The purpose of this study was to characterize the central and peripheral refraction across the horizontal meridian of the visual field without and with a multifocal dominant design soft contact lens of different add powers (+1.00 D to +4.00 D) in emmetropic eyes.
MethodsTwenty right eyes from 20 emmetropic patients (mean spherical equivalent central refraction –0.06±0.54 D) with a mean age of 21.6±2.3 years were fitted with Proclear Multifocal dominant design (Coopervision, Pleasanton, CA, USA). Lenses had add powers from +1.00 to +4.00 D in 1.00 D steps. The central and peripheral refraction was measured along the horizontal meridian up to 35° of eccentricity in the nasal and temporal retinal area in 5° steps using a open-field autorefractometer.
ResultsOnly the +3.00 and +4.00 D add powers generated a significant change in the peripheral refractive pattern compared to central refraction and compared with the no-lens wearing situation. The average myopic increase with these lenses was –3.00 D and –5.00 (p<0.001) at the margins of inspected nasal and temporal visual field, respectively.
ConclusionsMultifocal dominant design soft contact lenses are able to change the peripheral refractive profile in emmetropic eyes increasing relative peripheral myopia. Lenses with +3.00 D add power seem to be the best option to create such effect due to significant peripheral myopization.
El objetivo de este estudio fue caracterizar la refracción central y periférica a través del meridiano horizontal del campo visual con y sin lente de contacto blanda multifocal de diseño dominante de diferentes adiciones (+1,00 D a +4,00 D) en ojos emétropes.
MétodosSe colocaron lentes multifocales de diseño dominante Proclear (Coopervision, Pleasanton, Estados Unidos) en 20 ojos derechos de 20 pacientes emétropes (media del equivalente esférico de refracción central, –0,06±0,54 D) con una media de edad de 21,6±2,3 años. Las lentes tenían adiciones desde +1,00 hasta +4,00 D en pasos de 1,00 D. Se evaluó la refracción periférica a través del meridiano horizontal hasta 35° de excentricidad en el campo retiniano nasal y temporal en pasos de 5° utilizando un autorrefractómetro de campo abierto.
ResultadosSolamente las potencias de +3,00 y +4,00 D produjeron un cambio significativo en el patrón de refracción periférica en comparación con la refracción central y en comparación con la evaluación sin lente. El aumento medio de la miopía con estas lentes fue de –3,00 D y –5,00 (p<0,001) en los límites de los campos visuales nasal y temporal explorados, respectivamente.
ConclusionesLas lentes de contacto blandas, multifocales y de diseño dominante tienen la capacidad de cambiar el perfil de refracción periférica en ojos emétropes incrementando la miopía relativa periférica. Aparentemente, las lentes con potencia de+3,00 D serían la mejor opción para generar ese efecto debido a la miopización periférica significativa.
Myopia is a common visual problem affecting millions of people around the world.1,2 It has been shown that genetic3 and environmental factors are potentially involved in determining the refractive state of the eye.4 The increasing prevalence of myopia in Asian and Western1,5,6 populations has increased the interest of researchers to find methods of halting the progression of this condition.
The mechanisms that trigger myopia progression are presently unknown, however animal studies have shown that the quality of the retinal image is an important factor, particularly the peripheral retinal image.7 Hyperopic and emmetropic individuals present an average myopic defocus on the retinal periphery, while myopic individuals are predominantly hyperopic in the periphery of the retina.8 Some studies show that the anatomy of the posterior eyeball surface might contribute to this, being more oblate in emmetropes and hyperopes and less oblate or prolate in myopes. 9–11 Furthermore, there is evidence that correction of myopia with ophthalmic lenses might exacerbate the degree of peripheral hyperopia, 12–15 what could potentially contribute to myopia progression.
Contrary to the situation of myopia correction with spectacles, other forms of vision correction as orthokeratology, are able to keep foveal image focused while the peripheral retina experiences a significant myopic defocus. 16–18 These studies showed that the value of myopia induced in the peripheral retina is similar to the baseline axial spherical equivalent refraction measured. More recently, Shen et al19 have shown that soft contact lenses and rigid gas permeable contact lenses reduce the hyperopic relative peripheral refraction but were not able to invert the pattern towards myopic relative peripheral refraction. The potential of this strategy to slow-down myopia progression has been raised in two separate studies in Hong-Kong by Cho et al20 in the United States of America by Walline et al21 and more recently by Kakita et al in Japan22 although the exact mechanisms of action are still to be understood.
Despite some authors have hypothesized on the potential role of multifocal contact lenses to slow down myopia progression,23,24 there is no information in the peer-review literature on the potential impact of commercially available dominant design multifocal soft contact lenses on peripheral refraction, particularly those creating a peripheral increase in refractive power surrounding a central distance emmetropized area (dominant design). With the present study we attempt to explore this possibility using a commercial multifocal dominant design contact lenses in emmetropic patients.
MethodsSubjects and inclusion criteriaTwenty right eyes of 20 university students (18 women, 2 men) with ages from 18 to 28 years (21.1±2.3 years) were recruited for this study. Sample size was calculated to warrant an 80 % power (β=0.8) to detect differences of at least 0.5 D in the relative myopic peripheral refraction in a paired sample test considering a level of significance of α=0.05. Overall, central spherical equivalent refraction without lenses was –0.06±0.54 D. Mean axial length was 22.81±0.7mm measured with the IOL Master (Zeiss Meditec, CA, USA) instrument.
All the experiments were conducted at the Clinical and Experimental Optometry Research Lab (CEORLab, University of Minho, Braga, Portugal). After explaining the nature of the study, each patient signed a consent form before being enrolled. The research protocol followed the tenets Declaration of Helsinki and was reviewed and approved by the Scientific Committee of the School of Sciences of Minho University (Portugal). The inclusion criteria required that the subjects did not suffer from any current eye disease or injury and were not taking any ocular or systemic medication.
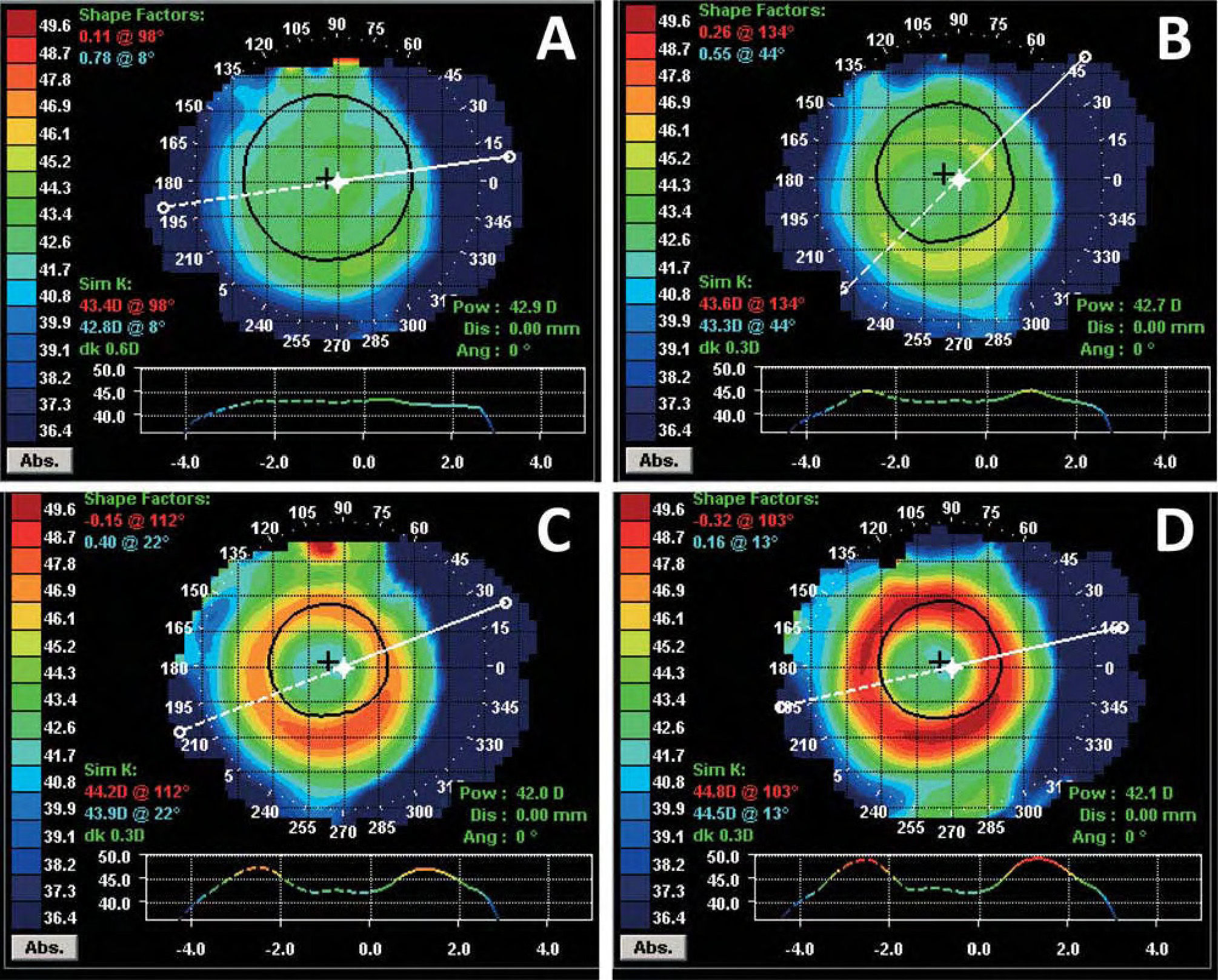
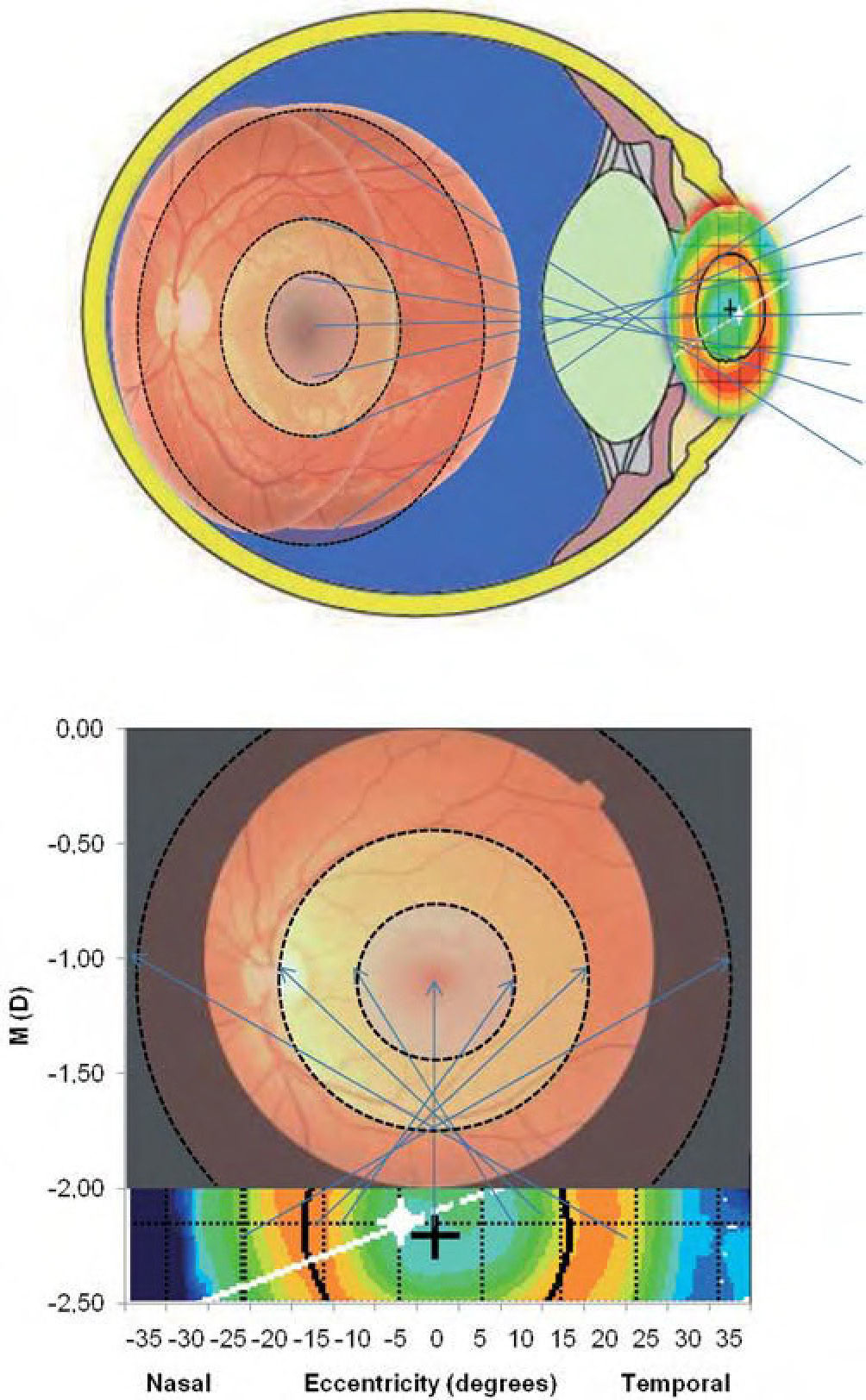
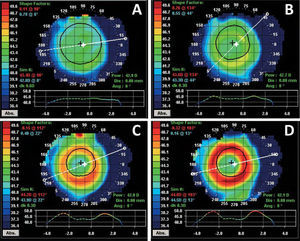
Contact lensesAll the participants were fitted with Proclear Multifocal Dominant (D) design lenses (Coopervision, Pleasanton, CA, USA). Lenses with plano distance power and +1.00, +2.00, +3.00 and +4.00 D add power were fitted in random order to the right eye of each of the patients involved in the experiment. Technical details of the lens are presented in Table 1. Figure 1 shows an example of the four lenses (add +1.00 to +4.00 D) placed on top of a nearly spherical cornea. It is observed how the add ring becomes more evident as the add power increases. Lenses were preserved in multipurpose solution for 24 hours before being trialed in patients.
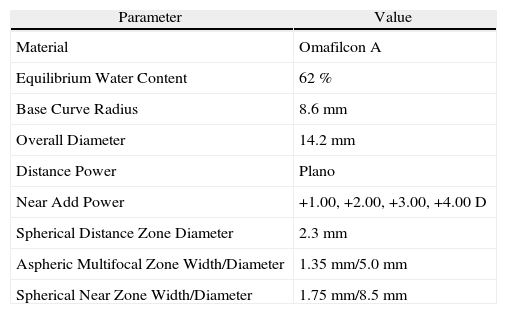
Technical details of the lenses used as reported by the manufacturer
| Parameter | Value |
| Material | Omafilcon A |
| Equilibrium Water Content | 62 % |
| Base Curve Radius | 8.6mm |
| Overall Diameter | 14.2mm |
| Distance Power | Plano |
| Near Add Power | +1.00, +2.00, +3.00, +4.00 D |
| Spherical Distance Zone Diameter | 2.3mm |
| Aspheric Multifocal Zone Width/Diameter | 1.35mm/5.0mm |
| Spherical Near Zone Width/Diameter | 1.75mm/8.5mm |
Tangential topographic maps of curvature measured over the front surface of contact lenses placed on a nearly spherical cornea. Lenses had add powers of +1.00 D (A), +2.00 D (B), +3.00 D (C) and +4.00 D (D). Obtained with Medmont E300 corneal topographer (Medmont, Australia). Values in diopters.
The measurement of central and peripheral (off-axis) refraction was obtained with an open-field Grand Seiko Auto-Refractometer/Keratometer WAM-5500 (Grand Seiko Co., Ltd., Hiroshima, Japan) up to 35° in the nasal and temporal retina along the horizontal visual field in 5° steps. This technology had been previously validated to measure axial refraction25 and the Grand Seiko has been also previously used to measure axial refraction26 and peripheral refraction.27 The system was attached to custom software (Digital Recording of Refractive Error-DRRE, CEORLab, Portugal) to automatically record data from the autorefractometer thus avoiding errors in data collection and allowing data to be automatically processed in Excel spreadsheet for later statistical process using appropriate software. Each eye was measured at baseline without any contact lens, and later with each one of the four lenses, in random order, in two different sessions at the same time of the day. Each measure was averaged from 5 consecutive readings at each point along the field of view under examination.
The illumination of the room was adjusted to obtain a pupil size greater than 4mm required to allow peripheral measurements, which was achieved in all cases. The fixation target was placed at a distance of 2.5 meters from the patient's corneal vertex and consisted of a flat array of 15 light emitting diodes (LEDs) in the horizontal direction: one central, seven to the right and seven to the left side. Although this configuration makes peripheral stimulus to be 50cm farer than central one, thus creating a lower accommodative stimulus by about 0.07 D, this difference is well below the level of clinical and statistical significance considered in these experiments. The LEDs were separated from each other by an angular distance of 5° at the patient's position. The subject was seated with the head stabilized in a chin/forehead rest so that the eye was aligned with the central LED. For the right eye, the fixation of an object positioned on the right side to the primary eye gaze (nasal visual field in the eye primary position) matches the temporal retina measures. The left eye was occluded while patients kept their head stationary and rotated their right eyes to view a series of fixation targets. Five readings were taken and averaged only on the right eye of each individual in all positions considering the center of the pupil as the reference point of measurement.
Descriptive statistics (mean±SD) were obtained for the refraction vector components M=Sph+Cyl/2, J0=–Cyl · cos(2α)/2 and J45=–Cyl · sin(2α)/2 according to Fourier analysis, as recommended by Thibos,28 where Sph, Cyl and α are the manifest sphere, cylinder and axis, respectively.
Statistical analysisThe SPSS software package v.17 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Kolmogorov-Smirnov test was applied in order to evaluate the normality of data distribution. When normality could not be assumed, Wilcoxon signed ranks test was used for paired comparison post and pre treatment and paired samples test was used when normality could be assumed for pair comparisons between treatments. For statistical purposes, a p value lower than 0.05 was considered statistically significant.
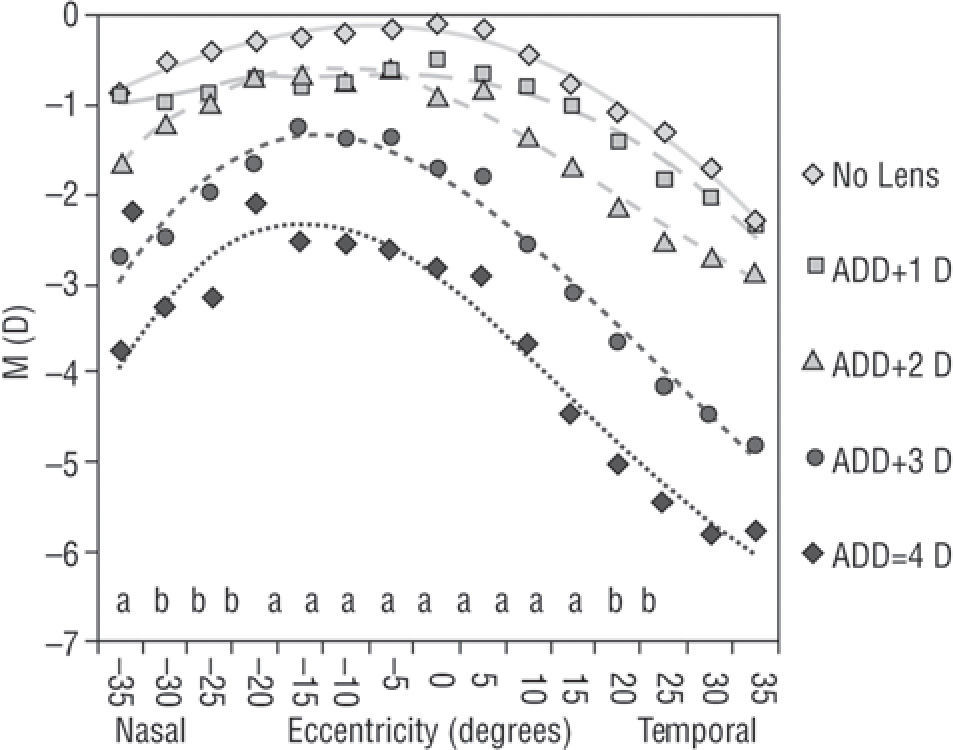
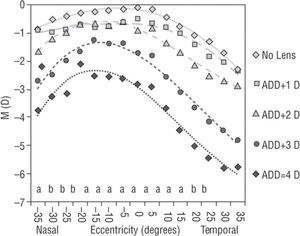
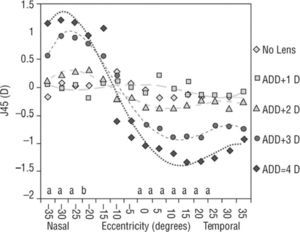
ResultsFigures 2, 3 and 4 show the values of central and peripheral refraction in terms of M, J0 and J45, respectivelly. Values of statistical significance represent the differences between mean values for the five experimental conditions. Tables 2, 3 and 4 represent data on the same refractive components, but now regarding the comparision between central and each peripheral refractive values within each experimental condition (relative peripheral refraction). Figure 2 shows the profiles of central and peripheral spherical equivalent refraction (M) along the 70 degrees of the horizontal visual field (nasal to temporal). Lenses with +1.00 D add power did not generate any statistically significant difference in spherical equivalent refraction compared to baseline values (p>0.05). Lenses with +2.00 D add power changed significantly the spherical equivalent refraction towards more myopic values at all points except for the most peripheral nasal and temporal locations measured. However, this change affected all the points at a similar extent (aproximatelly 0.87 D); this implies that no significant more myopic change occurred in the periphery compared to the central refraction, minimizing the potential effect on peripheral myopization achieved. Converselly, with +3.00 and +4.00 D add powers, a statisticaly significant higher shift towards more myopic values was demonstrated beyond 10° in the temporal field and 20° in the nasal field, thus demonstrating a true peripheral myopization effect. Despite this, there is a remarkable difference between both lenses. While +3.00 D lens essentially displaced the peripheral focalization, maintaining the central refraction closer to emmetropia (all lenses are plano at center 2.5mm), the +4.00 D lens significantly increased the central myopia within the central 35° (10 in the nasal direction and up to 25 in the temporal direction). Significance values for comparisions between central and peripheral locations without and with each lens are provided in Table 2.
Central and peripheral spherical equivalent refraction (M) across the 70 degrees of the horizontal visual field at baseline (no lens) and with the contact lenses with different add power. Equations fitted to data: Baseline (diamonds, continous line): y=5 E - 0 5x4 – 0.0022x3+0.001x2+0.2113x – 1.0081; r2=0.99; Add =+1.00 D (squares, dashed line): y=–0.0012x3+0.0058x2+0.0781x – 1.0714; r2=0.964. Add =+2.00 D (triangles, dashed line): y=0.0022x3 – 0.0834x2+0.7056x – 2.3105; r2=0.982. Add =+3.00 D (circles, dashed line): y=0.0033x3 – 0.1246x2+1.0516x – 3.9025; r2=0.98 and Add =+4.00 D (diamonds, dotted line): y=0.0045x3 – 0.1491x2+1.1617x – 4.9704; r2=0.966. Statistically significant differences between lenses for central (C) and eccentric positions (N and T): aKruskal-Wallis Test; bANOVA (Bonferroni).
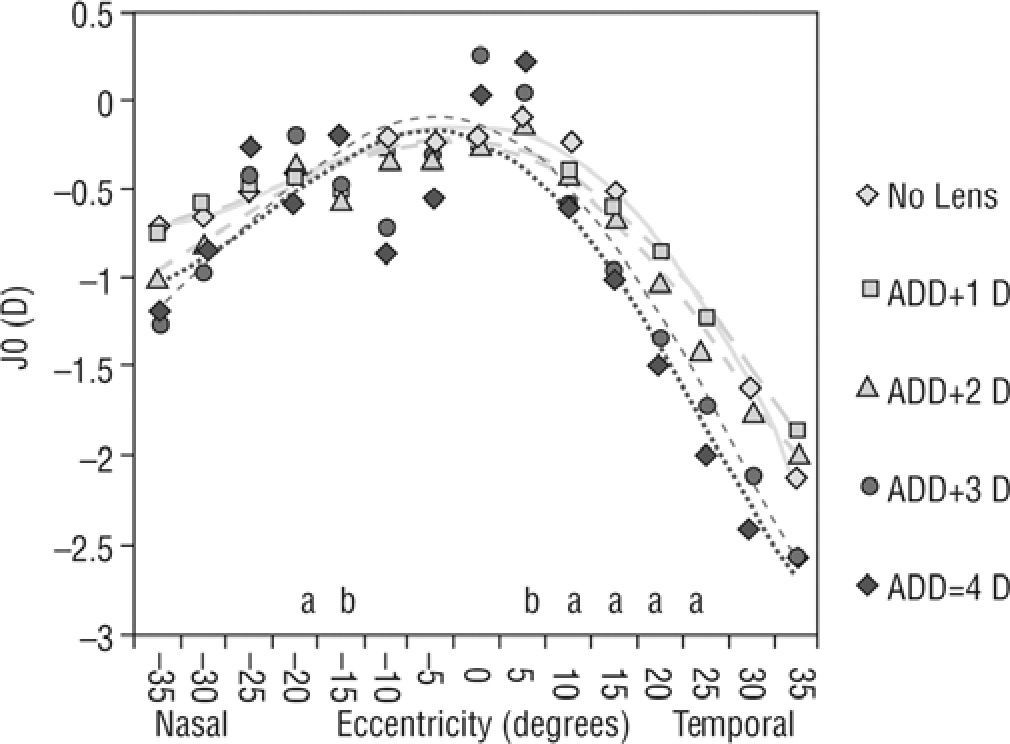
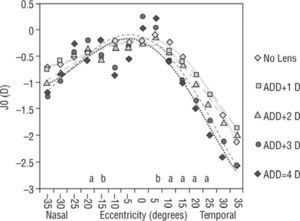
Central and peripheral J0 astigmatic component of refraction across the 70 degrees of the horizontal visual field at baseline (no lens) and with the contact lenses with different add power. Equations fitted to data: Baseline (diamonds, continous line): y=0.0001x4 – 0.0063x 3+0.0643x2 – 0.1243x – 0.6219; r2=0.9886; Add =+1.00 D (squares, dashed line): y=0.0001x4 – 0.0053x3+0.0483x2 – 0.062x – 0.6789; r2=0.9805. Add=+2.00 D (triangles, dashed line): y=0.0001x4 – 0.0052x3+0.0363x2+0.0675x – 1.036; r2=0.9571. Add=+3.00 D (circles, dashed line): y=0.0003x4 – 0.0085x3+0.058x2+0.096x – 1.2977; r2=0.9026 and Add=+4.00 D (diamonds, dotted line): y=0.0004x4 – 0.012x3+0.0964x2 – 0.0901x – 1.017; r2=0.8658. Statistically significant differences between lenses for central (C) and eccentric positions (N and T): aKruskal-Wallis Test; bANOVA (Bonferroni).
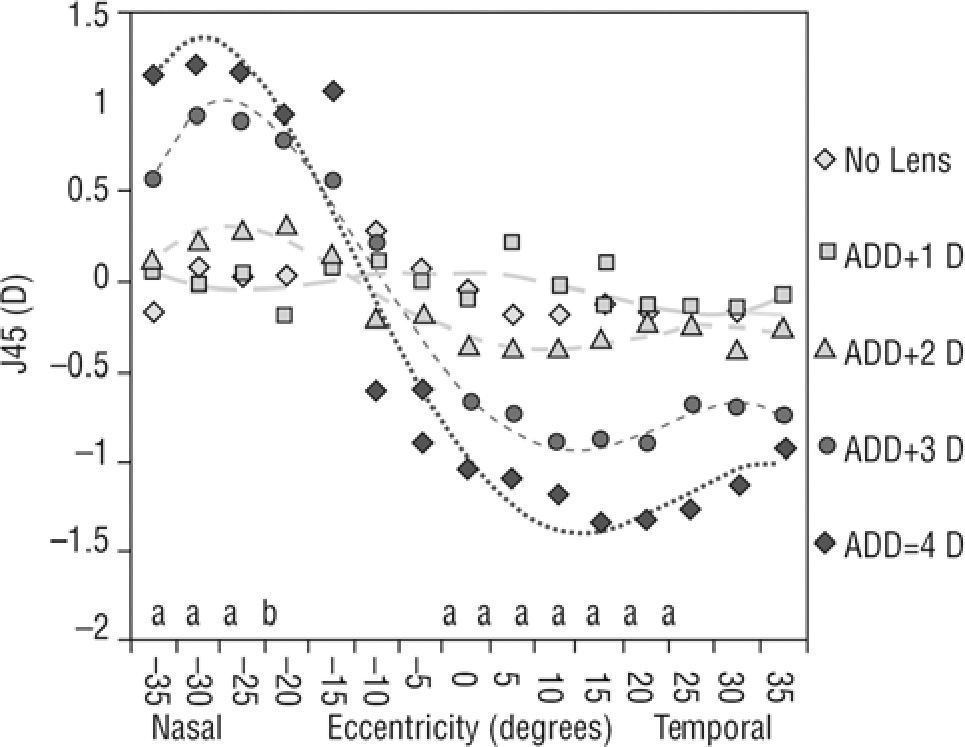
Central and peripheral J45 astigmatic component of refraction across the 70 degrees of the horizontal visual field at baseline (no lens) and with the contact lenses with different add power. Equations fitted to data: Baseline (diamonds, continous line): y=–9E-05x4+0.004x3 – 0.0611x2+0.3289x – 0.4476; r2=0.68; Add=+1.00 D (squares, dashed line): y=0.0002x4 – 0.0069x3+0.0693x2 – 0.2507x+0.2514; r2=0.4201. Add=+2.00 D (triangles, dashed line): y=–0.0004x4+0.0136x3 – 0.1523x2+0.5487x – 0.2984; r2=0.9282. Add=+3.00 D (circles, dashed line): y=–0.0008x4+0.0294x3 – 0.343x2+1.2502x – 0.4041; r2=0.9813 and Add=+4.00 D (diamonds, dotted line): y=–0.0008x4+0.0303x3 – 0.3459x2+1.0922x+0.3223; r2=0.946. Statistically significant differences between lenses for central (C) and eccentric positions (N and T): aKruskal-Wallis Test; bANOVA (Bonferroni).
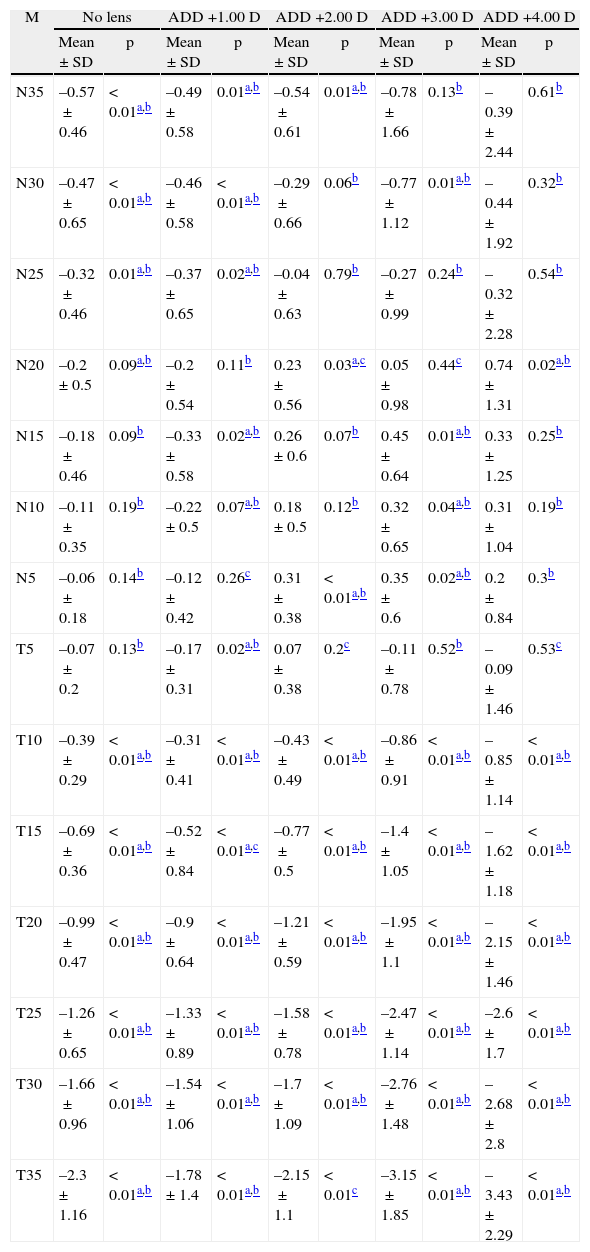
Difference in the values of M component between different eccentric points (Nasal/Temporal) and central value (relative peripheral refractive error) for the five experimental conditions: baseline (No lens), +1.00 D addition (ADD +1.00 D), +2.00 D addition (ADD +2.00 D), +3.00 D addition (ADD +3.00 D) and +4.00 D addition (ADD +4.00 D). Values are expressed in diopters
| M | No lens | ADD +1.00 D | ADD +2.00 D | ADD +3.00 D | ADD +4.00 D | |||||
| Mean±SD | p | Mean±SD | p | Mean±SD | p | Mean±SD | p | Mean±SD | p | |
| N35 | –0.57±0.46 | < 0.01a,b | –0.49±0.58 | 0.01a,b | –0.54±0.61 | 0.01a,b | –0.78±1.66 | 0.13b | –0.39±2.44 | 0.61b |
| N30 | –0.47±0.65 | < 0.01a,b | –0.46±0.58 | < 0.01a,b | –0.29±0.66 | 0.06b | –0.77±1.12 | 0.01a,b | –0.44±1.92 | 0.32b |
| N25 | –0.32±0.46 | 0.01a,b | –0.37±0.65 | 0.02a,b | –0.04±0.63 | 0.79b | –0.27±0.99 | 0.24b | –0.32±2.28 | 0.54b |
| N20 | –0.2±0.5 | 0.09a,b | –0.2±0.54 | 0.11b | 0.23±0.56 | 0.03a,c | 0.05±0.98 | 0.44c | 0.74±1.31 | 0.02a,b |
| N15 | –0.18±0.46 | 0.09b | –0.33±0.58 | 0.02a,b | 0.26±0.6 | 0.07b | 0.45±0.64 | 0.01a,b | 0.33±1.25 | 0.25b |
| N10 | –0.11±0.35 | 0.19b | –0.22±0.5 | 0.07a,b | 0.18±0.5 | 0.12b | 0.32±0.65 | 0.04a,b | 0.31±1.04 | 0.19b |
| N5 | –0.06±0.18 | 0.14b | –0.12±0.42 | 0.26c | 0.31±0.38 | < 0.01a,b | 0.35±0.6 | 0.02a,b | 0.2±0.84 | 0.3b |
| T5 | –0.07±0.2 | 0.13b | –0.17±0.31 | 0.02a,b | 0.07±0.38 | 0.2c | –0.11±0.78 | 0.52b | –0.09±1.46 | 0.53c |
| T10 | –0.39±0.29 | < 0.01a,b | –0.31±0.41 | < 0.01a,b | –0.43±0.49 | < 0.01a,b | –0.86±0.91 | < 0.01a,b | –0.85±1.14 | < 0.01a,b |
| T15 | –0.69±0.36 | < 0.01a,b | –0.52±0.84 | < 0.01a,c | –0.77±0.5 | < 0.01a,b | –1.4±1.05 | < 0.01a,b | –1.62±1.18 | < 0.01a,b |
| T20 | –0.99±0.47 | < 0.01a,b | –0.9±0.64 | < 0.01a,b | –1.21±0.59 | < 0.01a,b | –1.95±1.1 | < 0.01a,b | –2.15±1.46 | < 0.01a,b |
| T25 | –1.26±0.65 | < 0.01a,b | –1.33±0.89 | < 0.01a,b | –1.58±0.78 | < 0.01a,b | –2.47±1.14 | < 0.01a,b | –2.6±1.7 | < 0.01a,b |
| T30 | –1.66±0.96 | < 0.01a,b | –1.54±1.06 | < 0.01a,b | –1.7±1.09 | < 0.01a,b | –2.76±1.48 | < 0.01a,b | –2.68±2.8 | < 0.01a,b |
| T35 | –2.3±1.16 | < 0.01a,b | –1.78±1.4 | < 0.01a,b | –2.15±1.1 | < 0.01c | –3.15±1.85 | < 0.01a,b | –3.43±2.29 | < 0.01a,b |
C: center; N: nasal retina; T: temporal retina.
p represents the value of statistical significance according to:
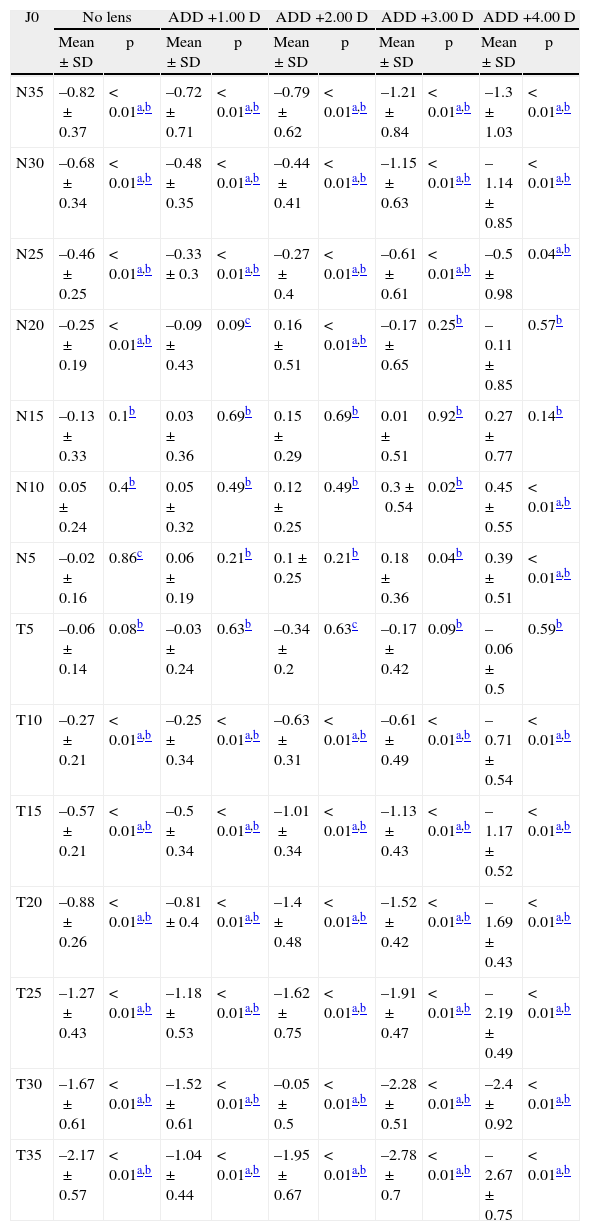
Difference in the values of J0 component between different eccentric points and central value (relative peripheral refractive error) for the five experimental conditions: baseline (No lens), +1.00 D addition (ADD +1.00 D), +2.00 D addition (ADD +2.00 D), +3.00 D addition (ADD +3.00 D) and +4.00 D addition (ADD +4.00 D). Values are expressed in diopters
| J0 | No lens | ADD +1.00 D | ADD +2.00 D | ADD +3.00 D | ADD +4.00 D | |||||
| Mean±SD | p | Mean±SD | p | Mean±SD | p | Mean±SD | p | Mean±SD | p | |
| N35 | –0.82±0.37 | < 0.01a,b | –0.72±0.71 | < 0.01a,b | –0.79±0.62 | < 0.01a,b | –1.21±0.84 | < 0.01a,b | –1.3±1.03 | < 0.01a,b |
| N30 | –0.68±0.34 | < 0.01a,b | –0.48±0.35 | < 0.01a,b | –0.44±0.41 | < 0.01a,b | –1.15±0.63 | < 0.01a,b | –1.14±0.85 | < 0.01a,b |
| N25 | –0.46±0.25 | < 0.01a,b | –0.33±0.3 | < 0.01a,b | –0.27±0.4 | < 0.01a,b | –0.61±0.61 | < 0.01a,b | –0.5±0.98 | 0.04a,b |
| N20 | –0.25±0.19 | < 0.01a,b | –0.09±0.43 | 0.09c | 0.16±0.51 | < 0.01a,b | –0.17±0.65 | 0.25b | –0.11±0.85 | 0.57b |
| N15 | –0.13±0.33 | 0.1b | 0.03±0.36 | 0.69b | 0.15±0.29 | 0.69b | 0.01±0.51 | 0.92b | 0.27±0.77 | 0.14b |
| N10 | 0.05±0.24 | 0.4b | 0.05±0.32 | 0.49b | 0.12±0.25 | 0.49b | 0.3±0.54 | 0.02b | 0.45±0.55 | < 0.01a,b |
| N5 | –0.02±0.16 | 0.86c | 0.06±0.19 | 0.21b | 0.1±0.25 | 0.21b | 0.18±0.36 | 0.04b | 0.39±0.51 | < 0.01a,b |
| T5 | –0.06±0.14 | 0.08b | –0.03±0.24 | 0.63b | –0.34±0.2 | 0.63c | –0.17±0.42 | 0.09b | –0.06±0.5 | 0.59b |
| T10 | –0.27±0.21 | < 0.01a,b | –0.25±0.34 | < 0.01a,b | –0.63±0.31 | < 0.01a,b | –0.61±0.49 | < 0.01a,b | –0.71±0.54 | < 0.01a,b |
| T15 | –0.57±0.21 | < 0.01a,b | –0.5±0.34 | < 0.01a,b | –1.01±0.34 | < 0.01a,b | –1.13±0.43 | < 0.01a,b | –1.17±0.52 | < 0.01a,b |
| T20 | –0.88±0.26 | < 0.01a,b | –0.81±0.4 | < 0.01a,b | –1.4±0.48 | < 0.01a,b | –1.52±0.42 | < 0.01a,b | –1.69±0.43 | < 0.01a,b |
| T25 | –1.27±0.43 | < 0.01a,b | –1.18±0.53 | < 0.01a,b | –1.62±0.75 | < 0.01a,b | –1.91±0.47 | < 0.01a,b | –2.19±0.49 | < 0.01a,b |
| T30 | –1.67±0.61 | < 0.01a,b | –1.52±0.61 | < 0.01a,b | –0.05±0.5 | < 0.01a,b | –2.28±0.51 | < 0.01a,b | –2.4±0.92 | < 0.01a,b |
| T35 | –2.17±0.57 | < 0.01a,b | –1.04±0.44 | < 0.01a,b | –1.95±0.67 | < 0.01a,b | –2.78±0.7 | < 0.01a,b | –2.67±0.75 | < 0.01a,b |
C: center; N: nasal retina; T: temporal retina.
p represents the value of statistical significance according to:
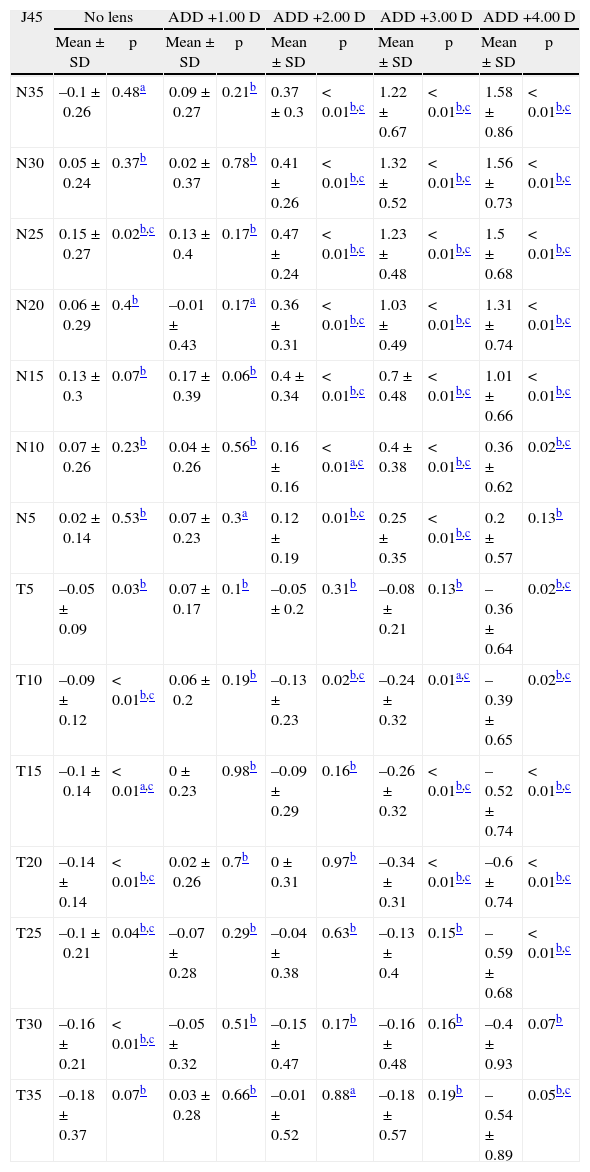
Difference in the values of J45 component between different eccentric points and central value (relative peripheral refractive error) for the five experimental conditions: baseline (No lens), +1.00 D addition (ADD +1.00 D), +2.00 D addition (ADD +2.00 D), +3.00 D addition (ADD +3.00 D) and +4.00 D addition (ADD +4.00 D). Values are expressed in diopters
| J45 | No lens | ADD +1.00 D | ADD +2.00 D | ADD +3.00 D | ADD +4.00 D | |||||
| Mean±SD | p | Mean±SD | p | Mean±SD | p | Mean±SD | p | Mean±SD | p | |
| N35 | –0.1±0.26 | 0.48a | 0.09±0.27 | 0.21b | 0.37±0.3 | < 0.01b,c | 1.22±0.67 | < 0.01b,c | 1.58±0.86 | < 0.01b,c |
| N30 | 0.05±0.24 | 0.37b | 0.02±0.37 | 0.78b | 0.41±0.26 | < 0.01b,c | 1.32±0.52 | < 0.01b,c | 1.56±0.73 | < 0.01b,c |
| N25 | 0.15±0.27 | 0.02b,c | 0.13±0.4 | 0.17b | 0.47±0.24 | < 0.01b,c | 1.23±0.48 | < 0.01b,c | 1.5±0.68 | < 0.01b,c |
| N20 | 0.06±0.29 | 0.4b | –0.01±0.43 | 0.17a | 0.36±0.31 | < 0.01b,c | 1.03±0.49 | < 0.01b,c | 1.31±0.74 | < 0.01b,c |
| N15 | 0.13±0.3 | 0.07b | 0.17±0.39 | 0.06b | 0.4±0.34 | < 0.01b,c | 0.7±0.48 | < 0.01b,c | 1.01±0.66 | < 0.01b,c |
| N10 | 0.07±0.26 | 0.23b | 0.04±0.26 | 0.56b | 0.16±0.16 | < 0.01a,c | 0.4±0.38 | < 0.01b,c | 0.36±0.62 | 0.02b,c |
| N5 | 0.02±0.14 | 0.53b | 0.07±0.23 | 0.3a | 0.12±0.19 | 0.01b,c | 0.25±0.35 | < 0.01b,c | 0.2±0.57 | 0.13b |
| T5 | –0.05±0.09 | 0.03b | 0.07±0.17 | 0.1b | –0.05±0.2 | 0.31b | –0.08±0.21 | 0.13b | –0.36±0.64 | 0.02b,c |
| T10 | –0.09±0.12 | < 0.01b,c | 0.06±0.2 | 0.19b | –0.13±0.23 | 0.02b,c | –0.24±0.32 | 0.01a,c | –0.39±0.65 | 0.02b,c |
| T15 | –0.1±0.14 | < 0.01a,c | 0±0.23 | 0.98b | –0.09±0.29 | 0.16b | –0.26±0.32 | < 0.01b,c | –0.52±0.74 | < 0.01b,c |
| T20 | –0.14±0.14 | < 0.01b,c | 0.02±0.26 | 0.7b | 0±0.31 | 0.97b | –0.34±0.31 | < 0.01b,c | –0.6±0.74 | < 0.01b,c |
| T25 | –0.1±0.21 | 0.04b,c | –0.07±0.28 | 0.29b | –0.04±0.38 | 0.63b | –0.13±0.4 | 0.15b | –0.59±0.68 | < 0.01b,c |
| T30 | –0.16±0.21 | < 0.01b,c | –0.05±0.32 | 0.51b | –0.15±0.47 | 0.17b | –0.16±0.48 | 0.16b | –0.4±0.93 | 0.07b |
| T35 | –0.18±0.37 | 0.07b | 0.03±0.28 | 0.66b | –0.01±0.52 | 0.88a | –0.18±0.57 | 0.19b | –0.54±0.89 | 0.05b,c |
C: center; N: nasal retina; T: temporal retina.
p represents the value of statistical significance according to:
Figures 3 and 4 show the effects of increasing add on peripheral astigmatic components of refraction. While no significant effect has been observed on J0, there is a marked increase in J45 component as the add power exceeds the 2 diopters of add. Significance values for comparision between central and peripheral locations without and with each lens are provided in Tables 3 and 4.
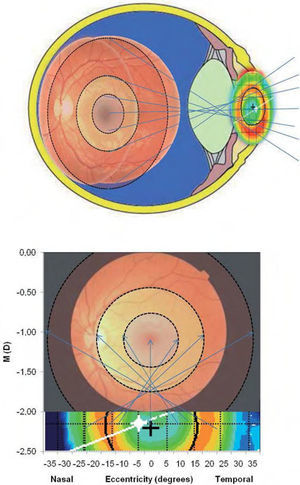
DiscussionMyopization of the peripheral visual field has been suggested as one of the potential strategies to affect patterns of ocular growth to avoid progression of myopia. This is usually accomplished by orthokeratology contact lens fitting, and different studies have shown to be effective to achieve myopia progression control.20,21 The present study has demonstrated that a similar effect on peripheral refraction can be achieved by using a multifocal center-distance soft contact lens. The retinal area affected by this approach can be easily visualized in Figure 5 suggesting that the myopization effect with these lenses begins already in the parafoveal area and extends up to the 70 degrees of eccentricity.
Graphical representation of the areas in the retina affected by the change in refraction induced by the multifocal contact lens. The draw assumes an asymmetrical distribution of myopic effect arround the fovea in every direction althouth present study only analyzes the horizontal meridian.
With the present work we have demonstrated that up to –6 D of peripheral spherical equivalent can be achieved by fitting a distance plano Proclear multifocal with dominant design. Moreover, we have shown that +1.00 and +2.00 D add lenses have not practical effects on peripheral myopization compared to baseline, while +4.00 D add lenses did not provided any advantage over +3.00 D add lens in terms of peripheral myopization, but significantly increased the central myopia what could be considered a negative issue because of potential interference with distance vision, particularly under low lighting conditions.
This unexpected effect of increasing central myopia with +3.00 D and particularly with +4.00 D add lenses might be related with an artifact from the Grand Seiko WAM 5500 open-field autorefractometer because the light beam used to compute refractive error is about the same size (2.3 to 2.5mm) of the central area intended for distance power (about thus simulating an increase in myopic refractive error when part of the light beam passes through the add ring surrounding the central area). These methodological concerns relating to the measuring method of these kind of instruments are recognized by the authors. However, as most of recent studies had been conducted with the same methodologies, the results continue being comparable with other authror's studies. Furthermore, slight decentration of the lens will magnify this effect. Other aspects such as lens decentration or movement during blinking might also contribute to compromise the target of plano power at distance. For the aforementioned reasons +3.00 D add power will be more suitable to achieve such a peripheral myopization without much compromise for central vision induced by the higher add lens.
The main limitation of the present study is that it has been conducted in emmetropes whose peripheral retinal profile might differ significantly from myopes.8 This must to be considered in future studies. The optical design of multifocal lenses with distance myopic correction might be different particularly regarding the distribution of power and the size of areas intended for distance and near vision when fitted in myopes. Considering this, the results of the present study might not be extrapolated directly to the myopic population because those patients will potentially have a different baseline refractive profile across the peripheral visual field and the mentioned potential differences in the optical design of the lenses might render different results from those obtained in emmetropes. Furthermore, another methodological limitation is the fact that we did not measure the peripheral refraction with plano lenses (non-multifocal design) what could be considered a better term of comparison as baseline condition. However, considering the lack of significant changes in peripheral refractive profile observed with the +1.00 D add lens, it is not expected to obtain any different results with a spherical plano lens. Moreover, different studies have shown that single vision contact lenses do not affect the pattern of peripheral refraction and has been used to correct defocus in other peripheral refraction experiments.29 Lens centration was not controlled in this study. However, it is not likely that the lack of symmetry between refractive data in the nasal and temporal areas of the visual field can be related with lens decentration as this effect is also observed in the baseline condition.
With the present study we do not attempt to claim the efficacy of Proclear Multifocal contact lens as a treatment for altering the pattern of ocular growth. Moreover, we cannot prove if the amount myopic defocus would be enough to prevent myopia progression nor if the power distribution of these lenses for myopic patients (with central distance minus correction) could play a similar role in peripheral defocus. Further studies with myopic populations might be conducted in order to allow a better characterization of the present experimental results on those patients that may potentially benefit from this fitting approach.
Conflict of interestsThe authors declare that they do not have any proprietary or financial interest in any of the materials mentioned in this article.
This research was supported in part by FCT – Portuguese Ministry of Science and European Social Funding under contract #PTDC/SAU-BEB/098392/2008# and #PTDC/SAU-BEB/098391/2008# and by the Ministry of Science and Innovation of Spain (Red Temática de Investigación en Optometría, SAF2008-01114-E).