To determine the effect of main morphological types and grades of age-related cataracts on refractive error.
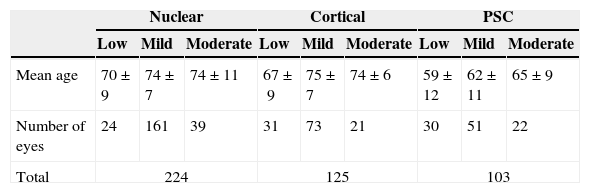
MethodsWe measured 276 subjects with optical compensation prior to the development of cataract. We evaluated 224 eyes with nuclear cataract, 125 with cortical cataract, and 103 with posterior subcapsular (PSC) cataract classified with LOCSIII. We measured visual acuity (VA) with their spectacles and best-corrected visual acuity (BCVA) with chart in decimal scale to obtain the optimal compensation with cataract. We evaluated the differences between compensations.
ResultsA significant myopic shift was observed in nuclear cataract from low to mild grade (p=0.031), the same as for PSC cataract from mild to advanced grade (p=0.025). No significant changes were found for cortical cataract (p=0.462). Regarding astigmatism, we observed power changes in cortical cataract from low to mild grade (p=0.03) and axis changes in PSC from low to mild grade (p=0.02) and in nuclear cataract from mild to advanced grade (p=0.02).
ConclusionsCataract produces changes in patient's compensation which depend on severity and type of cataract. For nuclear and PSC cataract, we observed that the higher the grade of severity, the greater the myopic shift. Power astigmatic changes were found in cortical cataract and axis changes in PSC and nuclear cataract.
Determinar el efecto sobre el error refractivo de los principales tipos morfológicos y grados de catarata asociada a la edad.
MétodosMedimos a 276 sujetos con compensación óptica, previamente a la aparición de la catarata. Evaluamos 224 ojos con catarata nuclear, 125 con catarata cortical, y 103 con catarata subcapsular posterior (CSP), clasificados con el sistema LOCSIII. Medimos la agudeza visual (AV) con sus gafas, y la mejor agudeza visual corregida (MAVC) con un test en escala decimal, para obtener la compensación óptima con la catarata. Evaluamos las diferencias entre las compensaciones.
ResultadosSe observó un cambio considerable en la catarata nuclear, al pasar del grado bajo al leve (p=0,031), al igual que en la catarata subcapsular posterior al pasar de grado leve a avanzado (p=0,025). No se observaron cambios en la catarata cortical (p=0,462). En cuanto al astigmatismo, observamos cambios de potencia en la catarata cortical al pasar de grado bajo a leve (p=0,03) y cambios en el eje en la catarata subcapsular posterior al pasar de grado bajo a leve (p=0,02), y en la catarata nuclear al pasar de grado leve a avanzado (p=0,02).
ConclusionesLa catarata produce cambios en la compensación del paciente, que depende de su severidad y tipo. En la catarata nuclear y subcapsular posterior, observamos que cuanto mayor era el grado de severidad, mayor era el cambio miópico. Se hallaron cambios de potencia astigmática en la catarata cortical, y cambios en el eje en la catarata subcapsular posterior y nuclear.
Healthy ageing of the eye shows a gradual hypermetropic change with time,1–4 but when a cataract appears, this hyperopic shift disappears.3
The symptoms that a particular type of cataract produces in a patient's vision are not the same and depend on the type and grade of maturity of the cataract. Apart from opacification in the formation of cataract, refractive changes occur that alter the patient's vision.
Some studies affirm that nuclear cataract can cause a myopic shift in some cases.1–3,5–11 Nevertheless, the effect of cortical and posterior subcapsular cataract on refractive error is less clear. Regarding cortical cataract, there are studies that suggest that cortical opacity can induce hyperopic shifts1,12 and a significant astigmatic shift.5,13,14 In the case of PSC cataract, some studies report that this type of cataract is associated with myopic compensations,6,15 but others state that PSC cataract can induce hyperopic shifts1; however further studies affirm that PSC cataract causes refractive changes similar to age-matched control groups with clear lenses.5 So, different studies report contradictions in their results in some cases, and none of them uses the degree of maturity of the cataract as a variable in their analyses.
In this paper, we aim to provide new data on the refractive changes that patients experience, depending on the type of cataract they are developing. Moreover, we propose to correlate such refractive changes with the grade of maturity of the cataract, which could explain some of the contradictions found in different studies.
MethodsThis study adheres to the tenets of the Declaration of Helsinki for Research Involving Human Subjects and was approved by the Institutional Review Board.
All the patients involved in the study were diagnosed of age-related cataract. They did not present retinopathies or any other ocular pathology that could affect the results.
Exclusion criteria were patients who had anomalies or guttas in their endothelial count, patients undergoing ocular treatment of any nature for at least one month prior to the commencement of the study or who had been taking medication that could produce somnolence – antihistamines, etc. – or who had a history of drug addiction or alcoholism, patients who did not dilate properly with mydriatics or cycloplegics, and diabetic patients with or without retinopathies.
All the patients selected used optical compensation prior to the development of cataract. Patients who did not use any type of optical compensation previously were excluded from the study, as although they might have been considered emmetropes, there could also have been cases of non-corrected low optical compensation which would distort the result. Moreover, to ensure that optical compensation was present prior to the development of cataracts, all patients who had not been using their current optical compensation for over two years were excluded from the study. In addition, all the patients were asked about the onset of their symptoms to ensure that the compensation of their spectacles was not modified after the symptoms appeared and that they had a good visual acuity with such spectacles before their problems with cataracts.
Initially, 515 patients with cataract who fulfilled the above requirements were evaluated; 132 patients with pure nuclear cataract, 81 patients with pure cortical cataract, 63 patients with pure PSC cataract, and 239 patients with combined cataract. In total, 224 eyes with nuclear cataract, 125 eyes with cortical cataract and 103 eyes with PSC cataract were analyzed. In this study we did not analyze combined cataracts. Mean age of selected patients was 70±9 years, and we recruited 163 eyes of men and 289 of women.
The tests were performed monocularly and we chose patients who were able to provide accurate responses during subjective refraction.
All the patients studied underwent the following vision examination (in this order):
- –
Measurement of refractive correction of the patients’ spectacles. This was determined using automated focimetry (TOPCON model EZ-200) and was recorded to the nearest 0.25D (the power) and 1 degree (axis of the cylinder). Astigmatism was recorded in the negative cylinder form.
- –
VA with their spectacles and BCVA with optotypes in decimal scale. We did not use logMAR scale because most of our patients had visual acuities more than 0.3 decimal units (20/60), and, with this value, we have more accuracy with decimal than with logMAR scale.
- –
Optimal refractive compensation was determined using an autorefractometer (TOPCON, model KR-8800) and subjective refraction with an automated phoropter (TOPCON, model CV-3000). The Jackson cross cylinder was used to determine astigmatism subjectively and subjective refraction was also measured to the nearest 0.25D (sphere and cylinder) and 1 degree (axis of cylinder).
Type and grade of cataract was defined based on slitlamp biomicroscopy after pupil dilatation with tropicamide (10mg/ml) and phenylephrine (100mg/ml), and lens examination was performed according to Lens Opacities Classification System III (LOCSIII),16,17 using the retroillumination images that illustrate the various stages of cortical, nuclear and PSC cataract. To categorize the cataract, we placed the test in an autoilluminated portable screen near the patient's shoulders to be able to see simultaneously the image of the patient's eye through the slitlamp and the LOCS test.
The efficiency and repeatability of this test have already been demonstrated.17 However, before initiating our study, the two ophthalmologists involved carried out tests to check that their criteria were comparable and to verify that significant differences between their diagnoses were not present. They obtained a coincidence rate between their criteria of more than 85%. Regarding opacity, distinction was made as shown in the test; the cataracts were classified as low (up to degree 2 in the test), mild (degree 3–4) and advanced (degree 5 or higher, only in nuclear cataracts). Table 1 shows how many eyes we examined in each group. We tried to include at least 20 eyes for each group. This was a difficult task, because according to our study, we have in our population 28.4% of nuclear cataracts, but only 6.2% of cortical cataracts and 5.9% of PSC cataracts.18
In order to prevent the two optometrists involved in the study from knowing in advance what type of cataract the patient had, the grading of cataract was the last procedure performed. With this procedure, we avoided some biases in the measurement of the optical compensation.
Statistical analysisFor the analysis of the results, we used vectorial notation. The polar form of the spectacle correction of patients as well as of the optimal compensation required were recorded in a spreadsheet and converted into spherical equivalents (M) and vectors J0 (ortho-astigmatism) and J45 (oblique astigmatism),19,20 defined as:
where S is the spherical power and C is the cylinder power at θ axis.We used the differences between both measurements of spherical and astigmatic refraction, respectively. We considered a myopic shift when differences between both measurements were lower than 0D, and hyperopic shift when these differences were higher than 0D. According to Ray and O’Day,21 the data from both eyes of one patient are not independent values, so if we include the data of both eyes as independent variables, we are duplicating the data. But according to our previous published statistical studies,18 in Spain 93.2% of our patients suffered bilateral cataract, but only in 72.5% of women and in 66.3% of men we could find the same grade of opacity in both eyes. Our data also showed patients with different grades of opacity and types of cataract in both eyes, and we could observe in some patients that the same type and grade of opacity could generate different levels of refractive change. We found differences between eyes of the same patient in the changes of the cylinder in nuclear and cortical cataracts (p=0.05) as well as in the best-corrected visual acuity (BCVA) in PSC cataracts with the same grade of opacity (p=0.01). In our sample, from 132 patients with nuclear cataract, we used only one eye of each patient in 60 of them. In cortical cataract, we used only one eye in 43 of 81 patients involved and in SCP we used only one eye in 29 of 63 patients.
Despite these factors, we compare both eyes of the same patient, and we observed that the type and the grade of cataract in our sample between eyes were statistically different (p=0.0008). With all this data analysis, we decided to use the information of both eyes of the same patient as independent variables.
The differences between cataract morphology, grade of opacity, spherical refractive error shift, and astigmatic changes in refraction were determined with analysis of variance (ANOVA) with Scheffé F test post-hoc significance testing. The null hypothesis was rejected if p<0.05.
ResultsIn all cases, we observed that the BCVA of all the patients improved with the new optic compensation, with a mean of improvement of 0.17 decimal units (from a mean visual acuity of 20/43 to 20/32) (p=0.000). The improvements were lower in higher grade of opacity for nuclear (0.16 decimal unit) and PSC cataract (0.10 decimal unit). For cortical cataract, we did not observe a great improvement regardless of the grade of opacity. We observed some patients that did not improve their VA when we compensate them. Specifically, a total of 4 eyes with low cortical cataract (12.9%) and one eye with advanced cortical cataract (4.8%), 5 eyes with low nuclear cataract (20.8%), 20 eyes with mild nuclear cataract (12.4%), and 6 eyes with advanced nuclear cataract (15.4%), 9 eyes with low SCP cataract (30%), 11 with mild SCP cataract (21.6%) and 4 eyes with advanced SCP cataract (18.2%) did not show any visual improvement with the new optical compensation.
In the cases in which we analyze BCVA and optical compensation of both eyes of the same patient, we observed that, although type and grade of cataract were equal in both eyes, the effect on optical compensation and BCVA were different between eyes.
The patients’ age was fairly homogeneous within the same type of cataract for mild and advanced grade (p>0.05). However, when we compared the patients with advanced grade of cataract and those with low grade, the advanced grade patients were statistically older than the lower group, regardless of the type of cataract. In addition, if the population groups of each type of cataract are compared, it can be seen that patients with PSC cataract were significantly younger than those with cortical or nuclear cataract.
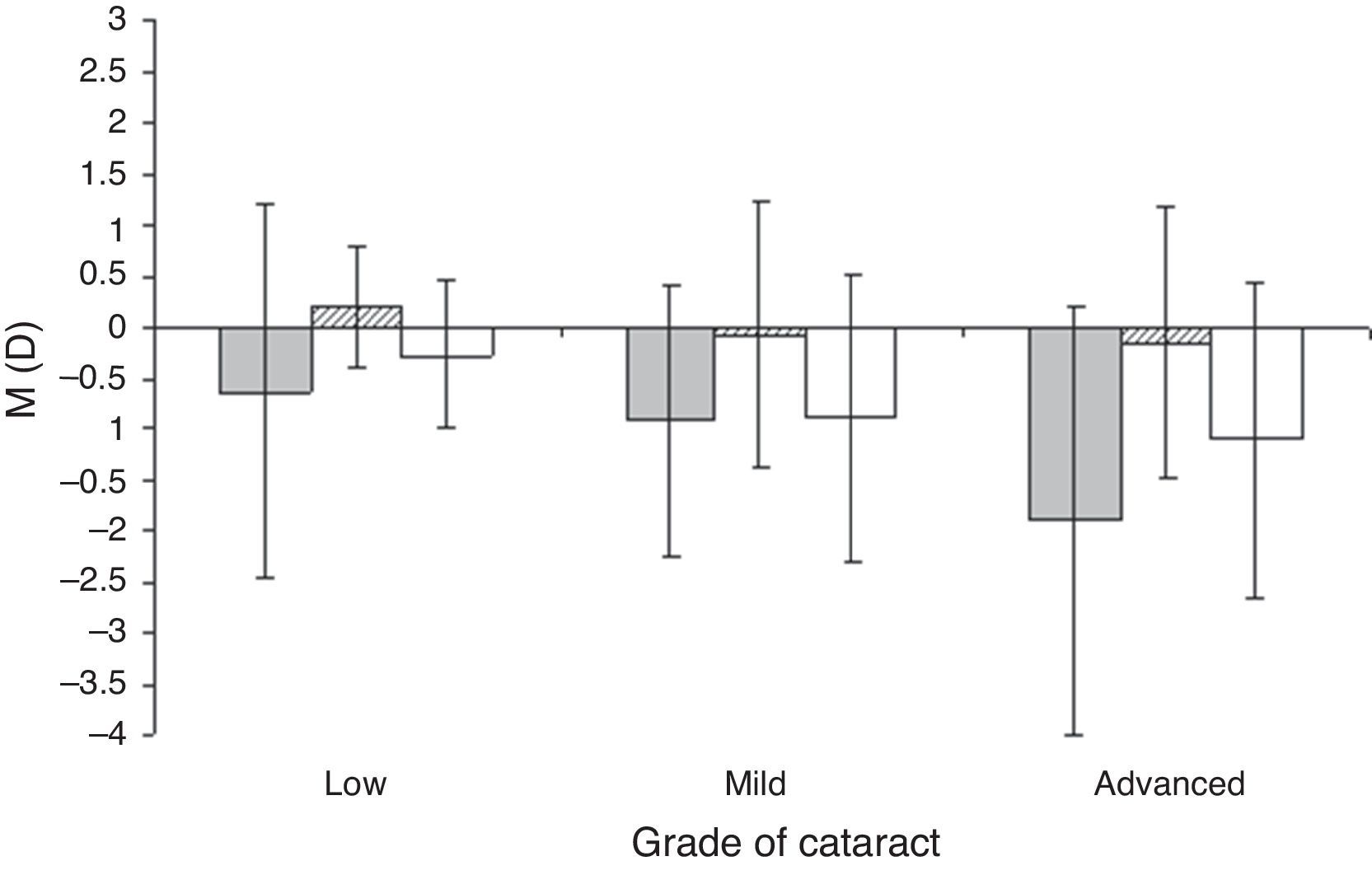
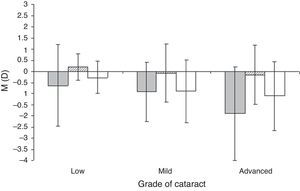
Fig. 1 shows the variation of the spherical component (M) for each type and grade of cataract. These data show significant differences in low grade between cortical and PSC cataract (p=0.037), in mild grade between cortical and PSC cataract (p=0.007) and between cortical and nuclear cataract (p=0.000), and in severe grade between cortical and PSC cataract (p=0.001) and between nuclear and PSC cataract (p=0.019).
With regard to the cataract grade, there was a significant myopic shift in the nuclear cataract from low to mild stage (p=0.031). The nuclear cataract varied from a slight myopic shift (in M component) of −0.27D in low stage to a mean myopic shift of −0.91D in mild stage. In the PSC cataract, the grade of development was more significant in severe stage (p=0.025) compared to moderate stage, and also compared to low grade (p=0.031). PSC changed from a mean myopic shift of −0.63D in low grade to a myopic shift of −0.92D in mild grade and to a myopic shift of −1.89D in severe grade. With regard to the cortical cataract, no significant variations were found when the grade of opacity changed (p=0.462), although we observed a slight myopic shift when the opacity increased (±0.21D at low stage, −0.07D at mild stage and −0.15D at severe stage).
The relationship between the M component and the grade of cataract could be adjusted by a linear equation (r2=0.91 for cortical and PSC cataract and r2=0.92 for nuclear cataract). In all cases the slope of the linear adjust was negative, so we can conclude that there was a myopic shift with the grade of opacity. Moreover, according to the value of the slope, we can conclude that the rate of myopic shift with the grade of opacity was higher in PSC cataract (slope of −0.63) than in the other two types of cataract (slopes of −0.18 in cortical cataract and −0.41 in nuclear cataract).
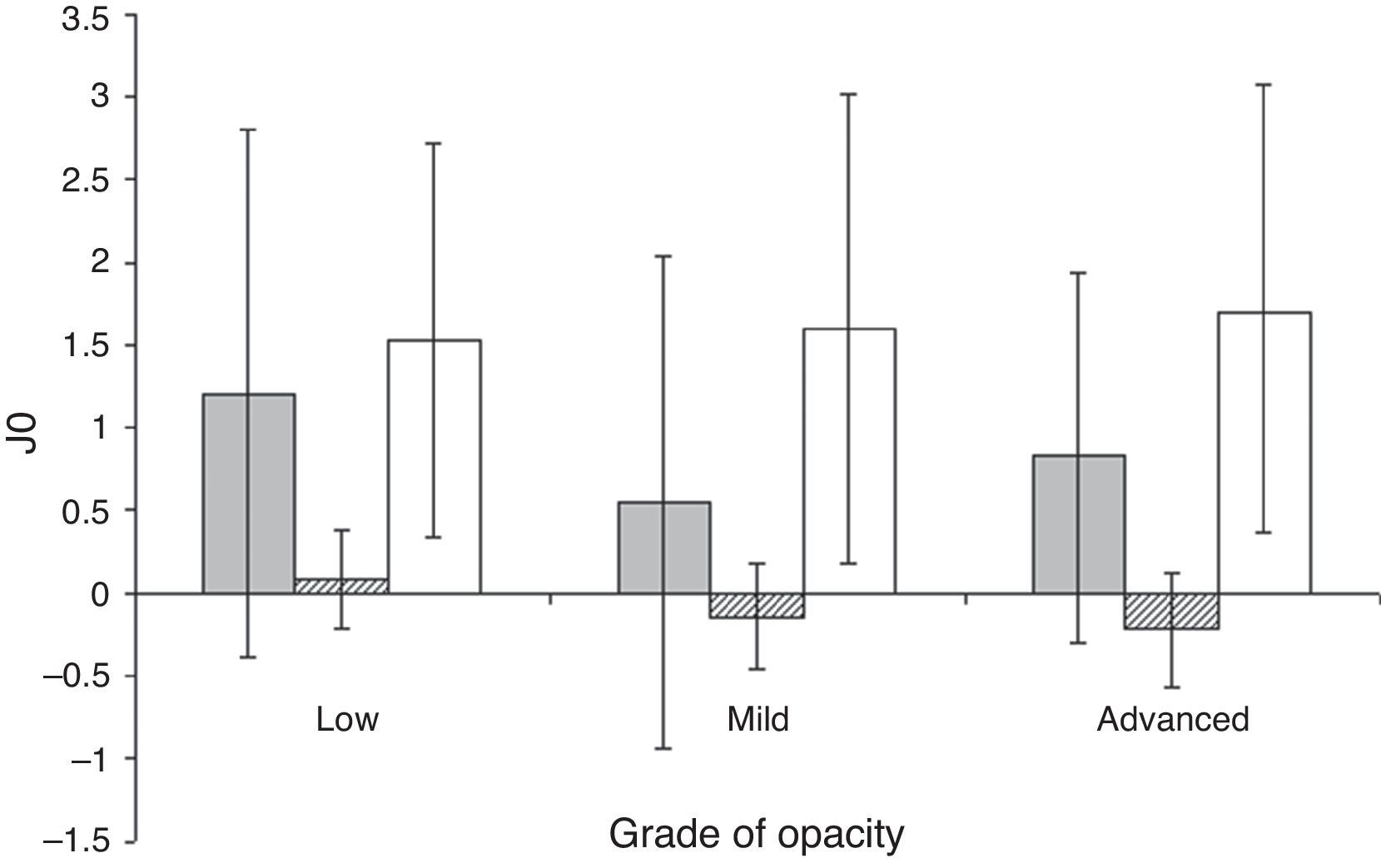
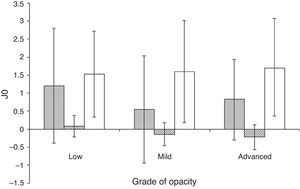
Fig. 2 shows the mean of the variation of the ortho-astigmatism component (J0) for each of the three types of cataract and depending on the grade of opacity. In this case, we observed significant differences between cortical and nuclear component regardless of the grade of opacity (p=0.000). We also observed the same trend between cortical and subcapsular J0 component (p=0.003 at low grade, p=0.008 at mild grade and p=0.021 at severe grade). We also observed significant differences between nuclear and PSC J0 component, but only at mild (p=0.000) and severe grade (p=0.022). Regarding the behaviour of this component with the grade, no statistically significant changes in the ortho-astigmatism component as the grade of opacity increased was observed for any of the three types of cataract.
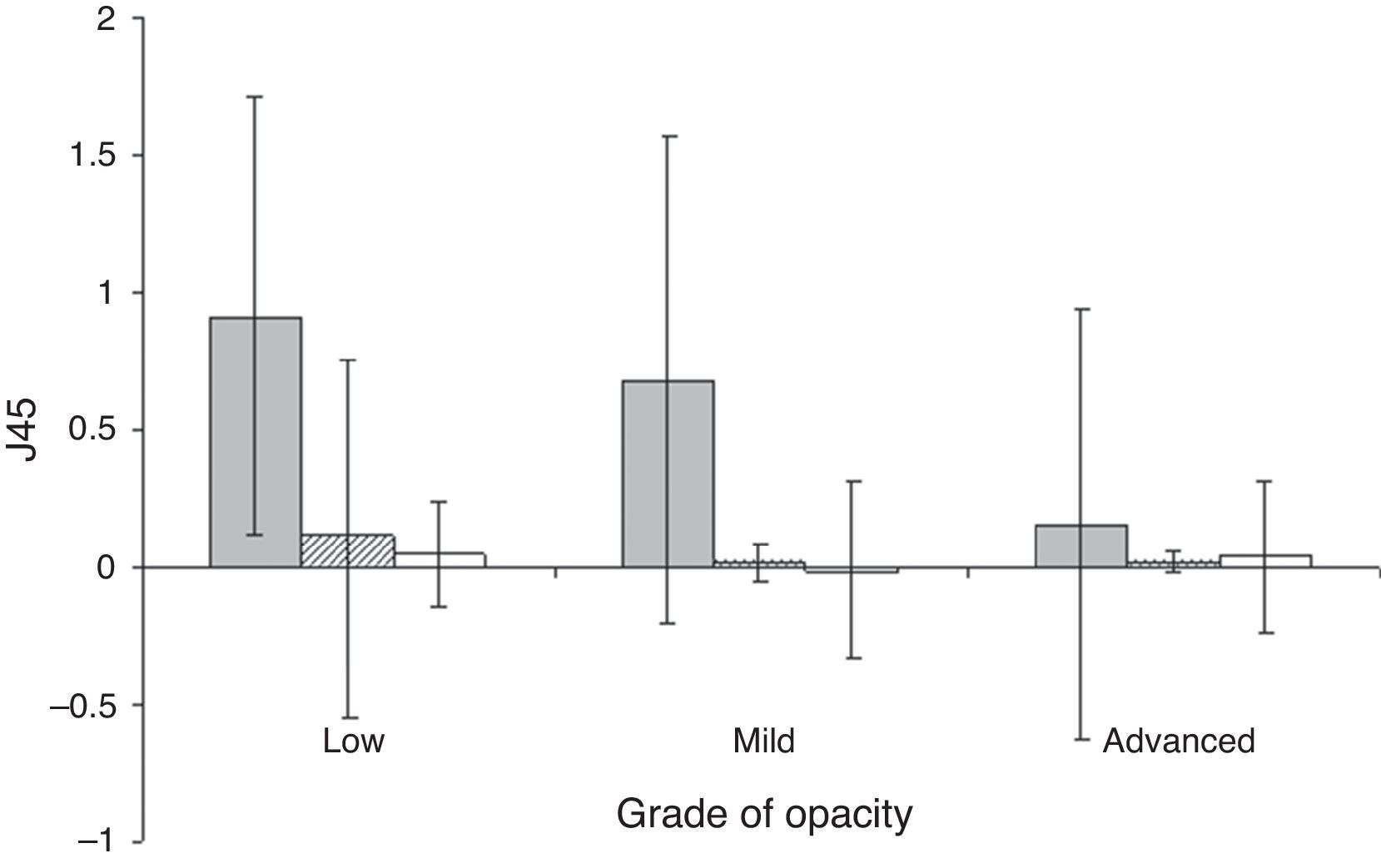
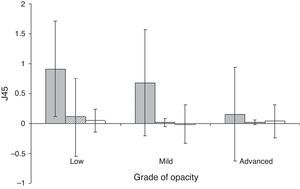
Fig. 3 shows the mean of the variation of the oblique-astigmatism component (J45) for each of the three types of cataract and depending on the grade of opacity. We observed significant differences between cortical and PSC J45 component at low (p=0.002) and mild stage (p=0.000), and between PSC and nuclear J45 component at the same grades of opacity (low: p=0.001, mild: p=0.006). No significant changes were found at advanced stage. Regarding the behaviour of this component with the grade, no statistically significant changes in the oblique-astigmatism component as the grade of opacity increased was observed, except for PSC cataract between low and advanced stage (p=0.036) and mild and advanced stage (p=0.025).
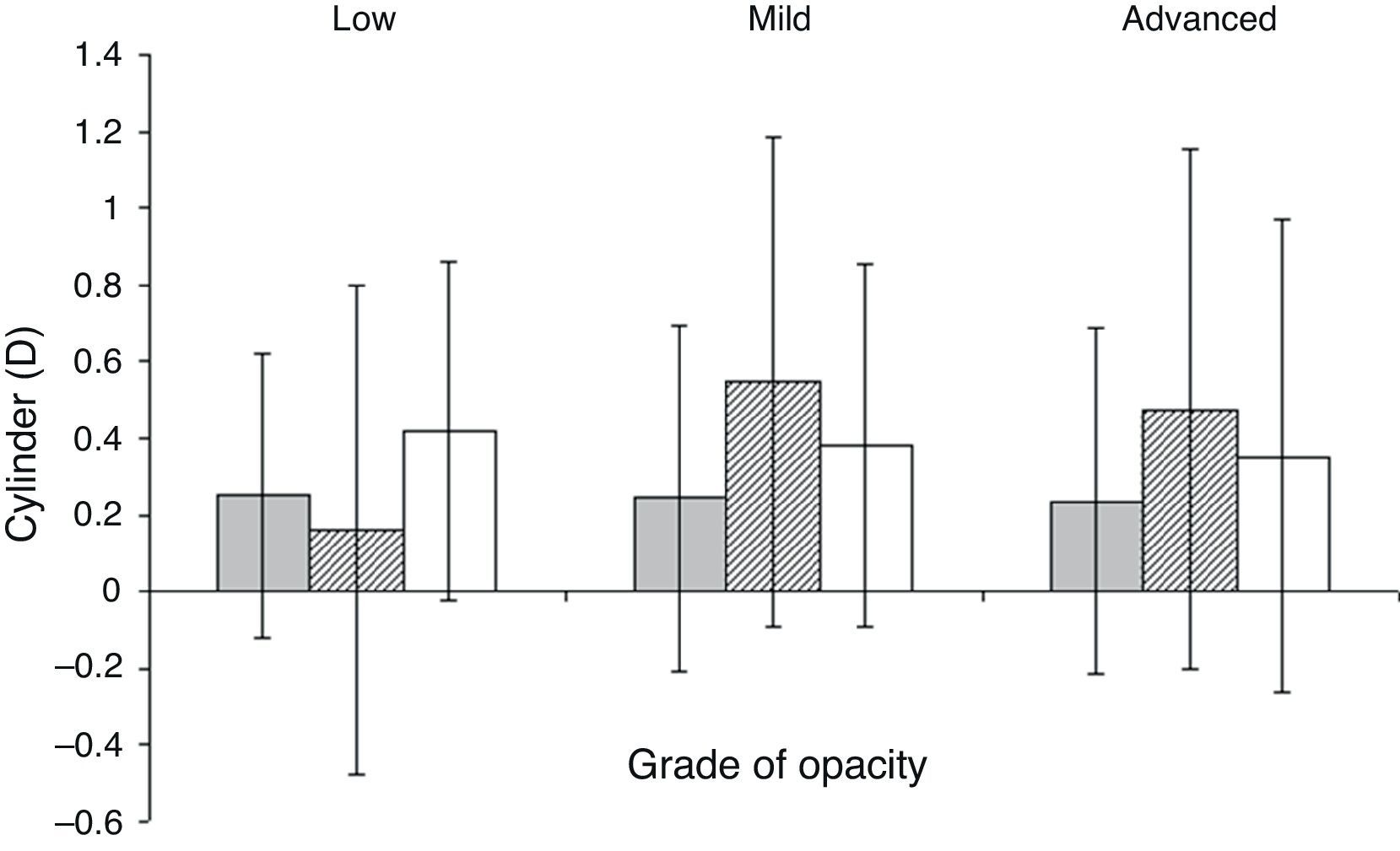
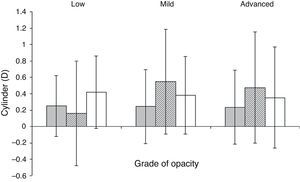
Fig. 4 shows the variation of the cylinder for each type and grade of cataract when we recompose the result obtained. We observed that the mean changes of cylinder power were less than 0.75D. We found the greatest changes for mild cortical cataracts (0.5±0.8D). When we compared between different cataract morphologies, we observed statistical differences between cylinder changes of cortical and PSC cataract at mild grade (p=0.01). We only observed statistical changes between low and mild grade of cortical cataract (p=0.03).
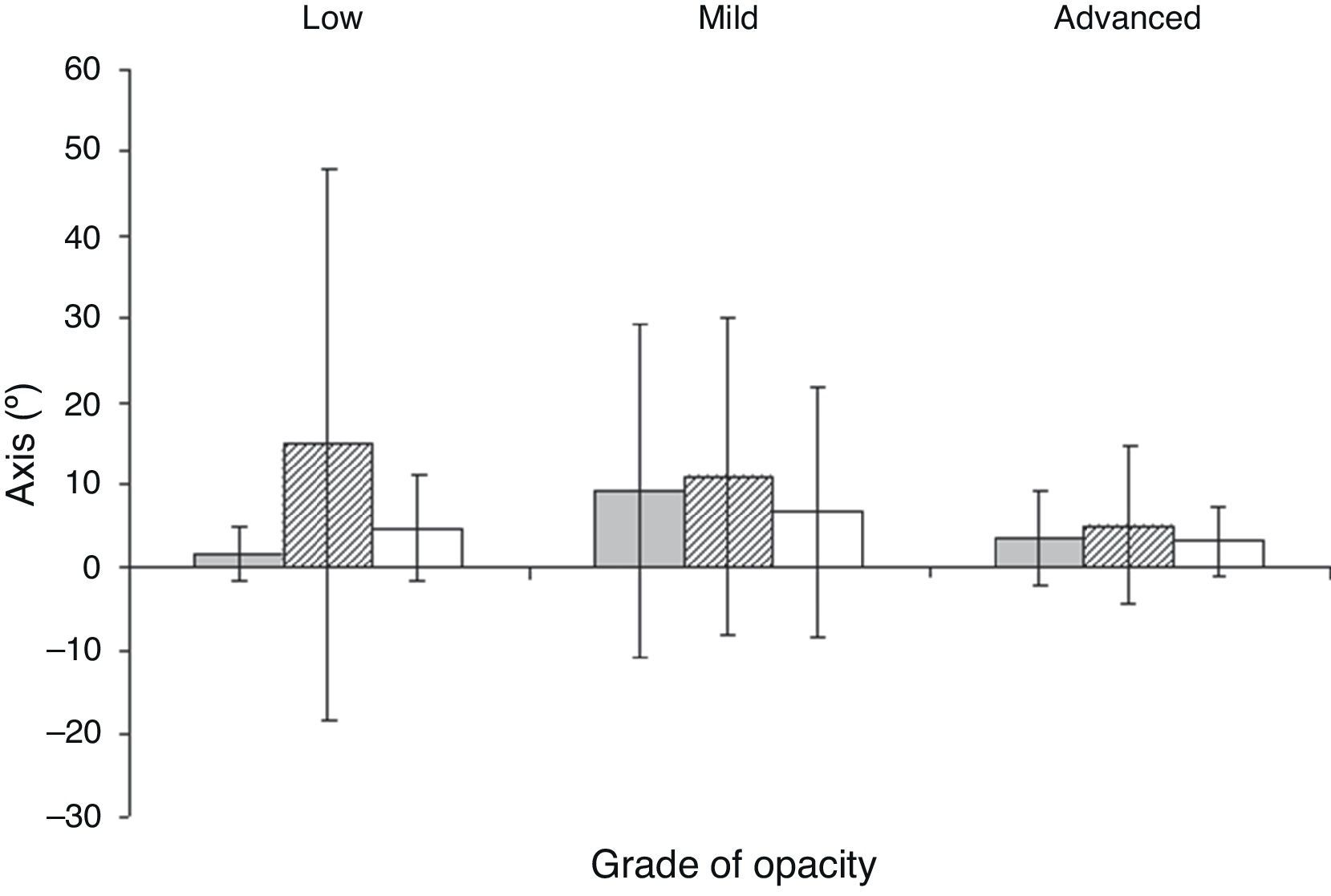
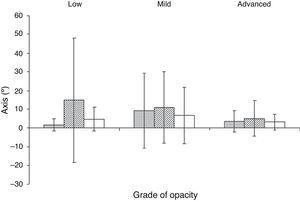
Fig. 5 shows the changes of the axis for each type and grade of cataract. We found the greatest changes in cortical cataract. Between cataract morphologies, we only observed statistical differences between cortical and PSC cataract at low grade (p=0.04). With regard to the grade of opacity, we only observed statistical differences between low and mild grade of PSC cataract (p=0.02) and between mild and advanced grade in nuclear cataract (p=0.02).
DiscussionAccording to the studies in the literature, there is no clear cut-off point at which normal ageing changes in the lens end and cataract begins.5,22,23 We can find studies that consider healthy subjects those patients with nuclear cataract less than 1.5 of opacity22 or 2.0,5,23 patients with cortical cataract of 122 or 2.05 of opacity, and PSC cataract less than 1 of opacity.22 In our study, patients with a grade of opacity less than 2.0 have been considered as patients with low grade of opacity and not as normal patients. All the patients enrolled in this study had a loss of VA caused by a cataract, so it does not seem logical to consider them as normal patients.
The fact that VA improves significantly when the patient is again compensated indicates that the refraction really changes with the cataract, as the patient attains a better VA with a different compensation from that present initially in their spectacles, before the development of the cataract. But, in severe grade of opacity (specially in PSC cataract, 18.2% of the eyes analyzed), most of the patients did not improve their VA when we compensated them. In nuclear and cortical cataract, these percentages were lower than in PSC cataract (13.7% for nuclear cataract and 14.3% for cortical cataract). In these cases we considered that the poor visual quality of these patients avoids a correct estimation of the grade of myopia that they had with the cataract.
In our study, we included patients with the same type and grade of opacity in both eyes, but the effect on their optical compensation was different in each eye. We also observed that BCVA could be different in patients with the same type and grade of opacity, or in the same patient with the same kind of cataract in both eyes. This fact could explain that we obtained a high dispersion in our data.
Nuclear cataractAs reported in other studies,1–3,5–11 nuclear cataract causes a significant myopic shift, probably on account of symmetrical refractive index changes within the nucleus of the lens, causing negative spherical aberration and a myopic shift.24
Our data confirm these results and also demonstrate that the degree of myopic shift clearly depends on the grade of opacity, as when the latter increases, so does the degree of myopic shift.
Our results also show that as the grade of the cataract development increases, so does the percentage of patients who are myopised, changing from 12 (50%) patients in the low grade to 33 (84.4%) in the severe grade, with ever greater levels of myopic shift. There was, however, a small group of patients with nuclear cataract who experienced a hyperopic shift, but with mean values of 0.50D. Finally, 27 (12%) nuclear patients analyzed in this study did not experience any variation in their spherical component when the cataract appeared.
Regardless of astigmatism, no significant changes were found in the power when the grade of opacity increased. But we found significant axis changes between mild and advanced grade, although this change was very small (of 3.5°). Pesudovs et al.5 found astigmatic changes in nuclear cataract, but they concluded that there were no significant.
PSC cataractThe PSC cataract presents a similar development to the nuclear cataract, confirming thus the studies reporting that the PSC cataract induces a myopic shift.6,15 There are 22 (21.3%) patients with this type of cataract who do not present spherical changes. As in the previous case, the rate of myopised patients increases with the severity of the cataract, changing from 13 (43.3%) patients in the low grade to 16 (72.7%) patients in the severe grade. In the few cases in which the patients experienced hyperopic shifts, these values do not exceed 0.5 D.
Nonetheless, the rate of myopic shift was very different in nuclear and PSC cataract. PSC cataract effect on the sphere during its development is greater than the effect that a nuclear cataract produces. However, some studies1,5 state that the PSC cataract does not cause changes in optical compensation other than those presented by a normal subject of the same age. This discrepancy may basically be due to two reasons. First, patients with PSC cataract belong to the group with the fewest number of patients when compared with the other two types of cataract. This is because it was difficult to find patients with PSC cataract at our latitude, as they are the least plentiful patients with pure cataract. Moreover, this type of cataract has great visual symptomatology,25,26 which makes it even more difficult to find severe cases. In any event, the number of patients analyzed in our study is similar to that of other studies.5 For this reason, although our data are fairly clear, a large sample with new patients should be studied in order to verify this result, as our sample was small when compared with cases of cortical and nuclear cataract that were analyzed.
Second, in the studies in which the results were contradictory to those encountered in our research work, the grade of maturity of the cataract was never taken into account. This suggests that the discrepancies were because there were differences in optical compensation depending on the grade of maturity, as can be concluded from our study.
Regardless of astigmatic changes, no statistical changes were found with the power of the cylinder as the grade of opacity increased, but we found a significant axis change between low and mild grade (from 1.7° to 9.2°). Again, Pesudovs et al.5 found astigmatic changes in PSC cataract, but they concluded that there were no significant.
Cortical cataractRegarding cortical cataract, our data indicate the same as those found in several studies1,5 in which the patients do not manifest changes other than those presented by a patient without cataract. In principle, this result seems logical as cortical cataract only affects the outer area of the visual field; consequently the central area of the crystalline lens seems to remain in good condition, just as that of a normal subject of the same age. An aberrometric analysis showed that patients with cortical cataract tend to show a slight positive spherical aberration, which is similar to control subjects with clear lenses.24
Regarding astigmatic changes, our results confirm those from other studies5,13,14,24 that report that cortical cataract produces an astigmatic effect on the patient's compensation. We found that there is a significant astigmatism change when the grade of opacity increases. According to the literature, this astigmatism changes must be caused by asymmetrical refractive index changes within parts of the cortex of the lens,27 causing coma-like aberration and astigmatic changes in refractive error.24 So, we can also confirm that cortical cataract produces astigmatism changes, in opposite to those studies28,29 in which astigmatism changes were not encountered.
But this study has a limitation. We have a great dependence on the accuracy of the spectacle compensation, that we did not measure it. Moreover, astigmatism changes with age, due to corneal, ocular muscle tone and lens changes with age.30,3 In our data, astigmatism changes may be due to all these factors, and we cannot distinguish between them. To exclude corneal contribution, we may have performed a corneal topography to any patient prior to the development of the cataract. So, at this point, we must be careful when analyzing astigmatism changes with age.
To conclude, our results generally corroborate previous studies in which authors state that refractive changes are produced with the development of cataract, and that such changes depend on the type of cataract. But in addition, we demonstrate that these refractive changes also depend on the grade of severity of the cataract and on the type of cataract. In the case of nuclear and PSC cataract, a greater myopic shift is observed when the grade of severity is higher. Regarding cortical cataract, the significant changes are observed in the astigmatism.
Financial supportNo financial support was received for this submission.
Conflict of interestNone of the authors have conflict of interest with the submission.