A longitudinal prospective, cross-over, double masked study was designed to evaluate task oriented visual satisfaction and wearing success with two types of simultaneous vision multifocal soft contact lenses.
MethodsTwenty-two presbyopic subjects followed two 14-day trial periods in which they were alternatively and randomly fitted with two types of multifocal lenses. Habitual tasks were described in terms of observation distance, visual demand level and time allocation. Subjects graded visual satisfaction with each pair of lenses and each habitual task at different times during each trial. Overall satisfaction was evaluated after completion of the two trial periods. Wearing success was determined by the percentage of subjects opting to continue multifocal lens wear and by the number of subjects still wearing their lenses six months later.
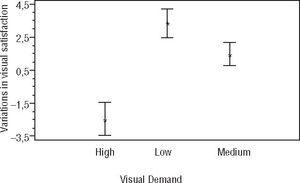
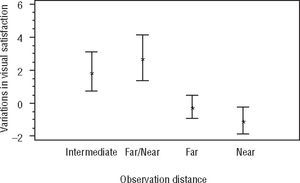
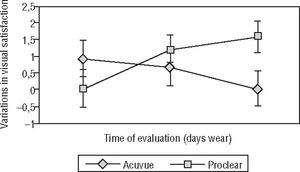
ResultsViewing distance and visual demand level were found to influence visual satisfaction (p<0.001). Visual satisfaction decreased for tasks involving higher visual demands and for near and far viewing distances, rather than for intermediate vision or a combination of near and far vision. A combined effect of lens type and evaluation time was discovered (p=0.046). Although 78% of subjects decided to continue lens wear, only one subject was wearing them on a daily basis 6 months after the completion of the study. Insufficient quality of vision was reported as the main reason for multifocal contact lens discontinuation.
ConclusionsA task oriented visual satisfaction evaluation may prove helpful in lens design selection, as well as in predicting wearing success.
Se diseñó un estudio longitudinal, prospectivo, cruzado y a doble ciego para evaluar la satisfacción visual durante tareas habituales y el éxito de uso con dos tipos de lentes de contacto blandas multifocales de visión simultánea.
Métodos22 sujetos con presbicia se sometieron a dos periodos de prueba de 14 días en los que llevaron de manera alternativa y aleatoria dos tipos de lentes multifocales. Las tareas habituales se describieron en términos de distancia de observación, nivel de demanda visual y asignación de tiempo. Los sujetos calificaron la satisfacción visual con cada par de lentes y cada tarea habitual en diferentes momentos durante el estudio. Después de completar los dos periodos de estudio, se evaluó la satisfacción global. El éxito de uso se determinó por el porcentaje de sujetos que optaron por seguir llevando lentes multifocales y por el número de sujetos que todavía llevaban las lentes 6 meses más tarde.
ResultadosSe descubrió que la distancia de observación y el nivel de demanda visual influyeron en la satisfacción visual (p<0,001). La satisfacción visual fue menor para tareas que suponían mayores demandas visuales y para distancias de observación cercanas y lejanas en lugar de visión intermedia o de una combinación de visión cercana y lejana. Se descubrió un efecto combinado del tipo de lente y el tiempo de evaluación (p=0,046). Aunque el 78% de los sujetos decidieron seguir llevando las lentes, solamente uno seguía llevándolas todos los días 6 meses después del fin del estudio. Como motivo principal de interrupción del uso de lentes de contacto multifocales se notificó la calidad de visión insuficiente.
ConclusionesLa evaluación de la satisfacción visual durante tareas habituales puede ser útil para la selección del diseño de las lentes y también para predecir su éxito de uso.
Over the last two decades there has been a slow but progressive increase in the presbyopic population in Europe. According to Eurostat, 18.9% of the European population in 2009 was aged between 50 and 65, reflecting a 2.3% increase from 1998 in the same age interval.1 The number of wearers of multifocal contact lenses has also experienced a significant growth in recent years, although only about 10% of UK contact lens wearers received a correction for presbyopia in 2008.2 Similarly, a recent international survey has revealed a considerable variance among countries with respect to contact lens fittings for presbyopia, ranging from 79% of all soft lens fittings to patients older than 45 years of age in Portugal to zero in Singapore.3 Interestingly, the same survey revealed that 63% of presbyopes were fitted with non-presbyopic corrections, with the remaining 29% and 8% of presbyopes being corrected with multifocal or monovision fitting philosophies, respectively.
Contact lens correction for presbyopia offers diverse options, including monovision, translating or simultaneous vision contact lenses. The goal of simultaneous vision designs is to provide concurrent clear vision at two or more distances by broadening the lens-eye system depth of focus. Simultaneous vision could be described as the overlapping of multiple individual focal points, each having its own range of clear vision, to provide a single, large expanse of clear vision from infinity to near distance.4 However, this method of correction involves a compromise in which depth of focus for high-contrast targets is gained at the expense of glare and losses in retinal image contrast, particularly manifest when the target contrast is low.5
Simultaneous vision may be achieved through concentric, aspheric or diffractive designs.6 Concentric or annular contact lenses are designed with a central zone, which provides either distance or near power, surrounded by a peripheral annulus granting either near or distance vision, respectively. Aspheric designs are truly multifocal to the extent that they display a gradual transition in lens power between distance and near powers by manufacturing the lens with a front, back or front and back aspheric surfaces. Diffractive designs have multiple echelettes that focus distant images by refraction and near images by diffraction of light. While they are considered to be truly pupil-independent, the design of diffractive contact lenses involves a loss in image contrast caused by the fraction of light that goes into higher diffraction orders.7,8 Diffractive contact lens designs are currently not available for presbyopia correction.
It is relevant to note that a successful simultaneous vision contact lens fit requires good lens centration, with little movement on blinking.9 Besides, a certain pupil diameter is required to allow light passing through the diverse zones of the lens to enter the eye, thus determining retinal image quality.9–11 Age has also been found to influence simultaneous vision contact lens success, not only as a result of an increase in the actual addition of the lens (i.e. larger power gradient across the lens surface)12 but also as a consequence of the associated decrease in pupil diameter (i.e. increase in depth of focus and reduced useful optic zone of the lens) and of a reported major tolerance to defocus4. The last two factors have been found to contribute to an increase in the subjective depth of focus of about 0.027 D per year from the age of 21 to 50 years.13
Ocular dominance has traditionally been considered of relevance in presbyopia correction, both in monovision and multifocal wearing modalities. It is interesting to note that several types of ocular dominance have been described in the literature14 whereby it is not uncommon for different dominance tests to yield different results. Indeed, Ooi and He15 described as, for a given person, ocular dominance changed with different test conditions, at different positions in the visual field and with different levels of attention.
Multifocal contact lens wearing success has been explored from different perspectives: objective retinal image quality analysis,10 psychophysical measures of visual quality (mainly visual acuity and contrast sensitivity evaluation)16,17 and subjective visual satisfaction.18–24
Subjective visual satisfaction and wearing success have been previously studied in different contact lens designs and wearing modalities.18–23 On the one hand, Papas and co-workers18 explored subjective visual satisfaction with a 100 point numerical rating scale, where 0 represented the worst and 100 the best possible response to such variables as ghosting, appearance of halos, lens comfort, vision quality, vision fluctuation, facial recognition and overall satisfaction. Significant reductions were found for all wearing modalities and all subjective vision variables under evaluation. Interestingly, these reductions were not associated with similar reductions in visual acuity, as measured by conventional chart based methods, leading the authors to encourage subjective vision evaluation as a better indicator of lens performance than traditional visual acuity tests. On the other hand, wearing success has been defined as wearers still using their lenses a minimum of 8 hours per day, 5 days per week, at three months after the initial contact lens adaptation19 or as a willingness of patients to acquire a new pair of lenses from their contact lens practitioner.18 Monovision, or some form of modified monovision, was initially identified as the most successful wearing modality for presbyopia,19 although more recent studies reveal bifocal and multifocal contact lenses to offer similar or superior patient satisfaction.20–24 The majority of these studies documented blurred and insufficient quality of vision as the principal reason for contact lens discontinuation.
Even though unsatisfactory vision has been identified as the main reason for multifocal contact lens discontinuation, our literature review revealed a large disparity of criteria to define wearing success and patient satisfaction. Very few studies investigate multifocal contact lens performance during visually demanding habitual tasks,25 opting, instead, for an approach consisting on asking patients for an overall quantification of contact lens performance and a simple description of adverse symptomatology.
In this work, a longitudinal prospective, cross-over and double masked study was designed in order to evaluate visual satisfaction and wearing success with two types of simultaneous vision multifocal contact lenses: Acuvue Bifocal (Johnson & Johnson Visioncare, Jacksonville, FL, US) and Proclear Multifocal (Cooper Vision, Pleasanton, CA, US). Visual satisfaction was assessed by means of several task oriented patient evaluation questionnaires where subjects had to grade satisfaction with the performance of their multifocal contact lens designs during diverse visually demanding habitual tasks at home or at the workplace, including near, distance and intermediate vision activities. Wearing success was defined by the percentage of subjects opting to continue multifocal lens wear after the completion of the study and also by the number of subjects still wearing their lenses six months later.
MethodsSubjectsA total of 22 subjects (16 female; 6 male) participated in the study. All subjects were university staff from the Universitat Politècnica de Catalunya. The study was conducted entirely at the University Vision Centre (UVC), the optometric clinic of the School of Optics and Optometry of Terrassa, Spain.
Inclusion criteria were age between 45 and 65 years (inclusive), previous monofocal contact lens wearers and non-wearers, vertex-compensated spherical prescription between −6.00 D and +4.00 D (inclusive), spectacle cylinder < 0.75 DC, best corrected distance monocular visual acuity according to the logarithm of the minimum angle of resolution (logMAR) of 0.0 or better, habitually uncorrected anisometropia < 2.00 D, free of amblyopia, strabismus and binocular vision anomalies, absence of ocular pathologies and of any previous history of refractive surgery and adequate tear film quality and volume (break up time > 8 s and Schirmer I test > 10mm in 3min). Only subjects with high distance and near visual requirements were included in the study.
Although the actual level of patient motivation was difficult to ascertain, all patients were informed with detail regarding the visual implications and vision quality compromises commonly associated with multifocal contact lens wear. Their subsequent willingness to participate in the study was interpreted as a tacit motivation cue. Any patients manifesting concerns about final visual outcome or expressing doubts about the benefits of multifocal contact lenses over their current visual correction were excluded from the study. In addition, all participants provided written informed consent after the nature of the study was explained to them. The study was conducted in accordance with the Declaration of Helsinki tenets of 1975 (as revised in Tokyo in 2004).
Contact lensesTwo different types of multifocal contact lenses were evaluated in the present study: Acuvue Bifocal and Proclear Multifocal. The main characteristics of these lenses, as provided by the manufacturers, are summarized in Table 1. The Acuvue Bifocal is a centre-near multizone design contact lens with five alternating distance and near zones, pursuing a certain independence of pupil size. Although this type of design would be suggestive of a purely bifocal behaviour, the manufacturer claims that the gradual transition zones between the diverse concentric rings offer intermediate vision powers. This assertion was confirmed by Hough26 with the use of a specially designed multifocal contact lens power profile analyser. The Proclear Multifocal design combines spherical and aspherical zones to produce a “D” lens, which emphasizes distance vision and an “N” lens, for near vision. Lens designs are not symmetrical with each other. Thus, the “D” lens consists in a distance spherical central zone of 2.3mm, surrounded by an aspherical annulus of 5mm and, finally, by a near spherical zone of 8.5mm. Conversely, the near spherical central zone of the “N” lens is 1.7mm in diameter, with an aspherical annulus of 5mm and a distance spherical zone of 8.5mm. The “D” lens is initially intended for the dominant eye, whereas the “N” lens is usually fitted in the non-dominant eye. However, the visual demands of each patient determine the final choice of lenses, and cases of subjects fitted with two “D” or two “N” lenses are not uncommon.
Summary of the main specifications of the Proclear Multifocal and the Acuvue Bifocal contact lenses (data provided by the manufacturers)
| Proclear Multifocal® | Acuvue Bifocal® | |
| Type | Multifocal | Bifocal |
| Recommended wearing regime | Daily | Daily/Continuous wear |
| Recommend replacement schedule | Monthly | Fortnightly/Weekly |
| Manufacturing technique | Moulding | Hydrated moulding |
| Material | OMAFILCON A | ETAFILCON A |
| Water content | 62% | 58% |
| Central thickness (−3.00 D) | 0.11mm | 0.075mm |
| Back optic zone radius | 8.70mm | 8.50mm |
| Overall diameter | 14.40mm | 14.20mm |
| Power range | −6.00 D to +4.00 D | −9.00 D to +4.00 D |
| Recommended care regime | Multipurpose solution or peroxide | Multipurpose solution or peroxide |
| Design | Non-symmetrical aspheric (D/N) | Concentric (5 rings of near/distance vision) |
Table 2 displays the percentage of pupil coverage of distance and near vision areas for the Acuvue Bifocal lens, and distance, intermediate and near vision areas for the Proclear Multifocal lens, with pupils of 3 and 5mm in diameter (intermediate vision coverage with the Acuvue Bifocal lens, although reported as existent, could not be determined by simple geometrical considerations).
Area and percentage of pupil coverage of distance, intermediate and near vision zones for the Acuvue Bifocal lens (intermediate vision, although possible with this type of design, could not be evaluated in terms of geometry) and the Proclear Multifocal lens, as determined with 3 and 5mm of diameter pupils
| ACUVUE BIFOCAL® | PROCLEAR MULTIFOCAL® | ||||||||
| Lens D | Lens D | ||||||||
| Pupil diameter | Distance vision zone | Near vision zone | Distance vision zone | Intermediate vision zone | Near vision zone | Distance vision zone | Intermediate vision zone | Near vision zone | |
| 3mm | mm2 | 3.14 | 3.92 | 4.15 | 2.91 | 0 | 0 | 4.79 | 2.27 |
| % | 44.48 | 55.52 | 58.78 | 41.22 | 0.00 | 0.00 | 67.85 | 32.15 | |
| 5mm | mm2 | 10.18 | 9.49 | 4.15 | 15.47 | 0 | 0 | 17.35 | 2.27 |
| % | 51.75 | 48.25 | 21.15 | 78.85 | 0.00 | 0.00 | 88.43 | 11.57 | |
Subjects were interviewed regarding their visual demands with the aid of a specially designed questionnaire where they indicated the number of hours per week or per day that they allocated to different previously defined habitual tasks, at home and at the workplace, respectively.
For study purposes all tasks were previously described in terms of visual demands (high, medium or low) and viewing distance (intermediate, far, near, or a combination of far and near vision) (see Table 3). Subjective judgement by the clinician was used to define the level of visual demand and the viewing distance for each task.
Habitual tasks at the workplace and home, with indication of visual demand (high, medium or low) and viewing distance (far, intermediate, near or a combination of far and near vision)
| Habitual Task | Visual Demand | Viewing Distance | |
| Workplace | Teaching | Medium | Combination far/near |
| Writing | High | Near | |
| Reading | High | Near | |
| Computer Work | High | Intermediate | |
| Meetings | Low | Combination far/near | |
| Home | Cinema/theatre | Medium | Far |
| Driving | High | Far | |
| House Care | Low | Combination far/near | |
| Sports | Medium | Far | |
| Reading | High | Near | |
| TV | Medium | Far | |
| Computer work | High | Intermediate |
We designed a visual satisfaction questionnaire consisting in multiple vertical visual analogue scales which allowed subjects to grade each habitual task as excellent or very poor in terms of vision. Subjects had to complete one such questionnaire (Q1) at the end of the first day of wear and an identical questionnaire at the end of the first week (Q7).
In addition, a very simple questionnaire evaluated overall lens satisfaction at the end of each trial (Q14) and a final questionnaire explored which pair of lenses provided subjects with a better visual performance for each habitual task and in general (Q30).
ProcedureTable 4 shows a summary of our procedure. At the beginning of the study, subjects were given a comprehensive ocular examination to ensure ocular health, to collect baseline information and to define the final sample by ensuring they met the inclusion/exclusion criteria described above. Ocular parameters were measured, including corneal topography and diameter (with the Pentacam imaging device, Oculus, Inc.), scotopic and mesopic pupil diameter (with the infrared Colvard pupillometer, Oasis Medical, Glendora, California, USA), palpebral aperture and lid position. As stated above, the stability and volume of the tear film were evaluated with the break up time and Schirmer I tests respectively.
Summary of procedure
| Day | ||
| Preliminary visit | 0 | Preliminary exams |
| Sensory dominance | ||
| Determination of frequency of habitual tasks at home and workplace | ||
| Visual satisfaction | 1 | First pair of lenses. 3 days for final lens distance and add power modificationsFinal lens parameters. Q1 at the end of day 1 |
| 7 | Q7 | |
| 14 | Overall satisfaction with first pair Q14Rest | |
| 16 | Second pair of lenses. 3 days for final lens distance and add power modificationsFinal lens parameters. Q1 at the end of day 1 | |
| 23 | Q7 | |
| 30 | Overall satisfaction with second pair Q14Choice of lenses Q30 in general and for each particular task | |
| Wearing success | 6 months later | Is subject still wearing multifocal lenses?If not, reason for discontinuation |
Sensory dominance was determined by placing a +2.00 D lens in front of one eye and the other while subjects were fixating a distance optotype. The dominant eye was identified as the one with a subjectively reported lower tolerance to blurred vision.
Finally, a complete case history was also conducted in the first visit, with particular attention to habitual tasks at home and at the workplace.
On a separate occasion, subjects were randomly fitted with a pair of either Acuvue Bifocal or Proclear Multifocal contact lenses. Contact lenses were fitted according to the manufacturer's recommendations and all fittings were reassessed according to feedback from patients after three days of lens use. Any necessary changes in distance power, as well as in add power, were implemented to improve distance or near vision, whereupon lens parameters were considered final and the first day of lens wear was defined for study and questionnaire purposes. For example, to improve distance vision we opted to add −0.25 D to distance power in the dominant eye first and, if this modification proved unsuccessful, to lower add power in the dominant eye. All contact lens fitting and evaluation procedures were conducted by an assistant clinician in order to ensure that neither the subjects, nor the investigating clinician, knew which lens type was being evaluated.
During the first two weeks, subjects completed the Q1 and Q7 questionnaires, whereupon they were asked to return to the clinic to fill the Q14 overall satisfaction questionnaire and change lenses. Following a 48 hours washout period, the process was replicated with the second pair of lenses. At the end of the second trial period, subjects completed the Q30 questionnaire. They were also allowed to decide whether they wanted to continue wearing multifocal contact lenses and, if answered affirmatively, they had to select between the two lens types.
Six months after the last visit, all subjects were contacted by phone in order to determine wearing success by asking them whether they were still wearing their lenses. Whenever appropriate, the reasons for multifocal contact lens wear discontinuation were investigated.
Data analysisAll visual satisfaction data that could be expressed numerically was analysed with repeated-measures analysis of variance tests (ANOVA) in order to explore the contribution of such factors as contact lens design, visual demand level, observation distance and time of evaluation on visual satisfaction. Categorical data and choice questions were submitted to Chi-square tests to determine whether participants preferred one type of lens or the other to perform any particular task, as well as to explore the final choice of lenses. A Fisher's Least Significant Difference (LSD) procedure was also used to explore statistical significance when paired groups of data were compared.
In order to investigate the influence of contact lens design on visual satisfaction during habitual tasks, all tasks were firstly defined in terms of visual demands and viewing distance. Thus, in addition to habitual tasks, a grid of 4 observation distances ×3 visual demand levels was also constructed. Besides, a preliminary analysis of the data disclosed a high intersubject variability with the potential to mask other significant effects and interactions. Consequently, all data points corresponding to the various habitual task visual satisfaction levels for each subject were transformed by subtracting from them the average visual satisfaction for that particular subject. Visual satisfaction values were thus defined as variations in visual satisfaction (VVS).
All statistical analyses were conducted with Statgraphics Plus 5.1 (Statpoint Technologies, Inc, Virginia, US) for Windows. A p-value of 0.05 or less was considered to denote statistical significance.
ResultsCharacteristics of the study sampleThe age of participants ranged between 45 and 59 years (Mean = 50.6 years; SD = 4.0 years). Twelve subjects had myopia between −0.75 D and −5.75 D (Mean = −2.33 D; SD = 1.47 D) and the remaining 10 subjects were hyperopic ranging from +0.50 D to +3.75 D (Mean = +1.29 D; SD = +1.00 D). Reading addition ranged from +0.75 D to +2.25 D (Mean = 1.55 D; SD = 0.43 D). Only two subjects had any previous experience with monofocal contact lenses.
Pupil diameter was found to decrease with age. Thus, when participants were organized into three age groups (45 to 49; 50 to 54; ≥ 55), a statistically significant difference in pupil diameter was encountered (p<0.05). As discussed bellow, it is interesting to note that the older group of subjects had a scotopic pupil diameter of just over 5mm (Mean = 5.28mm; SD = 0.13mm).
Contact lens fitting proceduresAll subjects in the present study were fitted with a “D” lens in one eye and an “N” lens in the other eye. In all cases except in three subjects, one of whom had undefined ocular dominance, subjects reported better initial satisfaction when the “D” lens was fitted in the dominant eye. Power of Acuvue lenses was adjusted when necessary to maximize distance vision in the dominant eye (adding negative power) and near vision in the non-dominant eye (increasing addition power).
Task oriented visual demands and satisfaction evaluationAll participants were recruited from the teaching and administrative staff of our university, with very demanding intermediate and near distance visual needs. Table 5 displays time allocation at the workplace, in terms of hours per day of dedication to the different habitual tasks, showing a marked predominance of computer work over other tasks such as teaching, reading, writing and formal or informal meetings. Similarly, the same table shows time dedication at home, in hours per week, with reading, watching TV and driving as the tasks where subjects devoted most of their free time.
Time allocation to diverse habitual tasks at home (in hours per week) and at the workplace (in hours per day)
| Habitual Task | Mean | SD | Range | |
| Workplace (hours/day) | Teaching | 1.0 | 0.34 | 0.5–1.5 |
| Writing | 0.5 | 0.29 | 0–0.9 | |
| Reading | 1.0 | 0.27 | 0.7–1.4 | |
| Computer Work | 4.8 | 0.26 | 4.5–5.2 | |
| Meetings | 1.2 | 0.28 | 0.8–1.6 | |
| Home (hours/week) | Cinema/theatre | 1.1 | 0.85 | 0.1–3.0 |
| Driving | 6.5 | 4.52 | 0–15.0 | |
| House Care | 0.3 | 0.34 | 0–1.0 | |
| Sports | 2.8 | 6.45 | 0–21.0 | |
| Reading | 6.7 | 5.01 | 2.0–20.0 | |
| TV | 6.3 | 4.45 | 0–15.0 | |
| Computer work | 3.1 | 3.78 | 0–15.0 |
Irrespective of lens design, a multifactor ANOVA revealed a statistically significant contribution of the factors “observation distance” (F = 10.34; p<0.001) and “visual demand level” (F=36.20; p<0.001) on VVS. A Fisher's LSD test disclosed statistically significant differences between the three visual demand levels. Indeed, as Figure 1 shows, visual satisfaction increased for less visually demanding tasks. Similarly, visual satisfaction was higher for those tasks involving intermediate vision, or a combination of far and near vision, than when the task required far or near vision only (see Figure 2). No statistically significant differences were encountered between visual satisfaction levels for far and near vision.
We also analyzed the effect of the factors “type of lens design” and “time of evaluation” (i.e., Q1, Q7 or Q14). A significant effect was disclosed when both factors were analyzed together (F=3.13; p=0.044). Thus, whereas visual satisfaction with the Acuvue Bifocal lens tended to decrease with time, the Proclear Multifocal lens displayed the opposite behaviour, allowing for higher visual satisfaction levels with time (see Figure 3). It is interesting to note that these differences reached statistical significance only at the end of a complete trial (F=3.08; p=0.046), that is, visual satisfaction levels at the end of the first day (Q1) and at the end of the first week (Q7) were similar for both lenses.
At the end of the two complete trials subjects had to decide on which contact lens design performed better for each habitual task (Q30). Although most subjects opted for the Proclear Multifocal lens, statistically significant differences were only encountered for three habitual tasks involving intermediate vision (computer work; χ2=4.00; p<0.05) or a combination of distance and near vision (house care; χ2=3.00; p<0.05 and meetings; χ2=4.45; p<0.05). In addition, when contact lens selection was explored in terms of “observation distance”, the Proclear Multifocal lens was chosen by a statistically significant larger number of subjects than the Acuvue Bifocal lens for distance (χ2=4.76; p<0.05) and intermediate vision (χ2=3.86; p<0.05). For near vision, observation distance was not found to be a contributing factor for lens selection.
Also, subjects were asked to choose between using one of both lens designs in order to continue contact lens wear or to stop multifocal contact lens wear altogether. Seventeen subjects (77.27%) decided to continue multifocal lens wear, with 12 subjects opting for the Proclear Multifocal lens (55%) and the other 5 for the Acuvue Bifocal lens (23%) (χ2=2.88; p<0.05).
A telephone interview, conducted six months after the completion of the study, revealed that only one subject (out of 17) was still wearing multifocal lenses daily, two subjects used their lenses for more than 3 days per week and eight subjects wore their lenses only occasionally. The remaining eight subjects had discontinued multifocal contact lens wear. The main reason for contact lens discontinuation was revealed to be insufficient vision quality, mostly for distance and near tasks. Driving in general, and at night in particular, proved to be the most challenging visual tasks.
DiscussionThe performance of various multifocal contact lens designs has been previously explored in terms of objective and subjective quality of vision. Although this approach may be useful, particularly for the development of new and better lens designs, multifocal lenses are actually put to the test when their wearers need to do a specially demanding visual task, mostly if it is a habitual task, either at home or at the workplace. For this reason, it was thought that a task oriented evaluation of multifocal lens performance, investigating visual satisfaction for each habitual task, could provide valuable information for practitioners to decide between different contact lens designs, as well as offering a better estimation of long term wearing success.
Ocular sensory dominance may not always be well defined. Indeed, although many contact lens manufacturers recommend determining sensory dominance (Proclear Multifocal) or either sighting or sensory dominance (Acuvue Bifocal) in order to select the eye for distance vision, difficulties may arise when subjects have undefined ocular dominance. These cases are often solved by trial and error. It is also relevant to observe that our elder group of subjects (> 55years) had an average pupil diameter of 5.28mm. Although pupil diameter was measured in predefined illumination conditions, which will vary in real daily life situations, it may be assumed that average pupil diameters of about 5mm may limit the percentage of light entering through the most peripheral area of the Proclear Multifocal lens, for both “D” and “N” designs. The obvious visual implications of this limitation are discussed below.
The study of the characteristics of the sample under evaluation revealed that participants devoted many hours per day to particularly demanding tasks in terms of vision, such as computer work, which involves mostly intermediate vision, or reading and driving, which favour near and distance vision, respectively. As expected, visual satisfaction with multifocal contact lens wear was lowest for those tasks with a higher visual demand.
As for observation distance, visual satisfaction was found to increase in those tasks requiring intermediate vision or a combination of distance and near vision. It may be speculated that the depth-of-focus enlargement associated with the simultaneous vision lens designs under evaluation offers a better compromise for intermediate vision, that is, the retinal image corresponding to an object located at an intermediate distance is sharper. Besides, pupil coverage of intermediate vision zones of the multifocal lens design (as determined for the Proclear Multifocal lens design) is superior to that of distance and near vision areas. Tasks involving a combination of distance and near vision are probably solved by taking momentarily advantage of the asymmetrical multifocal lens design as an alternating monovision solution. On the contrary, sustained distance or near vision tasks would require a more permanent unilateral suppression which, with a lens design allowing for a relatively good binocular vision of intermediate distances, may prove difficult to accomplish. These last considerations, however, are only valid for the Proclear Multifocal lens design and not for the Acuvue Bifocal lens which, notwithstanding fine adjustments in negative power in the dominant eye and addition power in the non-dominant eye, was not adapted following a modified monovision philosophy. As no interaction could be disclosed between “type of lens design” and “observation distance” at Q1 or Q7, further evaluation of these findings is required to draw definite conclusions.
The fact that visual satisfaction with the Proclear Multifocal lens tended to increase towards the end of the trial period (Figure 3) may be interpreted as a partial adaptation to the modified monovision provided by this lens design, not implemented in the Acuvue Bifocal lens. Indeed, success with monovision has been related to patient perseverance, that is, monovision performance seems to improve with time.27
There is a lack of agreement in the literature about the definition of wearing success, thus preventing direct comparison between studies. The present research, for example, would reflect a success rate between 88% and 5%, according to either the percentage of subjects opting for multifocal lens wear continuation after the initial trial, or those still using their lenses in a daily basis six months later. Nevertheless, if wearing success is defined as regular or sporadic lens wear six months after the completion of the initial trial, our success rate reaches 50%, in concurrence with previous studies.19,20
The main reason for multifocal lens wear discontinuation was found to be insufficient quality of vision. This finding has been extensively reported in the literature (see, for example, Papas et al., 2009; and Sheedy et al., 1991).18,21 Particularly demanding visual tasks such as driving at night were found to be the most challenging for this modality of contact lens wear, in agreement with a previous study by Chu and co-workers.28
Finally, a number of limitations of the study should be considered when interpreting these findings. Indeed, the visual requirements of our study sample are probably more demanding than those of a population of subjects from a similar range of ages. Although higher visual demand levels would lead to a better appreciation of multifocal designs limitations, it could be speculated whether wearing success was not actually underestimated, that is, whether other occupational groups with lesser visual demands would exhibit more positive results.
Additionally, multifocal contact lenses wear requires a higher level of commitment to adaptation by the patient than monofocal designs, being often associated with patients with a higher motivation.29 Although subjects with initial manifest poor motivation were excluded from the study, all participants opting for the continuation of multifocal lens wear were provided with free pairs of lenses and solutions for six months after the completion of the initial trials. This type of reward modulated selection may have given rise to a larger number of participants choosing to continue lens wear, probably including less motivated subjects, than if free lenses had not been awarded. This limitation could have been avoided if all participants in the study had received a similar type of compensation, either free contact lenses or another type of reward, with independence to whether they decided to continue lens wear or opted for lens discontinuation.
In conclusion, the results from the present study have revealed an effect of visual demand, observation distance and contact lens design on visual satisfaction of multifocal contact lens wearers. A thorough exploration of each patient's habitual tasks in terms of visual demand, observation distance and time dedication may prove beneficial when selecting lens design in order to increase future visual satisfaction and wearing success. Although the specific characteristics of our study sample probably precluded higher levels of wearing success and, as it is often the case in contact lens research, the findings of the present study are difficult to extrapolate to other, current or future, multifocal lens designs, this research may contribute to increase our understanding of such a complex issue as multifocal contact lens fitting and selection.
Conflicts of interestsThe authors have no conflicts of interests to declare.