Australian summer, sufficient sunlight is received, through both the sunscreen itself and the lack of total skin cover, to allow adequate Vitamin D production in people recommended to use sunscreens regularly.70
A 1997 article suggests that sufficient Vitamin D level may be achieved with limited sun exposure, illustrating the folly of reporting upregulated calcitriol levels rather than liver reserve status. Sollito et al. studied eight patients with xeroderma pigmentoisum (XP).71 These patients were treated with intensive sun protection (sunscreen and protective clothing) during a chemoprevention study of oral osoretinoin. All subjects had an expected estimated “normal” amount of Vitamin D intake but indeed were low normal in their liver 25(OH) D vitamin liver reserves. Mean values of 1, 25 (OH) D would be expected to be high as it is the active up regulated molecule.1 Both of these sunscreen studies have been criticized for not controlling application compliance. That is, the subjects unlikely did not completely cover their skin with sunblock.12
Is fortified milk enough for people of color?Vitamin D-fortified milk was designed to prevent childhood rickets, and not designed for adults. After the growing years, African Americans exhibit intolerance to milk products due to absence of lactase, with 81% of African Americans lactose intolerant compared with 12% of Scandinavian whites.72 According to one journal, “the National Dairy Council over-emphasizes the health benefits of calcium” and claims that African Americans can overcome their intolerance to diary products by employing a “few simple dietary strategies”73 The Dairy Council also claims that a low intake of CA++, K+ and Mg++ contribute to high risk of hypertension in African Americans. However, milk is a poor source of magnesium and potassium and plant based Vitamin D2 in milk is not as efficacious as natural animal based Vitamin D3 from cold water fish.
All people of color are particularly susceptible to Vitamin D deficiency. Dark melanin skin pigment slows the production of Vitamin D in the skin upon exposure to the sun. African Americans may require as much as 6–10 times more sun exposure to produce the same vitamin D liver reserve status as Caucasians. Virtually no vitamin D is produced with sun exposure at northern latitudes and African Americans have lower OH Vitamin D levels than Caucasians, regardless of geography. A profound shortage was found in 42% of black females compared to 4% of white females. Even among African American women who consume 200IU from supplements, 28% had a shortage of the vitamin.74 In another study, 21% of elderly blacks in Boston aged 64–100 had Vitamin D deficiency compared to 11% of whites.75 It is unlikely that African Americans living in northern latitudes (US & Canada) will acquire sufficient amounts of vitamin D from dietary sources (milk) to maintain optimum health.76–78
DiscussionAs primary care practitioners, each of us comes in contact with thousands of patients per year. The authors believe it is our responsibility to promote “sensible sunlight” exposure, eye and skin protection along with vitamin D3 supplementation. This is indeed an awesome new responsibility not to be taken lightly. It now remains the responsibility of practitioners, particularly those that practice in northern latitudes, to alert patients to the possibility of Vitamin D deficiency. It is worth reviewing the seminal work of dermatologist – PhD Michael Holick, who advocates “sensible sunlight exposure” (5min 2–3 times per week for whites, five times that for people of color) and the raising of the Vitamin D RDA for all age groups.66 A great source of emerging information on this topic is www.vitaminDcouncil.org, a non- profit attempting to end this scourge on humanity. John Cannell, MD, founded the group.12 Even practitioners in more sunny climates (i.e. Florida, California) may be surprised to learn their patients’ Vitamin D liver reserve status is insufficient or even deficient.76,77
Our front line vulnerable patients remain mothers, infants and people of color, who are plagued by higher prevalence of obstetrical complications, autism, cancer, cardiovascular disease, diabetes, autoimmune disorders and asthma. We must now ask ourselves whether or not “milk mustaches” are enough for people of color, and what happens to the 15% of infants consuming inferior baby formula devoid of vitamin D3. We should be concerned about what happens when vitamin D fortified baby formula is curtailed typically at age 12–18 months in favor of fruit juices.
All chronic disease figures in the US and Canada should be re-evaluated, based on the modulating effects of Vitamin D and the factor of race. This would save hundreds of billions of dollars in health care costs. Kaiser Permanente, California has decided to test all patients.12 The Public Health Agency of Canada (PHAC) has confirmed that it will be investigating the role of Vitamin D in protection against H1N1 (swine flu). The study is already underway at Mc-Master University, with Dr. Mark Loeb leading the project.78,79
Vitamin D deficiency is easy to screen for and even easier to treat with “sensible sunlight recommendations” and Vitamin D3 supplementation to achieve a 25 (OH) vitamin D level of 50ng/ml. We should urge our patients, particularly people of color, to have their 25 (OH) vitamin D liver reserve status checked and increase consumption of cold-water fish and Vitamin D. Sardines are ideal, as they are inexpensive, high in vitamin D3, low in PCBs (polychlorinated biphenyls) and mercury, storable and accessible.
It takes only about 12min of total-body midday summer sun exposure to produce 3000IU of natural vitamin D3 for a Caucasian. It takes a lot longer for a person of color living in Chicago in the summer months. It is not possible for anyone to achieve adequacy in the winter. The public has grown accustomed to prescription drugs that are intended to be used for single diseases rather than sunlight and Vitamin D that exert a broad biological effect. The ball is our court. Let us be a ray of light for our patients.
Conflicts of interestThe authors have no relevant financial relationships or conflicts of interest to disclose.
The authors also acknowledge the Department of Veterans Affairs, James A Lovell Federal Health Care Facility, North Chicago, IL and the Department of Family & Preventive Medicine at Rosalind Franklin University of Medicine & Science, North Chicago, IL as well as ICO, UMSL and Nova Southeastern University Colleges of Optometry.