Childhood accommodation interferes with accurate diagnosis of the latent refractive errors. Dynamic retinoscopy offers accurate measurements of accommodative response, while an autorefractometer can predict the accommodative system activation in children. A correlation of the accommodative effort with the dynamic refraction has been investigated in emmetropic children, before and after cycloplegia.
MethodsA prospective clinical study of accommodative effort in 149 emmetropic children, in the age group 3–16 years, has been conducted using TOPCON AR RM-8000B autorefractor. Dynamic refraction was performed by monocular estimation method before and after cycloplegia, using the retinoscope mirror light as target. Retinoscopic reflex produced ‘with the motion’ was corrected with positive spherical lenses, and that ‘against the motion’ was corrected with negative spherical lenses, to achieve neutralization.
ResultsMean accommodative effort measured for 149 children included in the study was −0.63±0.69D and dynamic refraction was −0.07±0.44D before cycloplegia, while the mean was+0.52D after cycloplegia, irrespective of the method used. Autorefractor measured −0.17D of accommodative effort per unit change in dynamic refraction before cycloplegia and +0.90D after cycloplegia.
ConclusionsThe performance of TOPCON AR RM-8000B autorefractor was comparable to dynamic retinoscopy. Presence of many children, and in turn, large number of accommodative response data in 11–13 and 14–15 years group is probably linked to prolonged reading/writing. The accuracy and the agreement of the actual accommodative measurements revealed after cycloplegia.
La acomodación infantil interfiere con la precisión diagnóstica de los errores refractivos latentes. La retinoscopía dinámica ofrece mediciones precisas de la respuesta acomodativa, mientras que el auto-refractómetro puede predecir la activación del sistema acomodativo en niños. Se ha investigado la correlación entre el esfuerzo acomodativo con la refracción dinámica en niños emétropes, antes y después de la ciclopejía.
MétodosSe realizó un estudio clínico prospectivo del esfuerzo acomodativo en 149 niños emétropes, dentro del grupo de edad de 3 a 16 años, utilizando el auto-refractómetro TOPCON AR RM-8000B. Se llevó a cabo la refracción dinámica mediante el método de estimación monocular, antes y después de la ciclopejía, utilizando la luz del retinoscopio como objeto de fijación. El reflejo retinoscópico producido ‘a favor’ se corrigió con lentes esféricas positivas, y el reflejo ‘contra’ se corrigió con lentes esféricas negativas, para lograr la neutralización.
ResultadosEl esfuerzo acomodativo medio, medido en los 149 niños incluidos en el estudio fue de -0,63±0,69 D, siendo la refracción dinámica de -0,07±0,44 D antes de la ciclopejía, mientras que la media fue de+0,52 D tras la ciclopejía, independientemente del método utilizado. El auto-refractómetro midió un esfuerzo acomodativo de -0,17 D por unidad de cambio en la refracción dinámica antes de la ciclopejía, y de +0,90 D tras la misma.
ConclusionesEl desempeño del auto-refractómetro TOPCON AR RM-8000B fue comparable al de la retinoscopía dinámica. La presencia de muchos niños y, a su vez, el gran número de respuesta acomodativa en el grupo de edades de 11–13 y 14–15 años, están probablemente vinculados a la lectura/escritura prolongadas. La precisión y concordancia de las mediciones acomodativas reales se revelaron tras la ciclopejía.
Accommodation system of the human eye is a highly complicated function essential to execute very fine and detailed work, without exerting much strain on the eyes. Duane (1912) has deduced the corrective formula based on the accommodative amplitude in 1000 subjects aged 8–70 years, which is useful even today for treating accommodative dysfunctions.1 The accommodative amplitude starts declining from age 3 to 40 years in a curvilinear manner.2 The daily variation of the accommodative amplitude is 1.00D, although the day-to-day values are relatively stable (±0.50D), according to a study of diurnal variation of tonic accommodation.3 Increasing accommodative response has been correlated with increased ciliary muscle thickness in children.4
Dynamic retinoscopy (DR) is the method of choice for rapid assessment of accommodative abilities in children to identify hyperopic and accommodative insufficiency.5 DR is also an objective and efficient technique for assessing maximum accommodative amplitude in early childhood.6,7 Accommodative amplitude can be measured subjectively by Donders push-up or Sheard's methods. Other objective methods of assessing accommodation include monocular estimation method (MEM), Nott dynamic retinoscopy, Bell retinoscopy and autorefraction (AR).
There are very few studies on accommodation by autorefraction and dynamic refraction in emmetropic children. A previous study on accommodative lag measurements, by the two methods in low myopic children with normal visual acuity, concluded that the retinoscopy methods underestimated the accommodative lag compared to the open-field autorefractor.8,9
Accommodative effort (AE), defined as positive or negative response to near target fixation, can be objectively measured by these two techniques. Measurement of distance refraction by AR is nearly accurate in adults, as there is progressive decrease in the accommodative capabilities. However, the performance of AR in children is less reliable. Despite the auto fogging system incorporated in the autorefractors, distance refraction values were not accurate in children with strong accommodative abilities. The readings were negative indicating spherical correction and highly variable on repeated acquisition. The changes are attributed to rapidly adjusting accommodative system, particularly in children. It could also be due to the exertion of the accommodation. In the present study, AR is compared with dynamic retinoscopy using MEM, before and after cycloplegia in emmetropic eyes.
In view of the paucity of studies, the objective of the present study is to compare the accommodative effort by the gold standard cycloplegic refraction with autorefraction and dynamic refraction in emmetropic children.
MethodsA prospective clinical investigation was conducted in the ophthalmology outpatient department, between October 2011 and April 2013, which recruited children between 3 and 16 years of age. Institutional ethical committee approved the study and an informed consent was obtained from the parents of the children. A total of 219 subjects were investigated, including 149 emmetropic, 48 hyperopic and 22 myopic children who presented to the department for their asthenopic symptoms. All the children with Snellen 6/6 visual acuity were included in the study. Hyperopia and myopia of more than ±0.75D were excluded, in addition to astigmatism more than ±1.50D, as determined by the cycloplegic refraction. Strabismus, amblyopic, postoperative patients, and those with anterior and posterior segmental problems that may alter the accommodative function were also excluded.
CycloplegiaCyclopentolate hydrochloride was used for cycloplegia, as it is known to be effective, especially in Indian children with darker iris.10 Topical 1% cyclopentolate hydrochloride solution instilled three times at intervals of 15min was sufficient for cycloplegia for 45min which was sufficient for making all the measurements.
AutorefractometryRefraction measurements were performed using TOPCON AR RM-8000B autorefractometer (Topcon, Germany). AR was performed first, without recording visual acuity that could activate the accommodation system. Children were instructed to keep the chin on the chin-rest of the instrument without closing the other eye. All children were instructed to look at the central target (tiny red colored house) in the field of view, and were instructed to keep the target always in view. The corneal reflection on the display screen was focused on the alignment mark and the refraction readings were obtained by gently pressing the ‘measurement’ button. Accommodative effort was computed as average of five readings.
Dynamic retinoscopyDynamic retinoscopy was performed before and after cycloplegia, by modified MEM using the retinoscope mirror light as the near target fixed at 60cm. The working distance correction of −1.66D was determined using a spherical lens that produced the neutralization at 60cm. Children were asked to fixate at the light target, and positive and negatively powered correctional lenses were used, respectively, to compensate for the “with” and “against” the motion until the neutralization point reached. Accommodative effort was calculated by adding the working distance correction to the corrective lens that produced neutralization.
Dynamic refractionDynamic refraction in children was determined using a spot retinoscope at 60cm from the subject, with the light serving as the target for fixation.11 A formal static refraction was done to observe the behavior of the pupillary retinoscope reflexes while fixating at the Snellens 6/60 top letter. The reflexes observed ‘with the motion’ were suddenly changed to ‘against the motion’ when the child fixated at the retinoscope light. Three-year-old children were provided with the alphabet ‘E’ cut out of a cardboard, and were instructed to hold it in the same direction as the letters shown on the Snellens illiterate chart. The MEM was performed by neutralizing retinoscope reflexes in a dimly illuminated room, while the child accommodated at the retinoscope light. The distance was measured using a metallic tape and dynamic radioscopy was performed by the assigned optometrist. Refraction was done along the patient's visual axis by inserting negative corrective lens if the reflex was ‘against the motion’ or with positive corrective lens when the reflex exhibited was ‘with the motion’. The tests were completed very quickly to minimize the glare, activation of binocular accommodation and convergence system.
Mohindra retinoscopyIt is useful in infants and babies in whom fixation reflexes are still under development. The technique used light as stimulus in darkly illuminated room as the accommodation not triggered, in contrast to DR which used mesoptic illumination conditions. Mohindra method allowed 0.75D for the tonic accommodation and subtracted 1.25D (corrective factor) for the working distance (instead of −2.00D at 50cm working distance).12 Two examiners performed the measurements separately and were blinded to each other. The categorization of ammetropic and emmetropic subjects was based on the cycloplegic refraction. Cycloplegic refraction was performed to identify children with actual refractive errors. A cycloplegic refraction of ±0.75D was considered emmetropic, and those with a higher value were grouped under hyperopic and myopic, respectively.
Statistical analysesThe accommodative effort of the right eye was analyzed for convenient statistical interpretation. Precycloplegic and cycloplegic statistical analyses were performed using XLSTAT software. The area under the curve (AUC) of the receiver operating characteristic (ROC) graph was set up in order to determine the accuracy of the testing methods.
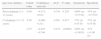
ResultsOne hundred and forty nine (n=149) emmetropic children were finally included in the analysis with 83 (55.71%) boys and 66 (44.29%) girls, with mean±SD age of 11.72±3.24 years. Table 1 shows the descriptive statistics of the accommodative response as measured by the autorefraction and dynamic refraction methods, before and after cycloplegia. Table 2 shows the mean AE recorded before and after cycloplegia by the two methods along with P values.
Precycloplegic and cycloplegic descriptive statistics of accommodative response by dynamic and autorefraction.
| Emmetropic (n=149) | Precyclo ARMinus | Precyclo ARPlus | Precyclo DRMinus | Precyclo DRPlus | Cycloplegic ARMinus | Cycloplegic ARPlus | Cycloplegic DRMinus | Cycloplegic DRPlus |
| Number of eyes | 127 (85%) | 20 (13.42%) | 82 (55.03%) | 55 (36.91%) | 12 (8.05%) | 132 (88.59%) | 7 (4.70%) | 111 (74.50%) |
| Mean (±SD) | −0.79D (0.58) | +0.43D (0.27) | −0.35D (0.25) | +0.36D (0.29) | −0.55D (0.28) | +0.61D (0.29) | −0.43D (0.12) | +0.58D (0.15) |
| SEM | 0.05 | 0.06 | 0.03 | 0.04 | 0.09 | 0.03 | 0.05 | 0.02 |
| Maximum | −3.66D | +1.30D | −1.50D | +1.75D | −1.20D | +1.75D | −0.50D | +0.75D |
| Minimum | −0.12D | +0.30D | −0.25D | +0.25D | −0.25D | +0.20D | −0.25D | +0.25D |
| Pearson | 0.19 | 0.02 | 0.19 | 0.02 | 0.11 | 0.15 | 0.11 | 0.15 |
| Exact P values | 0.09 | 0.92 | 0.09 | 0.92 | 0.81 | 0.12 | 0.81 | 0.12 |
Quantitative data of accommodative effort in emmetropic children before and after cycloplegia.
| Methods (n=149) | Mean (± standard deviation) | Standard error of the mean | Pearson correlation coefficient | Minimum | Maximum | Exact P values |
| Precycloplegic autorefraction | −0.63D (0.69) | 0.06 | 0.03 | −3.66D | +1.30D | 0.001 |
| Precycloplegic dynamic | −0.07 (0.44) | 0.04 | 0.03 | −1.50D | +1.75D | 0.001 |
| Cycloplegic autorefraction | +0.52 (0.44) | 0.04 | 0.59 | −1.20D | +1.75D | <0.0001 |
| Cycloplegic dynamic | +0.52D (0.28) | 0.03 | 0.59 | −0.50D | +0.75D | <0.0001 |
Precycloplegic AR and DR recorded zero readings in 2 (1.34%) and 12 (8.05%) children respectively, while cycloplegic AR and DR recorded in 5 (3.36%) and 31 (20.81%) respectively. Autorefraction measured zero accommodation in 2 and 5 children before and after cycloplegia, respectively. Dynamic retinoscopy measured zero accommodation (in reality not possible) in 5 and 31 children, before and after cycloplegia respectively. Precycloplegic ROC analysis missed in 7% and cycloplegic ROC analysis missed in 17% of the cohort (n=149).
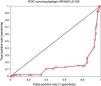
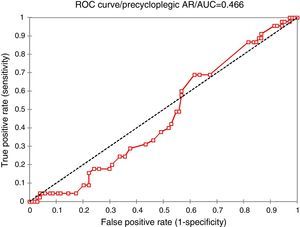
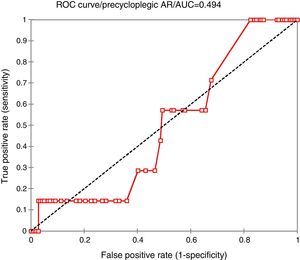
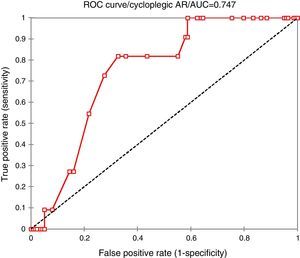
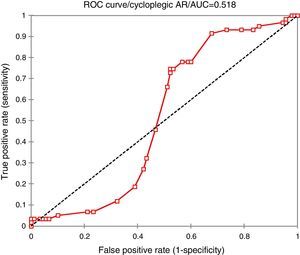
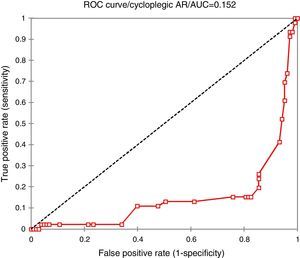
The AR and DR readings were considered as test and event data respectively. The ROC curve, sensitivity, and specificity have been calculated at 0.25, 0.50, and 0.75D cut point values to achieve higher accuracy (AUC), sensitivity, and specificity rates before and after cycloplegia. Statistical significance is reported for P<0.05. Precycloplegic ROC analyses are depicted in Figs. 1 and 2, while cycloplegic ROC in Figs. 3–5.
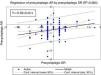
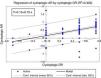
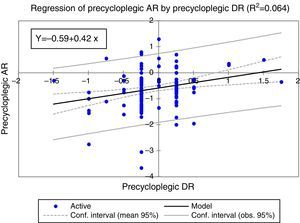
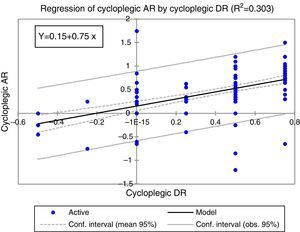
The regression analysis was performed to determine the linear relationship, in addition to prediction and the best-fit curve model for the methods. The prediction interval of regression analysis and the 95% confidence intervals (CI) of Bland–Altman analysis were compared to find out whether the two methods could be interchangeable. The upper and lower limits of predictable intervals for the slope and intercept were compared with 95% limits of agreement (LoA) by Bland–Altman plots for interchangeability of the methods as shown in Table 3. Precycloplegic and cycloplegic regression plots for AR and DR data are shown in Figs. 6 and 7, respectively.
Regression and Bland–Altman analysis of accommodative effort.
| Emmetropic (n=149) | Coefficient of determination (R2) | Slope (b) | Prediction interval (intercept a) | 95% confidence intervals (Bland–Altman) | Linear regression equation (y=a+bx) |
| Precycloplegic AE | 0.064 | 0.41 | −0.69, −0.48 | −0.55, −0.26 | y=−0.59+0.42x |
| Cycloplegic AE | 0.303 | 0.75 | 0.06, 0.25 | −0.63, −0.37 | y=0.15+0.75x |
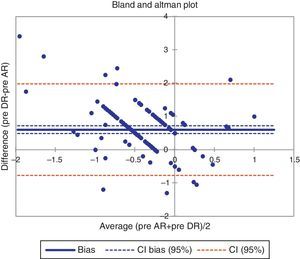
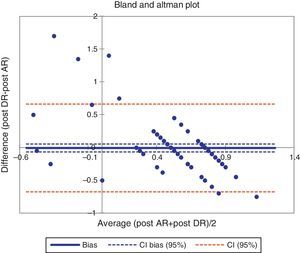
The AE data were analyzed using Bland–Altman difference plots to determine the limits of agreement (LoA) between the two methods. The difference between the two methods should lie within 95% CI, computed as the mean bias ±1.96SD13,14 for precycloplegic and cycloplegic AR and DR as shown in Figs. 8 and 9.
The children were sub-grouped according to the age as 3–6, 7–10, 11–13, and 14–16 years. Table 4 shows the descriptive analysis of AE in sub-groups before and after cycloplegia. Precycloplegic and cycloplegic ROC data calculated for different sub-groups are shown in Tables 5–8.
Descriptive statistics of accommodative effort by age stratification before and after cycloplegia.
| Variables | 3–6 years | 7–10 years | 11–13 years | 14–16 years |
| No. of eyes | 14 | 22 | 57 | 53 |
| Age (mean, ±SD) | 4.86 (0.94) | 8.69 (1.17) | 12.12 (0.78) | 14.99 (±0.80) |
| Precycloplegic AR | −0.33 (±0.61) | −0.41 (±0.62) | −0.77 (±0.83) | −0.62 (±0.54) |
| Precycloplegic DR | −0.07 (±0.36) | −0.01 (±0.33) | −0.14 (±0.51) | +0.01 (±0.34) |
| Cycloplegic AR | +0.55 (±0.61) | +0.57 (±0.40) | +0.50 (±0.42) | +0.40 (±0.44) |
| Cycloplegic DR | +0.38 (±0.28) | +0.44 (±0.34) | +0.47 (±0.30) | +0.40 (±0.37) |
ROC curve analysis of accommodative response before and after cycloplegia in 3–6 years old children.
| Age wise statistics | Cutoff value | Confidence intervals | AUC | P value | Sensitivity | Specificity |
| Precycloplegic (3–6 years) | −0.25 (71%)+0.25 (14%) | −0.499, −0.084 | 0.208 | 0.006 | 100% (at 0.70D) | 8% (at 0.70D) |
| Cycloplegic (3–6 years) | −0.25 (7%) +0.25 (7%) | 0.118, 0.420 | 0.769 | 0.000 | 100% (at 0.30D) | 77% (at 0.30D) |
| 0.50 (64%) | −0.432, 0.386 | 0.467 | 0.876 | 100% (at 1.00D) | 40% (at 1.00D) | |
| 0.75 (7%) | −0.574, −0.272 | 0.077 | <0.0001 | 100% (at 1.20D) | 7% (at 1.20D) |
ROC curve analysis of accommodative response before and after cycloplegia in 7–10 years old children.
| Age wise statistics | Cutoff value | Confidence intervals | AUC | P value | Sensitivity | Specificity |
| Precycloplegic (7–10 years) | −0.25 (23%)+0.25(23%) | −0.137, 0.207 | 0.535 | 0.688 | 80% (at 0.70D) | 47% (at 0.70D) |
| Cycloplegic (7–10 years) | 0.75 (23%) | −0.340, 0.105 | 0.382 | 0.30 | 60% (at 0.50D) | 40% (at 0.50D) |
ROC curve analysis of accommodative response before and after cycloplegia in 11–13 years old children.
| Age wise statistics | Cutoff value | Confidence intervals | AUC | P value | Sensitivity | Specificity |
| Precycloplegic (11–13 years) | 0.50 | −0.151, 0.632 | 0.741 | 0.228 | 100% (at −0.75D) | 51% (at −0.75D) |
| Cycloplegic (11–13 years) | 0.50 | −0.090, 0.212 | 0.561 | 0.427 | 77% (at 0.55D) | 57% (at 0.55D) |
| 0.75 | −0.447, −0.246 | 0.153 | <0.0001 | 100% (at +1.00D) | 27% (+1.00D) |
ROC curve analysis of accommodative response before and after cycloplegia in 14–16 years old children.
| Age wise statistics | Cutoff value | Confidence intervals | AUC | P value | Sensitivity | Specificity |
| Precycloplegic (14–16 years) | 0.25 | −0.220, 0.031 | 0.405 | 0.136 | 100% (at 0.00D) | 6% (at 0.00D) |
| 0.50 | −0.303, 0.165 | 0.431 | 0.566 | 100% (at −0.30D) | 31% (at −0.30D) | |
| Cycloplegic (14–16 years) | 0.25 | 0.244, 0.424 | 0.834 | <0.0001 | 100% (at 0.30D) | 67% (at 0.30D) |
| 0.50 | −0.128, 0.153 | 0.512 | 0.866 | 90% (at 0.60D) | 39% (at 0.60D) | |
| 0.75 | −0.507, −0.252 | 0.118 | <0.0001 | 63% (at −0.60D) | 97.3% (at −0.60D) | |
The proportion of the eyes with negative accommodative response has decreased after cycloplegia while the proportion of positive responses increased significantly. The mean accommodative effort measured by AR is higher than that by DR method. The mean difference between the methods for negative and positive responses is −0.44 and +0.07D, respectively. Performance of the two methods improved after cycloplegia as indicated by the standard error of mean (SEM) values, and the range of values were comparable.
DiscussionThe present prospective study has evaluated the accommodative effort in emmetropic children defined as positive or negative response. These accommodative responses measured by AR and DR methods have been compared, although true accommodation is not actually measured.
Autorefractor recorded higher levels of negative response of −3.66D compared to DR that measured −1.50D, conversely dynamic refraction measured higher levels of positive response of +1.75D compared to AR that measured +1.30D. The Pearson correlation coefficient (r) calculated was very low indicating weak correlation of both methods being no statistically significant (P>0.05) (Table 1).
Pre-cycloplegic AE was not measured in 2 (1.34%) and 5 (3.36%) children by AR and DR methods, respectively. However, after cycloplegia both methods showed a positive drift, probably attributable to revelation of latent hyperopia or residual accommodation. AR helped in estimating the amount of AE and residual accommodation (latent hyperopia) before and after cycloplegia in most of the children. Although AE measured by DR before cycloplegia were both positive and negative responses, after cycloplegia the positive trend was seen in 111 (74.50%) eyes. The number of eyes missed by DR was probably due to the complete cycloplegia or failure to reveal latent hyperopia observed in 31 (20.81%) eyes after cycloplegia.
AR measured higher mean AE of −0.63±0.69 compared to −0.07±0.44D by the DR method before cycloplegia. In a previous study on the accuracy and accommodation capability in 2–12 year old children, handheld autorefractor measurements were reliable under cycloplegic conditions, but were found to be over-correcting by more than −2.00D in 24% of children.15 AR measured maximum AE was −3.66D compared to +1.75D by DR method. Both methods provided statistically significant differences before cycloplegia, when both positive and negative accommodative responses were considered (P<0.001). Interestingly after cycloplegia, the true AE measured by both these methods converge to +0.52D, with statistically significant results (P<0.0001) and good correlation (r=0.59), as shown in Table 2. Another study has compared AE measured by three different autorefractors, Retinomax K plus 2, Canon RF10 and Grand Seiko WR5100K, with subjective refraction, with and without cycloplegia, in 117 primary school children. They have observed that all the three had a tendency toward negative over-correction in precycloplegic conditions. Nevertheless, they were accurate under cycloplegic circumstances, similar to the results of the present study.16
The low R2 value for AE before cycloplegia improved to 0.303 after cycloplegia, suggesting better fit of the curve. Low (R2) values might be misleading; the width of the prediction intervals became narrower after cycloplegia; however, the true AE observed was within an acceptable range of the 95% CI of Bland and Altman analysis, suggesting that both the methods may be interchangeable, for the measurement of AE in emmetropes.
The y-intercept (dependant variable) for the accommodative effort before cycloplegia was −0.59D whereas after cycloplegia the accommodative effort calculated was +0.15D when the x (independent variable) rose to zero. For every unit change in x value, the predicted accommodative effort before cycloplegia was −0.17D, but after cycloplegia for every unit change in x value was associated with +0.90D which might be taken as true accommodative effort.
Number of children in 11–13 and 14–16 years age groups was higher than the other two groups. Precycloplegic AR showed negative response for all the age groups, whereas positive response was obtained by DR for 14–16 years, probably due to activation of accommodation. Accommodative response drifted toward positive side after cycloplegia, by both the methods in all the age groups (Table 4).
The accuracy was low (AUC=0.208) in the 3–6 years group with 71% of the eyes showing −0.25D of accommodative response before cycloplegia. However, at 0.70D cut point value, 100% sensitivity and 8% specificity were obtained (P=0.006). After cycloplegia, the accuracy improved (AUC=0.769) with 100% sensitivity and 77% specificity (P=0.000). After cycloplegia, 64% of the eyes recorded +0.50D (AUC=0.467), but at 1.00D, the sensitivity and specificity were100% and 40%, respectively (P=0.876). Interestingly, there was statistical significance (p<0.0001) at 0.75D cut-off point with very poor AUC (Table 5). There was no statistical significance found in the 7–10 years group, in addition to low accuracy rates before and after cycloplegia. The ROC analyses failed to obtain high accuracy rates at 0.25, 0.50, and 0.75D cut-off points (Table 6).
Precycloplegic ROC curve analyses yielded good accuracy rates (AUC=0.741) with 100% sensitivity and 51% specificity rates at −0.75D cut point value in 11–13 years age group. On the other hand, cycloplegic ROC showed a low accuracy with 0.50D cut-off point with statistical significance (P<0.0001) at 0.75D. However, at +1.00D cut-off point, 100% sensitivity and 27% specificity were obtained (Table 7). For the 14–16 group, low to very low accuracy was observed along with 100% sensitivity and very low specificity, but improved (AUC=0.834) at 0.25D cut-off after cycloplegia with high statistical significance (P<0.0001). At 0.75D, the specificity increased to 97.3% with poor accuracy (AUC=0.118) after cycloplegia with a high statistical significance (P<0.0001).
Precycloplegic ROC curve analysis in 149 children showed low accuracy of 0.466 and 0.494 at 0.25 and 0.50D cut point values, respectively. The accommodative response was not analyzed in 11 (7%) eyes with 0.000D which is practically not possible and difficult to explain. The negative response of −0.25D calculated in 66 (44%) eyes, while positive response of +0.25D in 45(30%) eyes. The present AR results were comparable to a traditional retinoscopy measurement in 142 children aged 3–15 years that showed significantly higher negative responses (>0.50D) in 69 right eyes.17 The two studies, the traditional retinoscopy as well as the present study, have shown different results before and after cycloplegia, which are statistically significant. Similarly, for the positive responses, both studies demonstrated significantly lower values by AR after cycloplegia. The previous study has concluded that without cycloplegia, actual hyperopic underestimated and actual myopia was overestimated. In view of this, observations from the present study may indicate that the negative responses (pseudo accommodation) recorded by AR before cycloplegia could be due to prolonged near work that caused spurious myopia that was measured as positive response after cycloplegia in emmetropic children (Figs. 1 and 2).
Three autorefractors, Topcon RM-A 6000, Nidek AR 800 and Nikon NR 5000 have been compared with the hand-held Retinomax (R) autorefractor in 276 subjects and 48 infants under cycloplegia.18 This study has shown better accuracy with the hand-held AR, comparable to the present study, especially to the AUC of 0.747 at 0.25 cut point value under cycloplegia (Fig. 3).
Precycloplegic regression analysis in Fig. 6 shows very weak positive correlation (R2=0.064) with high statistical significance (P<0.0001), as seen by scatter of the data points around the curve. On cycloplegia, regression analysis improved (R2=0.303) revealing vertical alignment of the data points toward the positive side with only five outliers, as depicted in Fig. 7. The distribution of the data points shows positive gradient due to the positive relationship between the AR and DR methods.
Precycloplegic Bland–Altman difference plot in Fig. 8 shows nine data points outside the LoA with 95% CI of −0.55 to −0.26D (P<0.0001). Over- or under-estimation of the readings, by any of the methods, is indicated if the data points lie above or below the zero bias line, respectively. However, no such observation is seen in the present study (Fig. 9), implying good agreement between the methods in measuring accommodative response. A majority (95%) of data points are within the LoA (only 6 points outside of LoA) and the true value would lie within the 95% CI intervals between −0.63 and −0.37D.
The infrared autorefractor has shown significantly lower mean lag of accommodation when the near accommodative response was tested by the DR and the AR methods. Rosenfield et al. have observed closer agreement of AR with objective dynamic retinoscope, which is comparable to the present observation of good agreement of the AR after cycloplegia.19 Although their measurements were performed under binocular viewing conditions, the authors recommended DR under monocular conditions for assessing accommodative response. DR was performed by varying the working distance to achieve neutralization, eliminating the need for lenses. In the present study, DR performed by placing the appropriate spherical lens in the trail frame at 60cm, until neutralization neutralization was obtained.
SureSight wavefront autorefraction and the influence of accommodation have been studied and compared with cycloplegic retinoscopy in 195 eyes of 108 patients (1–81 years) under cycloplegia.20 Many emmetropic and hyperopic children were overcorrected up to −6.13D, and in young patients (2–17 years), 47% were overcorrected by more than −2.00D, but their accuracy results did not show the AUC measurements. Children with active accommodation were possibly identified on highly negative AR and DR readings. The positive correlation of the methods under cycloplegia may be used to diagnose latent hyperopic/residual accommodation. Insufficiency of cyclopentolate in some children may lead to such high values and larger studies are needed to arrive at accurate interpretations. Present study suggests appreciable accuracy in identifying emmetropic children by AR and DR under cycloplegia. The precycloplegic accommodative status is possibly predicted by the negative AR values.
In conclusion, the performance of AR is comparable to the DR in measuring accommodative effort, before and after cycloplegia. Both methods showed positive and negative spherical over-estimation before and after cycloplegia, respectively, in emmetropic children. The highly negative spherical correction recorded by autorefractor could suggest increased accommodative effort before cycloplegia. Under cycloplegia, both methods measured the refraction in positive spherical correction, suggesting concurrence of the two methods. The accuracy and the agreement of the actual accommodative measurements revealed dramatically after cycloplegia. Low accuracy rates for the AE measured in 7–10 years, and failure of ROC curve at all cut point values, warrant further investigation. Presentation of many children with asthenopic symptoms in the 11–13 and 14–15 years group is probably linked to prolonged reading and writing activities. Attainment of complete cycloplegia may be responsible for zero or missing AR data after cycloplegia. Revelation of latent hyperopia or residual accommodation due to insufficient cycloplegia in some children needs further investigation.
Conflicts of interestThe author has no conflicts of interest to declare.
We thank to the optometrist and ophthalmic assistant of the Department of Ophthalmology for cooperation with refraction measurements.