To explore differences in saccadic eye movements between children with oculomotor dysfunction and those in a control group across three age groups, using two assessment methods: the subjective Northeastern State University College of Optometry (NSUCO) Oculomotor test and objective analysis with the Tobii Eye X Eye Tracker (Tobii Eye X, Tobii, Stockholm, Sweden).
MethodsThis study included 31 children (ages 7–13) diagnosed with oculomotor dysfunction and 16 age-matched children in the control group. Participants were divided into three age groups: group 1 (7–8 years), group 2 (9–11 years), and group 3 (12–13 years). Saccadic eye movements were evaluated and compared using two methods: the NSUCO test and the Tobii Eye X eye tracker, along with specialized software analysis (Thomson Software Solutions, Welham Green, UK)
ResultsChildren in the oculomotor dysfunction group obtained significantly lower NSUCO scores (p < 0.001) compared to the control group. Regarding eye tracking analyses, a significantly higher number of hypometric saccades were found in oculomotor dysfunction group (p ≤ 0.044). Additionally, in this group a significantly higher percentage of regressions was observed for a 1-second stimulus presentation interval (p = 0.012). Significant correlations were found between different NSUCO scores and the percentage of regressions, the number of completed saccades and the number of hypometric saccades.
ConclusionThe presence of hypometric saccades and regressions appears to be a distinguishing characteristic of children with oculomotor dysfunction, detectable through both objective eye tracking analysis and the subjective NSUCO test, which can be easily implemented in clinical settings.
Eye movements are the natural, smooth, coordinated, and effortless ability of the human eye to move, maintaining a sharp, fused, and focused image at the center of the retina. This ability has been studied since the early 20th century.1 Eye movements must be efficiently integrated and can occur automatically with the involvement of the lower and frontal areas of the brain, without requiring direct intervention from the frontal lobe. This allows the frontal lobe to focus on tasks such as learning, attention, and comprehension.2
Oculomotor skills are used to predict the actions of objects and other people, helping to anticipate actions for protection or reaction.3 Smooth pursuits and saccades are two fundamental types of eye movements used to characterize eye motion dynamics. Smooth pursuits are voluntary eye movements, characterized by being slow, fluid, and coordinated between both eyes, allowing the image to remain stable on the fovea as stimuli move across the visual field.4
Saccades are rapid eye movements that help fixate on an object and bring it to the center of the retina. These movements can reach speeds between 100 and 800° per second, with an average frequency of 100,000 saccades per day.5,6
There are different types of saccadic movements: memory-guided, antisaccades, and visually guided. The latter are divided into recovery saccades, anticipatory movements, and regression movements (movements made toward the target but failing slightly, followed by a correction saccade). Saccade gain is the ratio between the actual saccadic amplitude and the desired saccadic amplitude. If the gain is <1, the saccade will be too small, which is known as a hypometric saccade.7 One the other hand, when the gain is greater than 1, the saccade will be too large, known as a hypermetric saccade.
Additionally, oculomotor performance plays a key role in organizing a wide variety of everyday activities, such as walking, driving, and cooking, and is essential for the development of reading. Oculomotor dysfunction can potentially lead to problems in these areas.8,9 Therefore, in optometric examinations, evaluating eye movements should be considered a crucial component, with particular emphasis on saccadic movements. It has even been suggested that eye movement analysis could serve as an additional tool to help diagnose certain oculomotor dysfunctions.10
Several studies have shown that neurological diseases11 and neurodevelopmental disorders (NDD), such as dyslexia, attention deficit hyperactivity disorder (ADHD), and developmental coordination disorder (DCD), can affect eye movements.12 Difficulties in the precision and execution of saccadic eye movements have been identified in all three types of NDD.12,13 In the case of children with ADHD, difficulties were found in the ability to inhibit oculomotor responses.14,15 For children with DCD, there were challenges in maintaining fixation and tracking moving objects, as well as a higher frequency of errors in anti-saccades.16
The objetive of this study is to explore saccadic eye movements in children across three age groups: group 1 (7–8 years), group 2 (9–11 years), and group 3 (12–13 years). The study compares the outcomes obtained using two assessment methods: the subjective Northeastern State University College of Optometry (NSUCO) Oculomotor test and an objective analysis using the Tobii Eye X Eye Tracker. Furthermore, saccadic eye movements in children with oculomotor dysfunction (ODG) are preliminarily compared with those of a control group (CG).
This research aims to provide useful insights into the evaluation of eye movements in pediatric clinical practice. By comparing a traditional subjective method with a novel objective technology, the study highlights the potential for integrating accessible tools like NSUCO with more advanced techniques. Such comparisons can contribute to more accurate and comprehensive assessments of oculomotor function in children, especially in cases where access to eye-tracking technology is limited.
Materials and methodsPatientsA prospective, non-randomized comparative study was conducted with 47 children aged 7 to 13 years at the Department of Optometry of Hospital Quirón Salud in Huesca, Spain. The study adhered to the principles of the Declaration of Helsinki and was approved by the Ethics Committee of the University of Valencia, Spain (2703478).
Before the optometric examination, the children's parents signed an informed consent form, which provided detailed information about the study protocols, risks, and benefits. Inclusion criteria required that all participants have a corrected distance visual acuity (CDVA) of 0.00 logMAR or better with the best correction. Exclusion criteria included the presence of any active ocular or systemic disease at the time of the examination. Children with neurodevelopmental disorders or learning difficulties were not excluded from the study, as our aim was to reflect the heterogeneity commonly seen in clinical optometric practice. Since these conditions are frequently associated with oculomotor dysfunction, including them allows for a more realistic evaluation of both assessment methods. Eligible 47 participants were then classified into three distinct groups according to age:
- 1.
Group 1: 17 [7–8] children. Control: 5, ODG: 12.
- 2.
Group 2: 24 [9–11] children. Control: 9, ODG: 15.
- 3.
Group 3: 6 [12–13] children. Control: 2, ODG: 4.
All groups included children with and without oculomotor dysfunctions, as determined by the Northeastern State University College Optometry (NSUCO) test de Maples & Flickin.17 Based on this classification, the participants were further divided into two main groups:
- •
A control group (CG) consisting of 16 children (n = 6 girls) aged 7 to 13 years.
- •
A group with oculomotor dysfunctions (ODG), which included 31 children (n = 16 girls).
Among the ODG participants, some had Neurodevelopmental Disorders (NDD); however, the exact number of affected patients was not specified.
Participants were classified into the oculomotor dysfunction group (ODG) or the control group (CG) based on their performance in the NSUCO test, following the normative criteria established by Maples and Ficklin.17 According to these norms, scores below the expected performance for age in any of the three evaluated domains (ability, accuracy, or associated head movements) were considered indicative of oculomotor dysfunction. This classification was used prior to subdividing the sample into the three age groups.13
Examination protocolPrior to the eye movement analysis, the following assessments were performed: manifest and cycloplegic refraction, uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), heterophoria at distance and near (40 cm) using the cover test, and near point of convergence (NPC). Most of the children were referred by an ophthalmologist after undergoing a comprehensive ophthalmological examination. Patients with neurodevelopmental disorders were diagnosed by a neuropediatrician.
The "Northeastern State University College of Optometry" (NSUCO) test subjectively evaluates saccadic eye movements by assessing three areas of performance:
- •
Ability: Determines whether the patient can perform the assigned task.
- •
Accuracy: Evaluates the precision of saccadic execution.
- •
Head movements: Assesses the extent of head movements used to complete the task.
The assessment was conducted with the patient standing 40 cm in front of the examiner, using binocular vision. Fixation stimuli consisted of 0.5 cm colored spheres mounted on a rod, following the standardized NSUCO test protocol. Saccadic movements were evaluated by instructing the patient to alternate fixation between two stimuli positioned 20 cm apart horizontally. Scoring was based on the examiner’s observation, following the criteria outlined in Table 1.13
Scoring methodology applied in the NSUCO test for assessing oculomotor function.
To objectively assess eye movements, the Tobii Eye X Eye tracking system (Tobii, Stockholm, Sweden) was used in combination with the Clinical Eye Tracker software from Thomson Software Solutions (Welham Green, United Kingdom).
To ensure transparency and replicability of our eye-tracking procedure, we followed the 2023 Minimal Reporting Guideline for Research Involving Eye Tracking Dunn et al.18 Eye movements were recorded using the Tobii Eye X eye tracker (Tobii, Stockholm, Sweden), with a sampling frequency of 60 Hz. Participants were seated 60 cm from a 24-inch monitor in a room with moderate ambient lighting. Head movement was not restricted but minimized through proper posture and examiner supervision. Calibration was performed prior to each measurement using a standard five-point calibration provided by the Tobii software.
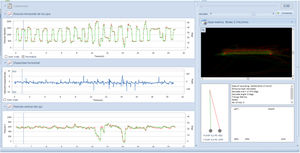
Saccadic movements were evaluated using two spheres placed 10 cm apart on either side of the midline, following a protocol similar to the NSUCO test. Initially, the spheres appeared consecutively at 0.5 s intervals. A second measurement was taken with 1-second intervals between the appearance of each sphere. Based on these measurements, the software provided data on: total number of saccades performed, percentage of regressions, number and percentage of complete saccades, as well as the number and percentage of hypometric and hypermetric saccades Fig. 1.
Screenshot of the clinical eye tracker software depicting eye movements during the test. The image on the right shows the representation of the screen observed by the children with the two red dots flashing, simulating the NSUCO test. On the left, graphs are plotted based on eye X position (right eye represented in red, left eye in green), fixation stability, and eye Y position.
All evaluations were completed in a single session, with the test order randomized. In some cases, objective assessments were performed first, while in others, subjective evaluations took precedence. Examinations were conducted using the best available optical correction for both distance and near vision. Two examiners carried out the patient assessments.
Statistical analysisAll the data from each participant were collected and recorded in an Excel spreadsheet. Statistical analysis was performed using PSPP software (version 1.6.2; Free Software Foundation, Boston, Massachusetts, USA). A significance level of p < 0.05 was applied in the analysis.
The normality of the variables was assessed using the Kolmogorov-Smirnov test, which revealed that most variables did not follow a normal distribution. Therefore, non-parametric tests were applied.
For each age group, the significance of differences between the control group and the oculomotor dysfunction group was analysed using the Mann-Whitney U test. This was done for both subjective and objective oculomotor parameters obtained with the NSUCO test and the Clinical Eye Tracker, respectively. To evaluate the significance of differences in sex and handedness distribution between groups within each age range, the Chi-square test was used. Finally, the level of correlation between the oculomotor parameters was examined using the Spearman correlation coefficient. All statistical tests were two-tailed, and p-values < 0.05 were considered statistically significant.
ResultsGeneral clinical dataA total of 47 children (aged 7 to 13 years; mean age = 9.29 [SD = 1.83]) were enrolled, with two distinct groups: CG (n = 16) and ODG (n = 31). The sample was further divided into three age groups as follows: 17 children in Group 1 (ages 7–8), 24 children in Group 2 (ages 9–11), and 6 children in Group 3 (ages 12–13).
Oculomotor analysisTable 2 shows the visual characteristics of the group with oculomotor dysfunction and the control group.
Summary of the main visual characteristics of the group with eye movement dysfunction and the control group involved in the study, according to age.
IQR, interquartile range; RE, right eye; LE, left eye; D, diopter; CDVA, corrected distance visual acuity; NPC, near point of convergence (cm); G1, group 1; G2, group 2; G3, group 3. exophoria values are represented in negative sign.
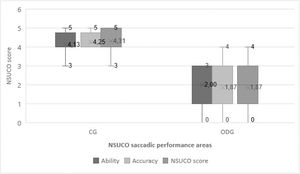
Table 3 summarizes the results of the saccadic eye movement analysis using the NSUCO test and the Eye tracker. Significant differences were found between groups in the three aspects of saccades evaluated with the NSUCO test (p < 0.001), with children from the ODG obtaining lower scores (Fig. 2).
Summary of the comparative statistical outcomes of the oculomotor examination in the two groups involved in the study: the control group (CG) and the oculomotor dysfuncion group (ODG).
| Mean (SD)Median (Range) | CG (n = 16) | ODG (n = 31) | P-value |
|---|---|---|---|
| NSUCO test | |||
| Saccadic ability | 4.13 (0.64)4.00 (3.00 to 5.00) | 2.12 (0.78)2.00 (1.00 to 3.00) | <0.001a |
| Saccadic precision | 4.27 (0.46)4.00 (4.00 to 5.00) | 2.00 (0.87)2.00 (1.00 to 3.00) | <0.001a |
| Body and head movements associated | 4.33 (0.62)4.00 (3.00 to 5.00) | 1.53 (0.62)1.00 (1.00 to 3.00) | <0.001a |
| Eye tracker analysis | |||
| Number of cycles 0.5 s | 18.73 (6.65)16.00 (13.00 to 37.00) | 17.38 (4.01)15.00 (14.00 to 25.00) | 0.455 |
| 1 s | 14.07 (1.98)15.00 (9.00 to 16.00) | 14.36 (1.34)15.00 (11.00 to 15.00) | 0.910 |
| % of regressions 0.5 s | 31.12 (9.91)29.00 (15.00 to 51.40) | 32.19 (5.64)31.05 (23.00 to 40.30) | 0.526 |
| 1 s | 32.26 (7.00)31.80 (13.00 to 43.50) | 37.39 (6.38)37.50 (21.00 to 47.10) | 0.012a |
| Number of completed saccades 0.5 s | 13.80 (5.12)15.00 (5.00 to 28.00) | 11.25 (4.96)14.00 (1.00 to 15.00) | 0.089 |
| 1 s | 10.50 (2.85)11.00 (5.00 to 15.00) | 8.71 (3.27)8.50 (4.00 to 15.00) | 0.114 |
| % of completed saccades 0.5 s | 75.63 (21.56)83.33 (33.33 to 100.00) | 66.63 (31.35)76.14 (6.67 to 100.00) | 0.411 |
| 1 s | 75.06 (19.35)73.33 (45.45 to 100.00) | 61.69 (24.57)60.00 (26.67 to 100.00) | 0.178 |
| Number of hypometric saccades 0.5 s | 4.20 (2.40)3.00 (2.00 to 10.00) | 7.88 (4.88)7.50 (2.00 to 21.00) | 0.010a |
| 1 s | 3.79 (2.97)3.00 (0.00 to 10.00) | 6.00 (2.77)6.50 (1.00 to 10.00) | 0.044a |
| Number of hypermetric saccades 0.5 s | 1.47 (1.46)1.00 (0.00 to 4.00) | 1.69 (1.78)1.00 (0.00 to 7.00) | 0.830 |
| 1 s | 0.57 (0.94)0.00 (0.00 to 3.00) | 1.14 (1.56)0.50 (0.00 to 5.00) | 0.401 |
| % hypometric saccades/completed 0.5 s | 32.19 (16.81)26.67 (13.33 to 66.67) | 57.99 (30.18)60.00 (13.00 to 100.00) | 0.022a |
| 1 s | 34.74 (21.87)34.85 (0.00 to 71.43) | 63.81 (27.07)70.00 (7.14 to 100.00) | 0.003a |
| % hypermetric saccades/completed 0.5 s | 10.85 (11.83)6.67 (0.00 to 40.00) | 19.83 (25.04)14.36 (0.00 to 100.00) | 0.370 |
| 1 s | 6.19 (10.14)0.00 (0.00 to 33.33) | 12.18 (14.02)5.56 (0.00 to 33.33) | 0.376 |
SD, standard deviation.
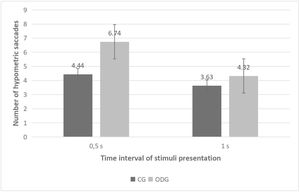
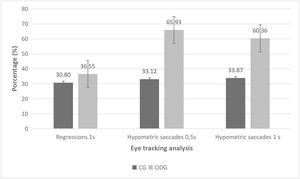
The Eye Tracker analysis revealed statistically significant differences between the groups in the number of hypometric saccades (Fig. 3). Additionally, differences were observed in the percentage of hypometric saccades relative to the total number of completed saccades for both stimulus presentation time intervals used in the evaluation (0.5 and 1 s, p ≤ 0.044) (Fig. 4). Specifically, the ODG exhibited a higher number of hypometric saccades than the CG, with a greater proportion of these anomalous movements relative to the total number of completed saccades. Furthermore, a significantly higher percentage of regressions was observed in the ODG compared to the CG when the stimulus presentation time interval was 1 s (p = 0.012) (Fig. 4). However, this difference was not statistically significant for the 0.5-second time interval (p = 0.526).
Diagram showing the statistically significant differences found between control group (CG) and oculomotor dysfunction group (ODG) in the percentage of regression detected with the eye tracker using a time interval of presentation of stimuli of 1 s as well as in the percentage of hypometric saccades detected using time intervals of 0.5 and 1 s; (s, second).
Several statistically significant correlations were found between the outcomes of the NSUCO test and the Eye Tracker measurements. The percentage of regressions for a 1-second stimulus interval, as measured by the Eye Tracker, showed significant correlations with three NSUCO test categories: ability (r = −0.416, p = 0.028), precision (r = −0.467, p = 0.012), and body/head movement (r = −0.465, p = 0.013). Similarly, significant correlations were observed between the number of saccades completed during a 0.5-second stimulus interval and the NSUCO scores for ability (r = 0.467, p = 0.012) and precision (r = 0.442, p = 0.019). A comparable pattern was found for the percentage of saccades completed during a 1-second stimulus interval, which correlated with ability (r = 0.489, p = 0.008) and precision (r = 0.449, p = 0.017).
The number of hypometric saccades during the 0.5-second stimulus interval showed significant correlations with NSUCO scores, including ability (moderate, r = −0.575, p = 0.001), precision (moderate, r = −0.536, p = 0.002), and body/head movement (weak, r = −0.398, p = 0.024). Similarly, the percentage of hypometric saccades relative to the total number of completed saccades for the 0.5-second stimulus interval significantly correlated with all three NSUCO scores: ability (moderate, r = −0.491, p = 0.004), precision (weak, r = −0.452, p = 0.009), and body/head movement (weak, r = −0.379, p = 0.033). Moderate to strong correlations were also found for these variables using the 1-second stimulus interval: ability (r = −0.495, p = 0.007), precision (r = −0.563, p = 0.002), and body/head movement (r = −0.494, p = 0.008). Finally, Table 4 summarizes the results of the linear regression analysis for all significant relationships identified.
Summary of the outcomes of the linear regression analysis for these relationships among subjective and objective oculomotor parameters showing statistically significant correlations in the whole sample (Y, objective parameter; X, subjective parameter) with NSUCO test.
| Relationship | Linear equation | R2 | P-value |
|---|---|---|---|
| Percentage regressions 1 s – Ability NSUCO | Y = 40.39 −1.77*X | 0.096 | 0.108 |
| Percentage regressions 1 s – Precision NSUCO | Y = 40.63–1.81*X | 0108 | 0.088 |
| Percentage regressions 1 s – Head/body movement associated NSUCO | Y = 39.52–1.61*X | 0.118 | 0.073 |
| Number saccades completed 0.5 s – Ability NSUCO | Y = 8.61+1.20*X | 0.083 | 0.109 |
| Number saccades completed 0.5 s – Precision NSUCO | Y = 9.19+1.01*X | 0.069 | 0.146 |
| Number saccades completed 1 s – Ability NSUCO | Y = 5.92+1.17*X | 0.214 | 0.013a |
| Number saccades completed 1 s – Precision NSUCO | Y = 5.84+1.17*X | 0.230 | 0.010a |
| Number hypometric saccades 0.5 s – Ability NSUCO | Y = 12.18–1.99*X | 0.349 | <0.001a |
| Number hypometric saccades 0.5 s – Precision NSUCO | Y = 11.09–1.63*X | 0.274 | 0.002a |
| Number hypometric saccades 0.5 s – Head/body movement associated NSUCO | Y = 9.29–1.13*X | 0.173 | 0.018a |
| Percentage hypometric saccades 0.5 s – Ability NSUCO | Y = 84.81–12.71*X | 0.324 | 0.001a |
| Percentage hypometric saccades 0.5 s – Precision NSUCO | Y = 79.15–10.86*X | 0.276 | 0.002a |
| Percentage hypometric saccades 0.5 s – Head/body movement associated NSUCO | Y = 69.61–8.34*X | 0.217 | 0.007a |
| Percentage hypometric saccades 1.0 s – Ability NSUCO | Y = 82.25–10.49*X | 0.211 | 0.014a |
| Percentage hypometric saccades 1.0 s – Precision NSUCO | Y = 86.71–11.65*X | 0.280 | 0.004a |
| Percentage hypometric saccades 1.0 s – Head/body movement associated NSUCO | Y = 74.94–8.76*X | 0.219 | 0.012a |
SD, standard deviation. aStatistical significant p-value.
Several statistically significant correlations were found between the results obtained with the NSUCO and the Eye Tracker. In age group 1, for the 0.5 s interval in the Eye Tracker, NSUCO ability showed a significant correlation with the number of hypometric saccades (moderate, r = −0.524, p = 0.02) and the percentage of hypometric saccades (strong, r = −0.851, p < 0.001). For a stimulus interval of 1 s, NSUCO ability was correlated with the number of complete saccades (strong, r = 0.809, p < 0.001), the percentage of complete saccades (strong, r = 0.762, p < 0.001), and the percentage of hypermetric saccades (moderate, r = −0.523, p = 0.041).
The accuracy of the NSUCO was significantly correlated with the number of complete saccades (moderate, r = 0.530, p = 0.038), the percentage of complete saccades (moderate, r = 0.526, p = 0.03), and the percentage of hypometric saccades (weak, r = −0.145, p < 0.001) for a stimulus interval of 0.5 s. Similar correlations were found for the same variables using a stimulus interval of 1 s, with the number of complete saccades (r = 0.853, p < 0.001), the percentage of complete saccades (strong, r = 0.802, p < 0.001), and the percentage of hypometric saccades (weak, r = −0.112, p < 0.001). The same applies to head movements studied with the NSUCO, which showed a significant correlation with the percentage of regressions (moderate, r = 0.547, p = 0.031), the number of complete saccades (moderate, r = 0.512, p = 0.019), and the percentage of complete saccades (moderate, r = 0.547, p = 0.02) for a stimulus interval of 0.5 s.
In Group 2, the percentage of regressions was negatively correlated with the three NSUCO skills: skill (moderate, r = −0.495, p = 0.019), precision (moderate, r = −0.530, p = 0.015), and head movements (strong, r = −0.616, p = 0.003). Additionally, the percentage of hypometric saccades in stimulus intervals of 1 s showed a very weak correlation with NSUCO precision (r = −0.050, p = 0.042), while the number of hypometric saccades for this same interval was moderately correlated with head movements (r = −0.482, p = 0.027).
In Group 3, strong correlations were found between the ability to perform saccadic movements assessed with the NSUCO and the number of complete saccades for a 1-s stimulus interval assessed with the Eye Tracker (very strong, r = 0.982, p = 0.004). For the same group, there was also a correlation between NSUCO saccade precision and the number of complete saccades (very strong, r = 0.953, p = 0.015) and the percentage of complete saccades (very strong, r = 0.981, p = 0.003) for a 1-s interval.
For the total sample, significant correlations were found with the percentage of Eye Tracker regressions for a 0.5-s stimulus interval (moderate, r = 0.552, p = 0.001). The number of complete saccades in the 0.5-s interval was correlated with the accuracy of the NSUCO (moderate, r = −0.329, p = 0.021).
For this same interval, there was also a negative correlation between the ability and precision of the NSUCO and the percentage of hypometric saccades (moderate, r = −0.396, p = 0.004) and (weak, r = −0.028, p = 0.023).
In the 1-s interval, the ability and precision of the NSUCO were respectively correlated with the number of complete saccades (moderate, r = 0.344, p = 0.022) and (moderate, r = 0.430, p = 0.004) and the percentage of complete saccades (moderate, r = 0.345, p = 0.025) and (moderate, r = 0.439, p = 0.007). There was a significant negative correlation between the accuracy of the NSUCO and the percentage of hypometric saccades (moderate, r = −0.325, p = 0.042).
DiscussionThe objetive of this pilot study was to explore saccadic eye movements in children using two different assessment tools: the subjective NSUCO test and an objective eye-tracking system. In addition, performance was compared between children with oculomotor dysfunction and a control group, and potential age-related differences were analyzed across three age groups. Despite the small sample size, preliminary results indicate that both assessment methods were able to detect differences in saccadic performance. Furthermore, some age-related trends were observed, suggesting that age may influence oculomotor function.
The established diagnostic criteria for oculomotor dysfunction have yet to be validated on a large scale. Maples et al.13 attempted this with the NSUCO, which specifically evaluates the saccades. One drawback is the influence of factor such as the examiner's need for control, the language barriers or the patient's attention. To address these limitations, research has focused on using eye tracking to eliminate biases introduced by the examiner's subjectivity.19,20 However, the ability to assess the saccadic remains crucial, as has already been demonstrated.12,13,15,17,20–23
In light of the results obtained, differences were found between the CG and ODG across all three age groups and in all categories assessed with the NSUCO, with worse values in the group with oculomotor dysfunction. This indicates significant differences in oculomotor assessment scores between children with oculomotor impairments and normative populations. Similar findings have been reported in several studies.12,14,15
Additionally, it is observed that in all three assessed categories, both in the CG and ODG, older age is associated with better ability, greater precision, and fewer head movements, although these improvements are less pronounced in the ODG compared to the CG. These findings align with those of Maples et al.,13 which explain the development and standardization of the NSUCO test and establish a correlation between age and test performance. Similarly, studies by Fukushima et al.24 and Stewart et al.25 suggest that the precision of initial saccadic movements is greater in adults than in children.
Likewise, in our study, the percentage and number of hypometric and hypermetric saccades are higher in the ODG across all age groups, with a greater increase in older children. In this group, the percentage of regressions also increases with age. This finding is noteworthy because, according to Rayner et al.26 and Blythe et al.27,28 regressions tend to decrease with age. This aligns with the observation that patients with oculomotor dysfunction tend to exhibit more regressions.
Blignaut et al. (2019)20 objectively compared the correlation between the two tests and found that the Eye Tracker has greater sensitivity in detecting hypometric and hypermetric saccades, as well as smaller deviations compared to subjective tests. Additionally, the same study reports a strong correlation between objective and subjective systems. This may explain the lack of significance in saccadic ability and precision observed in age group 3 with the NSUCO.
In group 1 (ages 7 to 8),NSUCO ability was negatively correlated with the number and percentage of hypometric saccades in 0.5-second intervals. Walker et al. (2019)29 found that children with sensory processing disorder (SPD) exhibit deficient oculomotor skills compared to children with typical development. However, for a 1-second interval, NSUCO ability was positively correlated with the number and percentage of complete saccades and negatively with the percentage of hypermetric saccades. Sinno et al.30 reported normative values for saccades and smooth pursuit in children aged 5 to 17 years, observing that saccadic accuracy improves with age, which supports the positive correlation with complete saccades and negative correlation with hypermetric saccades. These results are consistent, as a low score in NSUCO ability and precision indicates that the patient performs fewer complete saccades, leading to a higher number of hypometric and hypermetric saccades.
In group 2 (ages 9 to 11), a moderate correlation was found between the three NSUCO skills and the percentage of regressions with 1-second latencies, especially in individuals with a higher number of head movements. Namaeh et al.31 provided normative data for objective measures of vergence and saccades in children aged 9 to 17, highlighting the importance of accuracy and latency in assessment. Furthermore, in this group, the number of hypometric saccades in 1 s was correlated with NSUCO accuracy.
In group 3 (ages 12 to 13), a strong correlation was found between saccadic ability assessed with the NSUCO and the number of complete saccades for a 1-second stimulus interval. In this group, NSUCO precision was positively correlated with both the number and percentage of complete saccades for the same interval. Bucci et al.32 studied the development of horizontal saccades in children aged 6 to 15 years, finding that saccadic accuracy improves significantly with age, which supports the strong correlation found in our study.
Similar results were found in a study by Bilbao et al.,23 which analyzed a sample of children aged 6 to 12 with oculomotor dysfunction. Specifically, a correlation was observed between saccadic ability, precision, and reduced head/body movements in cases with a higher percentage of regressions.
Combining subjective tests such as the Northeastern State University College of Optometry (NSUCO) test with eye-tracking technology can offer a more comprehensive and practical evaluation strategy for assessing saccadic eye movements by leveraging the strengths of both approaches while mitigating their individual limitations.
Subjective tests like the NSUCO test are accessible, quick to perform, and easy to integrate into clinical practice. They rely on examiner judgment to assess saccadic performance, which can be beneficial for initial screenings and in settings where advanced technology is not available. However, these tests can be limited by their subjective nature and potential variability between examiners.
Eye-tracking technology, on the other hand, provides a detailed and quantifiable analysis of saccadic behavior. It offers objective measurements of parameters such as latency, peak velocity, and accuracy, which are crucial for diagnosing and monitoring neurological conditions.33 For instance, the study by Demian et al. established evaluative standards using video oculography (VOG) to objectively measure saccadic parameters across different age groups, highlighting the utility of such technology in clinical settings.33,34 Similarly, Kullmann et al. demonstrated the reliability of portable eye-tracking devices in assessing oculomotor and cognitive functions, further supporting their clinical application.
By combining these methods, clinicians can benefit from the rapid and accessible nature of subjective tests for initial assessments and use eye-tracking technology for detailed, objective analysis when needed. This hybrid approach allows for a more thorough evaluation of saccadic eye movements, enhancing diagnostic accuracy and patient care while addressing the limitations of each method individually.
This study presents several limitations that should be acknowledged. First, the overall sample size was small, with a particularly small control group, raising concerns about its representativeness and limiting the generalizability of the findings. Additionally, group 3 had a very limited number of participants, which may have affected statistical significance, increased variability, and reduced the statistical power of the comparative analyses.
Another important limitation is the lack of explicit information regarding the number of participants with and without oculomotor dysfunction within each of the three age groups. This information is crucial for interpreting the findings and should be clearly reported in future research.
Although neurodevelopmental disorders were not an exclusion criterion, we acknowledge that detailed diagnoses were not systematically recorded. This allowed for a more representative sample but may have introduced variability affecting oculomotor outcomes. Future studies should collect this information in a standardized.
It should also be noted that group 2 included participants across three different age ranges, while groups 1 and 3 each spanned only two, potentially introducing additional heterogeneity. Furthermore, the use of subjective tests inherently carries the limitation of examiner bias, which may have influenced the outcome interpretation.
We acknowledge that dividing the sample into three age groups further reduced the number of participants per group, limiting the statistical power to detect age-related differences. Nevertheless, this stratification was intentionally applied to reflect the developmental trajectory of oculomotor control in childhood, as supported by previous research. Despite the inherent constraints of a pilot study, this grouping allowed for a preliminary exploration of age-related patterns, which may help guide future studies aiming to establish age-specific normative data.
Given the variability observed in the results and the limited sample size of this pilot study, future research should include a formal sample size calculation and significantly increase the number of participants. This would help to enhance statistical power, improve the reliability of findings, and strengthen the diagnostic validity of both subjective and objective assessment tools. Additionally, it would be valuable to include other complementary tests, such as the DEM test, to explore correlations between different oculomotor assessment methods in pediatric populations.
ConclusionsAs age increases, the skill and precision of saccadic movements improve, and head movements decrease, with lower scores observed in the group with oculomotor dysfunctions. Furthermore, hypometric saccades and regressions are consistent indicators of oculomotor dysfunction, regardless of age. These can be detected using objective eye tracking analysis, as well as the subjective NSUCO test, which is easy to implement in clinical settings.
This study is the first, to our knowledge, to demonstrate a significant correlation between objective oculomotor analysis obtained through an Eye Tracker system and the subjective NSUCO test. In fact, oculomotor parameters derived from the Eye Tracker can be predicted based on the categories evaluated by the NSUCO subjective test. This finding has important clinical implications, confirming the validity of the NSUCO as a quick and effective method for assessing eye movements in children with oculomotor dysfunctions and healthy children, especially when Eye Tracker technology is not available due to economic or logistical constraints.
Author contributionsConceptualization, C.B., R.H.A. and D.P.P.; methodology, C.B., R.H.A., ACB. and D.P.P.; formal analysis, D.P.P.; investigation, C.B., ACB. and D.P.P.; resources, C.B. and D.P.P.; data curation, C.B., ACB. and D.P.P.; writing—original draft preparation, C.B., J-O.C-M.; writing—review and editing, C.B., R.H.A., ACB., D.P.P. and J-O.C-M.; supervision, D.P.P.. All authors have read and agreed to the published version of the manuscript.
FundingNo funding for this study.
The authors have no conflict of interest to declare. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Data available on request due to privacy/ethical restrictions. Conflicts of Interest: The authors declare no conflict of interest.