Monocular use of reduced-aperture optics in the form of a corneal inlay or contact lens may improve near vision of presbyopes by increasing their depth-of-focus (DOF). However, the associated induced interocular differences in retinal illuminance may cause distortion in spatial perception due to the Pulfrich effect.
MethodsThree young subjects were used to explore the Pulfrich effect during reduced-aperture monovision using afocal contact lenses (in the non-dominant eye) which were either opaque with a central clear aperture of 1.5, 2.5 or 3.5mm diameter, or had an annular opaque stop of inner and outer diameters 1.5 and 4.0mm, respectively. The two-alternative forced choice (2AFC) task of the subject was to state whether a 2° circular spot appeared in front or behind the plane of a central cross when moved left-to-right or right-to-left. The retinal illuminance of the dominant eye was varied using neutral density (ND) filters to establish the ND value which eliminated the Pulfrich effect for each lens.
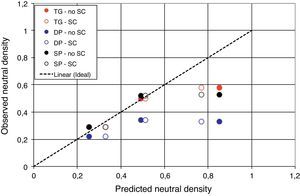
ResultsThe Pulfrich effect was observed with all the lenses. The ND value required to null the effect decreased as the diameter of the aperture of the lenses increased. A reasonably good agreement was found between observed ND values for the different lenses and those predicted from the relative areas of the effective pupils of the two eyes. Minor discrepancies were attributed to decentration of the contact lenses with respect to the natural pupils.
ConclusionsReduced-aperture monovision generates marked Pulfrich-type distortions in spatial perception under conditions where the visual world is changing dynamically as a result of movement.
El uso monocular de lentes de apertura reducida en forma de implante o lentes de contacto, pueden mejorar la visión de los pacientes présbitas gracias al incremento de su profundidad de enfoque. Sin embargo, las diferencias interoculares a nivel de iluminancia retiniana pueden originar una distorsión de la percepción espacial debido al efecto Pulfrich.
MétodosSe utilizó a tres pacientes jóvenes para explorar el efecto Pulfrich durante la inducción de monovisión de apertura reducida utilizando lentes de contacto afocales (en el ojo no dominante), que eran, bien opacas con una apertura central de 1,5, 2,5 ó 3,5mm de diámetro, o tenían un tope opaco anular con diámetros interiores y exteriores de 1,5 y 4,0mm, respectivamente. La tarea mediante 2AFC (dos alternativas de elección forzada) para el sujeto fue la de establecer si aparecía una mancha circular de 2 grados en el frente o posterior al plano de una cruz central cuando se movía de izquierda a derecha, o de derecha a izquierda. Se varió la iluminancia retiniana del ojo dominante utilizando filtros DN (densidad neutra) para establecer el valor DN que eliminaba el efecto Pulfrich para cada lente.
ResultadosSe observó el efecto Pulfrich con todas las lentes. El valor DN necesario para anular el efecto se reducía a medida que se incrementaba la apertura de las lentes. Se halló una concordancia razonable entre los valores DN observados para las diferentes lentes y aquellos predichos a partir de las áreas relativas de pupila efectiva de los dos ojos. Las pequeñas discrepancias se atribuyeron a descentramientos de las lentes de contacto con respecto a las pupilas naturales.
ConclusionesLa monovisión de apertura reducida genera unas marcadas distorsiones de tipo Pulfrich en la percepción espacial, en condiciones en las que el mundo visual se modifica dinámicamente como resultado del movimiento.
Although several different contact-lens approaches have been devised to provide reasonable standards of both distance and near vision for presbyopes, including spectacle overwear, monovision, simultaneous image, and alternating image methods, these have not succeeded in meeting the visual needs of all patients. It has, however, long been known that the DOF of the eye may be increased by reducing the pupil diameter. Many years ago it was therefore suggested that contact lenses, which were opaque except for a small central aperture might, by increasing the DOF, provide enhanced near vision for presbyopes while still allowing good distance vision.1 Efron2 suggests that the lens be worn monocularly in the non-dominant eye. The disadvantage of such lenses is that less light contributes to the retinal image, so that the wearer finds vision more difficult under mesopic or scotopic conditions. There may also be a reduction in visual field,2 leading to problems with mobility. As a result of these major limitations, reduced-aperture contact lenses have found little application, except as artificial pupils for albinos.3
Recently, however, this concept has re-emerged in the form of a monocularly implanted corneal inlay with a small, central, clear aperture, the other eye having a natural pupil4: the optical principles involved seem to be related to an earlier design of contact lens.5 The inlay is normally implanted in the non-dominant eye of the presbyopic emmetrope and the approach might be termed reduced-aperture monovision. The inlay which is currently commercially available is the Kamra (originally Acufocus) inlay (Acufocus Inc., Irvine, USA). This consists of a thin, quasi-opaque disc with an outer diameter of 3.8mm and a central clear aperture 1.6mm in diameter.6 The inner diameter represents a compromise between improved DOF, light loss and optical quality, since diffraction with smaller diameters degrades retinal image quality and acuity.7 The outer diameter was presumably selected on the basis of minimizing any obstruction of nutrients and waste products through the cornea, allied to the desire to increase retinal illuminance under dim lighting conditions when the natural pupil dilates behind the inlay: the normal appearance of the iris is largely preserved. The inlay is surgically inserted at about halfway through the thickness of the cornea. Clinical reports suggest good levels of patient satisfaction and useful improvements in binocular intermediate vision, near vision and reading performance, the effects being stable for up to 4 years.8–12 A laboratory study confirms that binocular acuity at near is similar to that achieved monocularly by the eye with the inlay.13 It is claimed that inlays have the advantage of being minimally invasive and easily reversible. Obviously the same basic approach could be implemented with a well-centred contact lens giving similar pupil geometry, with the advantage that the contact lens could be powered to correct any ametropia.
Although the reduced-aperture monovision approach may yield adequate distance and near static acuity, particularly if some small residual myopia is left in the reduced-aperture eye,14 several problems arise with this attempted solution for the difficulties of presbyopes, including reduced stereopsis and losses in binocular acuity and contrast sensitivity.15 We address here the problems that may arise in spatial vision when viewing a highly dynamic scene, as when the individual is walking or driving. These occur because, with monocular wear of a reduced-aperture contact lens or inlay, a substantial difference can exist between the retinal illuminances in the two eyes. As is well known, such a situation leads to the induced Pulfrich effect and distortion in the apparent path of objects which are moving with respect to the observer. The resultant misinterpretations of the relative positions, sizes and speeds of objects may cause significant problems with mobility and driving. Here we discuss first the characteristics of the Pulfrich and related effects, and then some experiments in which the Pulfrich effect is demonstrated to occur during reduced-aperture monovision using contact lenses. It is confirmed that the effects are largely explicable in terms of the relative retinal illuminances in the two eyes.
The Pulfrich effectIf a neutral density (ND) filter is placed in front of one eye, the path of moving objects is distorted. This effect (the induced or provoked Pulfrich effect) is best known for the way it distorts the apparent path of a simple pendulum swinging in a fronto-parallel plane, so that the pendulum bob appears to follow an elliptical path in depth rather than moving in a plane. The apparent departure of the path from the plane increases with the density of the filter, at least over the range up to about 0.4<ND<1.4.16 This distortion occurs largely as a result of the interocular difference in visual latency arising as a result of the difference in retinal illuminance between the two eyes.17,18 Spiegler19,20 has discussed the theoretical impact of the effect on the apparent position, size and velocity of objects moving both in the fronto-parallel plane and in planes which are not perpendicular to the line of sight. Related effects can also manifest themselves during various other types of motion,21 unilateral cataract,22,23 unilateral wear of such light-absorbing devices as the X-Chrom lens, or unilateral mydriasis.16,17 The Pulfrich effect (the spontaneous Pulfrich effect) is also found in patients suffering increased latency in one eye due to pathology or trauma.16,24–28 In practical terms these motion-related spatial distortions mean that patients may experience difficulties in moving about their environment at home, at work or when driving.22–24,29 Clinical symptoms in both the induced and spontaneous Pulfrich effect can usually be eliminated or much reduced by placing an appropriate ND filter in front of the eye with the shorter visual latency, so that its latency is increased to match that of the other eye.23,24,26,30
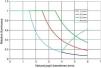
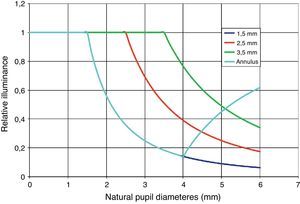
Materials and methodsPupil aperturesIn the experiments that follow, four types of afocal, hand-painted, opaque soft contact lenses (74% water content, Cantor & Nissel Ltd., Brackley, UK) were used. Three were opaque over an 8mm diameter but had central clear circular apertures of 1.5, 2.5 or 3.5mm in diameter. The fourth was clear except for a central annular opaque region, which had an inner diameter of 1.5mm and an outer diameter of 4.0mm. If we assume that the lens is centered to the natural pupil and that the natural pupil diameters in the two eyes are the same, the effective entrance pupil geometry in the contact lens-wearing eye is modified by that of the lens. The changes in the relative retinal illuminance in the eyes (i.e. retinal illuminance in the eye with the reduced-aperture contact lens/retinal illuminance in the eye with the natural pupil) as a function of the natural pupil diameter can then be calculated in terms of the relative areas of the pupils. The relative illuminance in eyes wearing each of the four types of contact lens is shown in Fig. 1. If required, allowance can be made for the reduction in effective pupil area due to Stiles–Crawford effect under photopic conditions,31 but this has only minor impact for the normal range of natural photopic pupil diameters. When correcting for the Stiles–Crawford effect, the actual area of a pupil of radius ρ is weighted by the factor [(1−exp(−βρ2))/βρ2], where β is the Stiles–Crawford coefficient and in the present study is assigned a value of 0.116.31
The retinal illuminance in the eye wearing a reduced-aperture contact lens relative to that of the eye with its natural, unobstructed pupil. The contact lenses have either central apertures 1.5, 2.5 or 3.5mm in diameter, or an annular opaque area with inner and outer diameters of 1.5 and 4.0mm, respectively.
Note that in the case of the eye wearing the lens with an annular pupil (similar to that produced by the Kamra inlay) the relative illuminance starts to increase again once the natural pupil diameter exceeds the outer diameter of the opaque annulus. Thus, the annulus is advantageous not only in increasing the absolute retinal illuminance under low light-level conditions when the natural pupil is large but also in improving the balance of the retinal illuminance between the two eyes.
If the natural pupil diameter remains unchanged, the values of relative illuminance effectively correspond to the transmittance, T, of the ND filter that, when placed in front of the eye without the contact lens, would balance the retinal illuminances in the two eyes: the density of the filter would be log10(1/T). The aim of our experimental work was to determine whether this expectation would be fulfilled in practice.
Experimental procedureThree emmetropic subjects (ages 27, 32 and 42), with normal acuity and other visual characteristics, were used to explore the Pulfrich effect under reduced-aperture monovision, using afocal contact lenses with geometries as described above. No mydriatics or cycloplegics were used.
The Pulfrich stimulus was a circular red spot of angular diameter 2.0° moving sinusoidally in a horizontal direction on a display screen, with a period of 3s and an amplitude of 11.25°. The luminances of the spot and its achromatic background were 10 and 30cd/m2, respectively. The display, which also incorporated a large black fixation cross (angular dimensions: 1.5°), was placed at a distance of 40cm from the seated subject, whose head position was stabilized with a headrest. The resultant full angular subtense of the display was 45.3°×37.3°. The two-alternative, forced-choice task of the subject was to state whether the spot appeared in front or behind the plane of the fixation cross when the spot moved left-to-right or right-to-left.
Ambient lighting conditions were such that natural pupils under binocular observing conditions for all subjects were about 5.0mm. The luminance as viewed by the dominant eye was varied by using 13 combinations of ND filters, ranging from 0.13 to 1.48 ND in approximately 0.11 ND intervals, together with the “no filter” condition. With the non-dominant eye wearing each of the 3 contact lenses with circular apertures (diameters 1.5, 2.5 and 3.5mm), filters were presented in random order in front of the dominant eye. A total of 15 tests were carried out with each filter, to allow a psychometric function to be plotted. This was fitted with a cumulative Weibull distribution function of the form P=1−exp(−10b(x−t)), where P is the response probability, x is the ND value and b and t are the parameters that define the threshold (in ND) and the slope of the Weibull function, respectively. The ND corresponding to P=0.50 was taken as the value required to counteract the artificial anisocoria.
In the case of the contact lens with the opaque annulus (inner and outer diameters 1.5 and 4.0mm, respectively) in principle light could enter the non-dominant eye through both the central clear aperture and the clear, outer part of the lens outside the annulus. Three cases were explored with this lens:
- (i)
The non-dominant eye had no other artificial pupil and the dominant eye had a 4.5mm artificial pupil in its spectacle plane. In this case the natural pupil diameter of the non-dominant eye was about 5.0mm but this altered slightly as filters were placed in front of the dominant eye.
- (ii)
The non-dominant eye had an additional 4.5mm artificial pupil in its spectacle plane. The dominant eye had a similar 4.5mm artificial pupil.
- (iii)
The non-dominant eye had an additional 4.0mm artificial pupil in its spectacle plane, and the dominant eye had a similar 4.0mm artificial pupil. Nominally in this case, if the contact lens is ideally centred, only light from the central clear region of the “annular” CL should enter the non-dominant eye.
Preliminary experiments showed that, when no contact lenses or artificial pupils were used, a filter with a ND of at least 0.2 was required to reliably elicit an obvious Pulfrich effect. A marked Pulfrich effect was observed with all the lenses and subjects.
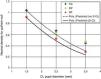
Fig. 2 shows the raw psychometric plots for the 3 CLs with circular central apertures. It will be noted that for all subjects the value of ND required to null the Pulfrich effect reduces as the diameter of the clear aperture of the contact lenses increases. Note additionally that the null point is generally fairly precisely defined, with a reliability ranging between ±0.04 and ±0.19 in ND.
Psychometric plots for 3 subjects of the probability of making the response “front” as a function of the value of the neutral density filter placed before the dominant eye, when the non-dominant eye wears a reduced-aperture contact lens with a central clear diameter as indicated. The values correspond to the neutral density required to null the Pulfrich effect (response probability, P=0.50). Reliability was calculated for the probability range between 0.25 and 0.75.
The results obtained for P=0.50 in the 3 cases when the “annular” contact lens was used are shown in Fig. 3. The filter value required to null the Pulfrich effect reduces as the amount of light which can enter the non-dominant eye from the region outside the CL's opaque annulus increases. Table 1 summarises the data for all lens conditions.
Psychometric plots for 3 subjects of the probability of making the response “front” as a function of the value of the neutral density filter placed before the dominant eye, when the non-dominant eye wears the annular contact lens (with inner and outer diameters of 1.5 and 4.0mm, respectively) with a natural pupil diameter (5.0mm) or an artificial pupil (of 4.5 and 4.0mm) placed in the spectacle plane. The values correspond to the neutral density required to null the Pulfrich effect (response probability, P=0.50). Reliability was calculated for the probability range between 0.25 and 0.75.
Results of the 3 subjects for the value (and the reliability) of the neutral density filter which nulls the Pulfrich effect under the pupil conditions studied with central clear aperture and the opaque annulus lenses (see text for details).
| Pupil diameter/Subject | TG | DP | SP |
| Values of ND for P = 0.50(and between 0.25 and 0.75) | |||
| Central clear aperture lenses | |||
| with 1.5mm aperture | 1.04 (±0.19) | 0.86 (±0.07) | 0.92 (±0.04) |
| with 2.5mm aperture | 0.67 (±0.10) | 0.64 (±0.11) | 0.53 (±0.03) |
| with 3.5mm aperture | 0.45 (±0.06) | 0.47 (±0.13) | 0.29 (±0.07) |
| Lenses with the opaque annulus | |||
| 4.0mm artificial pupils in both eyes | 0.58 (±0.01) | 0.33 (±0.05) | 0.53 (±0.04) |
| 4.5mm artificial pupils in both eyes | 0.50 (±0.02) | 0.34 (±0.01) | 0.52 (±0.03) |
| 5.0mm natural pupil in non-dominant eye, 4.5mm pupil in dominant eye | 0.29 (±0.02) | 0.22 (±0.10) | 0.29 (±0.01) |
The basic hypothesis was that the value of the ND filter required to null the Pulfrich effect under any set of conditions was that required to equalize the retinal illuminances in the two eyes, where the retinal illuminance in each eye was directly proportional to the clear areas of its effective pupil.
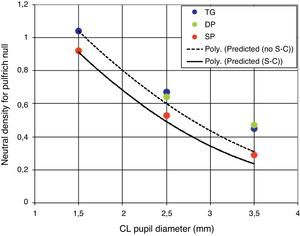
Fig. 4 shows the data for the cases in which the contact lens had a small central clear aperture. The full and dashed curves show theoretical predictions, respectively with and without allowance for the Stiles–Crawford effect, and the symbols the results obtained with the 3 subjects.
Values of ND filter required to null the Pulfrich effect when placed in front of the dominant eye, as a function of the diameter of the central clear aperture in the CL worn by the non-dominant eye. Both eyes have a fixed artificial pupil 4.5mm in diameter placed in their spectacle plane. The continuous and dashed curves are theoretical predictions based on the relative pupil areas, respectively, with and without correction for the Stiles–Crawford effect, and the assumption that all the pupils are ideally centred.
It can be seen that, while there is reasonably good agreement between theory and observation for the smallest, 1.5mm pupil, for 2 subjects and the 2.5 and 3.5mm pupils, a higher ND value is required than that predicted. We attribute this to the problems of centration with the contact lenses. Relative decentration of the clear aperture of the contact lens with respect to the 4.5mm artificial pupil may result in a reduction in effective pupil area for the non-dominant eye, due to the artificial pupil vignetting the aperture of the contact lens. This will create a requirement for increased filter density in front of the dominant eye.
Fig. 5 presents the results for the “annular” contact lens. In this case the observed filter values for the three configurations are plotted against those calculated on the basis that all pupils are exactly concentric. It can be seen that when the predicted values approach unity, the observed values are markedly lower. The highest value of ND corresponds to the case where the outer diameter of the opaque annulus matches the diameter of the 4.0mm diameter artificial pupil, so that ideally no light should enter the non-dominant eye from outside the annulus. It is clear that relative decentration between the two pupils must be increasing the light reaching the retina of the non-dominant eye and hence reducing the density required in front of the dominant eye to null the Pulfrich effect.
Results for the 3 observers and 3 conditions studied when the non-dominant eye wore the “annular” CL, as a function of the predicted values of ND. Filled symbols relate to predictions based simply on relative pupil areas, open symbols predictions where allowance is made for the Stiles–Crawford effect. The dashed line represents exact agreement with predictions.
In spite of these discrepancies occasioned by CL decentration, there is no doubt that small-aperture monovision generates the expected, marked Pulfrich-type distortions in spatial perception under conditions where the visual world is changing dynamically as a result of movement. The exact effects observed under real-world conditions will depend not only on the geometry of the small-aperture optics but also on the scene luminance and consequent natural pupil diameter (Fig. 1).
Experience with patients suffering from both the induced and spontaneous Pulfrich effects suggests that the spatial distortions experienced can adversely affect personal mobility and ability to cope with road traffic conditions, with the consequent risk of accident and injury.22,24–26,29 Although exact equivalence between the induced and spontaneous Pulfrich effects cannot be assumed, we note that the monocular filters required to null the Pulfrich effect and alleviate the symptoms in clinical patients typically lie in the range 0.1–0.5 ND.17,23 Under the various small-aperture monovision conditions used in the present study, filters with densities 0.2<ND<1.0 were required to null the induced Pulfrich effect. It might be expected, then, that in the absence of a correcting filter, under some conditions small-aperture monovision might lead to symptoms similar to those of the clinical patients, in at least some individuals. This is supported by the results of a recent study in which a 0.9 ND filter was worn in front of one eye, leading to a marked impact on the judgement of speed during driving.29 Although there is evidence that adaptation effects may reduce the Pulfrich-type distortions experienced as a result of interocular differences in retinal illuminance, the distortions persist at a reduced level.32–34 Adaptation is less likely to occur with small-aperture contact lenses than with permanent corneal implants, since the former are likely to be removed fairly regularly for at least part of the waking day.
Overall, the results suggest that reduced-aperture monovision can cause adverse distortions in spatial perception when there is relative movement with respect to the environment. Further limitations of this approach to presbyopic correction may include field restriction,2 and reduced stereopsis, contrast sensitivity and acuity.15 As a result of these deficiencies, we believe that small-aperture monovision is an unsatisfactory solution for the needs of the presbyope.
Conflicts of interestThe authors did not receive any financial support from any public or private sources.
IG Pallikaris forms the medical director of the Flexivue Corneal Inlay (Presbia). Sotiris Plainis, Dionysia Petratou, Trisevgeni Giannakopoulou, Hema Radhakrishnan and W Neil Charman have no proprietary or commercial interest in any material discussed.