The purpose of this study was to show the potential of a commercial center-distance multifocal soft contact lens to induce relative peripheral myopic defocus in myopic eyes.
MethodsTwenty-eight myopic right eyes from 28 patients (mean age: 22.0±2.0 years) were evaluated. The measurements of axial and off-axis refraction were made using a Grand-Seiko WAM-5500 open-field autorefractometer without lens and with multifocal contact lenses (Proclear Multifocal D® Design) of +2.00D and +3.00D add power applied randomly. Central mean spherical equivalent refraction was −2.24±1.33D. Ocular refraction was measured at center and at eccentricities between 35° nasal and 35° temporal (in 5° steps).
ResultsBaseline relative peripheral refractive error (RPRE) as spherical equivalent (M) was −0.69±1.14D and −0.46±1.38D at 35° in the nasal and temporal degrees of visual field, respectively. Both add powers increased the relative peripheral myopic defocus up to −0.82±1.23D (p=0.002) and −1.42±1.45D (p<0.001) at 35° in the nasal field; and −0.87±1.42D (p=0.003) and −2.00±1.48D (p<0.001) at 35° in the temporal retina with +2.00D and +3.00D add lenses, respectively. Differences between +2.00 and +3.00D add lenses were statistically significant beyond 20° in the nasal visual field and 10° in the temporal visual field.
ConclusionIt is possible to induce significant changes in the pattern of relative peripheral refraction in the myopic direction with commercially available dominant design multifocal contact lenses. The higher add (+3.00D) induced an significantly higher effect than the +2.00D add lens, although an increase of 1D in add power does not correspond to the same amount of increase in RPRE.
El objetivo de este estudio fue el de mostrar el potencial de inducción de desenfoque miópico en la retina periférica en ojos con miopia, por medio de una lente de contacto blanda multifocal de visión central-lejana, comercialmente disponible.
MétodosSe evaluaron veintiocho ojos derechos miopes pertenecientes a 28 pacientes (edad media: 22,0±2,0 años). Las mediciones de la refracción axial y fuera del eje se realizaron utilizando un autorrefractómetro de campo abierto Grand-Seiko WAM-5500 sin lentes, y con lentes de contacto multifocales (Diseño Proclear Multifocal D®) de adición de potencia de +2,00D y +3,00D, aplicadas de manera aleatoria. La refracción equivalente esférica media y central fue de -2,24±1,33D. La refracción ocular se midió en el centro, y a excentricidades comprendidas entre 35° nasales y 35° temporales (en pasos de 5°).
ResultadosEl error refractivo periférico relativo basal (RPRE), como equivalente esférico (M), fue de -0,69±1,14D y -0,46±1,38D a 35° en las regiones nasal y temporal del campo visual, respectivamente. Ambas adiciones de potencias incrementaron el desenfoque miópico periférico relativo hasta -0,82±1,23D (p=0,002) y -1,42±1,45D (p<0,001) a 35° en el campo nasal, y -0,87±1,42D (p=0,003) y -2,00±1,48D (p<0,001) a 35° en el campo retiniano temporal con lentes de adición de +2,00D y +3,00D, respectivamente. Las diferencias entre las lentes de adición de +2,00 y +3,00D fueron estadísticamente significativas para excentricidades superiores a 20° en el campo visual nasal, y superiores a 10° en el campo visual temporal.
ConclusiónEs posible inducir cambios miópicos significativos en el patrón de la refracción periférica relativa en la con las lentes de contacto multifocales de diseño dominante, comercialmente disponibles. La adición mayor (+3,00D) indujo un efecto significativamente mayor que las lentes de adición de +2,00D, aunque el incremento de 1D en la adición de potencia no se corresponde con la misma cantidad de incremento en términos de cambio en el error refractivo periférico relativo.
Retinal shape is one of several factors that may be related with myopia progression with many studies showing that the myopic eye has on average a more prolate retinal shape in comparison with emmetropic eyes.1–3 This probably reflects the result of stretching induced by posterior ocular elongation as modern techniques of magnetic resonance imaging and low coherence biometry have shown.4,5 Atchison et al.6 observed that the peripheral refraction was relatively more hyperopic in myopic eyes than in emmetropic eyes along the horizontal visual field. Smith's studies have shown that peripheral retina alone is capable to regulate the emmetropization process,7–9 and not the fovea as previously thought, thereby showing the relevance of peripheral retina in ocular development.
Conventional correction of myopia with spectacle lenses may result in an increase of peripheral relative hyperopic defocus10,11 which worsens with higher degree of myopia and with increase of eccentricity.12 By changing the peripheral optics of corrective devices it is now possible to invert the relative hyperopic defocus in myopic eyes into peripheral relative myopia.11 This is considered one possible strategy to counterbalance the unknown stimulus that triggers the eye elongation and the subsequent myopia progression.
There are several options to change the relative peripheral refractive error (RPRE) pattern, for example corneal refractive therapy (CRT)13–15 or laser in situ keratomileusis (LASIK) surgery.16 Special designs of spectacle lenses,17 and contact lenses18 are also produced with the aim of increasing the peripheral relative myopic defocus and to slow-down myopia progression. Some commercially available multifocal contact lenses (MFCL) (dominant-design) might afford a similar effect by means of a peripheral add power area primarily intended to increase spherical aberration and depth of focus in presbyopic patients. Dominant design multifocal contact lenses have been previously demonstrated to induce significant changes to the peripheral refractive error profile of the eye. Lopes-Ferreira et al. using an open-field auto-refractor found a more effective peripheral myopization with a +3.00D add dominant design Proclear Multifocal lens in a setting of 20 emmetropic eyes.19 More recently, Rosén et al. using an experimental Hartman-Shack sensor showed that the same lens was able to induce about 0.50D of relative peripheral myopia at 30° using a +2.00D lens in 3 emmetropic and 1 myopic patients.20 However, the potential effect of these lenses on myopic eyes that could be potentially treated with these lenses, is not well described in a larger sample size. The goal of this study was to use commercially available center-distance multifocal soft contact lenses (Proclear® Multifocal dominant design) to evaluate their impact in the peripheral optics of the myopic eye.
MethodsIn this study, we measured 28 eyes of 28 myopic patients (24 females and 4 males) aged 19–26 years (mean age: 22.0±2.0 years) with central spherical equivalent refraction (MSE±SD) of −2.24±1.33D. The experiments were conducted at the Clinical and Experimental Optometry Research Lab (CEORLab, University of Minho, Braga, Portugal). All volunteers were fully informed of the purpose and all the procedures of this study, and they gave written consent following the tenets of the Declaration of Helsinki.
The refractive error of the patients was assessed through a complete optometric examination, including non-cycloplegic objective and subjective refraction. Central and peripheral refraction without any correction (baseline) was measured using an open-view autorrefractometer/keratometer Grand-Seiko WAM-5500 (Grand Seiko Co., Ltd., Hiroshima, Japan).21,22 Subjects are instructed to fixate a target located at 2.5m consisting of a row of LEDs arranged horizontally. Measurements were made in straight-ahead viewing (in fovea) and in the positions corresponding to eccentricities between 35° nasal and 35° temporal, in 5° steps. The patient rotated the eye to fixate different LED targets,23,24 while the fellow eye was occluded. This technique has been used also to evaluate the effect of single vision soft contact lenses on peripheral refraction.25
Inclusion criteria required that patients had myopia lower than −6.00D, astigmatism lower than −1.00D and should be free of any current eye disease or injury, did not undergo refractive surgery and not being under effect of any ocular or systemic medication.
Proclear® Multifocal with Dominant design (Coopervision, Pleasanton, CA, USA) were fitted only to the right eye of all patients. The lens comprises a central spherical 2.3mm area targeted to compensate the refractive error of each patient, surrounded by an annular aspheric zone of increasing power reaching the maximum add power at 5mm chord area. Second spherical zone with the maximum near add covers the area from the 5 to 8mm chord (either +2.00 or +3.00D of add has been used in this study). Further technical details of the lens are presented in Table 1. Lenses with the two add powers were fitted in random order and in independent sessions, in different days. Lens fit was checked for lateral centration on primary gaze and lag on lateral gaze as this are the main factors that will potentially affect our measures. Only patients with less than 0.5mm of lateral decentration on primary gaze and less than 0.25mm of lag compared to primary gaze position at the maximum eye rotation (35°) to ensure minimal effect of lens lag upon eye rotation on the measures of peripheral refraction. We used a caliper attached to the ocular of the slit lamp to be able the measure this small effects of lag (0.1mm resolution). The illumination on examination room was adjusted to obtain sufficiently large pupil size to allow peripheral measurements without artificial pupil dilatation, which was achieved in all cases. Five measures of refraction (sphere, cylinder and axis) were obtained at each central or eccentric location. Individual data were converted to vector components of refraction as recommended by Thibos26: M, J0 and J45 according to Fourier analysis,
where Sph, Cyl and α represent sphere, cylinder and axis, respectively. Data were stored automatically in Microsoft Excel spreadsheet using custom software (DRRE, CEORLab, Portugal) and treated statistically using SPSS v.19 for Windows (SPSS Inc., IL, USA). Kolmogorov–Smirnov Test was applied in order to evaluate the normality of data distribution. When normality could not be assumed, Wilcoxon Signed Ranks Test was used for paired comparison between baseline and lens adds power and Paired Samples T-Test was used when normality could be assumed. For statistical purposes, a p value lower than 0.05 was considered statistically significant.Technical details of Proclear Multifocal Contact Lens.
| Parameter | Value |
| Material | Omafilcon A |
| Equilibrium water content | 62% |
| Base curve radius | 8.6mm |
| Overall diameter | 14.2mm |
| Distance power | Distant correction of each patient |
| Near add power | +2.00D and +3.00D |
| Spherical distance zone diameter | 2.3mm |
| Aspheric multifocal zone width/diameter | 1.35mm/5.0mm |
| Spherical near zone width/diameter | 1.75mm/8.5mm |
Table 2 presents the mean values of refractive error and standard deviations of all eyes without lens (WL), and wearing each one of two tested multifocal soft contact lens Proclear® multifocal D (dominant design) of near addition +2.00D (Add2) and +3.00D (Add3).
Mean spherical equivalent values (MSE±SD), horizontal astigmatism component (J0±SD) and oblique astigmatism component (J45±SD) for the whole sample (n=28 eyes) at different eccentricities under different conditions: without lens, MFCL addition +2.00D (Add2) and MFCL addition +3.00D (Add3). Values are expressed in diopters (D). N: nasal visual field; T: temporal visual field; C: center.
| Eccentricity | M | J0 | J45 | ||||||
| WL | Add2 | Add3 | WL | Add2 | Add3 | WL | Add2 | Add3 | |
| N35 | −2.93±1.68 | −1.92±1.32 | −2.92±1.62 | −1.04±0.46 | −0.99±0.34 | −1.21±0.60 | −0.08±0.32 | −0.12±0.38 | −0.20±0.40 |
| N30 | −2.73±1.63 | −1.71±1.22 | −2.90±1.25 | −0.71±0.29 | −0.72±0.35 | −1.09±0.48 | −0.04±0.26 | −0.01±0.32 | −0.16±0.48 |
| N25 | −2.68±1.43 | −1.49±0.84 | −2.23±1.02 | −0.46±0.21 | −0.47±0.40 | −0.71±0.49 | 0.00±0.23 | 0.03±0.30 | −0.02±0.46 |
| N20 | −2.58±1.46 | −1.25±0.81 | −1.70±0.84 | −0.23±0.30 | −0.21±0.40 | −0.36±0.45 | −0.05±0.31 | 0.02±0.29 | 0.03±0.38 |
| N15 | −2.64±1.46 | −1.25±0.59 | −1.50±0.86 | −0.31±0.42 | −0.08±0.45 | −0.14±0.60 | 0.01±0.26 | −0.03±0.42 | 0.14±0.46 |
| N10 | −2.51±1.33 | −1.10±0.52 | −1.35±0.74 | −0.07±0.22 | 0.10±0.26 | 0.04±0.46 | −0.03±0.24 | −0.01±0.32 | 0.11±0.44 |
| N5 | −2.39±1.38 | −0.88±0.47 | −1.15±0.68 | 0.03±0.22 | 0.07±0.26 | 0.09±0.26 | 0.02±0.17 | −0.01±0.27 | 0.07±0.32 |
| C | −2.24±1.33 | −1.10±0.53 | −1.50±0.62 | 0.03±0.20 | −0.05±0.33 | −0.09±0.35 | 0.00±0.14 | −0.01±0.34 | 0.01±0.43 |
| T5 | −2.26±1.42 | −1.15±0.71 | −1.71±0.76 | −0.08±0.16 | −0.14±0.34 | −0.29±0.30 | 0.02±0.15 | −0.04±0.35 | 0.03±0.50 |
| T10 | −2.39±1.49 | −1.41±0.75 | −2.22±0.69 | −0.14±0.22 | −0.34±0.30 | −0.59±0.29 | 0.00±0.16 | 0.00±0.41 | 0.02±0.49 |
| T15 | −2.53±1.50 | −1.61±0.67 | −2.81±0.76 | −0.34±0.23 | −0.48±0.31 | −0.88±0.33 | 0.00±0.16 | −0.07±0.35 | −0.08±0.56 |
| T20 | −2.62±1.58 | −1.93±0.92 | −3.28±0.73 | −0.56±0.24 | −0.78±0.34 | −1.19±0.27 | −0.02±0.19 | −0.08±0.34 | −0.07±0.57 |
| T25 | −2.66±1.66 | −2.05±1.12 | −3.48±0.76 | −0.79±0.31 | −1.07±0.35 | −1.50±0.31 | −0.04±0.18 | −0.12±0.27 | −0.13±0.40 |
| T30 | −2.64±1.82 | −2.05±1.30 | −3.62±1.01 | −1.11±0.40 | −1.35±0.40 | −1.71±0.42 | −0.09±0.26 | −0.09±0.29 | −0.20±0.30 |
| T35 | −2.70±2.08 | −1.97±1.52 | −3.51±1.12 | −1.50±0.50 | −1.68±0.52 | −2.07±0.53 | −0.11±0.27 | −0.17±0.33 | −0.16±0.33 |
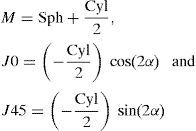
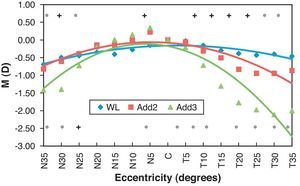
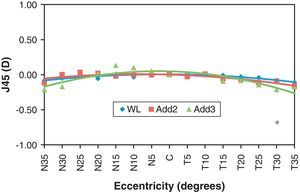
Figs. 1–3 represent the RPRE expressed as M, J0 and J45, respectively, in each case were represented values that corresponds to the situation without lenses and with each one of the contact lenses used in the study. According to Fig. 1, Add2 multifocal lens shows statistically significant differences in the peripheral visual field from N25 and from T10 compared to baseline. Add3 multifocal lens can induce significant myopization effect from N25 and T5 toward the more peripheral locations. Fig. 2 shows that differences against baseline in J0 significantly increase with eccentricity of the visual field and the changes are also higher for Add3 multifocal lens. In Fig. 3, it is shown that J45 values do not change significantly, along the horizontal visual field, with any of the lenses used.
Relative peripheral refractive error (eccentricity minus center) in mean spherical equivalent values (M) as a function of angle in temporal field (T) and nasal field (N), across 70° of horizontal visual field. One polynomial function of 2nd degree was adapted for each experimental situation and refractive components analyzed: for without lens condition (WL – ♦): y=−0.009x2+0.156x−0.826; with multifocal contact lens add +2.00D (Add2 – ¿): y=−0.018x2+0.259x−0.976 and with MFCL addition +3.00D (Add3 – ▴): y=−0.038x2+0.516x−1.850. *Wilcoxon Signed Ranks Test and +Paired Sample T-Test. Only those location with statistically significant differences (p<0.05) compared to center are illustrated (top symbols for Add2 and bottom symbols for Add3).
Relative peripheral refractive error (eccentricity minus center) in horizontal astigmatism component values (J0) as a function of field angle the temporal (T) and nasal (N) retinal area, across central 70° of horizontal visual field. One polynomial function of 2nd degree was adapted for each experimental situation and refractive components analyzed: for without lens condition (WL – ♦): y=−0.025x2+0.373x−1.406; with multifocal contact lens add +2.00D (Add2 – ¿, continuous line): y=−0.027x2+0.379x−1.270 and with MFCL addition +3.00D (Add3 – ▴): y=−0.032x2+0.448x−1.577. *Wilcoxon Signed Ranks Test and +Paired Sample T-Test. Only those location with statistically significant differences (p<0.05) compared to center are illustrated (top symbols for Add2 and bottom symbols for Add3).
Relative peripheral refractive error (eccentricity minus center) in oblique astigmatism component values (J45) as a function of field angle the temporal (T) and nasal (N) retinal area, across 70° of horizontal visual field. One polynomial function of 2nd degree was adapted for each experimental situation and refractive components analyzed: for without lens condition (WL – ♦): y=−0.002x2+0.030x−0.111; with multifocal contact lens add +2.00D (Add2 – ¿): y=−0.002x2+0.027x−0.079 and with MFCL addition +3.00D (Add3 – ▴): y=−0.005x2+0.080x−0.245. *Wilcoxon Signed Ranks Test and +Paired Sample T-Test. Only those location with statistically significant differences (p<0.05) compared to center are illustrated (top symbols for Add2 and bottom symbols for Add3).
The numerical values of differences between refractive components at each eccentricity and center are shown in Table 3 for values of M, J0 and J45 along with all the statistical comparisons against baseline and between both contact lenses used. It is evident that the differences between extreme peripheral points (35°) either nasal or temporal and the center became significant with Add2 multifocal contact lens reaching values of RPRE for M component of −0.82±1.23D and −0.87±1.42D; these differences are greater with Add3 reaching −1.42±1.45D and −2.00±1.48D in the nasal and temporal visual fields, respectively. Differences against baseline for each Add power were statistically significant beyond 25° N and 10° T, with Add2 and out of 25° N and 5° T in case of Add3. Differences between Add2 and Add3 were statistically significant beyond eccentricities of 25° in the nasal visual field and beyond 10° in the temporal visual field (p<0.05).
Relative peripheral refractive error (eccentric points minus center) as spherical equivalent values (M±SD), horizontal astigmatism component (J0±SD) and oblique astigmatism component (J45±SD) for the situation without lens, with MFCL addition +2.00D (Add2) and with MFCL addition 3.00D (Add3). Values are expressed in diopters (D). N: nasal side of retina; T: temporal side of retina; C: center. p represents the value of statistical significance according to: +Paired Sample T-Test or *Wilcoxon Signed Ranks Test. Bold indicates statistically significant power difference compared with central point (95% confidence).
| Point | M | J0 | ||||||
| WL±SD | Add2±SD | Add3±SD | Diff. Add2 vs Add3 | WL±SD | Add2±SD | Add3±SD | Diff. Add2 vs Add3 | |
| Sig. (p) | Sig. (p) | Sig. (p) | Sig. (p) | Sig. (p) | Sig. (p) | Sig. (p) | Sig. (p) | |
| N35 | −0.69±1.14 | −0.82±1.23 | −1.42±1.45 | 0.60±1.16 | −1.07±0.51 | −0.94±0.38 | −1.12±0.55 | 0.19±0.65 |
| 0.001* | 0.002* | <0.001* | 0.011* | <0.001* | <0.001* | <0.001* | 0.127+ | |
| N30 | −0.50±0.98 | −0.61±1.14 | −1.40±1.23 | 0.79±0.73 | −0.74±0.30 | −0.67±0.38 | −1.00±0.37 | 0.33±0.46 |
| 0.008* | 0.009+ | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | |
| N25 | −0.45±0.80 | −0.39±0.83 | −0.73±1.01 | 0.34±0.69 | −0.49±0.23 | −0.42±0.40 | −0.62±0.39 | 0.20±0.43 |
| 0.002* | 0.032* | 0.001+ | 0.016* | <0.001* | <0.001* | <0.001* | 0.022* | |
| N20 | −0.35±0.69 | −0.14±0.80 | −0.20±0.90 | 0.06±0.85 | −0.26±0.30 | −0.16±0.43 | −0.27±0.42 | 0.12±0.43 |
| 0.007* | 0.348* | 0.249+ | 0.801+ | <0.001* | 0.139* | 0.003* | 0.194+ | |
| N15 | −0.40±0.57 | −0.15±0.65 | 0.01±0.87 | −0.15±0.88 | −0.34±0.40 | −0.03±0.50 | −0.06±0.43 | 0.03±0.44 |
| 0.001* | 0.288* | 0.966+ | 0.368* | <0.001* | 0.692* | 0.657* | 0.561+ | |
| N10 | −0.27±0.47 | 0.00±0.49 | 0.15±0.77 | −0.15±0.70 | −0.10±0.25 | 0.15±0.31 | 0.13±0.38 | 0.02±0.45 |
| 0.007* | 0.914* | 0.291* | 0.418+ | 0.047* | 0.021* | 0.072* | 1.000+ | |
| N5 | −0.15±0.20 | 0.22±0.42 | 0.35±0.45 | −0.13±0.61 | 0.00±0.16 | 0.12±0.26 | 0.18±0.33 | −0.05±0.37 |
| <0.001+ | 0.009+ | 0.001* | 0.605+ | 0.732* | 0.023* | 0.013* | 0.657+ | |
| T5 | −0.03±0.28 | −0.05±0.42 | −0.21±0.47 | 0.15±0.66 | −0.11±0.15 | −0.09±0.25 | −0.20±0.22 | 0.11±0.34 |
| 0.586+ | 0.515+ | 0.029* | 0.285+ | 0.002* | 0.060* | <0.001* | 0.07 | |
| T10 | −0.15±0.40 | −0.31±0.40 | −0.72±0.56 | 0.41±0.62 | −0.17±0.17 | −0.29±0.22 | −0.50±0.29 | 0.21±0.33 |
| 0.054+ | <0.001+ | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | |
| T15 | −0.30±0.51 | −0.51±0.47 | −1.31±0.71 | 0.80±0.66 | −0.37±0.18 | −0.43±0.32 | −0.79±0.30 | 0.36±0.34 |
| 0.004+ | <0.001+ | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | |
| T20 | −0.38±0.63 | −0.83±0.72 | −1.78±0.79 | 0.94±0.68 | −0.59±0.23 | −0.73±0.30 | −1.10±0.32 | 0.37±0.37 |
| 0.003+ | <0.001+ | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | |
| T25 | −0.43±0.86 | −0.95±0.94 | −1.98±0.94 | 1.03±0.71 | −0.82±0.29 | −1.02±0.33 | −1.41±0.29 | 0.39±0.27 |
| 0.013+ | <0.001+ | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | |
| T30 | −0.40±1.13 | −0.94±1.09 | −2.11±1.27 | 1.17±0.93 | −1.13±0.42 | −1.30±0.41 | −1.63±0.43 | 0.33±0.57 |
| 0.071+ | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | |
| T35 | −0.46±1.38 | −0.87±1.42 | −2.00±1.48 | 1.13±1.00 | −1.53±0.51 | −1.63±0.59 | −1.99±0.52 | 0.36±0.61 |
| 0.088+ | 0.003* | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | 0.01* | |
| Point | J45 | |||
| WL±SD | Add2±SD | Add3±SD | Diff. Add2 vs Add3 | |
| Sig. (p) | Sig. (p) | Sig. (p) | Sig. (p) | |
| N35 | −0.09±0.31 | −0.12±0.52 | −0.21±0.73 | 0.10±0.63 |
| 0.019+ | 0.386+ | 0.274+ | 0.187* | |
| N30 | −0.05±0.25 | 0.00±0.54 | −0.17±0.83 | 0.17±0.75 |
| 0.015+ | 0.406+ | 0.227+ | 0.219* | |
| N25 | −0.01±0.24 | 0.03±0.49 | −0.03±0.81 | 0.06±0.59 |
| 0.085+ | 0.084+ | 0.873+ | 0.946* | |
| N20 | −0.05±0.24 | 0.02±0.49 | 0.02±0.70 | 0.00±0.61 |
| 0.071+ | 0.283+ | 0.692+ | 0.964* | |
| N15 | 0.01±0.25 | −0.02±0.50 | 0.13±0.73 | −0.15±0.65 |
| 0.239+ | 0.685+ | 0.298+ | 0.227* | |
| N10 | −0.03±0.23 | 0.00±0.25 | 0.10±0.43 | −0.10±0.50 |
| 0.218+ | 0.214+ | 0.181+ | 0.419* | |
| N5 | 0.01±0.20 | 0.00±0.26 | 0.05±0.34 | −0.06±0.44 |
| 0.678+ | 0.479+ | 0.091+ | 0.855* | |
| T5 | 0.01±0.12 | −0.03±0.22 | 0.02±0.28 | −0.04±0.35 |
| 0.653+ | 0.812+ | 0.672+ | 0.399* | |
| T10 | 0.00±0.11 | 0.01±0.25 | 0.00±0.33 | 0.01±0.41 |
| 0.484* | 0.097+ | 0.918* | 0.585* | |
| T15 | −0.01±0.14 | −0.06±0.23 | −0.09±0.33 | 0.04±0.39 |
| 0.699+ | 0.768+ | 0.144+ | 0.393* | |
| T20 | −0.03±0.15 | −0.07±0.24 | −0.08±0.48 | 0.02±0.46 |
| 0.500+ | 0.649+ | 0.306+ | 0.682* | |
| T25 | −0.04±0.19 | −0.11±0.30 | −0.15±0.39 | 0.03±0.41 |
| 0.290* | 0.574+ | 0.091* | 0.350* | |
| T30 | −0.09±0.24 | −0.09±0.30 | −0.21±0.39 | 0.13±0.32 |
| 0.110+ | 0.850* | 0.037* | 0.031* | |
| T35 | −0.11±0.28 | −0.16±0.35 | −0.17±0.52 | 0.01±0.40 |
| 0.075* | 0.251+ | 0.253* | 0.495* | |
In this study it was evaluated the relative peripheral refractive error (RPRE) along the horizontal field between 35° nasal and 35° temporal, with dominant design MFCL of two near add powers (+2.00 and +3.00D) in myopic eyes.
In a previous study we demonstrated that these multifocal design can induce significant peripheral myopic shift in emmetropic patients.19 As expected, with increasing of add power (from +1.00 to +4.00D) the myopization effect also increased in the peripheral visual field. However, there was not a linear relationship between the relative peripheral myopia induced and the add power such that there was no significant gain in fitting +1.00 lenses when compared with plano lenses made of the same material. There was also no significant improvement in the relative peripheral myopia induced by the +4.00 lens compared to the +3.00 lens. When it comes to choose a fitting add for myopes with the purpose of inducing significant peripheral myopia it is necessary to bear in mind this preliminary information. According to our previous results, a minimum add of +2.00 is necessary to induce significant effects in terms of peripheral myopization, while the +4.00D add MFCL would not seem to add significant advantages. Higher near add powers increase significantly the effect of visual distortion due to the expected increase in positive spherical aberration.
From the present study, it seems that the results obtained in emmetropes are reproducible in myopic patients. Furthermore, there is a significant increase in the peripheral myopization effect with the +3.00 Add compared to the +2.00 Add of 1.00D and 1.54D in nasal and temporal more eccentric points, respectively (Table 2). These findings, eventually will allow customizing the treatment to each particular eye considering its baseline peripheral refractive pattern and the desired level of change, to more conveniently interfere with the mechanism of refractive error development.
Since the refractive error was corrected by the lenses, we should expect to obtain central measurements near plano and the refractive change symmetrically distributed to both sides of the central line of sight. However, we obtain an average refractive error along the central line of sight of −1.10 with the Add2 MFCL and −1.40 with the Add3 MFCL. In this study we have controlled the effect of centration and lag effect on lateral gaze. However, the infrared light that measures refractive status of eye in the open-view autorefractor used27 is about 2.3mm in diameter and therefore may have influenced the amount of refractive power. With a center distance area of the same size, small misalignment of the lens (<0.5mm) will make the autorefractor to read a small part of the addition power, thus increasing the myopic value given for the central point. Although this might be considered a methodological limitation, in this particular study we are interested in analyzing the refractive profile across the center and the periphery and then derive the RPRE change induced by the lenses. By using the same procedure (area sampled) to measure all points the aperture-dependant issue is balanced between all the measured points. Thus, we are confident that the profiles we obtain are still valid and representative of the “relative” refractive change along the 70° visual field in the horizontal direction. The small decentration effect might be also reflected on the slight asymmetry of 0.5D between the nasal and temporal visual field RPRE for the Add3 lens.
The amount of RPRE change induced by each lens does not match the value of the add power placed by the manufacturer in the peripheral area of the optic zone. In this sample the change in RPRE was −0.87D for the Add2 lens and −2.00D for the Add3 lens. This is in agreement with our previous work in emmetropic eyes19 and with the measures of Rosén et al. who found a RPRE change of −0.50D at 30° using a different measuring technique.20 Two reasons might explain this effect. The peripheral add power is formed by an aspheric zone. Thus, the maximum add might be beyond the 35° we measure in this study. Second, the actual power of the surface might change slightly when the hydrophilic lens is coupled with the corneal surface so that part of the power might be masked. In our previous study, the lens Add3 was preferred because it produced a greater effect of significant relative peripheral myopization in a wider range of peripheral eccentricities like in our previous clinical trial.19 If MFCL design described in this trial eventually will apply for therapeutic purposes, there will be a necessity to expand central optical distance zone of the MFCL as a means of improving peripheral effect and quality of vision, once MFCL with high add and center distance design, as MFCL used, decreases the peripheral image quality at optimal defocus.20
In the present study we did not measure the peripheral refraction with plano contact lenses (non-multifocal design). However, considering the lack of significant changes in peripheral refractive profile observed with the +1.00 Add lens in our previous work with these lenses,19 we did not expect to obtain a significantly different result between baseline and spherical plano lens in this population either. Kang et al.25 found recently a significant difference between baseline and full correction of the refractive error with Proclear single vision contact lenses. They found a trend to measure higher hyperopic values at 20°, 30° and 40° of eccentricity with full correction in single vision contact lenses than at baseline. Although we do not have a control measure with plano lenses, the possibility of finding slightly higher hyperopic trends with single vision lenses will make our results to become even more relevant when it comes to the quantification of the peripheral myopization effect of the Add2 and Add3 lenses.
Other authors already conducted longitudinal studies evaluating axial growth and myopia progression in Chinese,28 Japanese29 and in American30 children wearing orthokeratology lenses during 24 month. It is believed that the effect of retention of myopia progression is related with the peripheral myopization induced by orthokeratology.13,14 Despite the benefits of orthokeratology, the effect of peripheral myopization is so far limited to the amount of central myopia to be compensated14 and also affect significantly the quality of vision due to increased aberrations.31 More recently some authors17 tried to produce peripheral myopization with newly designed spectacle lenses for myopia, the best lens from the three that were tested was optimized to achieve reduced astigmatism in the horizontal meridian while attaining a positive additional peripheral power of 1.9D at 25mm from the axis in that meridian. However, their results suggest that this approach was not able to reduce the rate of myopia progression, because in comparison with control group after 12 months, the lens showed a small and no statistical significant reduction of axial elongation. Spectacle lenses mounted in frames at a certain vertex distance do not warrant are not likely to induce the therapeutic effect afforded by contact lenses. Compared to spectacle lenses, contact lenses have the advantage of following the eye in its vergence movements, thus allowing that the optical effect pretended with these optic solutions will be continuously centered with the optical system of the eye. Recently, Shen et al.32 have observed that even non-multifocal, non-customized rigid gas permeable lenses might have a significant effect to induce relative peripheral myopic blur. However, this effect might be insufficient to play a significant role in retarding myopia progression as a clinical study conducted by Walline et al.33 came to show in 2004.
Within the contact lens field, custom-made contact lenses have also been developed to change purposely the relative peripheral refractive error patterns. Some lenses are intended to create a similar refractive effect to that induced in the dominant design multifocal contact lenses34 evaluated here. Indeed, the optical performance of other designs in terms of relative peripheral refractive error changes have already been tested, demonstrating a significant effect to create relative peripheral myopization.35 Peripheral gradient lenses34 have shown to be effective in decrease myopia progression in myopic children.18 Soft contact lenses visual correction was associated with more clarity of vision than orthokeratology,36 what could be an additional benefit. However, it is expected that these multifocal lenses with small center distance apertures, induce significant visual distortions.
In summary, it is possible to modify the pattern of peripheral refraction in the periphery with the wear of Dominant Design Multifocal Contact Lenses, preferably with +3.00D add power that has demonstrated to be more effective to produce the peripheral myopization effect.
Conflicts of interestThe authors have no conflicts of interest to declare.
We acknowledge the assistance of Dr. Raquel Maia with the experimental setup. This work was supported by FEDER through the COMPETE Program and by the Portuguese Foundation for Science and Technology (FCT) in the framework of the Strategic Project PTDC/SAU-BEB/098392/2008.